Abstract
Background
The Kin-Antwerp project aimed at improving the quality of care provided to patients with diabetes in Kinshasa, the Democratic Republic of the Congo in Central Africa, including the digitalisation of routine clinical data to improve patients’ follow-up. We aim to analyse the data of a study population of Kin-Antwerp to characterise their demographic features, assess their achievement of glycemic target over time, and identify groups requiring prioritised attention.
Methods
We performed a secondary database analysis of routinely collected information from primary care patients with type 2 diabetes followed from 1991 to 2019. Data included demographics (age, sex), anthropometrics (weight, height), clinical parameters (blood pressure, plasma glucose), and anti-diabetic treatments. Achievement of glycemic target, defined as fasting plasma glucose < 126 mg/dL, over time was assessed using a multilevel mixed-effects logistic regression model.
Results
Our study population of patients with type 2 diabetes (N = 8976) comprised a higher proportion of women (67%) and patients between 40 and 65 years old (70.4%). At the first follow-up, most patients were on treatment with insulin (56.5%) and had glycemic levels under the target (79.9%). Women presented more often with obesity (27.4%) and high systolic blood pressure (41.8%) than men (8.6% and 37.0%, respectively). Patients had a median follow-up of 1.8 (interquartile range: 0.5–3.4) years. Overall, the odds of achieving glycemic target increased by 18.4% (odds ratio: 1.184, 95% CI: 1.130 to 1.239; p < 0.001) per year of follow-up. Stratified analyses suggested that the odds of achieving glycemic control over time increased among older patients (> 40 years), but not among younger patients (< 40 years).
Conclusion
In our study population, an overall poor glycemic control was observed albeit with a modest improvement in the achievement of glycemic target throughout patients’ follow-up. Younger patients may benefit from prioritised attention to achieve glycemic targets. Based on the information provided by the database, continue monitoring and improvement of the project Kin-Antwerp is recommended. Introducing further efforts to improve type 2 diabetes management should include robust glycemia-monitoring tools and haemoglobin A1c, as well as further outlining self-management strategies.
Similar content being viewed by others
Background
Diabetes is a leading cause of morbidity and mortality and one of the major constraints to health systems worldwide [1, 2]. In 2019, the International Diabetes Federation (IDF) reported a global prevalence of diabetes of 9.3% for the adult population (18–79 years) [3]. This reported prevalence is greater in high-income (10.4%) than middle- (9.5%) and low- (4.0%) income countries, however, these numbers are expected to rise rapidly among those in the latter regions where economies are generally moving towards improvement [3]. In Africa, the prevalence of type 2 diabetes (T2D) has been increasing rapidly and is predicted to continue, likely driven by the increases in body weight and adiposity [4] as a consequence of unhealthy lifestyles, rapid urbanisation, and overall population ageing [5]. Estimations from 1980 to 2014 for the entire African continent have reported an increase in the prevalence of T2D of more than double for both women (4.1 to 8.9%) and men (3.4 to 8.5%) [4] and such increases being associated with the growing rates of obesity [6]. These estimates are, however, based on limited population-based data, as health data remain scarce in several low- and middle-income countries (LMICs) in Africa, particularly in those in sub-Saharan Africa (SSA) [7, 8]. This shortcoming has likely resulted in an underestimating of the burden of T2D across this region. In the Democratic Republic of the Congo (DRC), the IDF has estimated an age-adjusted prevalence of diabetes of 6% for adults (20-79 years) [3]. However, studies conducted in specific populations, such as mining workers in DRC, has reported a much higher prevalence of 11.9% [9].
Previous evidence from different African countries has reported an overall poor glycemic control (haemoglobin A1c (HbA1c) ≥ 7% and fasting plasma glucose (FPG) ≥ 126 mg/dL) in patients with T2D [10,11,12]. Moreover, it has been described that the sub-optimal management of T2D in LMICs is often related to the limited accessibility and availability of anti-diabetic drugs, and fragmented delivery of chronic care [13].
To address these concerns, availability and access to health data in DRC and improve the quality of care, international projects like Kin-Antwerp, a collaboration between the Institute of Tropical Medicine Antwerp (ITM), Memisa (Belgian NGO with representation in DRC), and Centre d’éducation diabète & Santé in Kinshasa, started in 2010. This project aimed at supporting the ongoing DRC Diabetes National Programme to improve health services and provide a closer follow-up to patients with T2D by centralising data collection. The latter focused on the digitalisation of routine clinical data collected during follow-up visits through the development of a software database. Thus, the primary aims of this study are to describe the demographic characteristics of a study population of patients with T2D of Kin-Antwerp, assess their overall achievement of glycemic target over the years of follow-up, and identify potential subgroups, based on sex and age, that may require prioritised attention. Through this, we also aim at providing an insight into the effectiveness of the project Kin-Antwerp. This study is an exploratory analysis; therefore, no pre-specified hypotheses were investigated.
