Abstract
Background
Polycystic ovary syndrome (PCOS) is often accompanied by increased oxidative stress levels; however, it is still unclear whether PCOS itself is causally related to oxidative stress (OS), whether OS can increase the occurrence of PCOS, and which characteristics of PCOS increase OS levels. Therefore, this study explored the causal relationship between PCOS, its characteristics, and OS.
Methods
Two-sample bidirectional and two-sample Mendelian randomisation studies were performed based on publicly available statistics from genome-wide association studies. PCOS; its characteristics, such as testosterone, low-density lipoprotein, high-density lipoprotein; and 11 major OS markers (superoxide dismutase, glutathione S-transferase, glutathione peroxidase, catalase, uric acid, zinc, tocopherol, ascorbic acid, retinol, albumin, and total bilirubin), were studied. The main analytical method used was inverse variance weighting (IVW). Pleiotropy was evaluated using the Mendelian randomisation-Egger intercept. Q and P values were used to assess heterogeneity.
Results
There was no causal relationship between PCOS and the OS indices (all P > 0.05). There was a causal relationship between the OS index, ascorbate level, and PCOS (IVW, odds ratio: 2.112, 95% confidence interval: 1.257–3.549, P = 0.005). In addition, there was a causal relationship between testosterone, low-density lipoprotein, high-density lipoprotein, sex hormone-binding globulin, body mass index, triacylglycerol, age at menarche, and most OS indices according to the IVW method. The F statistics showed that there was no weak instrumental variable. A sensitivity analysis was performed using the leave-one-out method. No pleiotropy was observed. The results were robust, and the conclusions were reliable.
Conclusions
This study showed for the first time that there was no causal relationship between PCOS and OS. However, there was a causal relationship between the OS index, ascorbate level, and PCOS. It revealed that PCOS itself could not increase OS, and the increase in OS in PCOS was related to other potential factors, such as testosterone, low-density lipoprotein, high-density lipoprotein, sex hormone-binding globulin, body mass index, triacylglycerol, and age at menarche.
Similar content being viewed by others
Background
Oxidative stress (OS) refers to an imbalance between the oxidative and antioxidant systems in the body [1, 2]. Common biomarkers of OS damage include enzymes, such as superoxide dismutase (SOD), glutathione S-transferase (GST), glutathione peroxidase (GPX), and catalase (CAT), and non-enzymes, such as uric acid (UA), zinc, tocopherol, ascorbic acid, retinol, albumin, and total bilirubin (TBIL) [3,4,5]. A balanced OS system is essential for maintaining normal body functions. Increased OS can lead to oocyte ageing and can affect the development of polycystic ovary syndrome (PCOS) and other female reproductive system diseases [6].
PCOS is one of the most common endocrine diseases in women of reproductive age [7]. In PCOS, OS levels are often increased [1, 8]. Serum malondialdehyde (MDA) levels, total oxidant status (TOS) and OS index (OSI) were reported to be higher in patients with PCOS than in the control group. Compared with the non-hyperandrogenism-PCOS subgroup, the hyperandrogenism-PCOS subgroup had higher levels of serum MDA, TOS, and OSI [9, 10], and more severe impairment of the antioxidant function of high-density lipoproteins [11]. Increasing circulating androgen levels can sensitise leukocytes, increase the expression of glucose-induced NADPH oxidase and production of oxidation-active molecules, and promote the occurrence of OS [12, 13]. Compared with non-obese patients with PCOS, patients with obesity and PCOS had higher TOS levels; however, there were no significant differences in OSI and MDA levels [9, 10]. The severity of OS was positively correlated with the hirsutism score, androgen level, blood glucose, and lipid levels [9,10,11].
