Abstract
Background
Mannheimia haemolytica is commonly associated with respiratory disease in cattle worldwide as a cause of fibrinous pneumonia, bronchopneumonia and pleuritis. M. haemolytica is further subdivided into 12 serovars, however not all are considered to be pathogenic in cattle. The study aim was to determine the most common serovars of M. haemolytica associated with respiratory disease in cattle in Great Britain, which is currently unknown and could be useful information for clinicians when considering preventative strategies.
Results
One hundred four M. haemolytica isolates isolated from bovine clinical pathology and post-mortem samples from pneumonia cases between 2016 and 2018 were tested using a multiplex PCR assay to identify M. haemolytica serovars A1, A2 and A6. 46 isolates (44.2%) typed as M. haemolytica serovar A1, 31 (29.8%) as M. haemolytica serovar A2 and 18 isolates (17.3%) as M. haemolytica serovar A6. Nine isolates (8.7%) were not A1, A2 or A6 so were considered to belong to other serovars or were not typable.
Conclusion
This study highlights the importance of M. haemolytica serovars other than A1 which may be responsible for respiratory disease in cattle and could help guide the veterinarian when making choices on preventative vaccination programmes.
Similar content being viewed by others
Background
Mannheimia haemolytica is associated with respiratory disease in cattle and sheep worldwide. The organism can be a primary component of pneumonia secondary to environmental stressors as well as infecting cattle synergistically with other bacterial, viral and Mycoplasma species [1].
There are twelve serovars of M. haemolytica, based on capsular antigens and labelled A1, A2, A5, A6, A7, A8, A9, A12, A13, A14, A16 and A17. A further serovar, A11, is restricted to M. glucosida [2, 3].
M. haemolytica serovars A1, A2 and A6 are the most prevalent worldwide [4] and are readily isolated from the nasopharynx of healthy cattle. Serovars A1 and A6 have been reported as common isolates from pneumonic lung tissue [5], serovar A2 is a major cause of disease in sheep [6] and has traditionally been considered as a commensal organism in cattle; however, a recent review paper highlighted some evidence to suggest this serovar may not be purely commensal in this species [7].
Several vaccines are licenced in Great Britain for protection against M. haemolytica but not all vaccines cover serovars A1 and A6. Reviews of the common serovars of M. haemolytica associated with respiratory disease can inform pharmaceutical companies on serovars required for inclusion in vaccines and to help veterinary surgeons make informed decisions on vaccine choice.
A multiplex PCR assay can provide a rapid, simple and cost-effective alternative to slide agglutination assays currently used for M. haemolytica serotyping and avoids the need to use laboratory animals for serotyping assays. We validated a PCR test for the most prevalent serovars of M. haemolytica in cattle based on the test development and primers described by Klima et al. [8]. We used this test to investigate the prevalence of each of these serovars amongst M. haemolytica isolates cultured from diagnostic material from bovine respiratory disease submitted to SRUC Veterinary Service laboratories in the years 2016–2018.
Results
The results of specificity testing of the M. haemolytica PCR assay confirmed that all M. haemolytica serovar A1, A2 and A6 strains were correctly identified. All confirmed non-M. haemolytica strains were negative using the M. haemolytica PCR assay.
The largest proportion of isolates (44.2%) typed as M. haemolytica serovar A1, 29.8% typed as M. haemolytica serovar A2 and 17.3% typed as A6. Nine isolates (8.7%) were not A1, A2 or A6 so were considered to belong to other serovars or were not typable (Table 1).
Discussion
The work presented here demonstrates that a multiplex PCR assay incorporating three serotype specific primer pairs for identification of M. haemolytica serovars A1, A2 and A6 is an effective test for typing isolates of these serovars. The test validation against known serovars and isolates showed that all confirmed M. haemolytica serovar A1, A2 and A6 strains were correctly identified using the M. haemolytica PCR assay. All confirmed other strains of M. haemolytica were negative using the M. haemolytica PCR assay.
The 104 M. haemolytica isolates tested were selected through scanning surveillance which does not allow general population conclusions to be drawn from any sample set that is collected in this way. One other source of bias was that a single colony isolate was selected from each case. However, the testing does confirm that M. haemolytica serovar A1 was identified most commonly and serovar A6 least commonly. A more structured survey would be required to estimate the relative prevalence of these different strains generally in the cattle population and in cases of respiratory disease.
