Abstract
Background
An obesity paradox has been described in relation to adverse clinical outcomes (e.g., mortality) with lower body mass index (BMI).
Aims
We sought to evaluate the association between BMI and weight loss with long-term all-cause mortality in adult populations under the care of family physicians.
Methods
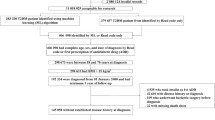
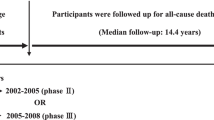
LIPIDOGRAM studies were conducted in primary care in Poland in 2004, 2006, and 2015 and enrolled a total of 45,615 patients. The LIPIDOGRAM Plus study included 1627 patients recruited in the LIPIDOGRAM 2004 and repeated measurements in 2006 edition. Patients were classified by BMI categories as underweight, normal weight, overweight and class I, II, or III (obesity). Follow-up data up to December 2021 were obtained from the Central Statistical Office. Differences in all-cause mortality were analyzed using Kaplan‒Meier and Cox regression analyses.
Results
Of 45,615 patients, 10,987 (24.1%) were normal weight, 320 (0.7%) were underweight, 19,134 (41.9%) were overweight, and 15,174 (33.2%) lived with obesity. Follow-up was available for 44,620 patients (97.8%, median duration 15.3 years, 61.7% females). In the crude analysis, long-term all-cause mortality was lowest for the normal-weight group (14%) compared with other categories. After adjusting for comorbidities, the highest risk of death was observed for the class III obesity and underweight categories (hazard ratio, HR 1.79, 95% CI [1.55–2.05] and HR 1.57, 95% CI [1.22–2.04]), respectively. The LIPIDOGRAM Plus analysis revealed that a decrease in body weight (by 5 and 10%) over 2 years was associated with a significantly increased risk of death during long-term follow-up—HR 1.45 (95% CI 1.05–2.02, p = 0.03) and HR 1.67 (95% CI 1.02–2.74, p < 0.001). Patients who experienced weight loss were older and more burdened with comorbidities.
Conclusions
Being underweight, overweight or obese is associated with a higher mortality risk in a population of patients in primary care. Patients who lost weight were older and more burdened with cardiometabolic diseases, which may suggest unintentional weight loss, and were at higher risk of death in the long-term follow-up. In nonsmoking patients without comorbidities, the lowest mortality was observed in those with a BMI < 25 kg/m2, and no U-curve relationship was observed.
Similar content being viewed by others
Introduction
Overweight and obesity are recognized risk factors for diabetes mellitus (DM), myocardial infarction (MI), hypertension (HTN) and heart failure (HF), as well as cancers, which are the main causes of mortality in developed countries [1,2,3,4,5,6]. Despite the continuous increase in body mass index (BMI) in various populations over the last decade [7] and the well-documented negative effects of obesity on the risk of developing the abovementioned diseases, some doubts persist as to the relationship between BMI and patient prognosis [7, 8].
Lower mortality in overweight patients or patients living with obesity compared with patients with a BMI within the normal values was reported in subpopulations with atherosclerotic cardiovascular diseases (ASCVD), especially stroke, acute coronary syndromes (ACS), HF as well as DM [9, 10]. Thus, there is a paradoxical contradiction between the recommendations [11] to reduce body weight in the case of overweight and obesity and reports on the alleged protective effect of increased BMI in some groups of patients. Therefore, we aimed to assess the association between BMI and weight loss long-term all-cause mortality in a population of adult patients under the care of family physicians in Poland.
Methods
Design
We conducted a nationwide cohort study in which patients in 2004, 2006 and 2015 were recruited by a random sample of primary care practices and all-cause mortality was observed until the end of 2021.
Study population
LIPIDOGRAM is a nationwide survey of cardiovascular risk factors carried out through primary care outpatient centers in Poland in 2004, 2006 and 2015–2016. The methodology of the LIPIDOGRAM2004, LIPIDOGRAM2006 and LIPIDOGRAM 2015 studies were described in detail elsewhere [12,13,14]. Briefly, physicians were selected randomly, using Medical Data Management Software. The number of physicians in each administrative region in Poland was selected in a manner proportional to the number of inhabitants. All consecutive patients aged ≥ 18 years were eligible for recruitment. In 2004, a total of 675 primary care physicians (PCPs) enrolled 17,522 patients in 444 cities. In 2006, 556 PCPs from 402 Polish cities recruited a total of 15,465 patients, while in 2015–2016 a group of 438 PCPs from 398 cities recruited additional 13,724 patients. After exclusion of doubled and incomplete records, 45,615 unique records were available for analysis. In conjunction with the LIPIDOGRAM 2004 and 2006 studies, the LIPIDOGRAM PLUS study encompassed 1627 patients who had repeated anthropometric and laboratory measurements in 2004 and 2006. Follow-up data were obtained from the Central Statistical Office using a unique identification number for each patient. The data were collected up to December 2021.