Several oxidative stress-related enzyme gene variants included platelet-activating factor acetyl hydrolase (PAF-AH) G994→T and paraoxonase (PON) 1 Q192→R, superoxide dismutase 2 (SOD2) V16→A, glutathione peroxidase 1 (GPX1) P198→L, myeloperoxidase (MPO) G-463→A, cytochrome P450 2E1 (CYP2E1) C-1054→T variants are genetic risk factors for PCOS [14,15,16,17,18,19]. The GCLC gene C-129→T variant is a protective factor for the development of hyperandrogenism-PCOS [20]. These studies indicate that patients with PCOS have increased genetic susceptibility to OS and that patients with hyperandrogenism-PCOS have more severe OS than those without hyperandrogenism-PCOS. However, whether PCOS can lead to increased OS and whether OS can increase the occurrence of PCOS remain unknown. Additionally, observational studies often include potential confounding factors and reverse causality; therefore, no clear causal relationship can be obtained [21, 22].
Mendelian randomisation (MR) is an instrumental variable (IV) analysis that detects and quantifies causality using genetic variation as an IV [23]. Because of its ability to overcome potential confounding factors and reverse causality, MR has been increasingly used in observational studies in recent years [24,25,26]. Therefore, this study aimed to clarify the causal association between PCOS, its characteristics, and OS using a two-sample MR study.
Methods
Study design
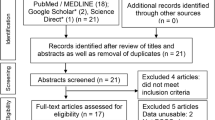
Two-sample MR design was used to detect the causal effects of PCOS and 11 OS injury biomarkers and the characteristic indices of PCOS and 11 OS indices (Fig. 1). It was based on the three hypotheses of MR: (1) Single nucleotide polymorphisms (SNPs) from genome-wide association studies (GWAS) were used as IVs, and the selected IVs were strongly correlated with exposure ; (2) IVs were not associated with confounding factors; (3) IVs affected outcomes (11 OS markers/PCOS/11 OS markers) only by exposure (PCOS/11 OS markers/ characteristic indices of PCOS) [27].
Flow chart of the Two-sample MR study design. Step 1, A two-sample bidirectional Mendelian randomisation study for PCOS and 11 oxidative stress indices; Step 2, Some two-sample Mendelian randomisation studies for characteristics indices of PCOS and 11 oxidative stress indices. IVs, instrumental variables; PCOS, polycystic ovary syndrome; GST, glutathione S-transferase; CAT, catalase; SOD, superoxide dismutase; GPX, glutathione peroxidase; UA, uric acid; SNP, single nucleotide polymorphism;T, testosterone; LDL, low-density lipoprotein; HDL, high-density lipoprotein; SHBG, sex hormone-binding globulin; BMI, body mass index; TAG, triacylglycerol
Selection of GWAS and IVs
The GWAS of PCOS included 10,074 PCOS cases and 103,164 controls, all of whom were of European descent [28]. Fourteen independent SNPs were used according to a previous article [29]. The GWAS sources of 11 OS markers, which consisted of SOD, GST, GPX, CAT, UA, zinc, alpha-tocopherol, ascorbate, retinol, albumin, and TBIL, were used according to the previously published article [30], and the details are shown in Table 1. The participants were of European descent. The criterions of selection of IVs related to exposures were as follows (unless otherwise stated): independent SNPs (r2 < 0.001 and clumping distance > 10,000 kb); P value < 5 × 10− 8; the F statistics of all SNPs included in the MR analysis were evaluated using mRnd (an online tool named, https://shiny.cnsgenomics.com/mRnd/), all the F statistics of the included SNPs were more than 10.
Statistical analysis
Random effects inverse variance weighting (IVW) was used as the main analytical method to evaluate the causal relationships among PCOS, characteristic indices of PCOS, and OS. MR-Egger, weighted median, simple mode, and weighted mode were used to verify the association. Then, the MR-Egger intercept and P values were used to evaluate horizontal and vertical pleiotropy. The MR-Egger and IVW Q and P values were used to evaluate the heterogeneity. Funnel plots were constructed to determine the presence of outlier SNPs. Odds ratios (ORs) and 95% confidence intervals (CIs) were used to express the causal effects of PCOS on the OS injury biomarkers, characteristic indices of PCOS, and OS indices. All analyses were performed using the R software (version 4.2.1) two-sample MR package. A P value of less than 0.05 was considered as evidence of statistically significant causality.
