Abstract
Background
Evidence on the association between the presence of fast-food outlets and Body Mass Index (BMI) is inconsistent. Furthermore, mechanisms underlying the fast-food outlet presence-BMI association are understudied. We investigated the association between the number of fast-food outlets being present and objectively measured BMI. Moreover, we investigated to what extent this association was moderated by neighbourhood socio-economic status (NSES) and healthy food outlets. Additionally, we investigated mediation by frequency of fast-food consumption and amount of fat intake.
Methods
In this cross-sectional study, we used baseline data of adults in Lifelines (N = 149,617). Geo-coded residential addresses were linked to fast-food and healthy food outlet locations. We computed the number of fast-food and healthy food outlets within 1 kilometre (km) of participants’ residential addresses (each categorised into null, one, or at least two). Participants underwent objective BMI measurements. We linked data to Statistics Netherlands to compute NSES. Frequency of fast-food consumption and amount of fat intake were measured through questionnaires in Lifelines. Multivariable multilevel linear regression analyses were performed to investigate associations between fast-food outlet presence and BMI, adjusting for individual and environmental potential confounders. When exposure-moderator interactions had p-value < 0.10 or improved model fit (∆AIC ≥ 2), we conducted stratified analyses. We used causal mediation methods to assess mediation.
Results
Participants with one fast-food outlet within 1 km had a higher BMI than participants with no fast-food outlet within 1 km (B = 0.11, 95% CI: 0.01, 0.21). Effect sizes for at least two fast-food outlets were larger in low NSES areas (B = 0.29, 95% CI: 0.01, 0.57), and especially in low NSES areas where at least two healthy food outlets within 1 km were available (B = 0.75, 95% CI: 0.19, 1.31). Amount of fat intake, but not frequency of fast-food consumption, explained this association for 3.1%.
Conclusions
Participants living in low SES neighbourhoods with at least two fast-food outlets within 1 km of their residential address had a higher BMI than their peers with no fast-food outlets within 1 km. Among these participants, healthy food outlets did not buffer the potentially unhealthy impact of fast-food outlets. Amount of fat intake partly explained this association. This study highlights neighbourhood socio-economic inequalities regarding fast-food outlets and BMI.
Similar content being viewed by others
Introduction
Overweight and obesity are risk factors for various chronic diseases, such as cardiovascular diseases, diabetes mellitus type II, dementia, and cancer [1]. Worldwide, the adult prevalence of overweight and obesity has tripled from 13% in 1975 to 39% in 2016 [2], currently affecting over 2 billion adults [2] and contributing globally to a rise in healthcare costs [3].
Researchers have focused increasing attention on environmental determinants of overweight and obesity, and particularly on the presence of fast-food outlets [4]. Frequency of fast-food consumption is known to be associated with caloric intake and Body Mass Index (BMI) [5], but evidence regarding the association between the presence of fast-food outlets and BMI remains inconsistent [6]. This heterogeneity in results may be explained partly by the accuracy of measurement of fast-food outlet presence [7] and BMI [8]. An accurate measurement of the presence of fast-food outlets around residential addresses requires complex linkages between fast-food outlet locations and participant residential addresses. Regarding BMI, many studies in the field relied on self-reported rather than objectively measured BMI. This can result in biased associations, as individuals with a higher BMI are more likely to underreport their BMI [9].
Furthermore, the complex interplay between the presence of fast-food outlets and other environmental factors on BMI is poorly understood. While previous studies typically studied fast-food outlet presence in isolation in relation to BMI, it is increasingly recognised that the role of fast-food outlet presence may be dependent on the wider context within a complex system consisting of other built environmental and socio-economic factors [10]. Besides, knowledge on the settings in which the association between fast-food outlet presence and BMI is stronger may be used by policy makers to create healthier living environments using tailored approaches. To date, little is known about the potentially moderating role of neighbourhood socio-economic status and the presence of healthy food outlets in the association between fast-food outlet presence and BMI. Algren et al. [11] suggested that adopting a healthy lifestyle in neighbourhoods with low socio-economic status (NSES) might be more difficult because of lower social support and higher presence of neighbourhood stressors (e.g., criminality). Previous studies reported a higher number of fast-food outlets in low NSES areas [12, 13] and that the association between the presence of fast-food outlets and BMI is stronger in people from low individual socio-economic status [14, 15]. Still, to our best knowledge, no study has assessed whether the association between the presence of fast-food outlets and BMI is moderated by neighbourhood socio-economic status. Contrary to the potentially amplifying role of low NSES ubiquitous presence of healthy food outlets (e.g., fruit and vegetable markets, supermarkets [16,17,18,19]) may provide a buffer against the potentially unhealthy influence of fast-food outlets by enabling individuals to opt for healthy alternatives. Yet, no study has assessed whether the association between the presence of fast-food outlets and BMI is weaker with a higher presence of healthy food outlets.