Anthropometric measurements and physical examination
Height and weight measurements were carried out by nurses or physicians on patients in their underwear and barefoot. BMI was calculated by dividing body weight in kilograms (kg) by squared height in meters (m) (kg/m2). Waist circumference (WC) was measured at the midpoint between the lower margin of the ribs and the anterior superior iliac crest spine in centimeters (cm).
Biochemical analyses
Blood samples were collected after fasting (> 12 h following last meal, there were no restrictions with regard to water intake). After centrifugation, blood samples were transferred to a core facility for processing. Biochemical analyses were performed within 12 h after blood sample collection in the core lab in Katowice, Poland. Serum concentrations of total cholesterol (TC) were measured using a photometric method. High density lipoprotein (HDL) cholesterol (HDL-C) and triglycerides (TG) were measured by an immunoseparation-based homogenous assay and colorimetric enzymatic test with glycerol-3-phosphate oxidase, respectively (DiaSys—Diagnostic Systems, Holzheim, Germany). Low density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald formula (LIPIDOGRAM2004 and LIPIDOGRAM2006 surveys) or was measured directly (LIPIDOGRAM2015).
Definitions
Patients within BMI categories of < 18.5, 18.5–24.9, 25–29.9, 30–34.9,35–39.99, and ≥ 40 kg/m2 were considered underweight, normal weight, overweight and living with obesity class I, class II and class III, respectively. Metabolic syndrome (MetS) was diagnosed according to the Joint Interim Statement Criteria (JIS) criteria [15]. Dyslipidemia was diagnosed by fulfilling at least one of the following criteria: increased LDL-C (> 115 mg/dl; > 3 mmol/l) or statin treatment. DM and HTN were diagnosed by the primary care physicians according to the contemporary guidelines [16,17,18,19].
Statistical analyses
Continuous variables are presented as means and standard deviations (SD). The comparison of continuous variables across BMI categories was performed using the Kruskal‒Wallis test. The comparison of dichotomous variables was performed using the chi-square test. Non-adjusted and adjusted associations between mortality and BMI categories (underweight, normal weight, overweight, class 1 obese, class 2 obese, class 3 obese) were assessed using a Cox regression model. In the latter, in addition to BMI categories, age, sex (male, female), education (higher/secondary vs primary/vocational), smoking, place of residence (urban vs rural), DM, HTN, and dyslipidemia were included. As BMI categories are to some extent arbitrary, we visualized associations between the hazard ratio of mortality and BMI by plotting adjusted and unadjusted Cox regression models using a penalized spline basis.
We also used a Cox regression model with penalized splines to assess the association between change in body weight and mortality in patients from the LIPDIOGRAM PLUS sub-study for whom we had repeated anthropometric and laboratory measurements. Additionally, Kaplan‒Meier analysis was carried out among patients from the LIPDIOGRAM plus sub-study stratified by a decrease in body weight of 5% and 10% over 2 years of follow-up.
Kaplan‒Meier analysis was carried out to explore associations between changes in BMI and long-term prognosis. A 2-sided p < 0.05 was considered statistically significant.
Ethics
The study protocol was approved by the Bioethical Committee of the Polish Chamber of Physicians (no. 51/2004/U) for 2004/2006 and by the Bioethical Commission of the District Medical Chamber in Częstochowa (no K.B.Cz.–0018/2015) for years 2015.
Results
Baseline characteristics
In the studied population of 45,615 patients, 10,987 (24.1%) were classified as normal weight, 19,134 (41.9%) were overweight and 320 (0.7%) patients had BMI below 18.5 kg/m2. Among the 15,174 (33.3%) patients with obesity, 11,117 (24.4%) were classified as having class I obesity, 3153 (6.9%) as having class II obesity, and 904 (2.0%) met the criteria for class III obesity. Baseline characteristics of the studied population are summarized in Table 1.
