Abstract
Background
Alpha-1 antitrypsin deficiency (AATD) is a rare disease that is associated with an increased risk of pulmonary emphysema. The European AATD Research Collaboration (EARCO) international registry was founded with the objective of characterising the individuals with AATD and investigating their natural history.
Methods
The EARCO registry is an international, observational and prospective study of individuals with AATD, defined as AAT serum levels < 11 μM and/or proteinase inhibitor genotypes PI*ZZ, PI*SZ and compound heterozygotes or homozygotes of other rare deficient variants. We describe the characteristics of the individuals included from February 2020 to May 2022.
Results
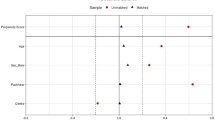
A total of 1044 individuals from 15 countries were analysed. The most frequent genotype was PI*ZZ (60.2%), followed by PI*SZ (29.2%). Among PI*ZZ patients, emphysema was the most frequent lung disease (57.2%) followed by COPD (57.2%) and bronchiectasis (22%). Up to 76.4% had concordant values of FEV1(%) and KCO(%). Those with impairment in FEV1(%) alone had more frequently bronchiectasis and asthma and those with impairment in KCO(%) alone had more frequent emphysema and liver disease. Multivariate analysis showed that advanced age, male sex, exacerbations, increased blood platelets and neutrophils, augmentation and lower AAT serum levels were associated with worse FEV1(%).
Conclusions
EARCO has recruited > 1000 individuals with AATD from 15 countries in its first 2 years. Baseline cross sectional data provide relevant information about the clinical phenotypes of the disease, the patterns of functional impairment and factors associated with poor lung function.
Trial registration www.clinicaltrials.gov (ID: NCT04180319)
Similar content being viewed by others
Introduction
Alpha-1 antitrypsin deficiency (AATD) is a rare disease that is associated with an increased risk of pulmonary emphysema in adults, and liver disease and panniculitis in adults and children [1]. It has been estimated that approximately 1/3500 and 1/6000 individuals of European descent may be affected by severe AATD in its homozygous PI*ZZ form [2] and that around 1/800 patients with chronic obstructive pulmonary disease (COPD) in Europe have severe AATD [3].
Understanding the clinical characteristics and the natural history of a rare disease can be challenging due to the lack of large cohorts. This is even more challenging in the case of AATD because of the important influence of external factors, such as smoking, alcohol consumption or other toxic exposures, on the clinical manifestations in patients with the disease [1, 4]. Traditionally, some European countries have organised national registries that have had different success in collecting prospective follow-up data of patients with AATD [5,6,7]. Some 20 years ago, the Alpha-1 International Registry (AIR) tried to harmonise the collection of prospective data from different European and non-European countries and included more than 4000 patients with severe AATD [8], but less than 400 had long-term follow-up [9]. The standardised collection of follow-up data of patients with AATD from different countries and under different regimens of treatment in a large international registry was an unmet need identified by patients and researchers [10]. Similarly, the European Commission [11] and the European Respiratory Society (ERS) [12] recommended the setup of large international registries to collect structured, prospective data to better understand the natural history of AATD.
The European Alpha-1 antitrypsin Deficiency Research Collaboration (EARCO) international registry is an initiative of the EARCO Clinical Research Collaboration (CRC) of the ERS, with the objective of characterising AATD of different genotypes and investigating their natural history and the impact of different treatments, including augmentation therapy [13, 14]. Although the EARCO registry was created as a European initiative, it has extended beyond European boundaries to become a global registry. In this article we describe the characteristics of individuals with AATD included in the registry during the first 2 years, compare the characteristics of augmented versus non augmented patients and the factors associated with impaired lung function in individuals with the PI*ZZ genotype.
Method
Structure of EARCO
The EARCO international registry is an observational, multicenter, international study to describe the natural history of subjects with AATD [14]. Participation in the registry is open to every clinician who manages patients with AATD. The observational design implies that patients are treated and followed according to the attending physicians’ criteria. The EARCO steering committee comprises pulmonologists, researchers and patients’ representatives, headed by two co-chairs.
The study protocol received central ethics approval by the research ethics committee of the Vall d’Hebron University Hospital of Barcelona, Spain (PR(AG)480/2018) and was subsequently approved by all participating centres. All participants provided written informed consent. The EARCO registry protocol has been registered in www.clinicaltrials.gov (ID: NCT04180319), published [14] and is hosted in www.earco.org. The personal data of the patients are kept under strict confidentiality in compliance with the provisions of the General Data Protection Regulation (GDPR) 2016/679 of the European Parliament and of the European Council of April 27th, 2016.
In countries with more than one recruiting center, there is a national coordinator that has access to fully anonymized data of the patients from their country for analysis and evaluation. Despite being an international registry, there is the possibility to build national registries in EARCO with an independent management [15,16,17].