Results
Causal association between PCOS and various OS markers: based on IVW method
As shown in Table 2, PCOS did not show a causal relationship with the 11 OS indices (based on different IVs, OR values, and 95% CI; all P values were > 0.05). Detailed information on PCOS IVs is provided in the Supplementary Materials: PCOS IVs (14SNPs). For alpha-tocopherol, nine SNPs served as IVs because the nine SNPs were found in the outcome (rs2349415, rs2178575, rs11031005, rs1784692, rs1795379, rs13164856, rs2271194, rs9696009, rs804279). For zinc, the nine SNPs (rs2349415, rs2178575, rs1795379,, rs1784692, rs13164856, rs2271194, rs804279, rs11031005, rs9696009) were also found in the outcome. When data of PCOS and zinc was harmonised, rs2271194 and rs804279 were removed as palindromic variants with intermediate allele frequencies. Therefore, seven SNPs served as IVs.
Causal association between PCOS and OS markers: heterogeneity and pleiotropy
As shown in Table 3, there was no pleiotropy according to the MR-Egger intercept and P value. Meanwhile, there was no heterogeneity except for GPX and UA.
Causal association between PCOS and SOD according to five methods
As shown in Table 4, PCOS did not show a causal relationship with SOD according to the five methods. MR sizes for PCOS on SOD, scatter plots, leave-one-out, and funnel plots are shown in Figs. 2, 3 and 4, and 5, respectively.
Causal association between PCOS and GST /GPX /CAT /UA /zinc /alpha-tocopherol /ascorbic acid /retinol /albumin /TBIL according to five methods
PCOS did not show causal relationship with GST (Supplementary Materials: Table S1) /GPX (Table S2) /CAT (Table S3) /UA (Table S4) /zinc (Table S5) / alpha-tocopherol (Table S6) /ascorbic acid (Table S7) /retinol (Table S8) /albumin (Table S9) /TBIL (Table S10) according to five methods. The MR effect size, scatter plot, leave-one-out, and funnel plots are shown in Supplementary Materials Figure S1-4 /S5-8 /S9-12 /S13-16 /S17-20 /S21-24 /S25-28 /S29-32 /S33-36 /S37-40.
Causal association between various OS markers and PCOS
As shown in Table 5, most OS indices did not show a causal relationship with PCOS (based on different IVs, OR values, and 95% CI; all P values were > 0.05), except for tocopherol (MR-Egger, OR: 3.74, 95% CI: 1.297–10.783, P = 0.035) and ascorbate (IVW, OR: 2.112, 95% CI: 1.257–3.549, P = 0.005).
Causal association between various characteristics indices of PCOS and OS markers: based on IVW method
As shown in Table 6, the characteristic indices of PCOS showed a causal relationship with most OS indices (based on different IVs, OR values, and 95% CI; all P values were less than 0.05).
Discussion
To the best of our knowledge, this is the first study exploring the causal effects of polycystic ovary syndrome and characteristic indices of PCOS on OS. In this study, phenotypic GWAS data were analysed using two-sample MR, and no evidence of a causal relationship between PCOS and OS markers was found. However, there was a causal relationship between OS index, ascorbate, and PCOS. This revealed that PCOS itself could not increase OS, ascorbate could increase the occurrence of PCOS, and the increase in the oxidative level of PCOS was related to other potential factors, such as testosterone, low-density lipoprotein, high-density lipoprotein, sex hormone-binding globulin, body mass index, triacylglycerol, and age at menarche, which may act as characteristic indices of PCOS. An observational study has emphasised the association between PCOS and OS [31]. However, relevant MR studies regarding this association are lacking. In addition to observational studies, relevant mechanistic studies have been conducted on OS and PCOS. A study pointed out that OS contributed to insulin resistance in the skeletal muscles of mice with dehydroepiandrosterone-induced PCOS [32]. Salidroside alleviates OS and apoptosis via AMPK/Nrf2 pathway in dihydrotestosterone-induced human granulosa cell line KGN [33].