Methods
Design
This research is a secondary database study of routine data collected from patients with T2D attending primary care and followed from 1991 to 2019. This research was approved by the Institutional Review Board of the Institute of Tropical Medicine Antwerp in Belgium (IRB/RR/ac/149) and the Ethical Committee of the University of Kinshasa in DRC (ESP/CE/153B/2021). This study was guided by the Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement [14], an extension from STROBE, The Strengthening the Reporting of Observational Studies in Epidemiology, guideline [15].
Setting
According to information and data from the World Bank in 2020, DRC is the largest country of SSA with approximately 89,561,404 million inhabitants and has a gross domestic product (GDP) annual growth of 1.7% [16, 17]. In 2018, it was estimated that DRC has one of the largest populations living in poverty, precisely the third one globally, as approximately 73% of the population lives with less than $1.90 a day [18].
In 2015, the World Health Organization (WHO) has described that DRC has a 3-level health system organisation: the implementation level, each district in DRC has a network of several health centres and district hospitals; the intermediate level focuses on the technical and logistic support and is mainly managed by provincial health departments; the central level has the normative responsibility [19]. Between 2008 and 2012, the health expenditures in DRC were rather low, $12–13 per capita per year [19]. A large part of the challenges of the health system in DRC originates in the political situation of three decades of non-governance resulting in the collapse of the state and economy [19].
In the big capital city of DRC, Kinshasa, adults seek medical help close to their homes when health complaints are present. During medical check-ups at primary health facilities, screening for T2D is typically done through medical history, clinical parameters (e.g. blood pressure and blood glucose) and anthropometric measurements such as body weight and height. When blood glucose is abnormal (random glucose test of > 200 mg/dL or FPG > 126 mg/dL) and/or diabetes-related symptoms are present, for instance, polyuria, polyphagia, or polydipsia, extreme fatigue or blurred vision, patients are referred, in most of the cases, to the endocrinology department of the hospital for further testing. After the diagnosis of T2D is confirmed and the physician has selected the most appropriate treatment, the national standard form for patients with T2D is completed. Developed by the Diabetes National Programme, this paper-based form collects the diabetes history of the patient, demographic details, diagnosis status, clinical evaluation, and anti-diabetic treatment records. Diagnosis of T2D is carried out by a doctor at the hospital or by a nurse at the primary health centres. If the diagnosis was performed at the hospital, from the moment the patient’s glycemia is stable, the continuation of treatment and care is decentralised to the primary health centres.
In Kinshasa, T2D care is often offered by Kin Réseau, a network initiative, which was set up in 1974 by mostly religious organisations, aiming at providing decentralised care for diabetes. This longstanding network, comprises 80 care centres, including hospitals and primary health centres, and has a patient referral system in place. This programme also offers patient education, medication for a subsidised price, and daily insulin administration at the health centre, as well as annual screening for complications of diabetes. More details on this programme can be found elsewhere [20]. Currently, Kin Réseau offers a basic diabetes package that includes one follow-up visit a week at the health centre and a bi-monthly medical examination by a trained doctor for a price of USD 3.5/month.
Data sources
The Kin Réseau network often provides T2D care by offering medical packages. The T2D care package includes disease follow-up visits in which routine measurements such as weight, blood pressure, and foot examinations are assessed. Glycemic control is monitored by measuring FPG. Based on clinical assessment and test results, the physician decides on treatment adjustments. Patients are encouraged to achieve glycemic targets recommended by the IDF of HbA1c < 7.0 % and its equivalent of FPG < 126 mg/dL [21]. The routine data gathered through these visits is collected in a paper-based follow-up form used systematically across DRC (additional file, Image S1). These forms have been collected and stored by the Centre d’éducation diabète & santé covering the years between 1991 and 2019. In the context of Kin-Antwerp’s main objective, supporting Kin Réseau in improving the quality of care and a better follow-up of patients, a database software was developed by the ITM in collaboration with staff from Memisa and the Centre d’éducation diabète & santé. After its development, staff from both Congolese institutions were trained on the use of the database and data entry and, throughout the years, the database has evolved based on data quality controls. Currently, the established electronic database is an independent effort from the Centre d’éducation diabète & santé and is limited to the information collected in the follow-up form (Image S1) of patients with T2D. Paper-based forms with information collected at 6-month follow-up visits, as this cut-off was set to indicate if a patient has not attended for disease follow-up, of patients with T2D have been entered retrospectively into the database from the latest forms received in 2019. Currently, the database contains information on approximately 13,000 patients. Data were checked for missingness and accuracy. Data-cleaning processes were carried out before the analyses and included removing irrelevant data, standardising terms and fixing typing errors, and converting data types. This study did not include any data linkage.
Study population and variables
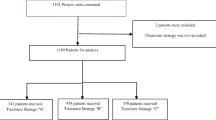
Kin-Antwerp gathers information from 65 health centres across Kinshasa, out of which 32 centres had updated information on patients with T2D. For this study, code was developed to retrieve information based on the following eligibility criteria. Data on adults (≥ 18 years old) diagnosed with T2D were included (N = 9700; 41,353 observations). Patients’ information was excluded if any of the following variables were not available at the first visit: date of the visit (0.3%), sex (0.0%), glycemic value (1.9%), and treatment (7.8%) leaving information for a total of 8976 patients with multiple follow-up visits representing 37,548 observations. The index date was defined as the date of the first prescription of anti-diabetic medication for a patient meeting the inclusion and exclusion criteria in the database.
