Abstract
Background
Characteristics of the built environment, such as neighbourhood fast-food outlet exposure, are increasingly recognised as risk factors for unhealthy diet and obesity. Obesity also has a genetic component, with common genetic variants explaining a substantial proportion of population-level obesity susceptibility. However, it is not known whether and to what extent associations between fast-food outlet exposure and body weight are modified by genetic predisposition to obesity.
Methods
We used data from the Fenland Study, a population-based sample of 12,435 UK adults (mean age 48.6 years). We derived a genetic risk score associated with BMI (BMI-GRS) from 96 BMI-associated single nucleotide polymorphisms. Neighbourhood fast-food exposure was defined as quartiles of counts of outlets around the home address. We used multivariable regression models to estimate the associations of each exposure, independently and in combination, with measured BMI, overweight and obesity, and investigated interactions.
Results
We found independent associations between BMI-GRS and risk of overweight (RR = 1.34, 95% CI 1.23–1.47) and obesity (RR = 1.73, 95% CI 1.55–1.93), and between fast-food outlet exposure and risk of obesity (highest vs lowest quartile RR = 1.58, 95% CI 1.21–2.05). There was no evidence of an interaction of fast-food outlet exposure and genetic risk on BMI (P = 0.09), risk of overweight (P = 0.51), or risk of obesity (P = 0.27). The combination of higher BMI-GRS and highest fast-food outlet exposure was associated with 2.70 (95% CI 1.99–3.66) times greater risk of obesity.
Conclusions
Our study demonstrated independent associations of both genetic obesity risk and neighbourhood fast-food outlet exposure with adiposity. These important drivers of the obesity epidemic have to date been studied in isolation. Neighbourhood fast-food outlet exposure remains a potential target of policy intervention to prevent obesity and promote the public’s health.
Similar content being viewed by others
Background
As a modifiable factor associated with elevated risk of type 2 diabetes [1], cardiovascular disease [2], some cancers [3], and all-cause mortality [4], obesity is a global public health priority. In England, high body weight is one of the leading drivers of mortality and morbidity [5], and obesity costs the National Health Service £6.1bn per year [6]. One of the greatest challenges to addressing this public health problem at a population level is that obesity is a complex, multifactorial condition, including biological and social determinants.
Among biological determinants, genetic epidemiological studies have firmly established the role of genetics in the development of obesity. Genome-wide association studies (GWAS) have been able to identify individual genetic loci associated with obesity and common metabolic diseases [7]. For example, single-nucleotide polymorphisms (SNPs) in the FTO gene are associated with higher risk of obesity and type 2 diabetes [8], while SNPs in the MC4R gene are associated with increased fat mass and obesity risk [9]. The most recent GWAS have observed SNPs at 97 loci that can collectively indicate an individual’s genetic predisposition to obesity [10], although the level of variance explained is typically less than 2% [11].
The rise of obesity in the last 40 years has also been attributed to changing lifestyles [12], for example, declining physical activity levels and diets increasingly composed of processed, energy-dense foods, which can promote weight gain [13]. Food outlets selling these types of food, typically fast-food outlets, have become ubiquitous in neighbourhood environments [14, 15], and the potential of such access to influence dietary choices and long-term weight status is increasingly recognised [16]. Although some studies report contradictory or null findings, a growing number of cross-sectional and longitudinal studies in the UK and USA indicate that exposure to higher densities of fast-food outlets is associated with higher intake of energy-dense fast foods, higher body weight, and greater odds of obesity [17,18,19,20,21,22]. However, none of these studies have been able to account for individual-level genetic predisposition to obesity.
Moreover, while there is strong evidence for both genetic and environmental drivers of obesity, to date there is little understanding of how these two types of determinants may interact. FTO, MC4R, and other SNPs have been associated with appetitive phenotypes including disinhibited eating and preferences for high-fat or energy-dense foods [23], which may be enabled in neighbourhood environments with higher densities of fast-food outlets. Therefore, we investigated the associations of genetic obesity predisposition and objectively-measured neighbourhood fast-food outlet exposure, independently and in combination, with body weight, in a population-based sample of UK adults. Motivated to understand a possible interaction, we also explored how associations between fast-food outlet exposure and body weight might be modified by genetic susceptibility to obesity.
