Abstract
Rationale
Lung recruitment and continuous distending pressure (CDP) titration are critical for assuring the efficacy of high-frequency ventilation (HFOV) in preterm infants. The limitation of oxygenation (peripheral oxygen saturation, SpO2) in optimizing CDP calls for evaluating other non-invasive bedside measurements. Respiratory reactance (Xrs) at 10 Hz measured by oscillometry reflects lung volume recruitment and tissue strain. In particular, lung volume recruitment and decreased tissue strain result in increased Xrs values.
Objectives
In extremely preterm infants treated with HFOV as first intention, we aimed to measure the relationship between CDP and Xrs during SpO2-driven CDP optimization.
Methods
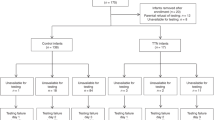
In this prospective observational study, extremely preterm infants born before 28 weeks of gestation undergoing SpO2-guided lung recruitment maneuvers were included in the study. SpO2 and Xrs were recorded at each CDP step. The optimal CDP identified by oxygenation (CDPOpt_SpO2) was compared to the CDP providing maximal Xrs on the deflation limb of the recruitment maneuver (CDPXrs).
Results
We studied 40 infants (gestational age at birth = 22+ 6-27+ 5 wk; postnatal age = 1–23 days). Measurements were well tolerated and provided reliable results in 96% of cases. On average, Xrs decreased during the inflation limb and increased during the deflation limb. Xrs changes were heterogeneous among the infants for the amount of decrease with increasing CDP, the decrease at the lowest CDP of the deflation limb, and the hysteresis of the Xrs vs. CDP curve. In all but five infants, the hysteresis of the Xrs vs. CDP curve suggested effective lung recruitment. CDPOpt_SpO2 and CDPXrs were highly correlated (ρ = 0.71, p < 0.001) and not statistically different (median difference [range] = -1 [-3; 9] cmH2O). However, CDPXrs were equal to CDPOpt_SpO2 in only 6 infants, greater than CDPOpt_SpO2 in 10, and lower in 24 infants.
Conclusions
The Xrs changes described provide complementary information to oxygenation. Further investigation is warranted to refine recruitment maneuvers and CPD settings in preterm infants.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Extremely preterm infants often need mechanical ventilation in their first days after birth [1]. Due to the preterm infant’s immature lungs, lung protective ventilation strategies are used in an attempt to limit ventilator-induced lung injury. A lung protective ventilation strategy minimizes alveolar overdistention during inspiration, reverses atelectasis, and stabilizes open lung units [2].
High-frequency oscillatory ventilation (HFOV) is an established ventilation mode in preterm infants associated with minimal tidal volumes and pressure changes at the alveoli [3]. Its efficacy critically depends on optimizing and stabilizing lung volume [4]. To this aim, periodically repeated lung recruitment maneuvers and continuous distending pressure (CDP) optimization are advocated. The strategy of lung recruitment, however, is not well defined. In clinical practice, oxygen response is widely used as a surrogate for lung volume [5]. In an animal study, recruitment maneuvers, consisting of stepwise CDP increases and decreases, were shown beneficial for oxygenation [6]. This strategy was adopted in a seminal study on HFOV initiation in preterm infants with RDS [7]. These maneuvers have a low risk of lung hyperinflation, air-leak syndrome, critically worsening cardiac function, and cerebral adverse events (e.g., intraventricular hemorrhage) in preterm infants [8, 9]. However, the heterogeneity of infants’ responses to recruitment maneuvers is well documented. Therefore, methods for evaluating the respiratory system response to pressure changes and identifying the optimal CDP are required [7]. Currently, recruitment maneuvers and optimal CDP identification are driven by oxygenation determined by peripheral oxygen saturation (SpO2) corrected by the fraction of inspired oxygen (FiO2) [3]. SpO2 is easily available at the bedside and correlates with lung volumes [10, 11]. However, it is only an indirect marker of lung volume recruitment and is affected by various factors, including hemodynamic changes and pulmonary hypertension [12]. Moreover, difficulties in determining SpO2 target ranges and FiO2 thresholds, together with the variable infants’ capabilities of increasing their spontaneous breathing activity to maintain SpO2 in the target range, further complicate using SpO2/FiO2 for CDP titration. Also, a previous study showed that the efficacy of the recruitment maneuver evaluated on changes in end-expiratory lung volume (monitored by respiratory inductive plethysmography) rather than SpO2 correlated better with improvements in clinical condition after 1 h [13].