There was a significant increase in the incidence of HTN, DM and dyslipidemia in both sexes as BMI increased (Table 1). In both female and male, a greater percentage of patients meeting the criteria for MetS across BMI categories was observed (see Additional file 1: Tables 1 and 2). In the entire cohort, as well as in female and male, the prevalence of smoking was highest in patients with the lowest BMI (Table 1; Additional file 1: Tables and 2). Patients with higher BMI more often lived in rural areas and had lower education levels compared with normal weight and underweight patients (Table 1; Additional file 1: Tables 1 and 2). In the entire cohort as well as among males, a history of MI was most prevalent in overweight and class I obese patients (Table 1; Additional file 1: Table 2). These groups also had the highest levels of LDL-C and TC in patients living with overweight and class I obesity in both the whole cohort and the male subpopulation (Table 1; Additional file 1: Table 2). Among females, the prevalence of previous MI was similar across overweight to class III obesity categories and was on average one-third higher than in underweight and normal weight patients (see Additional file 1: Table 1). Despite this, LDL-C levels differed by less than 0.4 mmol/L across BMI categories in the entire cohort in female as well as in male. HDL-C values decreased with increasing BMI, while TG levels increased with increasing BMI by 0.7 mmol/L between normal weight patients and those living with class III obesity. The lowest values of HDL-C and highest values of TG were observed in patients living with class III obesity (Table 1; Additional file 1: Tables 1 and 2). In general, the incidence of cardiovascular risk factors seen in both male and female individually follows trends found in the general population. They are presented in detail in Additional file 1: Tables 1 and 2.
Survival analysis
Follow-up data were available for 44,620 patients. Within the median follow-up of 15.3 years, we observed 7559 (16.9%) deaths, including 60 (19.3%) for underweight, 1532 (14.3%) for normal weight 3085 (16.5%) for patients living with overweight and 1996 (18.3%), 651 (21.0%) and 235 (26.3%) for patients living with class I, II and III obesity, respectively.
In the univariate analysis, the lowest long-term mortality was observed in patients of normal weight. The risk of death during the entire observation period increased from a hazard ratio (HR) of 1.13 (95% confidence interval (CI) 1.07–1.21) for overweight patients through HR of 1.31 (95% CI, 1.22–1.40, p < 0.001) and 1.58 (95% CI, 1.45–1.74, p < 0.001) for class I and class II obesity respectively to an HR of 2.14 (95% CI, 1.87–2.45, p < 0.001) for patients living with class III obesity. In unadjusted analysis, patients who were underweight experienced similar mortality rates as patients with class I obesity (HR 1.35 (95% CI, 1.04–1.75, p < 0.001) (Fig. 1 and Fig. 2). Similar trend was observed in the female subgroup, but in the male group the lowest mortality was observed in overweight patients. (see Additional file 1: Figure 1). In a subgroup analysis of patients after MI and in patients suffering from DM lowest mortality was observed for overweight and obese patients. In subgroup of cigarette smokers and individuals with dyslipidemia relationship between BMI and mortality resembled this from general population (see Additional file 1: Figure 2). Interestingly in nonsmoking patients without comorbidities, the lowest mortality was observed for underweight and normal weight patients (see Additional file 1: Figure 3).
In the multivariate analysis, after adjustment for covariates, an apparent survival advantage was observed for overweight and class I obese patients—a “shift” in the BMI value for which mortality was the lowest could be observed, a similar result has been reported previously [20]. The highest mortality was observed for patients with class III obesity and those who were underweight (HR: 1.79, (95% CI 1.55–2.05, p < 0.001) and HR 1.57, (95% CI 1.22–2.04, p < 0.001), respectively) suggesting a U-shaped curve relationship (Figs. 1, 2). In the LIPIDOGRAM PLUS substudy, follow-up data on all-cause mortality were available for 1625 out of 1627 participants (99.9%). The analysis of this cohort showed a significant increase in the long-term mortality risk associated with a 5% and 10% reduction in body weight over two years. The mean weight loss in patients who experienced 5% reduction in body weight was 8.0 kg (SD-5.0 kg, min 3.0 kg max 37.0 kg) while the corresponding values in patients who lost 10% of their body weight were 12.4 kg (SD- 61 kg, min 5.0 kg max 37.0 kg). The corresponding HRs were 1.45 (95% CI 1.05–2.02, p = 0.03) for patients with at least 5% body weight reduction and 1.67 (95% CI 1.02–2.74, p < 0.001) for patients with at least 10% body weight reduction, respectively (Fig. 3). Notably, patients who experienced weight loss tended to have higher initial BMIs, be older, smoke more, have diabetes, and suffer from HTN more frequently (see Additional file 1: Tables 3 and 4).