Demographic and clinical information described in the database included sex, age, and values at each follow-up visit for weight and height (the latter only at the first visit), and the clinical parameters of systolic and diastolic blood pressure (SBP, DBP; in mmHg) and FPG (mg/dL). Weight was measured in kilogrammes with a digital or mechanical scale placed on a firm and flat surface. Height was assessed using a measuring board positioned against a wall and taken in centimetres. For both measurements, weight and height, standard guidelines developed by each health centre in collaboration with the Centre d’éducation diabète et santé were followed. BMI was calculated as body weight in kilogrammes divided by height in metres squared and classified based on the WHO classification of adults (normal: BMI < 25 kg/m2; overweight: BMI ≥ 25 – < 30 kg/m2; obesity: BMI ≥ 30 kg/m2) [22]. SBP and DBP were measured using either a digital automatic blood pressure monitor or a sphygmomanometer, depending on the resources of the health centre. FPG was measured by pricking the skin with a lancet to obtain a drop of blood which is placed on a disposable test strip, followed by inserting it in the glucometer to estimate the glycemia in blood.
In this study, the operational definition of T2D relies on the physician’s written diagnosis by which patients were referred for follow-up in primary care centres using the standard national forms developed by the National Programme of Diabetes in DRC. Our primary outcome is the odds/probabilities of achieving glycemic target defined as FPG < 126 mg/dL. All available FPG values per patient were used to estimate the achievement of the glycemic target. Secondary outcomes entailed identifying demographic characteristics (sex and age) that could potentially influence the odds/probabilities of achieving glycemic target.
Statistical analysis
All analyses were conducted using STATA (Release 16/SE. College Station, TX: StataCorp LP). Demographic characteristics were reported as measures of central tendency for continuous data, mean ± standard deviation (SD) and medians and interquartile range (IQR) if not normally distributed, and counts and percentages for categorical variables. To assess the achievement of glycemic target (FPG < 126 mg/dL) over the years of follow-up, a multilevel mixed-effects logistic model (command melogit) was conducted. To account for patients nested within health centres, a random intercept was added for the health centres and to consider repeated measurements, we fitted a random intercept at the patient level and a random slope of the variable representing years of follow-up varying by patient. The results of this model are expressed as odds ratios (OR) and 95% confidence intervals (95% CI) and are conditional to the random effects. From this model, we derived probabilities by predicting the average marginal effects (AME) (command margins) and illustrated the average marginal effects at specific time points. AME indicates the average change in the probability, in this case, glycemic control, when x, years of follow-up, increases by one unit. We adjusted our model at baseline (first visit of follow-up) for sex, age categories (< 40 years, 40-65 years, > 65 years), BMI (normal, overweight, obesity), SBP (normal, elevated), treatment (oral glucose lowering drugs (OGLDs), insulin, insulin + OGLDs, or diet), and interactions between the years of follow-up and the mentioned covariates. These interactions are referred to as time interactions in the manuscript. We assumed the missingness mechanism was ‘missing at random’. Missing values in the covariates of the model were handled by listwise deletion in a long format, while a direct likelihood approach dealt with missing values in the outcome (i.e. the default strategy for regressions in STATA). To identify subgroups of patients that may do worse in terms of achieving the glycemic target, exploratory stratification models for sex and age categories were carried out. A p-value < 0.05 was considered statistically significant for the main model and a p-value < 0.008 for the stratified exploratory analyses after applying Bonferroni correction for multiple comparisons. As part of our objective was to assess the achievement of glycemic target, measured as odds/probabilities, over the years of follow-up, we chose a multilevel mixed-effects logistic regression, with random intercept and slope as this model allows for patient’s observations to be analysed as a cluster, hence allowing each participant to have its own starting point (intercept) and time of follow-up (slope). We favoured this approach in comparison to a survival analysis which implies selecting an event (achieving glycemic target) at a specific time, for example, time to the first or the last event. A mixed-effects logistic regression accounts for repeated evaluations of glycemic target over the follow-up time, reflecting what has happened in real practice, and taking into account the potential correlation between them, aside from also allowing adjusting the estimate for relevant covariates.
Results
The demographics and clinical characteristics of the study population at the first follow-up visit are presented in Table 1. Of a total of 8976 patients (Fig. 1) with T2D, 67% were women and 33% were men with an average age of 55.2 ± 11.3 years old. Most of the patients were diagnosed with T2D 5 to 10 years ago (49.1%), followed by patients diagnosed during the last 5 years (26.7%), fewer were diagnosed between 10 to 20 years ago (22.5%), and hardly any more than 20 years ago (1.7%). Patient follow-up time varied considerably, ranging between 0 and 17.4 years, and the number of follow-up visits ranged from 1 to 27. Patients had a median follow-up years of 1.8 (IQR: 0.5–3.4) and a median number of visits of 3 (IQR: 2–6). The distribution of the number of follow-up visits and years of follow-up is presented in the additional file (Fig. S1 and Fig. S2, respectively).