Objectives of the EARCO registry
The main objectives of the EARCO registry are: (1) to generate longitudinal long-term, high-quality clinical data of individuals with AATD; (2) to understand the natural history and prognosis of AATD; (3) to investigate the effect of AAT augmentation and other therapies on the progression of lung disease, and (4) to learn more about the course of the disease in patients with severe AATD with genotypes other than PI*ZZ.
In the current publication, we describe the characteristics of the individuals included in the EARCO registry from its launch in February 2020 to May 2022.
Population and measurements
The inclusion criteria are: (1) individuals with diagnosed AATD; (2) deficiency is defined as AAT serum levels < 11 μM (50 mg/dL) and/or proteinase inhibitor genotypes PI*ZZ, PI*SZ and compound heterozygotes or homozygotes of other rare deficient variants. The only exclusion criteria are having at least one normal M allele or lack of patient consent.
The data collected include: demographics, proteinase inhibitor genotype, comorbidities, lung function, respiratory symptoms, ultrasound-based elastography of the liver, exacerbations of respiratory disease, quality of life measured by the COPD Assessment Test (CAT) specific questionnaire [18] and the EuroQoL (EQ) 5D-3L generic questionnaire [19], physical activity measured by the Physical Activity Vital Sign (PAVS) [20] and the mean time walked per day [21], chest computed tomography (as applicable) and treatment.
Data are entered into a secure database through an electronic case report form (eCRF) hosted in the EARCO website (www.earco.org). Data are centrally monitored, and queries are sent for missing or invalid data.
Statistical analysis
Comparison of characteristics between augmented and non-augmented PI*ZZ subjects were conducted by the Student’s t-test or Mann–Whitney U-test (if normality was not assumed) in case of quantitative variables. The Chi-squared test (Fisher test for frequencies < 5) was used for the comparison of categorical variables.
The Fibrosis-4 (FIB-4) score was calculated as age (years) × AST [IU/L]/(platelet count [109/L] × √ALT [IU/L]). A FIB-4 value < 1.45 has a high negative predictive value for ruling out advanced fibrosis and > 3.25 a high specificity and a 65% positive predictive value for ruling in advanced fibrosis.
Impairment in FEV1(%), KCO(%) or both was considered when values were < 80% of reference; the Kappa index was carried out to analyse the concordance between them. Comparison of characteristics of PI*ZZ patients according to their type of impairment in lung function was performed by the Anova test with Bonferroni correction for multiple comparisons. Linear relationships were analysed using Pearson’s correlation coefficient.
Linear regression models for all PI*ZZ, augmented and non-augmented PI*ZZ subjects were performed to identify variables related with FEV1(%). Clinical variables of interest were included as independent factors. The results were described with beta coefficients (B), 95% confidence interval (CI) and p-values. For all the tests, p-values < 0.05 were considered statistically significant. The statistical package R Studio (V2.5.1) was used for the analyses.
Results
Participating centers and characteristics of the population
The EARCO international registry was launched in February 2020 and by May 2022 there were 47 recruiting centers in 15 countries. The database included 1079 individuals, of which 35 (3.2%) were excluded, 20 because there was no information about AAT genotype and 15 had a normal M allele, leaving 1044 subjects for analysis.
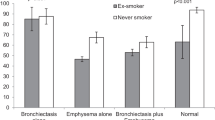
The most frequent genotype was PI*ZZ (629, 60.2%), followed by PI*SZ (305, 29.2%), PI*SS (41, 3.9%) and rare variants (69, 6.6%) (Additional file 1: Table S1). Regarding the Pi*ZZ participants, their mean age was 55.6 years (standard deviation (SD): 13.2), the age at diagnosis was 44.7 years (SD: 16.7), and 51.5% were male. Only 1.8% were active workers and 72.8% were index cases (i.e. diagnosed due to their presentation with symptoms consistent with AATD), with lung disease reported by 81.4%. Emphysema was the most frequent lung disease (57.2%) followed by COPD (55.9%) and bronchiectasis (22%), only 5 patients had panniculitis. The majority of Pi*ZZ participants were non exacerbators (Fig. 1), and 29.3% had a history of pneumonia. Comorbidities were frequent, with an age corrected Charlson index of 3.3 (SD: 1.9) and 26.1% had a cardiovascular disease (Table 1).
The mean FEV1(%) of Pi*ZZ participants was 66.9% (SD: 30.7%) and mean KCO(%) 68% (SD: 23.2%). In general participants showed a moderate impairment in quality of life with a mean CAT score of 13.2 (SD: 9.3) and EQ-5D 0.82 (SD: 0.22) and VAS 59.3 (SD: 28.2). The remaining spirometric, quality of life and activity variables, as well as the results of the blood analysis are summarised in Table 2. Differences in LFTs and quality of life parameters between different genotypes are shown in Fig. 2.