A meta-analysis has indicated that circulating markers of OS are abnormal in patients with PCOS [1]. OS in patients with PCOS may be associated with several diseases [34, 35]. A few antioxidants can ameliorate PCOS through reducing OS, such as Tempol [36], Kelulut honey [37], Standardised Aronia melanocarpa [38], astaxanthin [39], resveratrol [40], and N-acetyl cysteine [41]. Besides, silibinin [42] and vitamin E supplementation [43] as well as melatonin and/or magnesium supplementation [44] also ameliorate PCOS by reducing the level of OS.
This study included 11 different markers of OS injury, 10 characteristic indices of PCOS, and large-sample PCOS GWAS data from the same race- European ancestor. The proposed method has several advantages. First, it included a two-sample bidirectional MR. Hence, a causal association between OS and PCOS can be proven in reverse. In addition, PCOS itself does not increase OS; therefore, characteristic indices of PCOS were used to explore the causal effects on OS. Some indices related to PCOS characteristics have causal effects on OS. PCOS is a heterogeneous endocrine disorder. Patients with PCOS often present with hyperandrogenemia, glucose and lipid metabolism disorders, obesity, waist-to-hip ratio imbalance, menstrual disorders, ovulation abnormalities, and other symptoms. This study provides evidence for the need to regulate glycaemic and lipid metabolism, control body weight, reduce hyperandrogenemia, and replenish ascorbate and tocopherol in patients with polycystic ovary syndrome, with the aim to reduce the levels of OS or the occurrence of PCOS.
Meanwhile, this study has some limitations. First, GWAS data were obtained from a European ancestor, and whether this conclusion is true for other races needs to be studied. In addition, some analyses used a small number of SNPs (less than 10), and some analyses were not pleiotropic but heterogeneous, such as GPX and UA, which may lead to inaccurate results and compromise confidence. With the continuous update and release of PCOS GWAS data [28, 45,46,47,48], we are likely to overcome these limitations. Finally, the conclusion may be more accurate if the measures of OS included only women.
Conclusions
In summary, this two-sample MR study indicated that genetically predicted PCOS was not significantly associated with oxidative stress; however, the OS index, ascorbate, was significantly associated with PCOS. PCOS itself does not lead to an increase in OS levels, and the increase in OS levels in PCOS is related to other potential factors, such as hyperandrogenism, low-density lipoprotein, high-density lipoprotein, sex hormone-binding globulin, body mass index, triacylglycerol, and age at menarche. It is necessary to regulate glycaemic and lipid metabolism, control body weight, reduce hyperandrogenemia, and replenish ascorbate and tocopherol to reduce the levels of OS or the occurrence of PCOS. Further scientific studies are needed to uncover the mechanisms underlying the increased levels of OS in PCOS.
Data Availability
These oxidative stress injury biomarkers were based on the study-Lu Z, Pu C, Zhang Y, et al. Oxidative Stress and Psychiatric Disorders: Evidence from the Bidirectional Mendelian Randomization Study J. Antioxidants (Basel), 2022, (11). DOI:https://doi.org/10.3390/antiox11071386. Detailed oxidative stress injury biomarkers are shown in Table 1. Detailed information on studies and datasets used in this study. PCOS IVs were based on the study-Zhu T, Cui J, Goodarzi MO. Polycystic Ovary Syndrome and Risk of Type 2 Diabetes, Coronary Heart Disease, and Stroke J. Diabetes, 2021, (70):627 − 37. Doi: https://doi.org/10.2337/db20-0800. Detailed PCOS IVs are shown in Table 1. PCOS SNPs were used to construct the main IV in Europeans.
Abbreviations
- PCOS:
-
Polycystic ovary syndrome
- MR:
-
Mendelian randomisation
- IVW:
-
Inverse variance weighting
- SOD:
-
Superoxide dismutase
- GST:
-
Glutathione S-transferase
- GPX:
-
Glutathione peroxidase
- CAT:
-
Catalase
- UA:
-
Uric acid
- TBIL:
-
Total bilirubin
- SNP:
-
Single nucleotide polymorphism
- IVs:
-
Instrumental variables
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SE:
-
Standard error
- n:
-
Number
- T:
-
Testosterone
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- SHBG:
-
Sex hormone-binding globulin
- BMI:
-
Body mass index
- TAG:
-
Triacylglycerol
- GWAS:
-
Genome-wide association studies
- OS:
-
Oxidative stress
- TOS:
-
Total oxidant status
References
Murri M, Luque-Ramirez M, Insenser M, Ojeda-Ojeda M, Escobar-Morreale HF. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): a systematic review and meta-analysis. Hum Reprod Update. 2013;19(3):268–88.