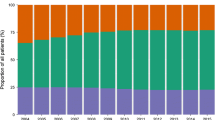
At the first follow-up visit, most patients had initiated treatment with insulin (56.5%), followed by OGLDs (32.9%) or a combination of both insulin + OGLDs (7.3%), while few patients were not prescribed medication and only lifestyle modification was recommended (3.3%). Patients in the database had a mean BMI of 25.9 ± 5.2 kg/m2, with 37.3% of women and 35.3% of males classified as overweight and 27.4% and 8.6%, respectively, obese. An average SBP of 131.5 ± 24.1 mmHg and DBP of 78.9 ± 13.5 mmHg was observed, with 14.4% of patients presenting an elevated SBP (≥ 130 to < 140 mm Hg) and 40.3% high SBP (≥ 140 mm Hg). Also, a median FPG of 199 mg/dL (IQR: 135–299) was recorded, with no difference between sex (199 mg/dL (IQR: 136–297) for women and 199 mg/dL (IQR: 133–303) for men), and representing a total of 79.9% of patients above the glycemic target, again, without a clear distinction between women 80.1% and men 79.3%. To provide a broader demographic description of the patients, the demographic characteristics at baseline and the latest follow-up stratified by sex and age groups of a subset of patients with a minimum of 1.5 years of follow-up are presented in the additional file (Table S1 and Table S2, respectively).
Achievement of glycemic target during the follow-up
Table 2 presents the crude and adjusted multi-level random-effect odds ratios for the achievement of glycemic target over the years of follow-up and the predicted average marginal effects. The adjusted multivariable model including 8648 patients with 35,499 observations (an average of 4.0 time points per patient) showed an increase in the odds of achieving the glycemic target of 18.4% (OR: 1.184, 95% CI: 1.130 to 1.239) per 1-year increase in the follow-up. The average marginal effect per one-year increase was 1.0% (0.010, 95% CI: 0.007, 0.012). In correspondence, Fig. 2 illustrates the average marginal effects with 95% CI of achieving glycemic target at specific time-points over the follow-up. Within the overall modest increase, it depicts an increase in the probability of achieving glycemic control over the first years of follow-up followed by a decline in the probability towards a longer follow-up period. Our model also showed that at baseline, men had a higher odds of achieving the glycemic target (OR: 1.342, 95% CI: 1.218 to 1.478) than women and those in the age groups of 40-65 years had a lower odds (OR: 0.843, 95% CI: 0.755 to 0.942) when compared to individuals > 65 years old. Moreover, patients with overweight appeared to have a higher odds of achieving glycemic target (OR: 1.289, 95% CI: 1.174 to 1.414) as well as those with obesity (OR: 1.306, 95% CI: 1.160 to 1.470) than individuals with a BMI < 25 kg/m2. At baseline, compared to insulin-treated patients, those treated with OGLDs (OR: 2.111, 95% CI: 1.913 to 2.331), OGLDs + Insulin (OR: 1.213, 95% CI: 1.015 to 1.449), and diet (OR: 7.717, 95% CI: 6.170 to 9.650) seemed to have a higher odds of achieving glycemic target. Our model revealed significant interactions between the years of follow-up and age groups, years of follow-up and BMI categories, and years of follow-up and treatments.
Probabilities and 95% confidence intervals for the achievement of glycemic control at specific time points of the total study population. This graph represents the average marginal effects (the annual marginal predicted means and 95% CI) for achieving the glycemic target at specific time points over the year of follow-up of the total study population. Within a modest overall increase, slightly higher probabilities of achieving glycemic control were observed over the first years of follow-up followed by a decline towards a longer follow-up
Achievement of glycemic target during the follow-up stratified by sex and age
The multi-level random-effects logistic regression stratified analyses based on sex and age categories for the achievement of glycemic target over the years of follow-up are presented in Table 3 and their average marginal effects in Table S3 (additional file). These findings revealed that only patients with an age > 40 years, independently of sex, increased their odds of achieving glycemic target over time. Per year of follow-up, for those between 40 and 65 years, it increased by approximately 12.0% (OR: 1.120, 95% CI: 1.070 to 1.173) for women and 13.5% (OR: 1.135, 95% CI: 1.072 to 1.200) for men, and for the age group of > 65 years, it increased by 14.1% (OR: 1.141, 95% CI: 1.050 to 1.240) for women and 21.6% (OR: 1.216, 95% CI: 1.104 to 1.340) for men. No change was observed among younger patients (< 40 years) associated with the increase of years of follow-up, but a fewer number of patients were observed within these age groups: 219 for men and 506 for women. In agreement with these findings, Fig. 3 exemplifies the average marginal effects and 95% CI for the achievement of glycemic control at specific time points over the follow-up by sex and age categories. Older individuals present a higher probability of achieving glycemic targets over the first years of follow-up while younger patients’ probability does not appear to change with increasing time. Nevertheless, towards the end of follow-up, the probability of achieving glycemic target was extremely low for all patients.