Oscillometry assesses respiratory reactance (Xrs) by measuring pressure and flow at the airways opening while a small-amplitude, high-frequency pressure stimulus is superimposed to ventilation. Xrs expresses the inertial and elastic properties of the respiratory system, reflecting lung volume recruitment and tissue strain. In particular, Xrs decreases as a result of lung volume derecruitment and/or lung (over)distension [14], similar to lung compliance. Oscillometry has recently become available at the bedside for newborns and has been safely applied to preterm infants during mechanical ventilation [15,16,17].
In preterm infants treated with HFOV as first intention, we aimed to measure the relationship between CDP, SpO2/FiO2, and Xrs during SpO2-driven CDP optimization.
Methods
This was a prospective observational study and sub-trial of a randomized controlled trial (ClinicalTrials.gov ID: NCT04289324) on recruitment maneuver during HFOV comparing infants receiving recruitment maneuvers either at 12 h intervals and when clinically indicated (intervention) or only when clinically indicated (control) [18]. The study was conducted at the neonatal intensive care unit of the Medical University of Vienna, Vienna, Austria, between March 2020 and June 2022. The study was approved by the local ethics committee (EK 1161/2019).
Study population
Preterm infants born before 28 weeks of gestation without any congenital anomalies of the heart and/or the lungs (as reported in ultrasound and/or fetal magnetic resonance imaging) were eligible in their first four weeks of postnatal age. Infants on HFOV were enrolled upon the availability of the study team to perform measurements during a single lung recruitment maneuver performed during the randomized controlled trial mentioned above. Written informed consent from parents or legal guardians was obtained before performing the measurements.
Study protocol
SpO2, transcutaneous CO2 (TcCO2), heart rate, and invasive blood pressure were continuously monitored as per local standard of care. Starting at the CDP in use (initial CDP, CDPi), CDP was increased (inflation limb) approximatively every 5 min (allowing intervals of 2–15 min upon the decision of the caregiving team) by 2 cmH2O (allowing for steps of 1 cmH2O when CDP was greater than 20 cmH2O). The fraction of inspired oxygen (FiO2) was reduced stepwise, keeping SpO2 within the predefined target range (88–96% or 90–96% in the presence of pulmonary hypertension requiring medication). The inflation limb ended when SpO2 no longer improved or FiO2 was ≤ 0.25. From the maximal CDP (CDPmax), CDP was gradually decreased (deflation limb) approximately every 5 min (allowing intervals of 2–15 min upon the decision of the caregiving team) by 2 cmH2O (allowing for steps of 1 cmH2O when CDP was lower than the initial CDP) until either a sustained SpO2 drop of at least 5% or a SpO2 value below 88% indicated the reaching of the closing CDP (minimal CDP of the recruitment maneuver, CDPmin). The minimum allowed CDP was 5 cmH2O. The HFOV frequency was kept at the clinically set values. The pressure amplitude was adjusted to target TcCO2 between 40 and 60 mmHg (SenTec Digital Monitor, Therwil, Switzerland, with a probe temperature of 41 °C). CDPOpt_SpO2 was defined as CDPmin +1 or 2 cmH2O [7]. Before setting CDPOpt_SpO2 on the ventilator (final CPD, CDPf) CDPmax was set for approximately 5 min (re-recruitment after the deflation limb) to promote lung volume re-recruitment after the application of CDPmin. Recruitment maneuvers were advised after the following situations: change of position (from prone to supine or vice versa), any manipulation with FiO2 increase of 0.1 or SpO2 decrease > 10% for > 5 min (e.g., suctioning, endotracheal tube disconnection), surfactant application, and suspected or confirmed atelectasis (e.g., diagnosed on chest X-ray). Infants were not disconnected from the ventilator nor underwent suctioning during the maneuvers, as these would have modified the lung volume history and the maneuver efficacy. The infant’s head and body position were not changed during the recruitment maneuver.
Measurements
SpO2 (Covidien-Nellcor, Boulder, CO) was monitored continuously and recorded at the end of each CDP step. Conversely, Xrs was measured after 3 min of stabilization at each CDP step (or at the end of the CDP step for shorter steps). The ventilator computed Xrs values (Fabian FOT 150,204 V5.0, Vyaire srl, US). When requested by the clinician, the ventilator reduced HFOV amplitude for ~ 3 s and set the oscillation frequency to 10 Hz, keeping the same CDP. At each time point, the ventilator provided a single measure as the mean Xrs values over the measurement time if the test passed a quality check for excluding measurements at risk of being affected by artifacts. No specific calibration procedure was required for performing the measurements. Clinicians were blinded to Xrs data. In two infants, we repeated oscillometry also at 6 min after CDP change to evaluate the stability of the Xrs values with time.