Methods
Study population
We used data from the Fenland Study, a population-based cohort of 12,435 adults aged 29–64 years in Cambridgeshire, UK. Study recruitment was from general practice lists across Cambridge, Ely, and Wisbech, conducted by the University of Cambridge MRC Epidemiology Unit. Data were collected from 2005 to 2015. Participants completed general questionnaires related to their lifestyle, medical history, and home address. Weight and height were measured to a standardised protocol by trained researchers, and the participants provided blood samples for genotyping. All study procedures were approved by the Health Research Authority National Research Ethics Service Committee East of England-Cambridge Central.
Assessment of neighbourhood fast-food outlet access
Data on food outlet locations were sourced from local councils throughout the study area in 2011 (approximately half-way through participant data collection). Fast-food outlets were classified as shown in Additional file 1: Table S1. These food outlets were geocoded at the postcode level using a geographic information system (ArcGIS 10, ESRI). Participant home addresses were also geocoded using postcodes. Using established methods [19, 22, 24], home ‘neighbourhoods’ were characterised as 1-mile straight-line radius (circular) buffers. The number of fast-food outlets was summed within neighbourhoods and categorised using quartiles.
Genotyping
Recent genome-wide association studies have identified 97 SNPs related to BMI [10]. These SNPs represent obesity susceptibility loci, including those near or in the well-characterised BMI-related FTO and MC4R genes. The genotyping procedure used here and method of imputation for SNPs not directly genotyped have been described in detail elsewhere [25, 26].
Genetic obesity predisposition score
Our genetic risk score for BMI (BMI-GRS) was derived from 96 of the 97 BMI-associated SNPs [25]. Each individual has 0, 1, or 2 copies of the BMI-increasing allele at each SNP, with BMI-GRS calculated by summing the number of alleles across all 96 variants. Scores were then weighted by the strength of association of each identified SNP with BMI, with higher scores indicating a greater predisposition to obesity. Participants were dichotomised at the median BMI-GRS (2.29) to define low- and high-risk groups [27].
Assessment of body weight and obesity
We defined two primary outcomes: body mass index (BMI, kg/m2), calculated from measured height and weight, and weight status (overweight: 25 ≥ BMI < 30; obese: BMI ≥ 30).
Statistical analysis
We used multivariable linear, and multinomial logistic regression models to examine associations between each of home neighbourhood fast-food outlet count (quartiles) and genetic risk (low, high), with BMI (kg/m2) and risk of being overweight (25 ≥ BMI < 30) and obese (BMI ≥ 30). Adjusted models included the following covariates theoretically determined a priori: age, sex, household income (< £20,000, £20,000–£40,000, > £40,000), highest educational attainment (≤ 11 years of education, 12–13 years, > 13 years), car access, smoking status (never, current, or ex), physical activity energy expenditure (kJ/kg/day, measured using individually calibrated combined acceleration and heart rate sensors (Actiheart, CamNtech) worn for up to 6 days) [28], and number of supermarkets belonging to major UK chains in the home neighbourhood. To establish independent associations, both fast-food outlet exposure and BMI-GRS models were mutually adjusted.
We tested for evidence of interaction (fast-food outlet exposure quartiles x BMI-GRS z-scores) using an F-test for BMI and likelihood ratio test for weight status. We estimated means and 95% CIs for BMI in high and low genetic risk groups, from stratified adjusted linear regression models.
We also cross-classified each participant into one of eight groups based on the combination of neighbourhood fast-food outlet exposure (four levels) and genetic risk (two levels) and used multivariable logistic regression with a single reference category (least exposed to fast-food outlets, low genetic risk) to estimate the combined associations of neighbourhood fast-food outlet exposure and genetic risk on the likelihood of being overweight and obese (both vs normal weight, i.e. BMI < 25).