Al-Gubory KH, Fowler PA, Garrel C. The roles of cellular reactive oxygen species, oxidative stress and antioxidants in pregnancy outcomes. Int J Biochem Cell Biol. 2010;42(10):1634–50.
Poljsak B, Suput D, Milisav I. Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxid Med Cell Longev. 2013;2013:956792.
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39(1):44–84.
Pisoschi AM, Pop A. The role of antioxidants in the chemistry of oxidative stress: a review. Eur J Med Chem. 2015;97:55–74.
Wang L, Tang J, Wang L, Tan F, Song H, Zhou J, Li F. Oxidative stress in oocyte aging and female reproduction. J Cell Physiol. 2021;236(12):7966–83.
Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018;14(5):270–84.
Merhi Z, Kandaraki EA, Diamanti-Kandarakis E. Implications and future perspectives of AGEs in PCOS Pathophysiology. Trends Endocrinol Metab. 2019;30(3):150–62.
Zhang R, Liu H, Bai H, Zhang Y, Liu Q, Guan L, Fan P. Oxidative stress status in chinese women with different clinical phenotypes of polycystic ovary syndrome. Clin Endocrinol (Oxf). 2017;86(1):88–96.
Fan P, Liu H, Wang Y, Zhang F, Bai H. Apolipoprotein E-containing HDL-associated platelet-activating factor acetylhydrolase activities and malondialdehyde concentrations in patients with PCOS. Reprod Biomed Online. 2012;24(2):197–205.
Zhang J, Zhang Y, Liu H, Bai H, Wang Y, Jiang C, Fan P. Antioxidant properties of high-density lipoproteins are impaired in women with polycystic ovary syndrome. Fertil Steril. 2015;103(5):1346–54.
Gonzalez F, Sia CL, Shepard MK, Rote NS, Minium J. Hyperglycemia-induced oxidative stress is independent of excess abdominal adiposity in normal-weight women with polycystic ovary syndrome. Hum Reprod. 2012;27(12):3560–8.
Gonzalez F, Nair KS, Daniels JK, Basal E, Schimke JM, Blair HE. Hyperandrogenism sensitizes leukocytes to hyperglycemia to promote oxidative stress in lean reproductive-age women. J Clin Endocrinol Metab. 2012;97(8):2836–43.
Pu Y, Liu Q, Liu H, Bai H, Huang W, Xi M, Fan P. Association between CYP2E1 C-1054T and 96-bp I/D genetic variations and the risk of polycystic ovary syndrome in chinese women. J Endocrinol Invest 2022.
Ma W, Li S, Liu H, Bai H, Liu Q, Hu K, Guan L, Fan P. Myeloperoxidase and CYBA genetic variants in polycystic ovary syndrome. Eur J Clin Invest. 2021;51(4):e13438.
Sun Y, Li S, Liu H, Gong Y, Bai H, Huang W, Liu Q, Guan L, Fan P. Association of GPx1 P198L and CAT C-262T genetic variations with polycystic ovary syndrome in chinese women. Front Endocrinol (Lausanne). 2019;10:771.
Liu Q, Liu H, Bai H, Huang W, Zhang R, Tan J, Guan L, Fan P. Association of SOD2 A16V and PON2 S311C polymorphisms with polycystic ovary syndrome in chinese women. J Endocrinol Invest. 2019;42(8):909–21.
Wang Y, Liu H, Fan P, Bai H, Zhang J, Zhang F. Evidence for association between paraoxonase 1 gene polymorphisms and polycystic ovarian syndrome in southwest Chinese women. Eur J Endocrinol. 2012;166(5):877–85.