Data analysis
The oxygen saturation index (OSI) was calculated as CDP × FiO2 × 100 ÷ SpO2. Xrs values at each CDP were exported from the ventilator and corrected for the impedance of the endotracheal tube (considering the diameter and the actual length of the tube) [19]. Missing Xrs data were estimated by linear interpolating Xrs values at the previous and following CDP steps. The average Xrs and SpO2/FiO2 vs. CDP relationship was computed by normalizing CDP between 0% (CDPmin) and 100% (CDPmax) and linearly interpolating the measured data to obtain values each 10% or 20%. CDPXrs was defined as the one providing maximal Xrs on the deflation limb of the recruitment. Xrs and SpO2/FiO2 values were averaged at CDPi, CDPmax, CDPmin, CDPOpt_SpO2, and CDPXrs. The difference between CDPXrs and CDPOpt_SpO2 was computed with a resolution of ± 1 cmH2O as CDP steps of the deflation limb were mainly of 2 cmH2O.
To quantify Xrs changes with CDP, we defined the following parameters: (1) ΔXinf_limb as the difference in Xrs at CDPi and CDPmax to evaluate the impact of increasing CDP; (2) ΔXcl as the difference in Xrs at CDPXrs and CDPmin to evaluate the impact of the lowest CDP applied; (3) ΔXrec as the difference in Xrs at CDPXrs during the deflation and the inflation limb. When CDPXrs was lower than CDPi, ΔXrec was computed at CDPi to guarantee that Xrs was compared at the same distending pressure. ΔXrec evaluated the Xrs vs. CDP curve hysteresis associated with lung recruitment. We considered Xrs changes relevant only if higher than 6.3 cmH2O*s/L and 10% of its value. The reproducibility of Xrs measures in preterm infants was 6.3 cmH2O*s/L and was within 10% of its value for Xrs < − 60 cmH2O*s/L [20].
To understand whether the Xrs response to pressure increases during the inflation limb was predictive of post-maneuver overall lung volume recruitment (as assessed by ΔXrec), we evaluated the shape of the Xrs vs. CDP graphs during inflation limb searching for different patterns and performed an exploratory sub-group analysis (see Additional File 1).
Statistical analysis
Friedman Repeated Measures Analysis of Variance on Ranks, followed by Pairwise Multiple Comparison by Tukey Test, as appropriate for data distribution, was used for comparing data at more than two CDPs. Correlations between variables were tested by the Spearman test. Differences were considered statistically significant for p < 0.05.
Results
We studied 40 infants with heterogeneous demographic characteristics (Table 1). The CDP applied, the number of CDP steps, and the duration of CDP intervals varied among SpO2-driven CDP optimization (Table 1). In each infant, monitoring parameters could be maintained in individually predefined target ranges as per local standard of care throughout the recruitment maneuver. A total of 588 Xrs measurements were attempted. Seven infants missed Xrs values at some CDPs for a total of 14 missing Xrs measures (2% of the total measures) because the ventilator reported unreliable conditions to perform the measurements. Eleven infants presented inconsistent Xrs values at some CDP steps for a total of 16 Xrs values (3% of the successful measurements), as they were outliers of the depicted Xrs vs. CDP curve as judged by visual inspection.
Initial Xrs values ranged from − 140 to -27 cmH2O*s/L and correlated with GA (ρ = 0.33, p = 0.04) but not SpO2/FiO2. In general, Xrs significantly changed with CDP from a minimum change of 13 cmH2O*s/L to a maximum change of 88 cmH2O*s/L. Xrs changes were heterogeneous among the infants for the amount of decrease at increasing CDP, the decrease at the lowest CDPs, and the hysteresis of Xrs vs. CDP curve (Fig. 1 right panel).