This was a complete case analysis, with the sample restricted to those with complete data across all covariates and outcomes of interest (Additional file 1: Fig. S1). The final analytic sample size was 10,798, remaining representative of the wider Fenland Study cohort across key variables (Additional file 1: Table S2). A two-sided α level of 0.05 was used to test for statistical significance throughout. Data were analysed in 2019–2020 using Stata 14.2 (StataCorp LP., Texas).
Results
Sample characteristics
Descriptive statistics, overall and stratified by high and low genetic risk, are presented in Table 1. The sample had a mean age of 49 years and was 47% men, with a mean BMI of 26.9 kg/m2, and 21.7% of the sample were classed as obese. Participants were exposed to an average of 9 fast-food outlets in their home neighbourhood. Stratifying the sample by genetic risk revealed some differences in socioeconomic factors and body weight. The high-risk group contained a lower percentage of participants with the highest income and educational attainment. This group also had a mean BMI of 27.5 kg/m2, with 24.9% obese, compared to a mean BMI of 26.4 kg/m2 and 18.5% obesity for the low BMI-GRS group. Descriptive statistics stratified by quartiles of fast-food outlet exposure are shown in Additional file 1: Table S3, with no systematic differences in mean BMI-GRS observed across fast-food exposure groups.
BMI and weight status according to genetic predisposition to obesity
High genetic risk of obesity was positively associated with greater BMI, risk of overweight and obesity (Table 1). In model 1 (adjusted for age and sex), the high BMI-GRS group had 1.11 kg/m2 (95% CI, 0.93 to 1.29) higher BMI, had 1.34 (95% CI, 1.23 to 1.46) times greater risk of overweight, and 1.69 (95% CI, 1.53 to 1.88) times greater risk of obesity, than the low BMI-GRS group. These associations were robust to further adjustment for socioeconomic, behavioural and neighbourhood-level covariates (model 2), including neighbourhood fast-food outlet exposure; those at higher genetic risk maintained a 1.06kg/m2 (95% CI, 0.89 to 1.23) higher BMI, had 1.34 (95% CI, 1.23 to 1.47) times greater risk of overweight, and 1.73 (95% CI, 1.55 to 1.93) times greater risk of obesity.
BMI and weight status according to fast-food outlet exposure
Higher neighbourhood fast-food outlet exposure was positively associated with greater BMI and risk of obesity, with a suggestion of a dose-response. After adjustment for BMI-GRS alongside demographic, socioeconomic, and behavioural covariates, those most exposed to fast-food outlets (Q4) had on average 0.65 kg/m2 (95% CI, 0.23 to 1.06) higher BMI than those least exposed (Table 2). Those most exposed also had 1.58 (95% CI, 1.21 to 2.05) times greater risk of obesity.
BMI and weight status according to genetic predisposition to obesity and fast-food outlet exposure
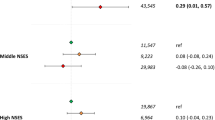
There was no evidence of interaction between BMI-GRS and fast-food outlet exposure on BMI (P = 0.09), the risk of being overweight (P = 0.51), or obese (P = 0.27). In an adjusted model stratified by BMI GRS (Table 2), those in the low genetic obesity risk group who were most exposed to fast-food outlets (Q4) had a significantly higher BMI (1.10 kg/m2, 95% CI, 0.54 to 1.66). In the high genetic obesity risk group, those most exposed to fast-food outlets did not have a significantly higher BMI (0.18 kg/m2, 95% CI, − 0.44 to 0.79). Adjusted means and 95% CIs for BMI in high and low genetic risk groups are shown in Fig. 1.
Mean (95% CI) BMI per quartile of fast-food outlet exposure in the Fenland Study (n = 10,798), stratified by genetic risk score for BMI (BMI-GRS, split by sample median: low ≤ 2.29; high > 2.29), adjusted for age, sex, household income, highest educational attainment, car access, smoking status, physical activity energy expenditure, counts of supermarkets in home neighbourhoods
High BMI-GRS in combination with highest fast-food outlet exposure was associated with significantly greater risk of obesity (RR = 2.70, 95% CI, 1.99 to 3.66), relative to those at low genetic predisposition and least exposed to fast-food outlets (Table 3).
