Abstract
Background
Acute respiratory distress syndrome (ARDS) is one of the most severe complications of SARS-CoV-2 infection. Non-Invasive Respiratory Support (NRS) as Continuous Positive Airway Pressure (CPAP) and/or Non-Invasive Ventilation (NIV) has been proven as effective in the management of SARS-CoV-2-related ARDS. However, the most appropriate timing for start NRS is unknown.
Methods
We conducted a prospective pilot study including all consecutive patients who developed moderate SARS-CoV-2-related ARDS during hospitalization. Patients were randomly divided into two intervention groups according to ARDS severity (assessed by PaO2/FiO2-P/F) at NRS beginning: group A started CPAP/NIV when P/F was ≤ 200 and group B started CPAP/NIV when P/F was ≤ 150. Eligible patients who did not give their consent to CPAP/NIV until the severe stage of ARDS and started non-invasive treatment when P/F ≤ 100 (group C) was added. The considered outcomes were in-hospital mortality, oro-tracheal intubation (OTI) and days of hospitalization.
Results
Among 146 eligible patients, 29 underwent CPAP/NIV when P/F was ≤ 200 (Group A), 68 when P/F was ≤ 150 (Group B) and 31 patients agreed to non-invasive treatment only when P/F was ≤ 100 (Group C). Starting NRS at P/F level between 151 and 200 did not results in significant differences in the outcomes as compared to treatment starting with P/F ranging 101–150. Conversely, patients undergone CPAP/NIV in a moderate stage (P/F 101–200) had a significantly lower in-hospital mortality rate (13.4 vs. 29.0%, p = 0.044) and hospitalization length (14 vs. 15 days, p = 0.038) than those in the severe stage (P/F ≤ 100). Age and need for continuous ventilation were independent predictors of CPAP/NIV failure.
Conclusions
Starting CPAP/NIV in patients with SARS-CoV-2-related ARDS in moderate stage (100 > P/F ≤ 200) is associated to a reduction of both in-hospital mortality and hospitalization length compared to the severe stage (P/F ≤ 100). Starting CPAP/NIV with a P/F > 150 does not appear to be of clinical utility.
Similar content being viewed by others
Background
Acute hypoxemic respiratory failure (hARF) is one of the most serious complications of SARS-CoV-2 infection, evolving into acute respiratory distress syndrome (ARDS). Its optimal management is still much debated. The efficacy of Non-Invasive Respiratory Support (NRS) as Continuous Positive Airway Pressure (CPAP) and/or Non-Invasive mechanical Ventilation (NIV) in SARS-CoV-2-related hARF is controversial [1,2,3], even if several studies support CPAP use [4,5,6,7,8,9,10]. A trial of CPAP seems to significantly reduce mortality and oro-tracheal intubation (OTI) rates compared to conventional oxygen therapy in patients with SARS-CoV-2-related ARDS [10]. Furthermore, a delay in the timing of OTI does not seem to worsen mortality and morbidity rates in critically ill patients with COVID-19 [9].
Application of a positive end-expiratory pressure (PEEP) through CPAP can prevent alveolar collapse and promote recruitment of already collapsed alveoli, thus improving ventilation of poorly ventilated though adequately perfused ones and reducing the shunt volume [2]. Moreover, compensatory mechanisms of hypoxic vasoconstriction (Euler-Lilijestrand mechanism) are inadequate in SARS-CoV-2-related ARDS, resulting in normal perfusion of poorly ventilated alveoli, with consequent severe hypoxemia [2]. The recruitment of these alveoli through PEEP would significantly improve hypoxia and may prevent OTI. In addition mortality rates in patients with COVID-19-related ARDS undergoing OTI and invasive mechanical ventilation (IMV) appear extraordinarily high [4, 9, 11,12,13,14,15,16], up to 97% during first pandemic waves, also due to the associated risk of bacterial superinfection [13]. More recently Peñuelas et al. [17] reports an overall 180-day survival rates of 59% in patients undergone IMV for COVID-19. During pandemic, the availability of intensive care units (ICUs) beds may also be poor. For all these reasons, an optimized and appropriate use of CPAP could represent a valuable weapon to the clinician.
CPAP has been reported to be effective in SARS-CoV-2-related hARF but, at present, the most appropriate timing to start treatment is unknown [3, 6, 18]. In this regard, Italian and English guidelines encourage new controlled studies on CPAP and NIV to define the role and timing for its use [18, 19]. Currently no standardized criteria for starting NRS have been defined. Clinical trials comparing the impact of CPAP/NIV on major outcomes when started at different severity levels of SARS-CoV-2-related ARDS (assessed by the PO2/FiO2-P/F ratio at blood gas analysis) as whether an early treatment can favor positive outcomes to date are not available.
The aim of this study was to evaluate if the timing of CPAP/NIV started at different P/F ratio levels could influence the outcomes (in-hospital mortality, OTI rate, hospitalization length) in patients with ARDS due to SARS-CoV-2 pneumonia.
Materials and methods
Study design
A prospective pilot study was carried out at the two Covid Centers of Policlinic Hospital, University of Campania "L. Vanvitelli", Naples. All patients with SARS-CoV-2 infection consecutively admitted to the Covid Centers of Internal Medicine and Infectious Diseases Units from December 13, 2020 to May 13, 2021, were evaluated. Diagnosis of ARDS and classification as mild (200 > PaO2/FiO2 ≤ 300), moderate (100 > PaO2/FiO2 ≤ 200) or severe (PaO2/FiO2 ≤ 100) were placed according to the Berlin Criteria [20].