Median (IQR) SpO2/FiO2 (Upper Panels) and Xrs (Lower Panels) vs. CDP. Left panels: CDP was normalized between 0% (CDPmin= minimal CDP) and 100% (CDPmax= maximal CDP). Parameters are computed for each 20% CDP change by linear interpolating the measured data. The grey and black lines represent the inflation and the deflation limbs, respectively. Right panels: values are averaged at initial CDP (CDPi), maximal CDP (CDPmax), CDP corresponding to maximal Xrs (CDPXrs), minimal CDP (CDPmin), optimal CDP as identified by SpO2 (CDPOpt_O2, grey circle). The figure reports the median [range] of Xrs and SpO2/FiO2 changes at selected CDPs. ΔXinf_limb = the difference in Xrs between CDPi and CDPmax, evaluating the impact of increasing CDP. The difference between CDPmax and CDPi was 10 [4–14] cmH2O and the Xrs change per cmH2O resulted: ΔXinf_limb/( CDPmax – CDPi ) = 1.5 [-7.3–14.1] s/L. ΔXcl = the difference in Xrs between CDPXrs and CDPmin to evaluate the impact of the lowest CDP applied. The difference between CDPXrs and CDPmin was 1 [0–10] cmH2O and the Xrs change per cmH2O resulted: ΔXcl/( CDPXrs - CDPmin) = 0.2 [0–16.4] s/L. ΔXrec = the difference in Xrs between CDPXrs during the inflation and the deflation limb to evaluate the hysteresis of the curve. It is reported as an absolute difference (cmH2O*s/L) and as a percentage of the value on the inflation limb. In 20 infants CDPXrs was lower than the CDPi, ΔXrec was computed at CDPi
Xrs vs. CPD curve: Xrs changes during the inflation limb and curve hysteresis
On average, Xrs decreased during the inflation limb and increased during the deflation limb (Fig. 1, left panel). However, in 6 infants, Xrs mainly increased with increasing CDP (ΔXinf_limb< 0). In all but 5 infants (87.5%), ΔXrec was higher than the reproducibility of the Xrs measure. ΔXrec was not dependent on the indication for performing the recruitment maneuver. Also, ΔXrec was not entirely predictable from Xrs changes during the inflation limb. In fact, ΔXrec weakly correlated to ΔXinf_limb (ρ = 0.33, p = 0.04), and it was not possible to predict ΔXrec higher than the reproducibility of Xrs measures from the pattern of Xrs vs. CDP graphs of the inflation limb. All the graphs showing Xrs increases or Xrs stability with increasing CDP for at least two CDP steps resulted in ΔXrec higher than the Xrs reproducibility. However, graphs showing a continuous decrease in Xrs resulted in ΔXrec both higher or lower than the Xrs reproducibility (Additional File 1: Figure S1). Repeated measures at the same CDP step showed Xrs values that were still increasing 3 min after the CDP increment in one infant at a few steps of the inflation limb (Fig. 2).
Xrs vs. CPD curve: last steps of the deflation limb and re-recruitment after the maneuver
In 22 infants (55%), Xrs decreased during the last steps of the deflation limb (ΔXcl > 0), and in 15 (37.5%), the decrease is higher than the reproducibility of the Xrs measure (ΔXcl > 6.3 cmH2O*s/L and 10%).
There were no differences between Xrs and SpO2/FiO2 values at the CDPOpt_SpO2 of the deflation limb and after the re-recruitment step (at CDPf) (median difference of -1.2 cmH2O*s/L and − 0.04, respectively) (Table 2). The re-recruitment allowed Xrs to recover at least its value of the deflation limb at the corresponding CDP (within the reproducibility of the Xrs measure) in 34 infants (85%). In six of these infants, Xrs was even higher than the one during the deflation limb (median [range] of the change, 10.2 [7.0;15.9] cmH2O*s/L). In the remaining six infants, Xrs after the second fast recruitment was lower than its value of the deflation limb at the corresponding CDP (median [range] of the change − 10.7 [-24.6;- 10.3] cmH2O*s/L).
Xrs and oxygenation changes
On average, and differently from Xrs, SpO2/FiO2 improved during the inflation limb and worsened at the deflation limb’s end. Changes in SpO2/FiO2 during the maneuver weakly correlated with Xrs (ρ = 0.28; p < 0.001).
CDPOpt_SpO2 and CDPXrs were highly correlated (ρ = 0.71, p < 0.001) and not statistically different (median difference [range] = -1 [-3; 8]) (Fig. 3). CDPXrs were equal to CDPOpt_SpO2 in 6 infants (15%), greater than CDPOpt_SpO2 in 10 (25%), and lower in 24 infants (60%). The difference between CDPXrs and CDPOpt_SpO2 was greater than 2 cmH2O*s/L in only four subjects (Fig. 3, Additional file 1: Figure S2). However, the difference can be underestimated as CDPXrs matched CDPmin in 18 infants, where we did not identify an Xrs decrease. Xrs was higher at CDPXrs than at CDPOpt_SpO2, while the other respiratory parameters were not different on average (Table 2).
The overall effect of the procedure
CDPf was not significantly different from CDPi (Table 2). In contrast, Xrs and SpO2/FiO2 were higher and OSI lower after the maneuver, indicating successful lung recruitment. Changes in SpO2/FiO2 pre-post maneuver were poorly correlated with both CDP and Xrs changes (0.34, p = 0.03 and 0.33, p = 0.04, respectively).