Discussion
In a sample of nearly 11,000 UK adults, we found that genetic predisposition to obesity and neighbourhood fast-food outlet exposure were independently associated with higher BMI and risk of obesity. We did not find evidence that the association of fast-food outlet exposure with BMI, overweight, or obesity differed between the low and high genetic risk groups. In combination, we observed a nearly threefold risk of obesity in those with both high genetic risk and with highest fast-food outlet exposure, relative to those at low genetic risk and least exposed to fast-food outlets.
The mechanisms by which BMI-associated SNPs confer a greater risk of obesity are not fully elucidated, but two SNPs included in our genetic risk score for BMI, FTO and MC4R, have been linked to dysregulation of appetite and loss of control over eating [29,30,31,32], and preferences towards energy-dense [33], high-fat foods [23, 34]. As such, studies using genetic risk scores similar to the one used here have found that the association between these scores and obesity can be partly explained by appetite and eating behaviours [26, 35]. However, previous research has been limited to examining the interaction of BMI-associated SNPs with behavioural factors (gene-lifestyle interactions) such as diet and physical activity. For example, the influence of FTO on obesity risk can be moderated by physical activity [27]. Similarly, dietary risk factors for obesity, including consumption of sugar-sweetened beverages [36], and fried food [37], have been more strongly associated with weight gain in those with higher genetic obesity predisposition.
To our knowledge, this is the first published investigation of the interplay between any characteristic of the neighbourhood environment and genetic obesity risk. Our study was motivated to explore the hypothesis that genetic obesity risk would be exaggerated in permissive neighbourhood environments, characterised by an abundance of fast-food outlets, where large portions of affordable, energy-dense foods are readily accessible [38]. We expected that the strength of the relationship between fast-food outlet density and body weight would be stronger for those more genetically susceptible to obesity (Fig. 2a). We found no evidence to support this hypothesis. Alternatively, if it were the case that those with higher genetic risk were equally susceptible to the food environment, we would have expected the relationship between fast-food outlet density and body weight to be similar in both groups, albeit with those at higher risk having higher body weight at any given level of environmental exposure (Fig. 2b). However, although we found no evidence of interaction, our results indicated a possible third alternative, of a weaker association of the food environment with BMI among those with higher genetic risk of obesity, compared with those with lower genetic risk (Fig. 2c). We observed that, at highest levels of fast-food outlet exposure, mean BMI for the lower and higher genetic risk groups converged.
Hypothetical associations between density of (or exposure to) fast-food outlets and BMI, which are: a moderated by genetic obesity risk, with the higher genetic risk group showing a stronger environmental association than the lower genetic risk group; b not moderated by genetic obesity risk; and c moderated by genetic obesity risk, with the higher genetic risk group showing a weaker environmental association than the lower genetic risk group
The key implication of our findings is the necessity for further research to test our observations and understand mechanisms in other samples. It is possible, for example, that the contribution of the food environment may simply be less detectable among a population of adults with higher risk of obesity stemming from multiple biological and metabolic determinants [25]. This explanation would be consistent with Rothman’s component cause model, which suggests that for outcomes with multiple causes, the apparent strength of any single causal component is influenced by the relative prevalence of other component causes [39]. Nonetheless, in the immediate term and over and above the contribution of genetic susceptibility, neighbourhood fast-food outlet exposure appears to be a significant and importantly modifiable contributor, subject to change via urban planning (‘zoning’) as a structural intervention to prevent obesity and promote the public’s health [40].