Distribution of values of lung function and quality of life according to the different genotypes. ZZ(na): non-augmented PI*ZZ; ZZ(a): Augmented PI*ZZ. In each box plot, the median value is indicated by the center horizontal black line, the 25th and 75th percentiles are indicated by the lower and upper box horizontal lines, and the mean value is indicated by the center horizontal white line. Whiskers above and below the box indicate the 90th and 10th percentiles. Circles on the high end indicate the outliers
Augmentation therapy: patterns of treatment and comparison of augmented versus non-augmented PI*ZZ individuals
A total of 190 (30%) PI*ZZ patients received augmentation therapy at the time of enrolment in the registry; of them 3 (1.5%) received infusions at home, 18 (9.5%) in Primary Care and the remaining 169 (88.9%) in the hospital. The treatment regimens most used were 120 mg/kg/biweekly in 93 (48.9%), 180 mg/kg/3 weekly in 55 (28.9%), 60 mg/kg/weekly in 35 (18.4%) and 2 patients (1%) at 250 mg/kg/monthly, in 5 cases the investigators indicate that they used a different regimen: 2 used 180 mg/kg/biweekly, and doses of 120 mg/kg/12 days, 140 mg/kg/biweekly and 60 mg/kg/biweekly were used by one patient each.
Augmented patients were older, more frequently male, former smokers and either unemployed or retired compared to non-augmented patients. They were more frequently index cases (79.9% versus 69.4%; p = 0.007) and with a chronic respiratory disease (98.9% versus 73.5%; p < 0.001). Only asthma was more frequent among non-augmented PI*ZZ patients (17.2% versus 7.4%; p < 0.001) (Table 1).
Augmented patients had more impaired lung function and worse quality of life, both respiratory-specific and generic; however, there were no significant differences in physical activity between augmented and non-augmented PI*ZZ individuals (Table 2). Differences in lung function and quality of life variables between augmented and non-augmented PI*ZZ are also shown in Fig. 2.
The haemoglobin levels and white blood cell counts were significantly higher in augmented PI*ZZ subjects versus non-augmented. Regarding liver function tests, only gamma-glutamyl transferase (GGT) (47.8 (SD: 40.1) IU/L vs 38.2 (SD: 45.2) IU/L; p < 0.001) was significantly higher in augmented patients (Table 2).
Analysis of lung function of PI*ZZ individuals: concordance between FEV1(%) and KCO(%)
Of the 449 PI*ZZ participants with valid measurements of FEV1(%) and KCO(%), 343 (76.4%) had concordant values (248 (55%) both impaired and 95 (21.2%) both normal), whereas 106 (23.6%) were discordant (Fig. 3), the Kappa index was 0.47 (95% confidence interval 0.38 to 0.55).
Patients with impairment in lung function tests or FEV1(%) alone were older, more frequently male, active or former smokers and index cases, and more frequently diagnosed with a respiratory disease. Those who had impairment in FEV1(%) alone had more frequently bronchiectasis (40.5%) and asthma (24.3%). Up to 20.2% of individuals with normal lung function had asthma and 19.1% bronchiectasis. There were no significant differences in the prevalence of liver disease, although this was numerically higher in patients with impairment in KCO(%) alone (26.1%) (Table 3).
Regarding quality of life, CAT and EQ-5D scores were worse in patients with impaired lung function tests and impaired FEV1(%) compared with the other two groups. However, there were no significant differences in the patterns of physical activity, and patients with impaired FEV1(%) had a significantly longer time walking per day (77.3 min (SD: 76.4)) compared with the other groups (Table 4).
The analysis of blood parameters showed a significant difference in the plasma levels of AAT, with the highest levels in patients with impaired FEV1(%) and the lowest in those with impaired KCO(%) (27.1 mg/dL (SD: 10) versus 22.1 mg/dL (SD: 9.2); p < 0.05). In contrast, FIB-4 was significantly higher in patients with impaired KCO(%) compared with the remaining groups and they also had numerically lower levels of platelets (Table 4).
Factors associated with impairment in FEV1(%) in multivariate analysis in PI*ZZ individuals
The multivariate analysis showed that advanced age, male sex, history of exacerbations, use of augmentation therapy and markers of inflammation (such as increased blood neutrophils and platelets) were associated with impaired FEV1(%). In contrast, increased serum levels of AAT were associated with better FEV1(%). When analysing these factors separately for augmented and non-augmented patients, the association of male sex and exacerbations remain for both groups, but markers of inflammation were only significant for the non-augmented patients (Table 5).