Fan P, Liu HW, Wang XS, Zhang F, Song Q, Li Q, Wu HM, Bai H. Identification of the G994T polymorphism in exon 9 of plasma platelet-activating factor acetylhydrolase gene as a risk factor for polycystic ovary syndrome. Hum Reprod. 2010;25(5):1288–94.
Yang C, Xi M, Liu H, Bai H, Jiang C, Liu Q, Fan P. Association of polymorphisms of Glutamate Cysteine ligase genes GCLC C-129 T and GCLM C-588 T with risk of polycystic ovary syndrome in chinese women. Reprod Sci. 2022;29(6):1790–800.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89–98.
Smith GD, Ebrahim S. Data dredging, bias, or confounding. BMJ. 2002;325(7378):1437–8.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133–63.
Burgess S, Timpson NJ, Ebrahim S, Davey Smith G. Mendelian randomization: where are we now and where are we going? Int J Epidemiol. 2015;44(2):379–88.
Chen H, Ye R, Guo X. Lack of causal association between heart failure and osteoporosis: a mendelian randomization study. BMC Med Genomics. 2022;15(1):232.
Li Z, Chen H, Chen T. Genetic liability to obesity and peptic ulcer disease: a mendelian randomization study. BMC Med Genomics. 2022;15(1):209.
Lawlor DA. Commentary: two-sample mendelian randomization: opportunities and challenges. Int J Epidemiol. 2016;45(3):908–15.
Day F, Karaderi T, Jones MR, Meun C, He C, Drong A, Kraft P, Lin N, Huang H, Broer L, et al. Large-scale genome-wide meta-analysis of polycystic ovary syndrome suggests shared genetic architecture for different diagnosis criteria. PLoS Genet. 2018;14(12):e1007813.
Zhu T, Cui J, Goodarzi MO. Polycystic ovary syndrome and risk of type 2 diabetes, Coronary Heart Disease, and stroke. Diabetes. 2021;70(2):627–37.
Lu Z, Pu C, Zhang Y, Sun Y, Liao Y, Kang Z, Feng X, Yue W. Oxidative stress and Psychiatric Disorders: evidence from the bidirectional mendelian randomization study. Antioxid (Basel) 2022, 11(7).
Uckan K, Demir H, Turan K, Sarikaya E, Demir C. Role of Oxidative Stress in Obese and Nonobese PCOS Patients. Int J Clin Pract 2022, 2022:4579831.
Yao Q, Zou X, Liu S, Wu H, Shen Q, Kang J. Oxidative Stress as a Contributor to Insulin Resistance in the Skeletal Muscles of Mice with Polycystic Ovary Syndrome. Int J Mol Sci 2022, 23(19).
Ji R, Jia FY, Chen X, Wang ZH, Jin WY, Yang J. Salidroside alleviates oxidative stress and apoptosis via AMPK/Nrf2 pathway in DHT-induced human granulosa cell line KGN. Arch Biochem Biophys. 2022;715:109094.
Rudnicka E, Duszewska AM, Kucharski M, Tyczynski P, Smolarczyk R. Oxidative stress in polycystic ovary syndrome (PCOS). Reproduction 2022.
Duica F, Danila CA, Boboc AE, Antoniadis P, Condrat CE, Onciul S, Suciu N, Cretoiu SM, Varlas VN, Cretoiu D. Impact of increased oxidative stress on Cardiovascular Diseases in Women with Polycystic Ovary Syndrome. Front Endocrinol (Lausanne). 2021;12:614679.
Li T, Zhang T, Gao H, Liu R, Gu M, Yang Y, Cui T, Lu Z, Yin C. Tempol ameliorates polycystic ovary syndrome through attenuating intestinal oxidative stress and modulating of gut microbiota composition-serum metabolites interaction. Redox Biol. 2021;41:101886.
Kamal DAM, Ibrahim SF, Ugusman A, Mokhtar MH. Kelulut Honey ameliorates Oestrus cycle, hormonal profiles, and oxidative stress in Letrozole-Induced polycystic ovary syndrome rats. Antioxid (Basel) 2022, 11(10).