Discussion
In this study, we reported the changes in Xrs during recruitment maneuvers in a heterogeneous population of extremely preterm infants receiving HFOV. Our main findings were: (1) measuring Xrs at the bedside in patients receiving HFOV was feasible and provided a high percentage of good quality data; (2) Xrs changed significantly during the recruitment maneuvers. Its variable baseline values and variable changes with CDP indicated a heterogeneity of lung mechanical condition in ventilated preterm newborns; (3) the majority of the infants (87.5%) presented a significant hysteresis of the Xrs vs. CDP curve, suggesting that exposing the lung to the high CDP of the maneuver resulted in lung volume recruitment. The hysteresis of the Xrs vs. CDP curve was not entirely predictable by the Xrs changes during the inflation limb. Also, 55% of infants presented an Xrs decrease at the end of the deflation limb, indicating lung volume derecruitment occurring after 3 min at the lowest CPD applied. Re-recruitment after the maneuver restored Xrs values of the deflation limb at the corresponding CDP in 87.5% of maneuvers; (4) on average, changes in Xrs correlated with changes in SpO2/FiO2. However, Xrs mainly improved on the deflation limb, whereas SpO2/FiO2 improved primarily on the inflation limb. Even if CDPXrs and CDPOpt_SpO2 were not statistically different overall, they differed most of the time, indicating that CDPOpt_SpO2 did not always attain optimal lung mechanics.
This is the first study addressing Xrs changes with CDP in a large population of preterm infants receiving HFOV. Only a few previous studies [9, 15, 21] reported changes in Xrs with distending pressure in intubated preterm infants, and only one of them was performed during HFOV [9]. In our study, only 2% of measurements were unsuccessful, and only 3% of the data points were outliers, supporting the feasibility of oscillometry measurements in clinical settings. The wide ranges of the parameters describing Xrs vs. CDP curve (ΔXinf_limb, ΔXcl, and ΔXrec) highlight the heterogeneity of lung condition, distensibility, recruitability, and tendency to derecruitment in our population.
Xrs vs. CPD curve: Xrs changes during the inflation limb and curve hysteresis
Figure 1 shows a marked decrease in Xrs with increasing CDP (ΔXinf_limb >0). Xrs changes during the inflation limb are determined by the balance between lung volume recruitment and increased lung tissue distention. Lung volume recruitment increases Xrs, whereas increased lung tissue distension (i.e., reduced tissue compliance) lowers Xrs [22]. Steeper decreases may be associated with greater tissue stress [16]. However, ΔXinf_limb was small or even negative in some infants, indicating that Xrs changes were mainly driven by lung volume recruitment. These data show that reaching the opening CDP according to SpO2 exposes the lung to very variable stress between infants.
ΔXrec is related to the hysteresis in the Xrs vs. CDP graph and, comparing Xrs at the same CDP during inflation and deflation, provides an indication of the recruited lung, as the contribution to Xrs of tissue distention is the same at the same CDP. 87.5% of infants had ΔXrec higher than the reproducibility of the Xrs measure, which testifies to lung volume recruitment. As 92.5% of these maneuvers were not performed at HFOV initiation, our results suggest that lung volume derecruitment may frequently occur during long periods of mechanical ventilation at constant CDP, and periodical CDP optimizations should be performed to maintain proper lung recruitment [23]. Also, 15 infants showing significant lung volume recruitment were on mechanical ventilation for over 6 days. This suggests that, in some patients, CDP optimizations can be effective also in a post-acute phase. Also, the general improvement of infant conditions after the overall procedure further supports the efficacy of the performed maneuvers.
However, ΔXrec was variable and not predictable from the patterns of Xrs changes with CDP during the inflation limb (see Additional File 1). If and how Xrs changes during the inflation limb can be used to tailor recruitment maneuvers for improving safety and efficacy remains to be addressed. The increasing Xrs with time at fixed CDP (Fig. 2, right panel) suggests the progression of slow lung volume recruitment during some CDP steps of the inflation limb. Future studies should address this topic for understanding the optimal step duration [24]. Repeating oscillometry tests during each CDP step may provide criteria for tailoring the step duration by identifying the stability of Xrs.
Xrs vs. CPD curve: last steps of the deflation limb and re-recruitment after the maneuver
Xrs changes during the deflation limb are determined by the balance between lung volume de-recruitment and decreased lung tissue distention. Lung volume derecruitment lowers Xrs, whereas reduced lung tissue distension increases Xrs [22]. The average behavior shows higher Xrs values at the lowest CDPs, indicating how easily the lung tissue is distended by pressure in preterm infants. However, in surfactant-depleted or collapsible lungs, the low CDPs reached at the end of the deflation limb can promote lung volume derecruitment and result in Xrs reduction with decreasing pressure toward the end of the maneuver (ΔXcl>0). Steeper decreases indicate greater lung periphery instability (i.e., a higher tendency to de-recruit). This characteristic of the Xrs vs. CDP loops was very variable between infants, with Xrs decreasing at the end of the maneuver in 55% of the infants.