Discussion
Despite the severe disruption caused by the COVID-19 pandemic, the EARCO registry has been able to recruit more than 1000 individuals with severe AATD from 15 countries over the course of its first 2 years. The clinical characteristics of the participants are similar to other previous series, with a mean age of 55 years and an even distribution between sex, with 71.8% suffering from with pulmonary disease and 14% from liver disease. The majority of PI*ZZ patients had a concordant impairment in FEV1(%) and KCO(%); however, those with impairment in FEV1(%) alone more frequently had asthma or bronchiectasis and those with impairment in KCO(%) alone more often had emphysema and liver involvement. As expected, PI*ZZ patients on augmentation therapy were more severely affected by lung disease and were more frequently index cases compared with non-augmented PI*ZZ cases. Increased age, male sex, more frequent exacerbations, and elevated markers of inflammation, such as blood neutrophils and platelets, were associated with impaired FEV1(%), whereas higher levels of serum AAT were associated with better FEV1(%) in multivariate analysis.
The investigation about the characteristics and natural history of rare diseases, such as AATD, requires the development of registries to collect information about a large number of cases [12, 22]. National registries have been developed in Europe, United States (US) and Canada [5,6,7] and more than 20 years ago, the Alpha 1 International Registry was funded to harmonise data collection from several countries [8]. However, the greatest challenge has always been the collection of long-term follow up data in multicenter, international registries. At the end of the last century, the National Heart, Lung and Blood Institute (NHLBI) registry of patients with severe AATD recruited + 1000 individuals in the US and followed them for between 3.5 to 7 years to investigate the effectiveness of augmentation therapy in slowing the rate of decline of FEV1 [23]. In Europe, the Swedish, UK and German registries, among others, have generated relevant information about clinical phenotypes, comorbidities and factors influencing rate of decline of lung function [5, 6, 24,25,26,27]. However, despite these and other examples, there is a clear unmet need of large series of severe AATD patients from different countries, with different genotypes and receiving different treatments to provide new information about the clinical and functional characteristics of the disease and its natural history.
Almost two thirds of the individuals recruited have the most frequent deficient genotype PI*ZZ, but up to 8% are carriers of rare deficient variants. Nearly 30% were non index cases, the mean FEV1(%) and KCO(%) were around 75% and participants showed a moderate impairment in quality of life.
Only 30% of the severe deficient PI*ZZ individuals received augmentation therapy; this percentage is influenced by the recruitment of patients from countries in which augmentation is not reimbursed [28]. Nevertheless, augmented patients were more frequently index cases, and had more severe impairment in lung function and more frequent exacerbations compared with non-augmented. Interestingly, most augmented patients were receiving regimens other than the approved dosage of weekly infusions of 60 mg/kg. The most frequent regimen was biweekly administration of 120 mg/kg, followed by 180 mg/Kg every 3 weeks, and 5 patients were using other regimens, probably individual adjustments of dosage according to trough levels of serum AAT, a frequent practice that is not recommended by experts [12].
The usual pattern of lung disease in severe AATD is basal, bilateral, panlobular emphysema; however, different series have described other lung phenotypes, such as bronchiectasis, chronic bronchitis, asthma or even apical emphysema [25, 26]. Our population reflects this heterogeneity with 17.7% (22% of the PI*ZZ) having bronchiectasis and 15.1% (14.1% of the PI*ZZ) having asthma. The majority of our PI*ZZ patients (76%) had concordant impairment in FEV1(%) and KCO(%); interestingly, among the discordant subjects, those with impairment in FEV1(%) alone had more frequently bronchiectasis or asthma, and those with impairment in KCO(%) alone had signs of more liver involvement with a significantly higher index FIB-4, lower levels of platelets and a higher percentage of subjects with diagnosed liver disease. To the best of our knowledge, this observation of the possible link between a predominant impairment in diffusion capacity and more frequent or severe liver disease has not been previously reported and requires further investigation. Moreover, patients with impairment in KCO(%) also had significantly lower levels of serum AAT compared with patients with impairment in FEV1(%), suggesting a stronger relationship between lower levels of AAT and lung parenchymal disease instead of bronchial disease. Alternatively, patients with FEV1(%) impairment may be more severe and had higher levels of systemic inflammation which may results in elevated plasma levels of AAT. Concordance between FEV1/FVC and KCO was also observed by Ward et al. [29] in 70% of a group of 530 PI*ZZ patients from the UK. However, in their study the number of patients with impaired KCO alone was too small (only 8 subjects) and no description of clinical phenotypes were provided [29]. In a further study by the same group, a different rate of progression of impairment in airflow obstruction or in gas transfer in PI*ZZ according to impairment in FEV1 or KCO was demonstrated [6].
Increased serum levels of AAT in PI*ZZ individuals were significantly and independently associated with better FEV1(%) in multivariate analysis; this observation concurs with the results of the RAPID trial which described those patients with higher trough serum AAT levels had a reduced rate of decline of lung density, even in the placebo arm, in which the range of AAT trough levels was very limited [30].