The major strengths of this study include objective assessment of neighbourhood fast-food outlet exposure, using accurate and contemporaneous food outlet location data; objective height and weight data, measured by trained researchers; and use of an empirically-derived genetic risk score based on 96 BMI-associated SNPs. The main limitation of this study is the cross-sectional, observational study design, which limits causal inference. It is possible that preference for fast food may drive the selection of residential neighbourhoods with abundant fast-food outlet access (reverse causality). Our estimates of combined associations might be confounded because preference for energy-dense fast food may arise as a function of genetic obesity predisposition. Our fast-food outlet exposure models may have residual confounding, for example from unobserved environmental attributes, such as exposure to food outlets beyond the home neighbourhood. This said, our models were comprehensively adjusted for behavioural and sociodemographic covariates.
Some misclassification may have occurred as our exposure (number of fast-food outlets) and outcome (adiposity) were measured at different time points (2011 and 2005–2015, respectively). This risk was minimised as far as possible through exposure data being collected at approximately the mid-point of the period of outcome data collection. Moreover, we minimised misclassification through operationalising fast-food outlet exposure in quartiles, which would have been less sensitive to food environment change over time. To test this, we cross-classified all participants, comparing their exposure classification based on 2011 food environment data, against that based on food environment data from 2014 (courtesy of the Food environment assessment tool, powered by Ordnance Survey) [41]. The resulting cross-classification was high (rs = 0.94, P < 0.001). Therefore, any individual recruited into the Fenland Study between 2011 and 2014 would likely have been characterised similarly in terms of their fast-food outlet exposure. We have described the limitations of our neighbourhood fast-food outlet exposure metric previously [19, 22, 24].
We used a genetic risk score composed of 96 BMI-increasing alleles, which enabled us to detect a large main effect both independently and in combination with neighbourhood fast-food outlet exposure. However, this approach masks the contribution of individual SNPs, which may act through discrete behavioural or metabolic pathways of relevance to the food environment. Moreover, given the highly polygenic nature of body weight, genetic risk scores that use a genome-wide set of common variants in their construction may have stronger predictive power for obesity and BMI and should be considered for future research [42]. The Fenland Study is a population-based cohort study, with working-age adults recruited who were largely educated, employed and white British, living in Cambridgeshire, which is a county in the East of England comprising urban, suburban and rural areas, including the major cities of Cambridge and Peterborough. Characteristics of this population and study area, although common elsewhere in the UK and beyond, may influence the generalisability of our findings.
Conclusions
Our study confirms previously-identified associations of both genetic and neighbourhood risk factors with adiposity, and for the first time demonstrated independence in these relationships. These important drivers of the obesity epidemic have to date been studied in isolation. Although obesity-related SNPs contribute substantially to obesity in the population, neighbourhood fast-food outlet exposure also appears to be a significant determinant and an important and modifiable target of policy intervention to prevent obesity and promote the public’s health. We found no evidence of interaction between these determinants.
Availability of data and materials
The Fenland Study data analysed here are not publicly available for reasons of confidentiality, but may be available upon reasonable request. For data sharing enquiries, please email datasharing@mrc-epid.cam.ac.uk.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- GRS:
-
Genetic risk score
- GWAS:
-
Genome-wide association study
- Q:
-
Quartile
- RR:
-
Relative risk
- SNP:
-
Single nucleotide polymorphism
- UK:
-
United Kingdom
References
Eckel RH, Kahn SE, Ferrannini E, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care. 2011;34(6):1424–30.
Bastien M, Poirier P, Lemieux I, Després J-P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56(4):369–81.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, and Straif K, for the International Agency for Research on Cancer Handbook Working Group.,. Body fatness and cancer - viewpoint of the IARC Working Group. N Engl J Med 2016;375(8):794–798.
The Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86.
Steel N, Ford JA, Newton JN, et al. Changes in health in the countries of the UK and 150 English local authority areas 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10158):1467–661.
Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical activity, smoking, alcohol and obesity in the UK: an update to 2006-07 NHS costs. J Public Health. 2011;33(4):527–35.
Speliotes EK, Willer CJ, Berndt SI, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. Nov 2010;42(11):937–48.
Frayling TM, Timpson NJ, Weedon MN, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889–94.
Loos RJF, Bouchard C. FTO: the first gene contributing to common forms of human obesity. Obesity Rev. 2008;9(3):246–50.
Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206.
Elks CE, den Hoed M, Zhao JH, et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front Endocrinol. 2012;3(29):1–16.
Rodgers A, Woodward A, Swinburn B, Dietz WH. Prevalence trends tell US what did not precipitate the US obesity epidemic. Lancet Public Health. 2018;3(4):162–3.
Mozzaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364:2392–404.
Maguire ER, Burgoine T, Monsivais P. Area deprivation and the food environment over time: a repeated cross-sectional study on takeaway outlet density and supermarket presence in Norfolk, UK, 1980-2008. Health Place. 2015;33:142–7.
United States Department of Agriculture: Economic research service. ERS's updated food environment atlas shows an increase in fast food restaurants between 2009 and 2014. 2017; https://www.ers.usda.gov/amber-waves/2017/december/ers-s-updated-food-environment-atlas-shows-an-increase-in-fast-food-restaurants-between-2009-and-2014/. Accessed 25/1/19.
Foresight. Tackling obesities: Future choices - Project report. London: Government Office for Science; 2007.
Wilkins E, Radley D, Morris M, et al. A systematic review employing the GeoFERN framework to examine methods, reporting quality and associations between the retail food environment and obesity. Health Place. 2019;57:186–99.
Burgoine T, Sarkar C, Webster C, Monsivais P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: evidence from 51,361 UK Biobank participants. Int J Behav Nutr Phys Activ. 2018;15(71):1–12.
Burgoine T, Forouhi NG, Griffin SJ, Brage S, Wareham NJ, Monsivais P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross sectional study. Am J Clin Nutr. 2016;103:1–8.
Black C, Moon G, Baird J. Dietary inequalities: what is the evidence for the effect of the neighbourhood food environment? Health Place. 2013;27:229–42.
Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson AM. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity. 2015;23:1331–44.
Burgoine T, Forouhi NG, Griffin SJ, Wareham NJ, Monsivais P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ. 2014;348(7950):1–10.
Grimm ER, Steinle NI. Genetics of eating behaviour: established and emerging concepts. Nutr Rev. 2011;69(1):52–60.
Burgoine T, Monsivais P. Characterising food environment exposure at home, at work, and along commuting journeys using data on adults in the UK. Int J Behav Nutr Phys Activ. 2013;10(85):1–11.
Clifton EA, Day FR, De Lucia RE, et al. Associations between body mass index-related genetic variants and adult body composition: the Fenland cohort study. Int J Obes. 2017;41(4):613–9.
de Lauzon-Guillain, Clifton EA, Day FR, et al. Mediation and modification of genetic susceptibility to obesity by eating behaviours. Am J Clin Nutr 2017;106(4):996–1004.
Li S, Zhao JH, Luan J, et al. Physical activity attenuates the genetic predisposition to obesity in 20,000 men and women from EPIC-Norfolk prospective population study. PLoS Med. 2010;7(8):1–9.
Cooper AJM, Brage S, Ekelund U, Wareham NJ, Griffin SJ, Simmons RK. Association between objectively assessed sedentary time and physical activity with metabolic risk factors among people with recently diagnosed type 2 diabetes. Diabetologia. 2013;57:73–82.
Loos RJF, Yeo GSH. The bigger picture of FTO - the first GWAS-identified obesity gene. Nat Rev Endocrinol. 2014;10:51–61.
Dougkas A, Yagoob P, Givens DI, Reynolds CK, Minihane AM. The impact of obesity-related SNP on appetite and energy intake. Br J Nutr. 2013;110(6):1151–6.
Kirac D, Kasimay Cakir O, Avcilar T, et al. Effects of MR4R, FTO, and NMB gene variants to obesity, physical activity, and eating behavior phenotypes. IUBMB Life. 2016;68(10):806–16.
Stutzmann F, Cauchi S, Durand E, et al. Common genetic variation near MC4R is associated with eating behaviour patterns in European populations. Int J Obes. 2009;33(3):373–8.