Among all admitted patients with SARS-CoV-2 infection, only those who developed a PaO2/FiO2 (P/F) ratio ≤ 200 during hospitalization were enrolled in the study. Patients who already showed a P/F ≤ 200 at admission were excluded to avoid different standards of care prior to enrollment, which could potentially affect the results. Patients with hypercapnic respiratory failure and patients with contraindications to NRS, such as hemodynamic instability (systolic blood pressure < 90 mmHg despite fluid resuscitation), coma (Glasgow Coma Scale—GCS < 8) or non-compliant, were also excluded.
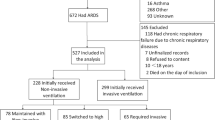
Enrolled patients were assigned to two intervention groups in relation to the ward they were admitted to. Patients admitted to the Covid Center of Internal Medicine Unit (group-A) underwent CPAP/NIV as soon as they developed a P/F below 200. Conversely, patients admitted to the Covid Center of Infectious Disease Unit (group-B) were treated with CPAP/NIV when the P/F level fell below 150. Beyond NRS treatment, both groups were guaranteed the same standard of care (see below). The study design is shown in Fig. 1.
Study design: Group A started CPAP/NIV when P/F fell below 200, Group B underwent CPAP/NIV when P/F fell below 150. Group C derives from patients initially excluded from the study for refusal of non-invasive treatment and who subsequently initiated treatment with CPAP/NIV in a severe stage of ARDS (P/F ≤ 100). CPAP Continuous Positive Airway Pressure, NIV Non-Invasive Ventilation, P/F PaO2/FiO2 rate
Part of the eligible patients (development of moderate respiratory distress during hospitalization) did not initially consent to CPAP/NIV treatment and were excluded from the study. A proportion of these patients gave consent to treatment in a severe phase of respiratory distress (P/F ≤ 100) and were also compared to those treated in moderate stage (groups-A and B, Fig. 1). The subgroup of patients who started the treatment in a severe stage of ARDS was identified as group-C.
Data collection
Diagnosis of SARS-CoV-2 infection was done by RT-PCR test of nasopharyngeal swab sample [21]. On admission, all patients underwent anamnestic data collection, physical examination, blood tests and gas analysis, chest X-ray and lung ultrasound evaluation (standardized using the Lung Ultrasound score—LUS) [22]. A high-resolution chest tomography (HRCT) was performed. CT severity score was used for quantitative severity assessment by evaluating the extent of lung damage due to SARS-CoV-2 infection [23].
Treatments
Medical treatments, respiratory support and clinical monitoring were performed in accordance with national and international guidelines.
NRS treatment was sequential. All patients who developed a P/F ≤ 200 (group-A) or ≤ 150 (group-B) during hospitalization started CPAP. Patients with inadequate response to CPAP were treated with NIV. In case of NIV failure, patients underwent OTI and IMV.
Initial PEEP was uniformly set at 7 cmH20, with titration upwards or downwards according to clinical response (peripheral oxygen saturation—SpO2, respiratory rate—RR, blood gases) and patient's tolerance. The delivered oxygen (FiO2) was titrated to guarantee SpO2 > 92%. We used low starting pressures to reduce risk of pneumothorax and/or pneumomediastinum [24]. Patients who showed an acceptable response (SpO2 ≥ 92%) to High Flow Nasal Cannula (HFNC) were guaranteed oral feeding and CPAP support < 18 h/day. For patients who did not reach an acceptable SpO2 (< 92%) on HFNC, continuous CPAP (> 18 h/day) and total parenteral nutrition were provided.
Patients on CPAP without any clinical improvement (SpO2 and/or P/F) after a 4–6 h trial and/or developing signs of respiratory fatigue (RR > 30 acts/min, increased lactate, activation of accessory respiratory muscles) and/or hypercapnia were converted to NIV (modality: Pressure Support Ventilation, PSV) by applying a pressure support (PS). Initial PS were set at an intermediate level, starting from 6–8 cmH2O with titration upwards to ensure a TV of 7–8 ml/kg or downwards, if not tolerated [25].
Patients either with hypoxemia unresponsive to NIV (PaO2 < 60 mmHg) or with P/F persistently < 100 despite NRS (at least 6 h long) or who develop hemodynamic instability, underwent rapid OTI and IMV, in absence of contraindications or patient refusal (DNI).
Conversely, patients with a P/F ≥ 200 and a RR < 25 acts/min after 48 h of NRS weaned fast if they underwent only CPAP. Otherwise, PS was progressively reduced to initial levels and then converted to CPAP if they underwent NIV. Subsequently, oxygen was supplemented by HFNC or nasal cannulae, according to clinical needs.
The chosen interface for CPAP was the helmet, for NIV a full-face mask was used instead (Dimar, Medolla—Italy). CPAP/NIV was delivered by a compressed gas-based ventilator (ResMed Astral 150, San Diego, United States) connected to the interface through a bi-tube circuit. To reduce aerosolization, filters were interposed in the expiratory circuit. Healthcare personnel was equipped with complete body protection (double gloves, long-sleeved water-resistant gowns, goggles/face shields) and filtering face-piece (FFP)-3 masks.