We did not find previous studies addressing the efficacy of the second phase of the recruitment maneuver, which consists of reaching the opening CDP (CDPmax) for a few minutes before setting CDPOpt_O2. Lung physiology suggests that this procedure should be performed after reaching CDPmin, to reverse the de-recruitment provoking the SpO2 drop defining the closing CDP. In our population, this procedure restored the Xrs value reached at CDPOPt_O2 of the deflation limb in 87% of maneuvers. In a previous study during conventional ventilation [16], restoring the clinical set positive end-expiratory pressure (PEEP) directly after 5 min at the clinical PEEP – 2cmH2O without reaching the opening pressure resulted in persistent de-recruitment in 32% of infants. This finding underlines the importance of performing this procedure after each recruitment maneuver.
Xrs and oxygenation changes
In our dataset, in accordance with previous studies [25, 26], oxygenation improved during inflation and remained more stable during deflation, whereas Xrs, deteriorated during inflation and improved during deflation. Oxygenation may be less sensitive to overdistension and less accurate in defining the optimal point of ventilation because of the uniformity of SpO2 readings over a wider range of airway pressures during the deflation limb. Similarly to what was reported for other respiratory variables studied during SpO2-driven maneuvers [27, 28], Xrs identified a range of optimal pressures just above CDPmin, in line with the definition of CDPOpt_O2.
The CDP value corresponding to the maximal Xrs may provide the optimal mechanical balance between maximizing lung volume recruitment and reducing tissue overdistention. This CDP (CDPXrs) correlates with CDPOpt_O2 but is not identical in 85% of the maneuvers, with a tendency to be lower, as previously noticed also during conventional ventilation [15]. Applying CDPXrs instead of CDPOpt_O2 would have led globally to higher Xrs, suggesting that Xrs may identify more protective ventilation settings. Future studies must clarify if this lower CDP setting can warrant similar gas exchange and stable lung mechanics in time.
We found a difference between CDPXrs and CDPOpt_SpO2 greater than 2 cmH2O*s/L in only four subjects (Fig. 3 and Additional File 1: Figure S1). Infants with CDPXrs higher than CDPOpt_O2 would likely have to deal with insufficient pressure to optimize lung mechanics and recruitment, leading to possible increased work of breathing and/or lung tissue stress. A higher CDPXrs than CDPOpt_O2 can be due to different factors. First, Xrs was measured 3 min after the CDP change, while SpO2 after a longer period. Xrs may still be decreasing after 3 min at the lowest CDPs as slow lung derecruitment may occur [29]. Second, Xrs may not identify increasing inhomogeneity due to a small volume loss until significant lung derecruitment occurs [30].
Determining CDPXrs can improve CDP tailoring as it increases the awareness of the lung mechanical conditions and, therefore, the risk of tissue stress and lung derecruitment.
Limitations
This study has some limitations. Xrs was measured 3 min after the CDP change as by default ventilator setting while SpO2 was recorded at the end of each CDP step (in median 6 min after CDP change) when infant conditions were judged stable. Therefore, SpO2 and Xrs values are compared at different time points. Also, CDP steps of 2 cmH2O during the deflation limb limited our resolution in comparing CPDopt_SpO2 and CDPXrs. Finally, performing oscillometry required a short interruption of HFOV. However, as the procedure lasted only 3–5 s and the CDP was not changed, it should not have significantly affected lung mechanics and gas exchange.
In conclusion, we described Xrs changes during SpO2-guided recruitment maneuvers in extremely preterm infants. The Xrs vs. CDP loop provides information on the lung mechanical status, which is complementary to oxygenation and may allow for improving the individualization of ventilatory settings at the bedside during HFOV. Further investigation is warranted to evaluate the impact of tailoring recruitment maneuvers and CDP according to Xrs measures on short- and long-term respiratory outcomes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- CDP:
-
continuous distending pressure
- CDPf :
-
final CDP at the end of the procedure, after re-recruiment after the deflation limb
- CDPi :
-
initial CDP of the maneuver
- CDPmax :
-
maximal CDP of the maneuver
- CDPmin :
-
minimal CDP of the maneuver
- CDPOpt_SpO2 :
-
optimal CDP as identified by peripheral oxygen saturation
- CDPXrs :
-
the CDP providing maximal Xrs on the deflation limb of the recruitment maneuver
- FiO2 :
-
fraction of inspired oxygen
- GA:
-
gestational age
- HFOV:
-
high-frequency oscillatory ventilation
- OSI:
-
oxygen saturation index
- SpO2 :
-
peripheral oxygen saturation
- TcCO2 :
-
transcutaneous CO2
- Xrs:
-
respiratory reactance
- ΔXinf_limb :
-
change in Xrs at the end of the inflation limb, computed as the difference in Xrs between CDPmax and CDPi
- ΔXcl :
-
decrease in Xrs at the closing CDP (CDPmin) from its maximal value (at CDPXrs)
- ΔXrec :
-
change in Xrs associated with possible lung volume recruitment that occurred during the maneuver, computed as the difference in Xrs at CDPXrs during the deflation and the inflation limbs
References
Donaldsson S, Drevhammar T, Li Y, Bartocci M, Rettedal SI, Lundberg F, et al. Comparison of respiratory support after delivery in infants born before 28 weeks’ gestational age: the CORSAD Randomized Clinical Trial. JAMA Pediatr. 2021;175(9):911–8.