Discussion
In this analysis from a population of > 45 000 consecutive patients under the care of family physicians, BMI within the normal range was present in only one in four patients. Furthermore, one in three participants had a BMI > 30 kg/m2. When not adjusted for comorbidities, normal weight was associated with the lowest mortality. These results are consistent with a large meta-analysis on BMI and all-cause mortality including > 10 million participants, which also reported the lowest all-cause mortality for normal weight patients [21]. On the other hand, studies involving patients with chronic coronary artery disease [20, 22, 23], acute coronary syndromes [24], DM [25], heart failure [26], and cancer [27] reported the lowest mortality for overweight patients or obese patients and an increase in mortality for underweight patients and for subjects in class II or III obesity. In our subgroup analyses of patients after MI and patients with DM we also observed presence of obesity paradox with lowest mortality for overweight patients and patients living with class I obesity.
It was shown that a normal weight trajectory is associated with the greatest body weight gain in males younger than 40 years and females under 50 years of age, and peak weight is typically reached between 50 and 69 years of age [28, 29]. In most instances, subjects who experience weight loss do so unintentionally [28]. Therefore greater BMI may in fact be an indicator of better health status in those age groups as compared to BMI within normal range or below 18.5 kg/m2. It might be especially true in those observational and cross-sectional studies where we do not have data on weight loss trajectory before enrollment and lower BMI might often a result of an underlying ongoing disease rather than a change in lifestyle. In patients with end-stage chronic diseases, such as HF and cancer, a predominance of catabolic processes, loss of appetite, impairment of digestion resulting in caloric restriction and malnutrition contribute to increased mortality [29,30,31,32,33,34,35,36]. In patients with diabetes, weight loss is a marker of disease severity and loss of physical reserve and insufficient insulin secretion [25]. Therefore, the obesity paradox in advanced stages of cardiovascular diseases, cancers and diabetes should be explained by lower body weight and muscle wasting and even bone mass loss, which result in worse prognosis, not vice versa [37]. Others also observed that a change in body weight from overweight/obese to normal weight or underweight may result primarily from unintentional reduction of muscle mass [38, 39]. It raises doubts about any practical implications of the obesity paradox, except for the obvious necessity of searching for the underlying cause of weight loss. This is also in line with the results of our study, as the obesity paradox was present in subgroups of patients with MI and DM while in general cohort it was observed only after adjustment for comorbidities. More importantly patients who lost weight were more burdened with comorbidities and in non-smoking patients without comorbidities mortality benefit was observed even in lower end of normal weight category.
The results of other studies also show that intentional weight loss (including bariatric surgery) might be associated with mortality benefit and reduction of cardiovascular events but unintentional weight loss is not [40, 41]. Most of observational studies, including ours, do not analyze if the weight loss was intentional or not which may greatly affect conclusions regarding obesity paradox. Intentional weight loss, and incorporating lifestyle changes is challenging and for many difficult to maintain. Studies from the same period as the LIPIDOGRAM PLUS study, show that, approximately 1/3 of patients analyzed in cross sectional studies undertake some action to lose body weight [28, 42]. Of these, only 20% are successful at sustaining a lower weight. The remaining two thirds do not engage in any action to lower body weight and despite this, as much as 30% experience unintentional weight loss [28, 42]. Recent data from the STEP1 (Effect and Safety of Semaglutide 2.4 mg once weekly in Subjects With Overweight or Obesity) trial show that one year after cessation of treatment with semaglutide, participants regained 2/3 of their prior weight loss [43].
On the basis of data from other epidemiological studies as well as from the fact that the obesity paradox appeared after adjustment for clinical characteristic including comorbidities and that weight loss was associated with worse long-term prognosis, we might assume that in most patients, weight loss was unintentional. As mentioned earlier the concept of the obesity paradox was seen mostly in observational studies that in vast majority do not have information on whether body weight loss was intentional or not [24, 44, 45].
Another possible cause of the high mortality among underweight people in our study is the high percentage of smokers in this group. Numerous studies indicate that the primary factor in the increase in mortality among smokers is lung cancer [46, 47]. In addition, because nicotine hinders appetite, it is easier for smokers to maintain their BMI and not gain weight [48, 49]. The fear of gaining weight is also one of the factors that make it difficult to quit smoking [50]. The results of our analysis showed that in nonsmokers without DM or a history of MI, the risk of mortality was lowest among patients with BMI within lower end of normal body weight category, and it increased with increasing BMI. Similarly, Veronese et al. showed that people with a BMI within the normal range (18.5–22.4 kg/m2), maintaining a healthy diet, engaging in physical activity, moderation in the use of stimulants, and not smoking, had the lowest risk of premature death [51].