Constant monitoring of patients' conditions and immediate OTI in case of NRS failure were guaranteed by a telemetry system (evaluation of vital parameters: SpO2, blood pressure, heart and respiratory rate, body temperature) and 24 h video-surveillance. Respiratory function was assessed with blood gas analysis, once daily or more frequently according to clinical status. In case of worsening, a chest imaging (ultrasound/X-ray/CT) was repeated.
Drug treatment included steroids (dexamethasone 6 mg/day for 10 days), low-molecular weight heparin (LMWH, prophylactic or therapeutic dosage depending on clinical needs), remdesivir (1st day 200 mg, 2nd-5th day 100 mg, only in patients within 10 days from symptoms’ onset) and tocilizumab (8 mg/kg once), according to the indications of National Institute of Health (NIH) and Italian Drugs Agency (AIFA) [26, 27]. Antibiotic therapy was given to all patients with evidence of bacterial superinfection.
Outcome
The primary endpoints were in-hospital mortality. Secondary endpoints were: OTI rate and overall hospitalization length. The composite outcome of death and/or need for OTI was used to define CPAP/NIV failure in the overall population.
Statistical analysis
Given the exploratory design of the study and no data available in literature on this topic to date, no formal sample size calculation is needed. However, due to the real-life nature of the study, we collected data on all consecutive patients with COVID-19 satisfying the inclusion criteria. All variables were summarized by descriptive statistics techniques. In depth, qualitative variables were presented as absolute and relative frequencies. Quantitative data, indeed, were summarized either as mean and standard deviation (SD), if normally distributed, or median and interquartile range (IQR), otherwise. Their distribution was previously assessed by the Shapiro–Wilk test. Between groups differences were analyzed either by Pearson Chi-square or Fisher exact test for qualitative variables, as appropriate. Student t-test or Mann–Whitney U-test were instead computed as for quantitative variables, according to their distribution. Potential predictive factors of the composite outcome of mortality and OTI were assessed by a univariate Cox regression model, with days between symptoms and death/OTI as time-for-event variables. Statistically significant variables at univariate analysis were included in a multivariable Cox regression model, consistently with the number of events. Overall survival and OTI rates were further summarized by Kaplan–Meier curves. A p-value < 0.05 was considered statistically significant. All analyses were performed by STATA 16 software (STATA Corp.).
Results
Of 512 SARS-CoV-2 infected patients admitted with a P/F > 200, 194 were admitted to the Covid Center of Internal Medicine Unit (group-A) and were eligible to start CPAP/NIV treatment if they developed a P/F ≤ 200; 318 patients were admitted to the Covid Center of Infectious Disease Unit (group-B) and were eligible to initiate CPAP/NIV if they developed a P/F ≤ 150 (Fig. 2).
In intervention group-A, of the 194 eligible patients admitted, 49 developed a P/F ≤ 200. Of these, 20 patients initially refused (14/20) or had ongoing contraindications (6/20: 3 septic shock, 2 hypercapnic respiratory failure, 1 coma) to NRS. Therefore, 29 patients were finally enrolled in the intervention group-A and underwent CPAP when P/F was ≤ 200 (Fig. 2).
In intervention group-B, of the 318 eligible patients admitted, 99 developed a P/F ≤ 200 and 97 of these (97/99, 98%) demonstrated further worsening to a P/F ≤ 150. Of these, 29 patients initially refused (22/29) or had ongoing contraindications (7/29: 2 septic shock, 3 hypercapnic respiratory failure, 2 coma) to NRS and 68 patients were finally enrolled in the intervention group-B and underwent CPAP when P/F was ≤ 150 (Fig. 2).
After initial refusal, 31 eligible patients consented to CPAP/NIV treatment when P/F was ≤ 100 and were subsequently enrolled as Group-C (Fig. 2).
The overall mortality rate among patients treated with CPAP/NIV was 17.2% (n = 22). According to the study methods, 33 cases of CPAP failure (25.8% of the total, subsequently treated with NIV) and 10 cases of NIV failure (30.3% of patients requiring PS, subsequently undergone OTI and IMV) have been reported. No infection among health personnel was recorded throughout the study period.
Baseline characteristics and outcome of patients with moderate ARDS according to P/F above or below 150
Baseline characteristics and outcomes of populations with moderate ARDS and P/F between 151 and 200 (group-A) and between 101 and 150 (group-B) are summarize in Tables 1 and 2.
Age, Charlson Comorbidity Index (CCI), prevalence of each comorbidity, duration of symptoms before admission, blood tests, gas analysis and/or radiological parameters do not show any statistically significant difference at admission (Table 1). Likewise, there is also no significant difference in ventilation modalities (pressures, need for PS or continuous ventilation, ventilation days) or in medications used (Table 2).
The CPAP failure rate and the need to convert to NIV were 17.2% and 19.1% in groups-A and B, respectively. The NIV failure rate and the need for OTI and therefore IMV was 6.9% and 11.8% in groups-A and B, respectively. The overall mortality rate among patients treated with CPAP/NIV in moderate ARDS was 13.4% (n = 13).