Kalikkot Thekkeveedu R, El-Saie A, Prakash V, Katakam L, Shivanna B. Ventilation-Induced Lung Injury (VILI) in neonates: evidence-based concepts and lung-protective strategies. J Clin Med. 2022;11(3).
Ackermann BW, Klotz D, Hentschel R, Thome UH, van Kaam AH. High-frequency ventilation in preterm infants and neonates. Pediatr Res. 2023;93(7):1810–8.
van Kaam AH, Rimensberger PC. Lung-protective ventilation strategies in neonatology: what do we know–what do we need to know? Crit Care Med. 2007;35(3):925–31.
Froese AB, Kinsella JP. High-frequency oscillatory ventilation: lessons from the neonatal/pediatric experience. Crit Care Med. 2005;33(3 Suppl).
Pellicano A, Tingay DG, Mills JF, Fasulakis S, Morley CJ, Dargaville PA. Comparison of four methods of lung volume recruitment during high frequency oscillatory ventilation. Intensive Care Med. 2009;35(11):1990–8.
De Jaegere A, Van Veenendaal MB, Michiels A, Van Kaam AH. Lung recruitment using oxygenation during open lung high-frequency ventilation in preterm infants. Am J Respir Crit Care Med. 2006;174(6):639–45.
De Jaegere AP, Deurloo EE, van Rijn RR, Offringa M, van Kaam AH. Individualized lung recruitment during high-frequency ventilation in preterm infants is not associated with lung hyperinflation and air leaks. Eur J Pediatr. 2016;175(8):1085–90.
Zannin E, Doni D, Ventura ML, Fedeli T, Rigotti C, Dellacá RL, et al. Relationship between Mean airways pressure, lung mechanics, and right ventricular output during high-frequency Oscillatory Ventilation in infants. J Pediatr. 2017;180:110–5.
Van Genderingen HR, Van Vught AJ, Jansen JRC. Regional lung volume during high-frequency oscillatory ventilation by electrical impedance tomography. Crit Care Med. 2004;32(3):787–94.
Suzuki H, Papazoglou K, Bryan AC. Relationship between PaO2 and lung volume during high frequency oscillatory ventilation. Acta Paediatr Jpn Overseas Ed. 1992;34(5):494–500.
Dantzker DR, Lynch JP, Weg JG. Depression of cardiac output is a mechanism of shunt reduction in the therapy of acute Respiratory Failure. Chest. 1980;77(5):636–42.
De Jager P, Burgerhof JGM, Koopman AA, Markhorst DG, Kneyber MCJ. Lung volume optimization maneuver responses in pediatric high-frequency oscillatory ventilation. Am J Respir Crit Care Med. 2019;199(8):1034–6.
King GG, Bates J, Berger KI, Calverley P, de Melo PL, Dellacà RL, et al. Technical standards for respiratory oscillometry. Eur Respir J. 2020;55(2):1900753.
Wallström L, Veneroni C, Zannin E, Dellacà RL, Sindelar R. Forced oscillation technique for optimising PEEP in ventilated extremely preterm infants. Eur Respir J. 2020;55(5):1–4.
Veneroni C, Wallström L, Sindelar R, Dellacà RL. Oscillatory respiratory mechanics on the first day of life improves prediction of respiratory outcomes in extremely preterm newborns. Pediatr Res. 2019;85(3):312–7.
Vendettuoli V, Veneroni C, Zannin E, Mercadante D, Matassa P, Pedotti A, et al. Positional effects on lung mechanics of ventilated preterm infants with acute and chronic lung Disease. Pediatr Pulmonol. 2014;50(8):798–804.
Werther T, Kueng E, Aichhorn L, Pummer L, Goeral K, Berger A, et al. Regular lung recruitment maneuvers during high-frequency oscillatory ventilation in extremely preterm infants: a randomized controlled trial. BMC Pediatr. 2022;22(1):1–9.
Pigmans RRWP, van Leuteren RW, Scholten AWJ, Veneroni C, van Kaam AH, Hutten GJ et al. Influence of neonatal endotracheal tube dimensions on oscillometry-acquired reactance: a bench study. Physiol Meas. 2023;44(1).