In our study, obesity paradox is indeed apparent in adjusted analysis and subgroup analyses (Additional file 1: Figures 2 and 3). Nevertheless, some superficial “beneficial” effects of obesity in patients with comorbidities can be at least partially explained by collider stratification bias [52, 53]. Colliders are factors that are correlated with both the exposure (BMI) and other factors. Collider stratification bias occurs when study inclusion criteria, adjustment or stratification depend on the collider(s). This creates a non-causal correlation between the exposure and factors that affect the collider [52, 54]. It may partially explain that obesity paradox was observed in studies including only patients with certain diseases i.e. diabetes, heart failure etc. but less often in general populations. In case of our work, colliders would be those conditions whose frequency increases with increasing BMI such as previous MI, DM, dyslipidemia, HTN. At the same time, occurrence of those colliders is also influenced by factors such as smoking, sex, education, place of residence or non-measured factors such as genetic influences. An example of collider bias may be a situation in which MI (collider) is caused by obesity and/or smoking. In this case, in the subgroup of patients defined by the collider (previous MI) those with a higher BMI would have an observed tendency not to have other factors that predispose towards MI. In this case higher BMI would appear protective, as in the subgroup defined by collider, it would be negatively correlated with factors like smoking, which may have a more negative impact on survival than BMI itself [12]. We are also the opinion that unmeasured variables such as time elapsed from the occurrence of obesity to the enrollment of participants and intentionality of body weight reduction are the two most important unmeasured confounders missing in our and other observational studies that evaluate the relationship between obesity and mortality (Fig. 4).
Collider stratification bias as an explanation of obesity paradox. A directed acyclic graph representing the relations between obesity (BMI), cardiometabolic mediators and mortality. Dashed red lines represent correlations created by conditioning/adjusting on colliders. The true causal effect of obesity on mortality may be largely mediated by cardiometabolic diseases. As those diseases can also be influenced by factors other than BMI, they are colliders. Subgroup analyses involving patients with or without cardiometabolic diseases are subject to collider bias as non-causal correlations between confounders and obesity are created
Study strengths and limitations
The main strength of this study is the inclusion of a large number of patients. Importantly, patients involved in the study were recruited from all 16 regions of Poland and were representative of the primary health care population. Another strength of the study is that all the biochemical measurements were conducted in a central laboratory, which conforms to all the required quality control standards; this ensures the reliability of the results. Medical history and office measurements were collected by doctors who knew the patients and looked after them on a regular basis. In 2004 and 2006, the data gathered were the same, but in 2015 this was extended to include blood pressure, heart rate and blood glucose.
A limitation of the study is that it was conducted in only one country. Primary healthcare practices were selected at random, but physicians enrolled patients consecutively. Moreover, we did not gain access to data on the causes of death of patients; therefore, we conducted our analysis based on all-cause death. Data pertaining to factors that influenced weight change in each patient were also unavailable. Additionally, although BMI is a popular measure of obesity, other indices also exist, some of which could be less prone to “obesity paradox”. While it remains possible that some beneficial effects of obesity on survival exist in some populations, this would need to be contrary to the trend in the overall population. Nevertheless, if those populations suffer from conditions caused in part by obesity, observational studies like this one are difficult to interpret due to potential for collider bias and factors that influence both weight and mortality.
In medical sciences, counterintuitive results—such as those from the ACCORD Study on aggressive glycemic control in diabetes or the Minnesota Coronary Experiment—can lead to important discoveries [55, 56]. We therefore acknowledge the possibility of some protective effects of obesity, as recently postulated by the increased levels of plasminogen activator inhibitor 1 in obese patients with MI, which we were not able to test in this analysis [57].
Conclusions
Being underweight, overweight or obese is associated with higher mortality risk in a population of patients in primary care. Patients who lost weight were older and more burdened with cardiometabolic diseases which may suggest unintentional weight loss and were at higher risk of death in the long-term follow-up. In nonsmoking patients without comorbidities, the lowest mortality was observed in those with a BMI < 25 kg/m2 and mortality benefit was observed even in the lower range of normal weight interval and no U-curve relationship was observed. Obesity paradox should not be a reason to advocate possible benefits of weight gain in normal weight individuals.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347(5):59–60. https://doi.org/10.1056/NEJMOA020245.