The initiation of NRS at a P/F level between 151 and 200 does not result in a statistically significant difference for in-hospital mortality rate (13.8% group-A, 13.2% group-B, p = 1), OTI rate (6.9% group-A, 11.8% group-B, p = 0.72) and hospitalization length (p = 0.25) as compared to NRS started at a P/F level between 101 and 150 (Table 2). Furthermore, no statistically significant difference emerged between the two groups in pressure (PEEP/PS) used, need for PS or continuous ventilation, nor for ventilation length and days between the start of NRS and OTI or weaning.
Figure 3a, b further show no significant differences in overall survival and OTI rates between patients undergoing NRS at P/F level 151–200 and 101–150.
Above: Kaplan–Meier curves related to the analysis of mortality rates (a) and overall oro-tracheal intubation (OTI, b) among patients undergoing treatment with CPAP/NIV with a P/F between 151 and 200 (group A) and patients who initiated the treatment with a P/F between 101 and 150 (group B). Below: Kaplan–Meier curves related to the analysis of mortality (c) and OTI (d) rates among patients undergone CPAP/NIV in a moderate degree of respiratory distress (group A + B, P/F 101–200) and patients referred for treatment in a severe degree of respiratory distress (group C, P/F ≤ 100)
Baseline characteristics and outcomes of group-B (100 < P/F ≤ 150) vs. group-C (P/F ≤ 100) and patients with moderate (group A + B) versus severe (group-C) ARDS
An analysis was performed on patients initially eligible (development of moderate respiratory distress during hospitalization) but who gave consent to CPAP/NIV treatment only in a severe stage of respiratory distress.
The data obtained in this population (group-C) were compared to those of patients who had started CPAP/NIV at a 100 < P/F ≤ 150 (group-B) and to those obtained from all patients with moderate ARDS (group-A + group-B). Baseline characteristics and outcomes of these populations are summarized in Tables 1 and 2.
The three groups (A + B vs. B vs. C) are comparable for baseline characteristics such as age, gender, CCI and comorbidities (Table 1). Prevalence of chronic obstructive pulmonary disease (COPD) appears significantly higher in moderate ARDS group (group A + B and group B) than in the severe one (group-C). Furthermore, no statistically significant difference emerged at baseline neither for blood tests and gas analysis, nor for radiological severity scores. All group C patients were treated with HFNC before they consent to CPAP/NIV treatment.
All patients were treated with LMWH and steroids; tocilizumab were given in 13.4%, 14.7% and 12.9% in group A + B, B and C respectively (Table 2). A higher statistically significant percentage of remdesivir-treated patients (33% in group A + B, 29.4% in group-B and 9.7% in group-C) was seen in groups with progressively less severe ARDS, consistent with the drug’s datasheet (not indicated in patients on HFNC or mechanical ventilation) [27].
Table 2 shows the outcomes of these populations. In the comparison between group B and C was observed a growing trend for in-hospital mortality, even though not statistically significant, for patients undergoing NRS treatment in severe ARDS (13.2% in group-B vs. 29% in group-C, p = 0.059) (Table 2). Furthermore, patients undergoing NRS treatment in the severe ARDS phase needed more continuous rather intermittent CPAP/NIV (22.1% and 54.8% in group-B and C, respectively—p = 0.002) and PS through conversion from CPAP to NIV (19.1% and 48.4% in group-B and C, respectively—p = 0.002). No statistically significant difference emerged, instead, for pressures (PEEP/PS) required, overall ventilation and hospitalization length or days between the start of NRS and OTI or weaning.
The comparison of combined data of patients undergone NRS in moderate (100 < PF ≤ 200) and severe stage of ARDS (P/F ≤ 100) showed that starting NRS treatment in the severe phase of ARDS is associated to a significant increase in in-hospital mortality as compared to moderate stage (29.0 vs. 13.4%, p = 0.044). On the other hand, the two populations do not disclose any statistically significant difference in OTI rate (12.9% severe group, 10.3% moderate group, p = 0.69). Indeed, severe stage group also shows a statistically significant increase in the median hospitalization length (15 vs. 14 days in moderate group, p = 0.038) and need for continuous ventilation (54.8 vs. 22,7% in moderate group, p = 0.0007) or PS (48.4 vs. 18.6% in moderate group, p = 0.003).
Figure 3 shows overall survival and OTI rate curves of patients underwent CPAP/NIV in these populations. Patients who started NRS in ARDS-moderate stage (Fig. 3c) show a significantly higher survival than patients undergone NRS in a severe stage (p = 0.038). No statistically significant difference emerged in OTI rate (Fig. 3d, p=0.667).
Predictors of CPAP/NIV failure
Potential predictors of CPAP/NIV failure are shown in Table 3. The composite outcome of death and need for OTI is defined as "failure". On univariate analysis, age (HR 1.152; CI 1.084–1.2224, p < 0.001), CCI (HR 1.514; CI 1.274–1.798, p < 0.001), need for conversion to PSV (HR 0.135; CI 0.048–0.3777, p < 0.001) and continuous rather than intermittent ventilation (HR 0.046; CI 0.006–0.355, p = 0.003) found to be significantly associated with CPAP/NIV failure. At multivariate analysis, independent predictors of CPAP/NIV failure were instead advanced age (HR 1.147; CI 1.076–1.2222, p < 0.001) and need for continuous ventilation (HR 0.031; CI 0.003–0.328, p = 0.004).