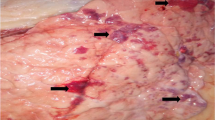
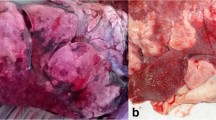
The finding that M. haemolytica serovar A1 is the most common serovar in this set of British isolates is consistent with other studies of European isolates [9]. A large proportion of respiratory samples typed as serovar A2, moreover 97% of the M. haemolytica serovar A2 isolates were isolated from pneumonic lung tissue with gross pathology consistent with bacterial pneumonia. Histopathology was carried out on 40% of the cases and this detailed examination confirmed lesions consistent with bacterial bronchopneumonia. This serovar has previously been reported as a commensal organism in North America, however a more recent review paper stated, ‘the commonly accepted idea that M. haemolytica A2 isolates are primarily non-pathogenic bacteria associated with healthy cattle should be considered with caution’ [7]. Therefore, more research is required to understand the contribution of this serovar to the bovine respiratory disease complex.
Not all vaccines against M. haemolytica cover all the major serovars and studies of this nature may be of assistance in the selection of the appropriate bovine respiratory disease vaccination programme.
Conclusion
M. haemolytica serovars A1 and A6 were commonly isolated from cases of bovine respiratory disease in this study, mirroring similar research in other countries. A large proportion of clinical samples typed as serovar A2, however more work is required to fully understand the contribution of this serovar to the bovine respiratory disease complex. These results could help veterinarians select the appropriate preventative vaccination programme when pneumonia attributed to M. haemolytica is diagnosed on UK cattle farms.
Methods
A multiplex PCR was validated for this study using three serotype specific primer pairs for identification of M. haemolytica serovars A1, A2 and A6 based on published work [8]. DNA was extracted and amplified using standard techniques and the serotype specific primers. PCR amplification was performed using a conventional thermal cycler and reaction products were separated by electrophoresis on a 2% agarose gel. Images of the gel were captured and analysed on an Image Lab 4.0 Image Analysis system. Negative and positive controls were included in each run with the positive controls comprising DNA extracts of each M. haemolytica serovar 1, 2 and 6. Identification of M. haemolytica serovars in clinical isolates was determined by comparing PCR amplification product band sizes with those in the positive PCR control lanes (M. haemolytica serovars A1, A2 and A6) of the analysed gel.
Specificity of the M. haemolytica PCR assay was determined by testing panels of known M. haemolytica serovars (A1, A2 and A6), un-typed M. haemolytica strains and closely related strains including Bibersteinia trehalosi, Pasteurella multocida, Mannheimia glucosida, Mannheimia varigena and Mannheimia granulomatis.
The sample set comprised material received from one hundred and four cases or disease outbreaks with a clinical history of respiratory disease occurring between 2016 and 2018, each defined as a submission. All submissions produced an isolate of M. haemolytica and only one isolate per submission and per affected farm was included in the study. Submission selection was not random but was selected as a representative sample from the overall number of submissions of respiratory disease cases to the SRUC laboratories between 2016 and 2018 to give as wide a UK distribution as possible and be representative of farm type (dairy or beef), animal breed, age, and sex.
The sample set included a mixture of breeds and cross-bred animals derived from 70 animals on beef units, 25 animals on dairy units and no data was available for 9 samples. Where the gender of the animal was recorded, 41 animals were female and 41 were male. The age range of the animals from which samples were derived was from 1 day to 8 years old with 46 animals 0–3 months old, 19 animals > 3 months and < 6 months old, 16 animals 6 months – 2 years old, 5 animals > 2 years old and 18 animals where the age was not available. Results were obtained from animals throughout the Great Britain, 22 from England, 4 from Wales and 78 from Scotland.
Sample type comprised nasopharyngeal swabs (17 cases), broncho-alveolar lavage fluid (2 cases) submitted by veterinary practitioners and post-mortem material (85 cases). Bovine carcases submitted to SRUC Veterinary Services post-mortem rooms by livestock keepers were examined for the presence of visible lesions of pneumonia and affected lung was then sampled for bacterial culture. For all sample types, primary bacterial cultures were made on Columbia sheep blood agar (CSBA) (Thermo-Fisher, Perth, UK), following 18–24 h incubation at 37 °C in capnophilic conditions. Identification was confirmed using routine phenotypic tests and isolates were stored at − 80 °C in Microbank® cryovials (Prolab Diagnostics, Wirral, UK). The pathogenic significance of the isolates was assessed by clinical history and the pathology seen thus providing an accurate representation of 104 M. haemolytica isolates of clinical significance.