Manson JE, Colditz GA, Stampfer MJ, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 2010;322(13):882–9. https://doi.org/10.1056/NEJM199003293221303.
Yousufuddin M, Takahashi PY, Major B, et al. Association between hyperlipidemia and mortality after incident acute myocardial infarction or acute decompensated heart failure: a propensity score matched cohort study and a meta-analysis. BMJ Open. 2019;9(12):1–12. https://doi.org/10.1136/bmjopen-2018-028638.
Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007;8(1):41–59. https://doi.org/10.1111/J.1467-789X.2006.00248.X.
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335(7630):1134–9. https://doi.org/10.1136/BMJ.39367.495995.AE.
Banach M, Burchardt P, Chlebus K, et al. WYTYCZNE PTL/KLRwP/PTK/ PTDL/PTD/PTNT DIAGNOSTYKI I LECZENIA ZABURZEŃ LIPIDOWYCH W POLSCE 2021. Lekarz POZ Suplement. Published online 2021. https://www.termedia.pl/WYTYCZNE-PTL-KLRwP-PTK-r-nPTDL-PTD-PTNT-DIAGNOSTYKI-r-nI-LECZENIA-ZABURZEN-r-nLIPIDOWYCH-W-POLSCE-2021,166,45338,1,1.html
Global InfoBase W. The SuRF Report 2 Surveillance of chronic disease Risk Factors: Country-level data and comparable estimates The SuRF Report 2 CD-rom included The SuRF Report 2-Country-level data and comparable estimates.
Bentham J, Di Cesare M, Bilano V, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42. https://doi.org/10.1016/S0140-6736(17)32129-3.
Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. 2014;63(14):1345–54. https://doi.org/10.1016/J.JACC.2014.01.022.
Alagiakrishnan K, Banach M, Ahmed A, Aronow WS. Complex relationship of obesity and obesity paradox in heart failure - higher risk of developing heart failure and better outcomes in established heart failure. Ann Med. 2016;48(8):603–13. https://doi.org/10.1080/07853890.2016.1197415.
Dobrowolski P, Prejbisz A, Kuryłowicz A, et al. Guidelines/Recommendations Metabolic Syndrome Metabolic syndrome-a new definition and management guidelines. Agnieszka Mastalerz-Migas. 2022;16:24. https://doi.org/10.5114/aoms/152921.
Osadnik K, Osadnik T, Gierlotka M, et al. Metabolic syndrome is associated with similar long-term prognosis in non-obese and obese patients. An analysis of 45 615 patients from the nationwide LIPIDOGRAM 2004–2015 cohort studies. Eur J Prev Cardiol. 2023. https://doi.org/10.1093/eurjpc/zwad101.
Kaess BM, Jóźwiak J, Nelson CP, et al. The relation of rapid changes in obesity measures to lipid profile—insights from a nationwide metabolic health survey in 444 Polish cities. PLoS ONE. 2014. https://doi.org/10.1371/JOURNAL.PONE.0086837.
Jóźwiak J, Kasperczyk S, Tomasik T, et al. Design and rationale of a nationwide screening analysis from the LIPIDOGRAM2015 and LIPIDOGEN2015 studies. Arch Med Sci. 2020. https://doi.org/10.5114/aoms.2020.96052.
Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Rydén L, Grant PJ, Anker SD, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013;34(39):3035–87. https://doi.org/10.1093/EURHEARTJ/EHT108.
Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. Diabet Med. 1999;16(5):442–3. https://doi.org/10.1046/j.1464-5491.1999.00059.x.
De G, Ambrosioni E, Borch-Johnsen K, et al. Executive summary European guidelines on cardiovascular disease prevention in clinical practice Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Atherosclerosis. 2004;173:381–91. https://doi.org/10.1016/S0021-9150(03)00419-2.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. https://doi.org/10.1001/JAMA.289.19.2560.
Afzal S, Tybjærg-Hansen A, Jensen GB, Nordestgaard BG. Change in body mass index associated with lowest mortality in Denmark, 1976–2013. JAMA. 2016;315(18):1989–96. https://doi.org/10.1001/jama.2016.4666.
Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–78. https://doi.org/10.1016/S0140-6736(06)69251-9.
Niedziela J, Hudzik B, Niedziela N, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol. 2014;29(11):801–12. https://doi.org/10.1007/S10654-014-9961-9.