Discussion
The efficacy of CPAP or NIV in the management of patients with SARS-CoV-2-related ARDS have not been established yet, since the available data are controversial. While some studies reported that patients undergoing CPAP, and then IMV, showed high mortality rates [3, 28], others have demonstrated a positive impact on survival [5,6,7,8,9,10, 29,30,31,32,33]. Our data show a survival rate of 87% (84/97) among patients undergone CPAP/NIV with moderate ARDS and of 83% (106/128) in all populations. Results from our study agree with those recently reported by Brusasco et al. [5], who showed a 94% survival rate in patients with moderate to severe ARDS undergone CPAP.
One of the most important concerns was that NRS could delay IMV those affecting survival rate. Recently, Menzella et al. [8] highlighted that NRS failure resulting in OTI does not lead to excess of mortality as compared to those continuing NIV even with evidence of failure. Perkins et al. [10] confirmed that a trial with CPAP significantly reduces mortality and OTI rate compared to conventional oxygen therapy. In a meta-analysis, the mortality rate among patients undergoing IMV after a trial of NIV seems comparable to that found among patients undergoing primary OTI (48.9% vs. 42.5%, p = 0.08) [9]. Therefore, the meta-analysis demonstrated that risks associated with delayed IMV in SARS-CoV-2-related ARDS are negligible and a CPAP/NIV trial would lead to a reduction of OTI rate. Moreover, mortality rate in patients undergoing IMV seems significantly high, up to 97% during first pandemic waves [4, 9, 11,12,13,14,15,16]. Thus, early use of IMV should be avoided since it could potentially worsen patient’s outcomes and lead to unjustified ICU overload. In this regard, recent Italian guidelines support the use of CPAP/NIV in patients with SARS-CoV-2-related hARF when standard oxygen support seems no longer sufficient, though not requiring immediate OTI [18].
Given that CPAP/NIV is probably effective in treating COVID-19-related ARDS, no data are available about the best timing to start non-invasive treatment that would maximize results and minimize side effects and waste of resources (equipment/dedicated personnel). The Italian guidelines [18] underline the need to define standardized criteria for both initiation and use of CPAP/NIV in COVID-19 patients. Although complications (e.g., pulmonary embolism) may occur in the clinical course of COVID-19 regardless of stage of disease, in the natural history of SARS-CoV-2-related ARDS, respiratory distress severity is usually progressive, but the rate of damage progression is extremely variable [34]. Thus, the most appropriate timing to start treatment during SARS-CoV-2 infection cannot be defined by the days since the onset of the disease, rather by the severity of the clinical picture. In this context, the P/F ratio is the parameter that best expresses the degree of severity of respiratory distress and therefore can be crucial in defining the timing of intervention [20]. All trials evaluating the efficacy of NRS in this setting use extremely heterogeneous and arbitrary cut-offs (P/F ≤ 150, ≤ 200, ≤ 250, ≤ 300) [1, 5, 6, 8, 35], without well-specified criteria to start NRS [3, 9, 29, 31, 32, 35,36,37], affecting results and proposed algorithms.
To our knowledge, our study is the first to evaluate the impact of initiating CPAP/NIV at different levels of respiratory distress severity. In our study, there were no significant differences in outcomes (mortality, OTI rate, hospital days) among patients with moderate respiratory distress who started CPAP/NIV when the P/F was between 151 and 200 compared to patients initiated non-invasive treatment when the P/F was between 101 and 150. Data indicate that starting NRS treatment in the earlier stage of moderate ARDS (group-A) does not significantly reduce in-hospital mortality rates compared to starting treatment in the later stage (group-B, 13.8 vs. 13.2%, p = 1), as well as the need for PS or continuous ventilation, OTI rate and hospitalization length (Table 2). Conversely, this would potentially lead to an increased waste of resources (equipment/dedicated personnel) and a greater and unjustified risk of ventilator-associated lung injury (VILI, potential but not found in our series) or deep vein thrombosis (when helmet is chosen as interface) [24, 38].
Patients who initiated treatment at 100 < P/F ≤ 150 show a clear downward trend in in-hospital mortality compared to patients with a P/F ≤ 100 at NRS starting (13.2% in group-B vs. 29% in group-C, p = 0.059). These data appears to be of clinical relevance even though not statistically significant due to the low sample size. From the analysis of combined data of patients undergone NRS in the moderate ARDS phase (group A + B) or severe (group C) emerged that patients who started the treatment in a severe stage show a statistically significant increase in the mortality rate (29%) comparing to patients treated with CPAP/NIV in a moderate stage (13.4%, p = 0.044, Table 2). Therefore, data suggest that delaying CPAP/NIV in a severe stage of ARDS leads to an unjustified increase in in-hospital and overall mortality rate (Fig. 3c).
On the other hand, our data do not show a significant impact of NRS timing on OTI rate, likely in relation to the low number of cases (Table 2). Indeed, trials focused on the absolute OTI risk during SARS-CoV-2-related hARF showed that CPAP is associated to a reduction in the need for IMV in 35–50% of cases [6, 8, 10, 35]. Oranger et al. showed a higher reduction in the need for OTI (75%) following the use of CPAP [7]. In a recent Italian trial [1], Grieco et al. showed that continuous NIV leads to a reduction in OTI rate compared to HFNC (30% vs. 51%, p = 0.03).