Probabilities and 95% confidence intervals for the achievement of glycemic control at specific time points by sex and age categories. This graph represents average marginal effects (the annual marginal predicted mean and 95% confidence interval) for achieving the glycemic target at specific time points over the years of the follow-up by sex and age category. In this representation, older individuals present a higher probability of achieving glycemic targets, particularly during the first years of the follow-up, while younger patients’ probability does not appear to change much with increasing time. Towards the end of follow-up, the probability was extremely low for all patients
Discussion
This retrospective database study of routine data described demographic features and evaluated the achievement of glycemic control over the years of follow-up of more than 8000 adult patients with T2D attending health centres for disease follow-up in Kinshasa. In our study population, our findings revealed a higher proportion of women seeking treatment follow-up as well as a higher proportion of metabolic risk factors among women, particularly obesity and high blood pressure. We observed modest improvements in achieving the glycemic target over time.
Potential explanations for the demographic feature of the predominance of women (67%) in our study population comprise (1) women are more prone to seek health care and follow-up when ill, as supported by previous evidence in similar settings [23, 24], and (2) T2D affects more women than men in this context, potentially explained also by our finding of higher proportions of metabolic risk factors, particularly obesity, which is a well-known and a primary risk factor for the development of T2D [25]. In DRC or similar settings, the higher proportion of T2D in women remains controversial. A small cross-sectional study conducted in 2017 in Kinshasa aiming at quantifying the prevalence of determinants of psychological insulin resistance among patients with T2D attending often three diabetic centres observed that among 213 participants, 60.6% were female [26]; however, this was not confirmed by other studies conducted across different African settings. A systematic review and meta-analysis based on 36 cross-sectional studies conducted between 1983 and 2009 in SSA found a slightly higher prevalence of T2D in women (5.9%; 95% CI: 4.6–7.6) than in men (5.5%; 95% CI: 4.1–7.2) [27]. In contrast, another meta-analysis including 41 cross-sectional or population-based studies conducted between 2000 and 2015 across Africa found an overall prevalence of T2D of 13.7% in adults > 55 years old but the prevalence did not differ significantly by sex [28], as was also reported by the WHO in DRC’s country profile of 2016 (women 4.3% and men 4.2%) [29]. Our findings concerning the higher proportion of metabolic risk factors, overweight, obesity, and elevated SBP, among women are aligned with the existing body of evidence in the DRC and Africa [30,31,32,33,34]. In this regard, further research is needed to understand if the higher proportion of women attending health centres for T2D follow-up is related to seeking care more often or a matter of a higher prevalence of diabetes potentially linked to a higher prevalence of risk factors. Our findings also highlight the necessity for the implementation of health promotion strategies, particularly for women, targeting modifiable risk factors (e.g. optimal diet, promotion of physical activity, weight management) for cardiometabolic diseases.
We observed a modest improvement towards the achievement of the glycemic target over the years of follow-up. Particularly, higher probabilities of achieving glycemic control were seen over the first years of follow-up followed by a decline towards a longer follow-up. However, glycemic control remained poor overall. Poor glycemic control (HbA1c ≥ 7% and/or FPG ≥ 126 mg/dL) has been observed in reports of previous observational cross-sectional studies using hospital or primary care data from the DRC [10, 35], South Africa [12], and Ethiopia reporting a glycemic control achieved in at most one-fourth to one-third of the population [11]. A narrative study also suggested poor glycemic control across SSA countries due to poor knowledge of T2D in patients [36]. Evidence has also reported inadequate monitoring of disease-related complications regardless of chronic care programmes in place, hence stressing the importance of incorporating self-monitoring strategies to reduce T2D-related complications [37]. Despite differences in study methods (study design, parameters of comparison and sample size), there is a clear indication of poor glycemic control across primary care facilities in Africa. To advance from these findings, future research should align with The Lancet Commission on diabetes report describing key points to improve diabetes care in LMICs [38] as well as comprehensively evaluate the evolution and control of T2D through strong study designs with sufficiently long follow-up periods, using reliable and complementary indicators (e.g. HbA1c), monitor T2D-related comorbidities and promote self-management. This approach will allow for the translation of clear messages derived from research to patients, health providers, and policy-makers influencers.
The median duration of 1.8 years of follow-up within a time frame of almost 30 years suggests that one of the main aims of the project Kin-Antwerp, to have a better tool to monitor and improve retention in care of patients, has not been reached. Interviews with patients during field visits provided some service-related and person-related factors such as the long travel and waiting times for consultations, the concurrence with other duties in life, and lack of acquaintances to guide them to the clinic. Literature from other chronic care projects in similar settings points to migration linked to seasonal labour [39]) and financial and other priorities that interfere with self-management and empowerment [40]. As for a key element of a chronic care programme, it is essential is to retain retention patients in care in the control of their disease, further in-depth assessment of Kin-Antwerp is necessary to understand the motives why closer follow-up was not achieved, identify areas for improvement, and assess the continuation of the project.