Gravina G, Ferrari F, Nebbiai G. The obesity paradox and diabetes. Eat Weight Disord. 2021;26(4):1057–68. https://doi.org/10.1007/S40519-020-01015-1.
Gurevitz C, Assali A, Mohsan J, et al. The obesity paradox in patients with acute coronary syndromes over 2 decades—the ACSIS registry 2000–2018. Int J Cardiol. 2023;380:48–55. https://doi.org/10.1016/j.ijcard.2023.03.038.
Khalangot M, Tronko M, Kravchenko V, Kulchinska J, Hu G. Body mass index and the risk of total and cardiovascular mortality among patients with type 2 diabetes: a large prospective study in Ukraine. Heart. 2009;95(6):454. https://doi.org/10.1136/hrt.2008.150524.
Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61(2):151–6. https://doi.org/10.1016/J.PCAD.2018.05.005.
Lee DH, Giovannucci EL. The obesity paradox in cancer: epidemiologic insights and perspectives. Curr Nutr Rep. 2019;8(3):175–81. https://doi.org/10.1007/S13668-019-00280-6.
Shaw GB, Bosomworth NJ, Fcfp C. The downside of weight loss: realistic intervention in body-weight trajectory. Can Fam Physician. 2012;58(5):517.
Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. https://doi.org/10.1016/S0140-6736(09)60318-4.
Marcks N, Aimo A, Januzzi JL, et al. Re-appraisal of the obesity paradox in heart failure: a meta-analysis of individual data. Clin Res Cardiol. 2021;110(8):1280–91. https://doi.org/10.1007/S00392-021-01822-1.
Ali S, Garcia JM. Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options—a mini-review. Gerontology. 2014;60(4):294–305. https://doi.org/10.1159/000356760.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726. https://doi.org/10.1093/EURHEARTJ/EHAB368.
O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–50. https://doi.org/10.1001/JAMA.2009.454.
Taylor RS, Walker S, Smart NA, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: individual participant meta-analysis. J Am Coll Cardiol. 2019;73(12):1430–43. https://doi.org/10.1016/J.JACC.2018.12.072.
Prausmüller S, Heitzinger G, Pavo N, et al. Malnutrition outweighs the effect of the obesity paradox. J Cachexia Sarcopenia Muscle. 2022;13(3):1477–86. https://doi.org/10.1002/jcsm.12980.
Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev. 2009;22(1):93–108. https://doi.org/10.1017/S0954422409990035.
Overvad TF, Rasmussen LH, Skjøth F, Overvad K, Lip GYH, Larsen TB. Body mass index and adverse events in patients with incident atrial fibrillation. Am J Med. 2013. https://doi.org/10.1016/J.AMJMED.2012.11.024.
Springer J, Springer JI, Anker SD. Muscle wasting and sarcopenia in heart failure and beyond: update 2017. ESC Heart Fail. 2017;4(4):492–8. https://doi.org/10.1002/EHF2.12237.
Emami A, Saitoh M, Valentova M, et al. Comparison of sarcopenia and cachexia in men with chronic heart failure: results from the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF). Eur J Heart Fail. 2018;20(11):1580–7. https://doi.org/10.1002/EJHF.1304.
Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr Obes Rep. 2017;6(2):187. https://doi.org/10.1007/S13679-017-0262-Y.
Wadden TA. The look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring). 2006;14(5):737. https://doi.org/10.1038/OBY.2006.84.
Sørensen TIA, Rissanen A, Korkeila M, Kaprio J. Intention to lose weight, weight changes, and 18-y mortality in overweight individuals without co-morbidities. PLoS Med. 2005;2(6):0510–20. https://doi.org/10.1371/JOURNAL.PMED.0020171.
Wilding JPH, Batterham RL, Davies M, et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022;24(8):1553–64. https://doi.org/10.1111/DOM.14725.
Huang S, Shi K, Ren Y, et al. Association of magnitude of weight loss and weight variability with mortality and major cardiovascular events among individuals with type 2 diabetes mellitus: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21(1):78. https://doi.org/10.1186/s12933-022-01503-x.
Orsi E, Solini A, Penno G, et al. Body mass index versus surrogate measures of central adiposity as independent predictors of mortality in type 2 diabetes. Cardiovasc Diabetol. 2022;21(1):266. https://doi.org/10.1186/s12933-022-01706-2.