Our findings also underline that the initiation of CPAP/NIV in the moderate ARDS phase significantly reduces the median hospitalization length compared to starting treatment in the severe stage (14 days, group A + B vs. 15 days, group C, respectively; p = 0.038, Table 2) and could help in optimizing the availability of beds, a crucial issue during pandemic. Moreover, starting CPAP/NIV in a severe stage leads to a significantly greater need for PS (due to CPAP failure) and continuous ventilation (> 18 h/day), potentially increasing the risk of VILI and need for total parenteral nutrition, as well as the risk of sepsis and electrolytic disorders. In this regard, the two populations undergone NRS in a moderate stage at a P/F level above or below 150 show the same outcomes, underlying that early CPAP/NIV (P/F > 150) does not positively affect the need for PS or continuous ventilation, as mortality, OTI rate and hospitalization length.
Overall, our findings, consistent with those from the most recent trials [1, 5, 8, 10], suggest that an appropriate use of NRS could reduce in-hospital mortality in SARS-CoV-2 related ARDS [39]. To our knowledge, our study is the first to evaluate the most appropriate timing to initiate non-invasive treatment comparing the efficacy of starting NRS in patients at different severity levels of respiratory distress. The integration of all performed analyzes suggests that starting CPAP/NIV in a moderate ARDS stage (100 < P/F ≤ 200) would allow to optimize outcomes. Although data obtained do not allow definitive conclusions due to small sample size, mortality trend suggests that the best window to start treatment with CPAP/NIV could be probably that of P/F between 100 and 150. Starting NRS treatment in this range could be cost-effective, minimizing on one hand in-hospital mortality rate and hospitalization length (higher for delayed treatments at P/F ≤ 100) and, on the other, the waste of resources in terms of equipment and dedicated personnel, as well as potential VILI (due to similar outcomes for treatment started with a P/F above or below 150). Moreover, advanced age and need for non-invasive continuous ventilation seems to be predictors of CPAP/NIV failure. Assuming the difference in mortality rates between patients underwent NRS at a P/F level between 150 and 100 compared to those underwent treatment in a severe phase of ARDS clinically relevant, although not showing statistical significance, we suggest a possible flow chart for starting NRS treatment in patients with SARS-CoV-2-related ARDS that needs to be validated in future powered studies (Fig. 4).
The main limitation of our research is due to its exploratory study design which does not reach uniformity in the sample size as well as an adequate power because of the small sample size. However, it should be emphasized that no significant differences in baseline parameters were found between our subpopulations. No significant differences emerged for the main risk factors known for adverse outcomes (age and CCI) and comorbidities. For these reasons, we are persuaded that the data can be considered with sufficient confidence.
As reported in the study methods, a sequential ventilatory support has been used (from conventional oxygen to CPAP, to NIV, to OTI). However, if the role of CPAP in the management of ARDS is being defined, to date no strong evidences about the role of NIV are available. As not yet validated, NIV treatment after CPAP failure could be not appropriate and could have affected the results by delaying OTI. For the same reasons, the ventilation pressures used (PEEP, PS) could be arbitrary and, potentially, have influenced the results. A further limitation is that, due to the absence of reference data, an arbitrary P/F cut-off of 150 was chosen in the assessment of the timing to start CPAP/NIV in patients with moderate ARDS. Therefore, it cannot be considered an absolute reference value. However, our data indicate that early treatment with CPAP/NIV in moderate ARDS stage has no significant clinical benefit and exposes the patients to the risks related to ventilation. Thus, for the mentioned reasons, our data must be considered preliminary and confirmed in future studies with adequate power.
Caution is also required about the use of P/F ratio, which seems fundamental in stratification of ARDS severity and in the choice of most appropriate therapies, but it does not represent the only factor to be considered in the evaluation of the outcomes. Hence, a tailored treatment appears mandatory to define the most suitable therapeutic approach in each case. Different pathogenetic mechanisms (e.g.: coagulopathy and pulmonary vascular thrombosis) and different phenotypes of interstitial pneumonia may in fact require diversified therapeutic approaches.
Conclusions
In conclusion, data from this pilot study indicate that starting CPAP/NIV treatment in patients with SARS-CoV-2-related ARDS in moderate stage is associated to a significative reduction of in-hospital mortality and length of hospitalization compared to treatment started in severe stage. It seems likely that the distress severity stage to start CPAP/NIV able to maximize results ranges a P/F between 101 and 150. An earlier start does not lead to significant differences in mortality, OTI rate and hospitalization length, resulting only in waste of resources and potential VILI. Advanced age and the need for continuous ventilation emerged as independent predictors of CPAP/NIV failure. However, the data require confirmation from studies with adequate power.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIFA:
-
Italian drugs agency
- ARDS:
-
Acute respiratory distress syndrome
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- CT:
-
Computed tomography
- DNI:
-
Do not intubate
- FFP:
-
Filtering face-piece
- FiO2 :
-
Delivered oxygen
- GCS:
-
Glasgow coma scale
- hARF:
-
Acute hypoxemic respiratory failure
- HFNC:
-
High flow nasal cannula
- HR:
-
Hazard ratio
- HRCT:
-
High-resolution chest tomography
- ICUs:
-
Intensive care units
- IMV:
-
Invasive mechanical ventilation
- IQR:
-
Interquartile range
- LMWH:
-
Low-molecular weight heparin
- LUS:
-
Lung ultrasound score
- NIV:
-
Non-invasive ventilation
- NRS:
-
Non-invasive respiratory support
- OTI:
-
Oro-tracheal intubation
- PEEP:
-
Positive end-expiratory pressure
- P/F:
-
PaO2/FiO2 rate
- PS:
-
Pressure support
- PSV:
-
Pressure support ventilation
- RR:
-
Respiratory rate
- SD:
-
Standard deviation
- SpO2 :
-
Peripheral oxygen saturation
- TVs:
-
Tidal volumes
- VILI:
-
Ventilator-associated lung injury
References
Grieco DL, Menga LS, Cesarano M, Rosà T, Spadaro S, Bitondo MM, COVID-ICU Gemelli Study Group, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA. 2021;325:1731–43.