Evidence has reported that the management of T2D in LMICs is often suboptimal due to challenges related to accessibility/availability of medication and has emphasised the need for T2D management guidelines to be tailored to constrained resources [13] and also to consider the patients’ proximal environment [41]. These barriers are also relevant in the DRC context suggesting that the limited accessibility and availability of care and treatments, particularly driven by financial barriers of the health system, may play key roles in poor glycemic control and follow-up.
Aiming at identifying subgroups of patients that may have difficulties in attaining glycemic targets and may require prioritised attention, stratified analyses revealed that those patients with an age < 40 years independently of their sex seem to have lower odds of achieving glycemic target over time. Overweight and obesity may also play a role in suboptimal glycemic control. This is in agreement with previous evidence in which younger age has been identified as a predictor of poor glycemic control in Ethiopia [11], Uganda [42], and other settings [43]. Also, literature has suggested a positive association between overweight/obesity and suboptimal glycemic control [44, 45]. We suggest further research on identifying the drivers of poor glycemic control in these subgroups to be able to develop tailored and effective strategies.
As our research entails a large study population, more than 8000 patients, and a 30-year follow-up time frame, it allowed us to provide an overall insight into the demographic characteristics and disease control of a study population participating in the Kin-Antwerp project. Another strength includes the advanced subgroup analyses conducted in this study that will potentially inform and improve strategies for the prevention and control of T2D. This study has also limitations. Findings are based on FPG and measured by a glucometer; hence, our results might not be completely representative and reliable of overall glycemic control of these patients and should be interpreted with caution; however, in the context of DRC, the recommended disease monitoring of high-income countries, including HbA1c, continuous glucose monitoring, and self-monitoring blood glucose at multiple instances a day, is not common nor affordable practice. Conclusions regarding the treatments could not be made, as this information was insufficient and any discussion would be too speculative. Our study sample population is not representative of the general patients with T2D in DRC; thus, our findings may not be generalisable to other populations. Also, it is important to acknowledge the measurements and registration errors by physicians/nurses in the written forms, as well as data-entry errors in the database. With the information available in the database, we cannot exclude the presence of residual confounding in our models as some important variables influencing glycemic control such as lifestyle behaviours (diet, exercise) or demographics such as economic status, were not registered in the database.
Conclusion
This study sheds light on the disease control of more than 8000 patients with T2D followed within a time frame of almost 30 years in Kinshasa. Our findings highlight the poor glycemic control as well as the short duration of disease follow-up. Younger (< 40 years) patients seem to require prioritised attention to achieve the glycemic targets. Aligned with these findings, we recommend a deeper look into the Kin-Antwerp programme to understand what are the barriers to optimal effectiveness, identify key improvement areas, and explore the needs for continuation. Regardless, additional efforts for diabetes management guided by The Lancet Commission on diabetes report are necessary, particularly the introduction of reliable indicators (HbA1c) for disease monitoring along with self-management strategies including promotion of optimal lifestyle and treatment adherence.
Availability of data and materials
Data used for this research is owned by Centre d’Éducation Diabète & Santé and currently is not publicly available. Data may be made available from the owner on reasonable request.
Abbreviations
- 95% CI:
-
95% confidence interval
- BMI:
-
Body mass index
- DBP:
-
Diastolic blood pressure
- DRC:
-
The Democratic Republic of the Congo
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Haemoglobin A1c
- IDF:
-
International Diabetes Federation
- IQR:
-
Interquartile range
- ITM:
-
Institute of Tropical Medicine
- LMICs:
-
Low- and middle-income countries
- OGLDs:
-
Oral glucose lowering drugs
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SSA:
-
Sub-Saharan Africa
- T2D:
-
Type 2 diabetes
- WHO:
-
World Health Organisation
References
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10:1–11.
Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33:811–31.
International Diabetes Federation. IDF Diabetes Atlas, 9th edn. Brussels, Belgium: 2019. https://www.diabetesatlas.org.
Kengne AP, Bentham J, Zhou B, Peer N, Matsha TE, Bixby H, et al. Trends in obesity and diabetes across Africa from 1980 to 2014: an analysis of pooled population-based studies. Int J Epidemiol. 2017;46:1421–32.
World Health Organization. Report on the status of major health risk factors for noncommunicable diseases: WHO Africa Region, 2015. https://www.afro.who.int/publications/report-status-major-health-risk-factors-noncommunicable-diseases-who-african-region-0.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults NCD Risk Factor Collaboration (NCD-RisC)*. Lancet. 2017;390:2627–42.
Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–66.
Kehlenbrink S, Smith J, Ansbro É, Fuhr DC, Cheung A, Ratnayake R, et al. The burden of diabetes and use of diabetes care in humanitarian crises in low-income and middle-income countries. Lancet Diabetes Endocrinol. 2019;7:638–47.
Mawaw PM, Yav T, Mukuku O, Lukanka O, Kazadi PM, Tambwe D, et al. Prevalence of obesity, diabetes mellitus, hypertension and associated risk factors in a mining workforce, Democratic Republic of Congo. Pan Afr Med J. 2017;28:282.