Other independent variables associated with impaired lung function were male sex, exacerbations and some blood inflammatory markers. A faster decline in lung function in males has been already described [31, 32]; although the reason is unclear, among others, males are more often involved in “blue collar” occupations and exposed to environmental pollutants that may impact in lung function [24, 33]. The significant and strong association of exacerbations with impaired lung function may be bidirectional: patients with more severe impairment in FEV1(%) have an increased risk of exacerbations and more frequent exacerbations accelerate FEV1(%) decline. Our results agree with previous findings in longitudinal studies that confirm the impact of exacerbations in the natural history of lung disease in AATD [27, 31, 34] and stress the importance of prevention of exacerbations in patients with AATD and lung disease.
Patients with COPD have increased lung and systemic inflammation, and since AAT is an acute phase protein, they also have increased serum levels of AAT compared with healthy controls [35]. Some studies have suggested that there is a relationship between increased markers of systemic inflammation and the severity of lung and liver disease [36,37,38]. In our PI*ZZ patients, markers of systemic inflammation, such as increased neutrophils and platelets, were associated with more impaired FEV1(%), but this association was not observed in augmented patients. This may be an statistical effect due to a smaller sample size, but it may also be a consequence of the anti-inflammatory effect of the infused AAT that attenuates bronchial [39] and systemic inflammation [38, 40].
Our study has some limitations, the most important is the cross-sectional nature of data; however, there was a lack of information about the characteristics of large, international series of patients with severe AATD. On the other hand, it has the strength of a harmonised collection of data from many different countries with a single protocol and with close monitoring and quality control of the included data.
Conclusions
The EARCO registry has shown novel information about the clinical and functional characteristics of a large, international registry of patients with AATD. EARCO is a prospective study that will provide relevant information about the natural history of AATD in the future and is the platform for the development of other clinical studies in the field.
Availability of data and materials
The data that support the findings of this study are available from the EARCO group but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the EARCO steering committee.
Change history
18 February 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12931-023-02340-6
Abbreviations
- AAT:
-
Alpha-1 antitrypsin
- AATD:
-
Alpha-1 antitrypsin deficiency
- AIR:
-
Alpha-1 International Registry
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- BODEx:
-
Body mass index, obstruction, dyspnoea, exacerbations index
- CAT:
-
COPD assessment test
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CRC:
-
Clinical Research Collaboration
- CRP:
-
C-reactive protein
- EARCO:
-
European Alpha-1 antitrypsin Research Collaboration
- eCRF:
-
Electronic case report form
- ERS:
-
European Respiratory Society
- EQ-5D:
-
Euro QoL 5 dimensions questionnaire
- FEV1:
-
Forced expiratory volume in 1 s
- FIB-4:
-
Fibrosis 4
- FVC:
-
Forced vital capacity
- GDPR:
-
General Data Protection Regulation
- GGT:
-
Gamma-glutamyl transferase
- IU:
-
International units
- KCO:
-
Carbon monoxide transfer coefficient
- NHLBI:
-
National Heart, Lung and Blood Institute
- NS:
-
Non-significant
- PAVS:
-
Physical Activity Vital Sign
- PI:
-
Protease inhibitor
- SD:
-
Standard deviation
- UK:
-
United Kingdom
- US:
-
United States of America
- VAS:
-
Visual analogue scale
References
Strnad P, McElvaney NG, Lomas DA. Alpha1-antitrypsin deficiency. N Engl J Med. 2020;382(15):1443–55.
Blanco I, Bueno P, Diego I, Pérez-Holanda S, Casas F, Esquinas C, et al. Alpha-1 antitrypsin Pi*Z gene frequency and Pi*ZZ genotype numbers worldwide: an update. Int J Chron Obstruct Pulmon Dis. 2017;12:561–9.
Blanco I, Diego I, Bueno P, Pérez-Holanda S, Casas-Maldonado F, Miravitlles M. Prevalence of α1-antitrypsin PiZZ genotypes in patients with COPD in Europe: a systematic review. Eur Respir Rev. 2020;29(157):200014.
Miravitlles M, Herepath M, Priyendu A, Sharma S, Vilchez T, Vit O, et al. Disease burden associated with alpha-1 antitrypsin deficiency: systematic and structured literature reviews. Eur Respir Rev. 2022;31(163):210262.
Piitulainen E, Tanash HA. The clinical profile of subjects included in the Swedish National Register on individuals with severe alpha-1 antitrypsin deficiency. COPD. 2015;12(S1):36–41.
Stockley RA, Edgar RG, Pillai A, Turner AM. Individualized lung function trends in alpha-1-antitrypsin deficiency: a need for patience in order to provide patient centered management? Int J Chron Obstruct Pulmon Dis. 2016;11:1745–56.
Piras B, Ferrarotti I, Lara B, Martinez MT, Bustamante A, Pirina P, et al. Characteristics of Italian and Spanish patients with alpha-1-antitrypsin deficiency: Identifying clinical phenotypes. Eur Respir J. 2013;42:54–64.