Pfeifer M, Ewig S, Voshaar T, Randerath WJ, Bauer T, Geiseler J, et al. Position paper for the state-of-the-art application of respiratory support in patients with COVID-19. Respiration. 2020;99:521–42.
Bertaina M, Nuñez-Gil IJ, Franchin L, Fernández Rozas I, Arroyo-Espliguero R, Viana-Llamas MC, HOPE COVID-19 investigators, et al. Non-invasive ventilation for SARS-CoV-2 acute respiratory failure: a subanalysis from the HOPE COVID-19 registry. Emerg Med J. 2021;38:359–65.
Nightingale R, Lewis J, Monsell KR, Jones L, Smith C, Kundu S, et al. CPAP delivered outside critical care during the second wave of COVID-19: outcomes from a UK respiratory surge unit. BMJ Open Respir Res. 2021;8: e000907.
Brusasco C, Corradi F, Di Domenico A, Raggi F, Timossi G, Santori G, Galliera CPAP-Covid-19 study group, et al. Continuous positive airway pressure in COVID-19 patients with moderate-to-severe respiratory failure. Eur Respir J. 2021;57:2002524.
Aliberti S, Radovanovic D, Billi F, Sotgiu G, Costanzo M, Pilocane T, et al. Helmet CPAP treatment in patients with COVID-19 pneumonia: a multicentre cohort study. Eur Respir J. 2020;56:2001935.
Oranger M, Gonzalez-Bermejo J, Dacosta-Noble P, Llontop C, Guerder A, Trosini-Desert V, et al. Continuous positive airway pressure to avoid intubation in SARS-CoV-2 pneumonia: a two-period retrospective case-control study. Eur Respir J. 2020;56:2001692.
Menzella F, Barbieri C, Fontana M, Scelfo C, Castagnetti C, Ghidoni G, et al. Effectiveness of noninvasive ventilation in COVID-19 related-acute respiratory distress syndrome. Clin Respir J. 2021;15:779–87.
Papoutsi E, Giannakoulis VG, Xourgia E, Routsi C, Kotanidou A, Siempos II. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of non-randomized cohort studies. Crit Care. 2021;25:121.
Perkins GD, Ji C, Connolly BA, Couper K, Lall R, Baillie JK, RECOVERY-RS Collaborators, et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the RECOVERY-RS randomized clinical trial. JAMA. 2022;327:546–58.
Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the seattle region—case series. N Engl J Med. 2020;382:2012–22.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81 (Erratum in: Lancet Respir Med. 2020;8:e26).
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62 (Erratum in: Lancet. 2020;395:1038).
Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, COVID-19 Lombardy ICU Network, et al. Risk factors associated with mortality among patients with covid-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345–55 (Erratum in: JAMA Intern Med. 2021;181:1021).
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, the Northwell COVID-19 Research Consortium, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–9 (Erratum in: JAMA. 2020;323:2098).
Radovanovic D, Santus P, Coppola S, Saad M, Pini S, Giuliani F, et al. Characteristics, outcomes and global trends of respiratory support in patients hospitalized with COVID-19 pneumonia: a scoping review. Minerva Anestesiol. 2021;87:915–26.
Peñuelas O, Del Campo-Albendea L, de Aledo ALG, Añón JM, Rodríguez-Solís C, Mancebo J, et al. Long-term survival of mechanically ventilated patients with severe COVID-19: an observational cohort study. Ann Intensive Care. 2021;11:143.
Bassetti M, Giacobbe DR, Bruzzi P, Barisione E, Centanni S, Castaldo N, Italian Society of Anti-infective Therapy (SITA) and the Italian Society of Pulmonology (SIP), et al. Clinical management of adult patients with COVID-19 outside intensive care units: guidelines from the Italian Society of Anti-Infective Therapy (SITA) and the Italian Society of Pulmonology (SIP). Infect Dis Ther. 2021;10:1837–85.
NICE. Guidance for the role and use of non-invasive respiratory support in adult patients with coronavirus (confirmed or suspected), March 26, 2020. https:/www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/CLEARED_Specialty-guide_-NIV-respiratory-support-and-coronavirus-v2-26-March-003.pdf. Accessed 5 Mar 2022.
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319:698–710.
WHO Recommendations for national SARS-CoV-2 testing strategies and diagnostic capacities. 25 June 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-lab-testing-2021.1-eng. Accessed 5 Mar 2022.