Rigotti C, Zannin E, Veneroni C, Ventura ML, Dellacà RL. Oscillatory mechanics response to inhaled bronchodilators in very preterm infants: a retrospective study. J Pediatr. 2022;1–7.
Dellacà RL, Veneroni C, Vendettuoli V, Zannin E, Matassa PG, Pedotti A, et al. Relationship between respiratory impedance and positive end-expiratory pressure in mechanically ventilated neonates. Intensive Care Med. 2013;39(3):511–9.
Kaczka DW, Dellacà RL. Oscillation mechanics of the respiratory system: applications to lung Disease. Crit Rev Biomed Eng. 2011;39(4):337–59.
Dargaville Pa, Tingay DG. Lung protective ventilation in extremely preterm infants. J Paediatr Child Health. 2012;48(9):740–6.
Tingay DG, Kiraly N, Mills JF, Dargaville PA. Time to Lung volume Stability after pressure change during high-frequency Oscillatory Ventilation. Crit Care Explor. 2021;3(6):e0432.
Miedema M, De Jongh FH, Frerichs I, Van Veenendaal MB, Van Kaam AH. Changes in lung volume and ventilation during lung recruitment in high-frequency ventilated preterm infants with respiratory distress syndrome. J Pediatr. 2011;159(2).
Miedema M, McCall KE, Perkins EJ, Oakley RB, Pereira-Fantini PM, Rajapaksa AE et al. Lung recruitment strategies during high frequency oscillatory ventilation in preterm lambs. Front Pediatr. 2019;6(436).
Miedema M, De Jongh FH, Frerichs I, Van Veenendaal MB, Van Kaam AH. The effect of airway pressure and oscillation amplitude on ventilation in pre-term infants. Eur Respir J. 2012;40(2):479–84.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA. Indicators of optimal lung volume during high-frequency oscillatory ventilation in infants. Crit Care Med. 2013;41(1):237–44.
Bates JHT, Irvin CG. Time dependence of recruitment and derecruitment in the lung: a theoretical model. J Appl Physiol. 2002;93(2):705–13.
Veneroni C, Van Muylem A, Malinovschi A, Michils A, Dellacà RL. Closing volume detection by single-breath gas washout and forced oscillation technique. J Appl Physiol. 2021;130(4):903–13.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Acknowledgements
Not applicable.
Funding
This study was partially funded by the Medical Scientific Fund of the Mayor of the City of Vienna (Project number 19103). This study was partially funded by the National Plan for NRRP Complementary Investments (PNC, established with the decree-law 6 May 2021, n. 59, converted by law n. 101 of 2021) in the call for the funding of research initiatives for technologies and innovative trajectories in the health and care sectors (Directorial Decree n. 931 of 06-06-2022) - project n. PNC0000003 - AdvaNced Technologies for Human-centrEd Medicine (project acronym: ANTHEM). This work reflects only the authors’ views and opinions, neither the Ministry for University and Research nor the European Commission can be considered responsible for them.
Author information
Authors and Affiliations
Contributions
CV: analysed the data, interpreted the data, and drafted the manuscript. BB: analysed the data and critically revised the manuscript. EK managed data acquisition and critically revised the manuscript. AB supervised data acquisition and critically revised the manuscript. RLD: interpreted the data and critically revised the manuscript. TW: conceived and designed the study, managed data acquisition, interpreted the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Medical University of Vienna (EK 1161/2019). Written informed consent from parents or legal guardians was obtained prior to the start of the measurements.
Consent for publication
Not applicable.
Competing interests
Politecnico di Milano University, Institution of CV, BB, and RLD, received grants from Restech, Philips Healthcare, and Vyaire; RLD reports a patent on the detection of expiratory flow limitation by oscillometry with royalties paid to Philips Respironics and Restech Srl outside the submitted work; a patent on monitoring lung volume recruitment by oscillometry with royalties paid to Vyaire; a patent on early detection of exacerbations by home monitoring of oscillometry with royalties paid to Restech, outside the submitted work; he is co-founder and shareholder of Restech Srl, a spin-off company of the Politecnico di Milano University producing medical devices for lung function testing based on oscillometry, outside the submitted work. TW received speaker honoraria and travel expenses from Vyaire. EK and AB have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12931_2023_2639_MOESM1_ESM.docx
Additional file 1. Description of Xrs vs. CPD curve patterns during the inflation limb and resulting curve hysteresis. Description of the CDP trials of the four infants with the highest difference between CDPOpt_SpO2 and CDPXrs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Veneroni, C., Dellacà, R.L., Küng, E. et al. Oscillometry for personalizing continuous distending pressure maneuvers: an observational study in extremely preterm infants. Respir Res 25, 4 (2024). https://doi.org/10.1186/s12931-023-02639-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-023-02639-4