Stockley RA, Luisetti M, Miravitlles M, Piitulainen E, Fernandez P, on behalf of the Alpha One International Registry (A.I.R.) group, et al. Ongoing research in Europe: Alpha One International Registry (AIR) objectives and development. Eur Respir J. 2007;29:582–6.
Schouten IGM, Kasteleyn MJ, Tsonaka R, Bals R, Turner AC, Ferrarotti I, et al. Long-term effect of α1-antitrypsin augmentation therapy on the decline of FEV1 in deficient patients: an analysis of the AIR database. ERJ Open Res. 2021;7(3):00194–2021.
Barrecheguren M, O’Hara K, Wilkens M, Boyd J, Kolda E, Lara B, et al. Research priorities in alpha-1 antitrypsin deficiency: results of a patients’ and healthcare providers’ international survey from the EARCO Clinical Research Collaboration. ERJ Open Res. 2020;6(4):00523–2020.
http://ec.europa.eu/health/archive/ph_threats/non_com/docs/contribution_policy.pdf. Accessed 19 Apr 2022.
Miravitlles M, Dirksen A, Ferrarotti I, Koblizek V, Lange P, Mahadeva R, et al. European Respiratory Society Statement: diagnosis and treatment of pulmonary disease in alpha-1 antitrypsin deficiency. Eur Respir J. 2017;50:1700610.
Miravitlles M, Chorostowska-Wynimko J, Ferrarotti I, McElvaney NG, O'Hara K, Stolk J, et al. The European Alpha-1 Research Collaboration (EARCO): a new ERS Clinical Research Collaboration to promote research in alpha-1 antitrypsin deficiency. Eur Respir J. 2019;53(2).
Greulich T, Altraja A, Barrecheguren M, Bals R, Chlumsky J, Chorostowska-Wynimko J, et al. Protocol for the EARCO Registry: a pan-European observational study in patients with α1-antitrypsin deficiency. ERJ Open Res. 2020;6(1):00181–2019.
Barrecheguren M, Torres-Duran M, Casas-Maldonado F, Miravitlles M. Spanish implementation of the new international alpha-1 antitrypsin deficiency international registry: The European Alpha-1 Research Collaboration (EARCO). Arch Bronconeumol. 2021;57(2):81–2.
Sucena M, Gomes J, Guimarães C, Miravitlles M. Implementation of European Alpha-1 Research Collaboration (EARCO) in Portugal: the future starts now. Pulmonology. 2020;26(4):181–3.
Torres-Duran M, López-Campos JL, Rodríguez-Hermosa JL, Esquinas C, Martínez-González C, Hernández-Pérez JM, et al. Demographic and clinical characteristics of patients with alpha-1 antitrypsin deficiency genotypes PI*ZZ and PI*SZ in the Spanish registry of EARCO. ERJ Open Res. 2022;8(3):00213–2022.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline LN. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54.
EuroQoL Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Greenwood JL, Joy EA, Stanford JB. The Physical Activity Vital Sign: a primary care tool to guide counseling for obesity. J Phys Act Health. 2010;7(5):571–6.
Ramon MA, Esquinas C, Barrecheguren M, Pleguezuelos E, Molina J, Quintano JA, et al. Self-reported daily walking time in COPD: relationship with relevant clinical and functional characteristics. Int J Chron Obstruct Pulmon Dis. 2017;12:1173–81.
Chorostowska-Wynimko J, Wencker M, Horváth I. The importance of effective registries in pulmonary diseases and how to optimize their output. Chron Respir Dis. 2019;16:1479973119881777.
Survival and FEV1 decline in individuals with severe deficiency of alpha-1 antitrypsin. The Alpha-1 Antitrypsin Deficiency Registry Study Group. Am J Respir Crit Care Med. 1998;158:49–59.
Piitulainen E, Tornling G, Eriksson S. Environmental correlates of impaired lung function in non-smokers with severe alpha 1-antitrypsin deficiency (PiZZ). Thorax. 1998;53:939–43.
Wood AM, Simmonds MJ, Bayley DL, Newby PR, Gough SC, Stockley RA. The TNFalpha gene relates to clinical phenotype in alpha-1-antitrypsin deficiency. Respir Res. 2008;9(1):52.
Parr DG, Guest PG, Reynolds JH, Dowson LJ, Stockley RA. Prevalence and impact of bronchiectasis in alpha1-antitrypsin deficiency. Am J Respir Crit Care Med. 2007;176(12):1215–21.
Fähndrich S, Bernhard N, Lepper PM, Vogelmeier C, Seibert M, Wagenpfeil S, et al. Exacerbations and duration of smoking abstinence are associated with the annual loss of FEV1 in individuals with PiZZ alpha-1-antitrypsin deficiency. Respir Med. 2017;129:8–15.
Horváth I, Canotilho M, Chlumský J, Chorostowska-Wynimko J, Corda L, Derom E, et al. Diagnosis and management of α1-antitrypsin deficiency in Europe: an expert survey. ERJ Open Res. 2019;5(1):00171–2018.