Loeb LA, Ernster VL, Warner KE, Abbotts J, Laszlo J. Smoking and lung cancer: an overview. Cancer Res. 1984;44(12 Pt 1):5940–58.
Cornfield J, Haenszel W, Hammond EC, Lilienfeld AM, Shimkin MB, Wynder EL. Smoking and lung cancer: recent evidence and a discussion of some questions. Int J Epidemiol. 2009;38(5):1175–91. https://doi.org/10.1093/IJE/DYP289.
Dare S, Mackay DF, Pell JP. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE. 2015. https://doi.org/10.1371/JOURNAL.PONE.0123579.
Watanabe T, Tsujino I, Konno S, et al. Association between smoking status and obesity in a nationwide survey of Japanese adults. PLoS ONE. 2016. https://doi.org/10.1371/JOURNAL.PONE.0148926.
Borrelli B, Mermelstein R. The role of weight concern and self-efficacy in smoking cessation and weight gain among smokers in a clinic-based cessation program. Addict Behav. 1998;23(5):609–22. https://doi.org/10.1016/S0306-4603(98)00014-8.
Veronese N, Li Y, Manson JE, Willett WC, Fontana L, Hu FB. Combined associations of body weight and lifestyle factors with all cause and cause specific mortality in men and women: prospective cohort study. BMJ. 2016. https://doi.org/10.1136/BMJ.I5855.
Sperrin M, Candlish J, Badrick E, Renehan A, Buchan I. Collider bias is only a partial explanation for the obesity paradox. Epidemiology. 2016;27(4):525. https://doi.org/10.1097/EDE.0000000000000493.
Banack HR, Stokes A. The ‘obesity paradox’ may not be a paradox at all. Int J Obes. 2017;41(8):1162–3. https://doi.org/10.1038/ijo.2017.99.
Schneider EB. Collider bias in economic history research. Explor Econ Hist. 2020;78:101356. https://doi.org/10.1016/j.eeh.2020.101356.
Ramsden CE, Zamora D, Majchrzak-Hong S, et al. Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968–73). BMJ. 2016;353:i1246. https://doi.org/10.1136/bmj.i1246.
Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559. https://doi.org/10.1056/NEJMoa0802743
Pavlov M, Nikolic-Heitzler V. Obesity paradox in acute myocardial infarction: is plasminogen activator inhibitor 1 the culprit? Med Hypotheses. 2023;176:111096. https://doi.org/10.1016/j.mehy.2023.111096.
Acknowledgements
Not applicable.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Polish Lipid Association (PoLA) and the College of Family Physician in Poland (CFPIP) provided non-material support by endorsing the project Polish Lipid Association College of Family Physician in Poland. The present study was funded by an unrestricted educational grant from Valeant (Warsaw, Poland). Valeant had no role in the study design, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Consortia
Contributions
JJ, MB, TO, DN and KO contributed to the conception and design of the work. JJ, MB, AW, TT, MGi, MM, BŁR and KJ contributed to the acquisition and interpretation of data. TO, JJ, MB, DN and KO drafted the manuscript. TO and MGi contributed to the analysis and interpretation of the data, and GL, DM, PT, NS, and MGo critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work, ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Research involving human subjects complied with all relevant national regulations and institutional policies, was in accordance with the Helsinki Declaration (as revised in 2013), and was approved by the Bioethical Committee of the Chamber of Physicians (No.K.B.Cz.-0018/ 2015).
Consent for publication
Not applicable.
Competing interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J.J. and M.B. have received an unrestricted educational grant from Valeant and have served as consultants or speakers for Valeant. P.T. owns four shares in AstraZeneca PLC and has received honoraria and/or travel reimbursement for events sponsored by AKCEA, Amgen, AMRYT, Link Medical, Mylan, Napp, and Sanofi. All other authors declare no conflicts of interest concerning the results of this analysis. All authors revised the article critically for important intellectual content. All authors gave final approval of the work, have participated sufficiently in the work, and take public responsibility for appropriate portions of the content.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Clinical characteristics of patients by sex; clinical characteristics of patients by weight loss experienced, mortality hazard ratio versus BMI in sex and comorbidity subgroups as well as patients without comorbidities..
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Osadnik, T., Nowak, D., Osadnik, K. et al. Association of body mass index and long-term mortality in patients from nationwide LIPIDOGRAM 2004–2015 cohort studies: no obesity paradox?. Cardiovasc Diabetol 22, 323 (2023). https://doi.org/10.1186/s12933-023-02059-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-02059-0