M. haemolytica isolates derived from the above submissions were revived by culture on CSBA for testing in the PCR assay.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- M. haemolytica :
-
Mannheimia Haemolytica
- PCR:
-
Polymerase Chain Reaction
- SRUC:
-
Scottish Rural College
- CSBA:
-
Columbia Sheep Blood Agar
References
Rice JA, Carrasco-Medina L, Hodgins DC, Shewen PE. Mannheimia haemolytica and bovine respiratory disease. Anim Health Res Rev. 2008;8:117–28.
Angen Ø, Mutters R, Caugant DA, Olsen JE, Bisguard M. Taxonomic relationships of the (Pasteurella haemolytica) complex as evaluated by DNA-DNA hybridizations and 16S rRNA sequencing with proposal of Mannheimia haemolytica gen. Nov., comb. nov., Mannheimia granulomatis sp. nov., Mannheimia glucosida sp. nov., Mannheimia ruminalis sp. nov., and Mannheimia varigena sp. nov. Int J Syst Bacteriol. 1999;49:67–86.
Blackall PJ, Bojesen AM, Christensen H, Bisguaard M. Reclassification of (Pasteurella trehalosi) as Bibersteinia trehalosi. Int J Syst Evol Microbiol. 2007;57:666–74.
Al-Ghamdi GM, Ames TR, Baker JC, Walker R, Chase CCL, Frank GH, et al. Serotyping of Mannheimia (Pasteurella) haemolytica isolates from the upper Midwest United States. J Vet Diag Invest. 2000;12:576–8.
Klima CL, Alexander TW, Hendrick S, McAllister TA. Characterization of Mannheimia haemolytica isolated from feedlot cattle that were healthy or treated for bovine respiratory disease. Can J Vet Res. 2014;78:38–45.
Fodor L, Varga J, Hajtos I, Szemeredi GY. Serotypes of Pasteurella haemolytica isolated from sheep, goats and calves. Zoonoses Public Health. 1984;31:466–9.
Arnal JL, Fernández A, Vela AI, Sanz C, Fernández-Garyzábal JF. Capsular type diversity of Mannheimia haemolytica determined by multiplex real-time PCR and indirect hemagglutination in clinical isolates from cattle, sheep, and goats in Spain. Vet Microbiol. 2021;258:109121.
Klima CL, Zaheer R, Briggs RE, McAllister TA. A multiplex PCR assay for molecular capsular serotyping of Mannheimia haemolytica serotypes 1, 2, and 6. J Microbiol Methods. 2007;139:155–60.
Andrés-Lasheras S, Zaheer R, Klima C, Sanderson H, Polo RO, Milani MRM, et al. Serotyping and antimicrobial resistance of Mannheimia haemolytica strains from European cattle with bovine respiratory disease. Res in Vet Sci. 2019;124:10–2.
Acknowledgements
The M. haemolytica isolates used in this work originated from samples submitted by veterinary practices as part of the Scottish Government funded veterinary surveillance programme. The help of the submitting veterinary surgeons and their farmer clients is acknowledged.
Funding
This work was funded by MSD Animal Health UK. The funding covered the time for the SRUC laboratory technicians to undertake development of the laboratory test required by this work and the sample testing and analysis. The funding also covered time taken for SRUC staff to produce a written report of the results. The funding body had a minor contribution to the design of the study (specifying the inclusion of serovars A1, A2 and A6) and no contribution, other than funding as described above, to collection, analysis, and interpretation of data. KBS, an author employed by the funding body, contributed to writing the manuscript.
Author information
Authors and Affiliations
Contributions
Authors CM, JE, GF, JT and OG are employees of SRUC and worked together on development of the laboratory test, recruiting, and testing the samples and analysing the results. Authors CM and KBS produced the draft manuscript and all authors contributed to, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This paper refers to testing of samples of M haemolytica isolates from cattle pneumonia cases that were previously collected by the Scottish Rural College (SRUC) staff during disease surveillance work, where consent for using the samples for research purposes was given. This study was approved by SRUC’s Animal Ethical Review Body (AWERB).
Consent for publication
Not applicable.
Competing interests
Author KBS is an employee of MSD Animal Health, the funding body of this study. The other authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mason, C., Errington, J., Foster, G. et al. Mannheimia haemolytica serovars associated with respiratory disease in cattle in Great Britain. BMC Vet Res 18, 5 (2022). https://doi.org/10.1186/s12917-021-03121-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-021-03121-3