Ward H, Turner AM, Stockley RA. Spirometric and gas transfer discordance in alpha-1 antitrypsin deficiency; patient characteristics and progression. Chest. 2014;145:1316–24.
Chapman KR, Burdon JG, Piitulainen E, Sandhaus RA, Seersholm N, Stocks JM, et al. Intravenous augmentation treatment and lung density in severe α1 antitrypsin deficiency (RAPID): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;386(9991):360–8.
Dawkins PA, Dawkins CL, Wood AM, Nightingale PG, Stockley JA, Stockley RA. Rate of progression of lung function impairment in alpha-1-antitrypsin deficiency. Eur Respir J. 2009;33:1338–44.
Demeo DL, Sandhaus RA, Barker AF, Brantly ML, Eden E, McElvaney NG, et al. Determinants of airflow obstruction in severe alpha-1-antitrypsin deficiency. Thorax. 2007;62(9):806–13.
Rangaraju M, Turner AM. Why is disease penetration so variable in alpha-1 antitrypsin deficiency? The contribution of environmental factors. Chronic Obstruct Pulmon Dis. 2020;7(3):280–9.
Hiller AM, Piitulainen E, Jehpsson L, Tanash H. Decline in FEV1 and hospitalized exacerbations in individuals with severe alpha-1 antitrypsin deficiency. Int J Chron Obstruct Pulmon Dis. 2019;14:1075–83.
Janciauskiene S, DeLuca DS, Barrecheguren M, Welte T, Miravitlles M. Serum levels of alpha1-antitrypsin and their relationship with COPD in the General Spanish Population. Arch Bronconeumol. 2020;56:76–83.
Núñez A, Belmonte I, Miranda E, Barrecheguren M, Farago G, Loeb E, et al. Association between circulating alpha-1 antitrypsin polymers and lung and liver disease. Respir Res. 2021;22(1):244.
Beiko T, Janech MG, Alekseyenko AV, Atkinson C, Coxson HO, Barth JL, et al. Serum proteins associated with emphysema progression in severe alpha-1 antitrypsin deficiency. Chronic Obstruct Pulmon Dis. 2017;4(3):204–16.
O’Brien ME, Fee L, Browne N, Carroll TP, Meleady P, Henry M, et al. Activation of complement component 3 is associated with airways disease and pulmonary emphysema in alpha-1 antitrypsin deficiency. Thorax. 2020;75(4):321–30.
Stockley RA, Bayley DL, Unsal I, Dowson LJ. The effect of augmentation therapy on bronchial inflammation in alpha1-antitrypsin deficiency. Am J Respir Crit Care Med. 2002;165(11):1494–8.
Schmid ST, Koepke J, Dresel M, Hattesohl A, Frenzel E, Perez J, et al. The effects of weekly augmentation therapy in patients with PiZZ α1-antitrypsin deficiency. Int J Chron Obstruct Pulmon Dis. 2012;7:687–96.
Acknowledgements
The authors would like to thank the patients who participated in this study and the EARCO study investigators (listed below). We wish to acknowledge Elise Heuvelin from the ERS office (Lausanne, Switzterland) for her support in the management of EARCO, and Gemma Vilagut and Christina Founti (Bioclever, Barcelona, Spain) for their support in EARCO data monitoring. We also acknowledge the participation of Eduardo Loeb (Barcelona, Spain) in the development of the database and the monitoring of the data.
List of EARCO study investigators: Georg-Christian Funk (Austria), Wim Janssens, Silvia Pérez-Bogerd (Belgium), Leidy Prada (Colombia), Ana Hecomovic (Croatia), Eva Bartosovska, Jan Chlumsky, (Czech Republic), Alan Altraja, Jaanus Martti (Estonia), Angelo G. Corsico, Ilaria Ferrarotti, Simone Scarlata, Mario Malerba (Italy), Jan Stolk, Emily F van’t Wout (Netherlands), Joanna Chorowstoska-Wyminko (Poland), Catarina Guimaraes, Maria Sucena, Ana Caldas Raquel Marçoa, Isabel Ruivo dos Santos, Bebiana Conde, Maria Joana Reis Amado Maia Da Silva, Rita Boaventura (Portugal), Ruxandra Ulmeanu (Romania), María Torres-Duran, Marc Miravitlles, Miriam Barrecheguren, Juan Luis Rodriguez-Hermosa, Myriam Calle-Rubio, José María Hernández-Pérez, José Luis López-Campos, Francisco Casas-Maldonado, Ana Bustamante, Carlota Rodriguez-García, Cristina Martinez-González, Cruz González, Eva Tabernero, Lourdes Lázaro, Virginia Almadana, Mar Fernández-Nieto, Francisco Javier Michel de la Rosa, Carlos Martíez-Rivera, Layla Diab, María Isabel Parra (Spain), Hanan Tanash, Eeva Piitulainen (Sweden), Christian F. Clarenbach (Switzerland), Serap Argun Baris, Dilek Karadogan, Sebahat Genç (Turkey), Alice M. Turner, Beatriz Lara, David G. Parr (United Kingdom). EARCO Steering committee: Christian F Clarenbach and Marc Miravitlles (Co-chairs), Robert Bals, Jan Stolk, Joanna Chorostowska-Wynimko, Karen O’Hara, Marion Wilkens, José Luis López-Campos, Alice M. Turner, Ilaria Ferrarotti, Gerry McElvaney and Robert A. Stockley.