Blum J, Chaney M, Mudji J, Mfungwa J, aimé K, Rice T, Labhardt ND. Glycaemic control among patients with type 2 diabetes followed in a rural African primary care setting — a reality check in the Democratic Republic of Congo. Prim Care Diabetes. 2020;14:139–46.
Gebreyohannes EA, Netere AK, Belachew SA. Glycemic control among diabetic patients in Ethiopia: a systematic review and meta-analysis. PLoS One. 2019. https://doi.org/10.1016/j.pcd.2019.08.002.
Kalain A, Omole OB. Lifestyle advice, processes of care and glycaemic control amongst patients with type 2 diabetes in a South African primary care facility. Afr J Prim Heal Care Fam Med. 2020;12:a2163.
Mohan V, Khunti K, Chan SP, Filho FF, Tran NQ, Ramaiya K, et al. Management of type 2 diabetes in developing countries: balancing optimal glycaemic control and outcomes with affordability and accessibility to treatment. Diabetes Ther. 2020;11:15–35.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Peteresen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12:1001885.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:1623–7.
The World Bank. Population, total - Congo, Dem. Rep. | Data. 2020. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=CD. Accessed 20 May 2022.
The World Bank. GDP growth (annual %) - Congo, Dem. Rep. | Data. 2020. https://data.worldbank.org/indicator/NY.GDP.MKTP.KD.ZG?locations=CD. Accessed 20 May 2022.
The World Bank. Democratic Republic of Congo Overview: development news, research, data | World Bank. 2022. https://www.worldbank.org/en/country/drc/overview#1. Accessed 20 May 2022.
World Health Organization. Improving health system efficiency: Democratic Republic of the Congo: improving aid coordination in the health sector. World Health Organization. 2015. https://apps.who.int/iris/handle/10665/186673.
Van Olmen J, Marie KG, Christian D, Clovis KJ, Emery B, Maurits VP, et al. Content, participants and outcomes of three diabetes care programmes in three low and middle income countries. Prim Care Diabetes. 2015;9:196–202.
International Diabetes Federation. Recommendations For Managing Type 2 Diabetes In Primary Care, 2017. www.idf.org/managing-type2-diabetes.
World Health Organization: Obesity: preventing and managing the global epidemic. World Health Organization Technical Report Series No. 894; Geneva; 2000. https://apps.who.int/iris/handle/10665/42330.
Yeatman S, Chamberlin S, Dovel K. Women’s (health) work: a population-based, cross-sectional study of gender differences in time spent seeking health care in Malawi. PLoS One. 2018;13:e0209586.
Das M, Angeli F, Krumeich AJSM, Van Schayck OCP. The gendered experience with respect to health-seeking behaviour in an urban slum of Kolkata, India. Int J Equity Health. 2018;17:24.
Goedecke JH, Mtintsilana A, Dlamini SN, Pascal KA. Type 2 diabetes mellitus in African women. Diabetes Res Clin Pract. 2017;123:87–96.
Rita SL, Lubaki FJP, Bompeka LF, Ogunbanjo GA, Ngwala LP. Prevalence and determinants of psychological insulin resistance among type 2 diabetic patients in Kinshasa, Democratic Republic of Congo. African J Prim Heal Care Fam Med. 2019;11:e1–5.
Hilawe EH, Yatsuya H, Kawaguchi L, Aoyama A. Differences by sex in the prevalence of diabetes mellitus, impaired fasting glycaemia and impaired glucose tolerance in sub-Saharan Africa: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:671–682D.
Werfalli M, Engel ME, Musekiwa A, Kengne AP, Levitt NS. The prevalence of type 2 diabetes among older peopl e in Africa: a systematic review. Lancet Diabetes Endocrinol. 2015;8587:1–13.
World Health Organization. Diabetes Democratic Republic of the Congo 2016 country profile. 2016. https://www.who.int/publications/m/item/diabetes-cod-country-profile-democratic-republic-of-the-congo-2016.
Adeboye B, Bermano G, Rolland C. Obesity and its health impact in Africa: a systematic review. Cardiovasc J Afr. 2012;23:512–21.
Buila NB, Ngoyi GN, Bayauli PM, Katamba FK, Lubenga YN, Kazadi SM, et al. Analysis of blood pressure and selected cardiovascular risk factors in the democratic republic of the Congo: The may measurement month 2018 results. Eur Hear J Suppl. 2020;22:H50–2.
Gómez-Olivé FX, Ali SA, Made F, Kyobutungi C, Nonterah E, Micklesfield L, et al. Regional and Sex Differences in the prevalence and awareness of hypertension: an H3Africa AWI-Gen study across 6 sites in Sub-Saharan Africa. Glob Heart. 2017;12:81–90.
Lasi K, On’kin JB, Longo-Mbenza B, Nge Okwe A, Kangola Kabangu N. Survey of abdominal obesities in an adult urban population of Kinshasa, Democratic Republic of Congo. Cardiovasc J Afr. 2007;18:300–7.
Ofori-Asenso R, Agyeman AA, Laar A, Boateng D. Overweight and obesity epidemic in Ghana - a systematic review and meta-analysis. BMC Public Health. 2016;16:1239.