Rudic J, Jakovljevic V, Jovic N, Nikolic M, Sretenovic J, Mitrovic S, Bolevich S, Bolevich S, Mitrovic M, Raicevic S et al. Antioxidative Effects of standardized Aronia melanocarpa extract on Reproductive and metabolic disturbances in a rat model of polycystic ovary syndrome. Antioxid (Basel) 2022, 11(6).
Gharaei R, Alyasin A, Mahdavinezhad F, Samadian E, Ashrafnezhad Z, Amidi F. Randomized controlled trial of astaxanthin impacts on antioxidant status and assisted reproductive technology outcomes in women with polycystic ovarian syndrome. J Assist Reprod Genet. 2022;39(4):995–1008.
Karimi A, Tutunchi H, Naeini F, Vajdi M, Mobasseri M, Najafipour F. The therapeutic effects and mechanisms of action of resveratrol on polycystic ovary syndrome: a comprehensive systematic review of clinical, animal and in vitro studies. Clin Exp Pharmacol Physiol. 2022;49(9):935–49.
Kose SA, Naziroglu M. N-acetyl cysteine reduces oxidative toxicity, apoptosis, and calcium entry through TRPV1 channels in the neutrophils of patients with polycystic ovary syndrome. Free Radic Res. 2015;49(3):338–46.
Marouf BH, Ismaeel DO, Hassan AH, Ali OJ. Therapeutic Effects of Silibinin Against Polycystic Ovary Syndrome Induced by Letrozole in rats via its potential anti-inflammatory and anti-oxidant activities. J Inflamm Res. 2022;15:5185–99.
Tefagh G, Payab M, Qorbani M, Sharifi F, Sharifi Y, Ebrahimnegad Shirvani MS, Pourghazi F, Atlasi R, Shadman Z, Rezaei N, et al. Effect of vitamin E supplementation on cardiometabolic risk factors, inflammatory and oxidative markers and hormonal functions in PCOS (polycystic ovary syndrome): a systematic review and meta-analysis. Sci Rep. 2022;12(1):5770.
Mousavi R, Alizadeh M, Asghari Jafarabadi M, Heidari L, Nikbakht R, Babaahmadi Rezaei H, Karandish M. Effects of Melatonin and/or magnesium supplementation on biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome: a Randomized, Double-Blind, placebo-controlled trial. Biol Trace Elem Res. 2022;200(3):1010–9.
Chen ZJ, Zhao H, He L, Shi Y, Qin Y, Shi Y, Li Z, You L, Zhao J, Liu J, et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat Genet. 2011;43(1):55–9.
Shi Y, Zhao H, Shi Y, Cao Y, Yang D, Li Z, Zhang B, Liang X, Li T, Chen J, et al. Genome-wide association study identifies eight new risk loci for polycystic ovary syndrome. Nat Genet. 2012;44(9):1020–5.
Day FR, Hinds DA, Tung JY, Stolk L, Styrkarsdottir U, Saxena R, Bjonnes A, Broer L, Dunger DB, Halldorsson BV, et al. Causal mechanisms and balancing selection inferred from genetic associations with polycystic ovary syndrome. Nat Commun. 2015;6:8464.
Hayes MG, Urbanek M, Ehrmann DA, Armstrong LL, Lee JY, Sisk R, Karaderi T, Barber TM, McCarthy MI, Franks S, et al. Genome-wide association of polycystic ovary syndrome implicates alterations in gonadotropin secretion in european ancestry populations. Nat Commun. 2015;6:7502.
Acknowledgements
The author thanks Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, validation, writing and editing were finished by Pu Y f. The author has read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable. Ethical approval and informed consent for studies included in the analyses were provided in the original publications.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yifu, P. Evidence for causal effects of polycystic ovary syndrome on oxidative stress: a two-sample mendelian randomisation study. BMC Med Genomics 16, 141 (2023). https://doi.org/10.1186/s12920-023-01581-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-023-01581-0