Rouby JJ, Arbelot C, Gao Y, Zhang M, Lv J, An Y, APECHO Study Group, et al. Training for Lung Ultrasound Score Measurement in Critically Ill Patients. Am J Respir Crit Care Med. 2018;198:398–401.
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295:202–7.
Gidaro A, Samartin F, Brambilla AM, Cogliati C, Ingrassia S, Banfi F, et al. Correlation between continuous Positive end-expiratory pressure (PEEP) values and occurrence of Pneumothorax and Pneumomediastinum in SARS-CoV2 patients during non-invasive ventilation with Helmet. Sarcoidosis Vasc Diffuse Lung Dis. 2021;38: e2021017.
Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–300.
National Istitutes of Health (NIH). COVID-19 Treatment Guidelines. October 27, 2021. https://www.covid19treatmentguidelines.nih.gov/about-the-guidelines/. Accessed 5 Mar 2022.
Agenzia Italiana del Farmaco (AIFA). October 21, 2021. https://www.aifa.gov.it/en/web/guest/home. Accessed 5 Mar 2022.
Wendel Garcia PD, Aguirre-Bermeo H, Buehler PK, Alfaro-Farias M, Yuen B, David S, RISC-19-ICU Investigators, et al. Implications of early respiratory support strategies on disease progression in critical COVID-19: a matched subanalysis of the prospective RISC-19-ICU cohort. Crit Care. 2021;25:175.
Forrest IS, Jaladanki SK, Paranjpe I, Glicksberg BS, Nadkarni GN, Do R. Non-invasive ventilation versus mechanical ventilation in hypoxemic patients with COVID-19. Infection. 2021;49:989–97.
Zhou A, Song Q, Peng Y, Deng D, Liao X, Huang P, et al. The effect of noninvasive ventilation support on covid-19 patients and risk factors for invasive ventilation—a retrospective and multicenter study. Int J Gen Med. 2021;14:6085–92.
Vaschetto R, Barone-Adesi F, Racca F, Pissaia C, Maestrone C, Colombo D, et al. Outcomes of COVID-19 patients treated with continuous positive airway pressure outside the intensive care unit. ERJ Open Res. 2021;7:00541–2020.
Coppadoro A, Benini A, Fruscio R, Verga L, Mazzola P, Bellelli G, et al. Helmet CPAP to treat hypoxic pneumonia outside the ICU: an observational study during the COVID-19 outbreak. Crit Care. 2021;25:80.
Cammarota G, Esposito T, Azzolina D, Cosentini R, Menzella F, Aliberti S, et al. Noninvasive respiratory support outside the intensive care unit for acute respiratory failure related to coronavirus-19 disease: a systematic review and meta-analysis. Crit Care. 2021;25:268.
Radovanovic D, Rizzi M, Pini S, Saad M, Chiumello DA, Santus P. Helmet CPAP to Treat Acute Hypoxemic Respiratory Failure in Patients with COVID-19: A Management Strategy Proposal. J Clin Med. 2020;9:1191.
Coppola S, Santus P, Sotgiu G, Mondoni M, Gandola A, Saad M, et al. Feasibility and Clinical Outcomes of a Step Up Noninvasive Respiratory Support Strategy in Patients with Severe COVID-19 Pneumonia. J Clin Med. 2021;10:5444.
Gautret P, Million M, Jarrot PA, Camoin-Jau L, Colson P, Fenollar F, et al. Natural history of COVID-19 and therapeutic options. Expert Rev Clin Immunol. 2020;16:1159–84.
Franco C, Facciolongo N, Tonelli R, Dongilli R, Vianello A, Pisani L, et al. Feasibility and clinical impact of out-of-ICU noninvasive respiratory support in patients with COVID-19-related pneumonia. Eur Respir J. 2020;56:2002130.
Mumoli N, Dentali F, Conte G, Colombo A, Capra R, Porta C, et al. Upper extremity deep vein thrombosis in COVID-19: Incidence and correlated risk factors in a cohort of non-ICU patients. PLoS ONE. 2022;17: e0262522.
Arabi YM, Fowler R, Hayden FG. Critical care management of adults with community-acquired severe respiratory viral infection. Intensive Care Med. 2020;46:315–28.
Acknowledgements
We thank the nursing and health staff for the commitment and expertise that have distinguished them.
Funding
No funding received.
Author information
Authors and Affiliations
Contributions
NR and SS contributed to the study conception and design. Material preparation and data collection were performed by NR, RA, SS, AC, AM, BD, BC, CC, CF, CG, CS, DCM, GK, IS, MG, MLA, NF, PA, RR, RC, RR, RC, SA, SA, SP and VA. Statistical analysis was performed by RA and PPC. The first draft of the manuscript was written by NR. ALE supervised the project, editing the draft and revised the manuscript. CN, CD, CG, MA, RL, RCP and SFC editing the draft and revised the manuscript for important intellectual content. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the University of Campania “L. Vanvitelli”, Naples (n° 10877/2020; approval date: May 6, 2020). All procedures performed in this study were in accordance with the ethics standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethics standards. Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nevola, R., Russo, A., Scuotto, S. et al. Non-invasive respiratory support in SARS-CoV-2 related acute respiratory distress syndrome: when is it most appropriate to start treatment?. Respir Res 23, 327 (2022). https://doi.org/10.1186/s12931-022-02258-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02258-5