Cedrick LM, Lubaki JPF, Francois LB, Gboyega OA, Philippe LN. Prevalence and determinants of poor glycaemic control amongst patients with diabetes followed at Vanga Evangelical Hospital, Democratic Republic of the Congo. African J Prim Heal Care Fam Med. 2021;13:1–6.
Ntontolo PN, Lukanu PN, Ogunbanjo GA, Fina J-PL, Kintaudi LNM. Knowledge of type 2 diabetic patients about their condition in Kimpese Hospital diabetic clinic, Democratic Republic of the Congo. African J Prim Heal care. Fam Med. 2017;9:a1385.
Masupe T, De Man J, Onagbiye S, Puoane T, Delobelle P. Prevalence of disease complications and risk factor monitoring amongst diabetes and hypertension patients attending chronic disease management programmes in a South African Township. Afr J Prim Heal Care Fam Med. 2021;13:e1–7.
Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2020;396:2019–82.
Topp SM, Mwamba C, Sharma A, Mukamba N, Beres LK, Geng E, et al. Rethinking retention: mapping interactions between multiple factors that influence long-term engagement in HIV care. PLoS One. 2018;13:1–27.
Abrahams N, Gilson L, Levitt NS, Dave JA. Factors that influence patient empowerment in inpatient chronic care: early thoughts on a diabetes care intervention in South Africa. BMC Endocr Disord. 2019;19:133.
De Man J, Aweko J, Daivadanam M, Alvesson HM, Delobelle P, Mayega RW, et al. Diabetes self-management in three different income settings: cross-learning of barriers and opportunities. PLoS One. 2019;14:1–22.
Patrick NB, Yadesa TM, Muhindo R, Lutoti S. Poor glycemic control and the contributing factors among type 2 diabetes mellitus patients attending outpatient diabetes clinic at mbarara regional referral hospital, Uganda. Diabetes Metab Syndr Obes Targets Ther. 2021;14:3123–30.
ToH MPHS, Wua CX, Leong HSS. Association of younger age with poor glycemic and cholesterol control in Asians with type 2 diabetes mellitus in Singapore. J Endocrinol Metab. 2011;1:27–37.
Bae JP, Lage MJ, Mo D, Nelson DR, Hoogwerf BJ. Obesity and glycemic control in patients with diabetes mellitus: Analysis of physician electronic health records in the US from 2009-2011. J Diabetes Complicat. 2016;30:212–20.
Watson L, Wilson BP, Alsop J, Kumar S. Weight and glycaemic control in type 2 diabetes: what is the outcome of insulin initiation? Diabetes Obes Metab. 2011;13:823–31.
Acknowledgements
We thank Sr Margérite LeClerque for the initiation of the database and the efforts and resources she invested in capacity building for diabetes care in DRC. Also, we thank Memisa Kinshasa and the Centre d’Education Diabète et Santé who also contributed to the development of the database, Yves Claeys, Epko Hasker, and Billy Malombo for their efforts in the digitalisation of the database and Els Genbrugge for the statistical advice in the analyses. We thank the City of Antwerp and in particular Sabine De Meulder and Nele Verschelden for their committed support to Kin-Antwerp.
Funding
The Kin-Antwerp project was sponsored by the City of Antwerp. The secondary analyses of the Kin-Antwerp database were sponsored internally by the Department of Public Health from the Institute of Tropical Medicine Antwerp.
Author information
Authors and Affiliations
Contributions
DS performed the analysis and drafted the manuscript; EM, JP, and JDM provided methodological support; JVO developed and supervised Kin-Antwerp; DKS, JCD, JCKK, and JDM developed and implemented Kin-Antwerp; JLP supervised the analysis of the Kin-Antwerp database and contribute to drafting the manuscript. All authors have read, reviewed, and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Institutional Review Board of the Institute of Tropical Medicine Antwerp (IRB/RR/ac/149) in Belgium and the Ethical Committee of the University of Kinshasa in DRC (ESP/CE/153B/2021). Waiver of consent was approved by both bodies as the risk of confidentiality was well mitigated and data underwent through strict anonymisation processes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Image S1
. Follow-up paper-based form for diabetes in DRC. Figure S1. Histogram representing the distribution of the number of follow-up visits. Figure S2. Histogram representing the distribution of the years of follow-up. Table S1. Baseline characteristics stratified by sex and age group (subset of patients with a minimum of 1.5 years of follow-up). Table S2. Last follow-up characteristics stratified by sex and age group (subset of patients with a minimum of 1.5 years of follow-up). Table S3. Stratified analysis by sex and age categories for the achievement of glycemic target over the follow up time (Average marginal effects -estimated probabilities and 95% confidence interval derived from the multi-level random effect logistic model).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sagastume, D., Mertens, E., Sibongwere, D.K. et al. A retrospective database study of the demographic features and glycemic control of patients with type 2 diabetes in Kinshasa, Democratic Republic of the Congo. BMC Med 20, 258 (2022). https://doi.org/10.1186/s12916-022-02458-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02458-2