Cecil JE, Tavendale R, Watt P, Hetherington MM, Palmer CN. An obesity-associated FTO gene variant and increased energy intake in children. N Engl J Med. 2008;359(24):2558–66.
Tanofsky-Kraff M, Han JC, Anandalingham K, et al. The FTO gene rs9939609 obesity-risk allele and loss of control over eating. Am J Clin Nutr. 2009;90(6):1483–8.
Jacob R, Drapeau V, Tremblay A, Provencher V, Bouchard C, Pérusse L. The role of eating behaviour traits in mediating genetic susceptibility to obesity. Am J Clin Nutr. 2018;108(3):445–52.
Qi Q, Chu AY, Kang JH, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med. 2012;367(15):1387–96.
Qi Q, Chu AY, Kang JH, et al. Fried food consumption, genetic risk, and body mass index: gene-diet interaction analysis in three US cohort studies. BMJ. 2014;348:1–12.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16.
Rothman KJ. Causes. Am J Epidemiol. 1976;104(6):587–92.
Keeble M, Burgoine T, White M, Summerbell C, Cummins S, Adams J. How does local government use the planning system to regulate hot food takeaway outlets? A census of current practice in England using document review. Health Place. 2019;57:171–8.
Burgoine T., Monsivais P., and the Feat Development Team. Food environment assessment tool (Feat). 2017; www.feat-tool.org.uk. Accessed 12/6/18.
Khera VK, Chaffin M, Wade KH, et al. Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell. 2019;177:587–96.
Acknowledgements
We thank local councils for kindly supplying the data to enable this work, and all the volunteers who participated in the Fenland Study, as well as Fenland Study Coordination, Field Epidemiology, and Data Management teams.
Funding
This work was undertaken by the Centre for Diet and Activity Research (CEDAR), a UK Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research, and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged (grant number MR/K023187/1). TB received support from the MRC (grant number MC_UU_00006/7). The Fenland Study is funded by the MRC and the study PIs (NJW and NGF) acknowledge this support (grant numbers MC_UU_00006/1, MC_UU_00006/3, MC_UU_00006/6). NJW and NGF also acknowledge support from NIHR Biomedical Research Centre Cambridge: Nutrition, Diet, and Lifestyle Research Theme (grant number IS-BRC-1215-20014). PM received support from the Health Equity Research Center at Washington State University. The funders played no role in the design of the study, the collection, analysis, and interpretation of data, or the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
The analysis was designed by TB and PM. TB led on fast-food outlet data collection from local councils, and led on data analysis, in consultation with PM, NGF, SJS and NJW. NGF and NJW are principal investigators of the Fenland Study and were responsible for its overall design, management and supervision of data collection. TB and PM drafted the manuscript together. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All study procedures were approved by the Health Research Authority National Research Ethics Service Committee East of England-Cambridge Central. The Fenland Study volunteers provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Detailed fast-food outlet and chain supermarket characteristics. Table S2. Fenland Study cohort, analytic sample and excluded subset sociodemographic comparisons. Table S3. Characteristics of participants in the Fenland Study (n = 10,798), Cambridgeshire, UK, overall and stratified by quartile of exposure to fast-food outlets. Table S4. Associations between genetic risk score (BMI-GRS) and each of: body mass index and risks of overweight and obesity in the Fenland Study (n = 10,798), Cambridgeshire, UK, estimated using linear and multinomial logistic regression models, respectively. Table S5. Combined associations of fast-food outlet exposure and genetic risk score (BMI-GRS) with risk of overweight in the Fenland Study (n = 10,798), Cambridgeshire, UK, estimated using multinomial logistic regression with a single reference group. Fig. S1. Flow diagram for Fenland Study cohort sample restriction to the Fenland Study analytic sample.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Burgoine, T., Monsivais, P., Sharp, S.J. et al. Independent and combined associations between fast-food outlet exposure and genetic risk for obesity: a population-based, cross-sectional study in the UK. BMC Med 19, 49 (2021). https://doi.org/10.1186/s12916-021-01902-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-021-01902-z