Funding
The International EARCO registry is funded by unrestricted grants of Grifols, CSL Behring, Kamada, pH Pharma and Takeda to the European Respiratory Society (ERS).
Author information
Authors and Affiliations
Contributions
MM and CFC drafting of the manuscript. CE performed the stistical analysis. All authors participated in the study concept, design and acquisition of data. All authors performed a critical revision and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol received central ethics approval by the research ethics committee of the Vall d’Hebron University Hospital of Barcelona, Spain (PR(AG)480/2018) and was subsequently approved by all participating centres. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
Marc Miravitlles has received speaker fees from AstraZeneca, Boehringer Ingelheim, Kamada, Chiesi, Cipla, Menarini, Rovi, Bial, Sandoz, Takeda, Zambon, CSL Behring, Specialty Therapeutics, Grifols and Novartis, consulting fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Bial, Gebro Pharma, Kamada, CSL Behring, Laboratorios Esteve, Ferrer, Mereo Biopharma, Verona Pharma, TEVA, Spin Therapeutics, pH Pharma, Novartis, Sanofi and Grifols and research grants from Grifols. Alice M Turner has received either grants or speaker fees from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Chiesi, CSL Behring, Takeda, Vertex and Grifols Biotherapeutics. María Torres-Durán has received speaker fees from Chiesi, CSL Behring, Grifols and Resmed and consulting fees from CSL Behring and Grifols. José Luis López-Campos has received honoraria during the last 3 years for lecturing, scientific advice, participation in clinical studies or writing for publications for (alphabetical order): AstraZeneca, Boehringer Ingelheim, Chiesi, CSL Behring, Esteve, Ferrer, Gebro, GlaxoSmithKline, Grifols, Menarini, Novartis, Rovi, and Teva. Juan Luis Rodriguez-Hermosa has received speaker fees from Zambon, Bial, Gebro Pharma, GlaxoSmithKline, Chiesi, Boehringer Ingelheim, CSL Behring and Grifols. José María Hernández-Pérez has received speaker fees from Grifols, CSL Behring, Astra-Zeneca, GSK, Bial laboratory, Teva laboratory, support for attending meetings from Grifols, CSL Behring, and consulting fees from CSL Behring. David G Parr has received consulting fees from Mereo Biopharma. Francisco Casas-Maldonado has received speaker fees from AstraZeneca, Bial, Boehringer Ingelheim, Chiesi, Gebro Pharma, GlaxoSmithKline, Laboratorios Esteve, Laboratorios Ferrer, Menarini, Novartis, Rovi, TEVA, VERTEX, Zambon, CSL Behring and Grifols and consulting fees from AstraZeneca, Chiesi, GlaxoSmithKline, CSL Behring and Grifols. Miriam Barrecheguren has received speaker fees from Grifols, Menarini, CSL Behring, GSK, Boehringer Ingelheim and consulting fees from GSK, Novartis, CSL Behring and Boehringer Ingelheim. Ana Bustamante has received speaker fees from Boehringer Ingelheim, AstraZeneca, GSK, Novartis and Ferrer, and funding for traveling or attending meetings from CSL Behring, AstraZeneca and Chiesi. Cruz González has received speaker fees from, Menarini, GSK, Novartis, Boehringer Ingelheim and Chiesi. Carlota Rodriguez has received speaker fees from GSK, AstraZeneca, Grifols, Chiesi, Ferrer, Menarini and Boehringer Ingelheim, expert testimony for Chiesi, support for attending meetings from FAES. Cristina Esquinas has received speaker fees from CSL Behring. Christian F Clarenbach received advisory fees from Roche, Novartis, Boehringer, GSK, Astra Zeneca, Sanofi, Vifor, OM Pharma, CSL Behring, Grifols, Daiichi Sankyo and MSD. The remaining authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The error in Figure 2 legends. It has been corrected.
Supplementary Information
Additional file 1: Table S1.
Description of rare variants identified in EARCO.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Miravitlles, M., Turner, A.M., Torres-Duran, M. et al. Clinical and functional characteristics of individuals with alpha-1 antitrypsin deficiency: EARCO international registry. Respir Res 23, 352 (2022). https://doi.org/10.1186/s12931-022-02275-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02275-4