Moreover, more research is needed on mediating pathways in the association between the presence of fast-food outlets and BMI. Elucidating such mediating pathways may provide insight into the mechanisms through which fast-food outlets may exert their health effects, and inform approaches to limit the impact of fast-food outlets. The frequency of fast-food consumption or amount of fat intake may mediate the association between the presence of fast-food outlets and BMI [20]. Frequency of fast-food consumption may have a mediating role, as the presence of fast-food outlets may promote social norms regarding eating fast-food [20]. A European cross-sectional study by Mackenbach et al. [21] found that associations between the presence of fast-food outlets and BMI were not mediated by the frequency of fast-food consumption. However, mediated associations may have been underestimated, as Mackenbach et al. had to rely on self-reported BMI. Furthermore, the amount of fat intake may mediate the association between the presence of fast-food outlets and BMI, as large amounts of fat are a major unhealthy component of fast-food meals [22]. To understand the mechanisms underlying the association between the presence of fast-food outlets and BMI, more research is needed regarding the mediating role of the frequency of fast-food consumption and the amount of fat intake.
In this study, we investigated the association between the presence of fast-food outlets and objectively measured BMI. Moreover, we investigated the moderating role of NSES and the presence of healthy food outlets in the association between the presence of fast-food outlets and objectively measured BMI. Furthermore, we examined to what extent this association is mediated by the frequency of fast-food consumption and the amount of fat intake.
Methods
Study population
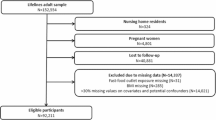
In this cross-sectional study, we used baseline adult data (≥ 18 years) from the Lifelines Cohort Study [23]. Lifelines is a prospective population-based cohort study examining in a unique three-generational design the health and health-related behaviours of 167,729 persons living in the north of the Netherlands. It employs a broad range of investigative procedures in assessing the biomedical, socio-demographic, behavioural, physical and psychological factors, which contribute to the health and disease of the general population, with a special focus on multi-morbidity and complex genetics. Recruitment took place between December 2006 and December 2013 through general practitioners, participants’ family members, and online registrations. At baseline, participants underwent a physical examination and filled out online questionnaires. Lifelines is broadly representative of the general population of the Northern Netherlands in terms of socio-economic and lifestyle factors, prevalence of chronic diseases, and general health [24]. Participants’ residential addresses were geo-coded based on a nationwide address registry [25]. Specifically for this study, we excluded nursing home residents (N = 181), as they may not be able to interact with their fast-food environment, and pregnant women (currently or last year; N = 2,757), whose current BMI may not represent their actual weight status.
Data linkage
Based on the geo-coded residential addresses of Lifelines participants, we established a linkage with LISA data (‘Landelijk Informatiesysteem van Arbeidsplaatsen’; www.lisa.nl) [26]. LISA data consist of Dutch retail outlet locations where paid work is performed for at least one hour/month. We used LISA data from 2012, corresponding with the median recruitment year of Lifelines’ baseline participants (2012).
To retrieve locations of fast-food outlets, healthy food outlets, and physical activity facilities we used specific Standard Business Information (SBI) codes. We defined fast-food outlets as outlets offering food that was (1) paid for at the counter, (2) predominantly highly caloric, unhealthy, and prepared in bulk and kept hot, and (3) meant to be eaten directly [27]. SBI-codes used to select fast-food outlets were based on a previous article on this topic [18]. We defined healthy food outlets as outlets offering food that was (1) predominantly unprocessed and meant to be prepared at home and (2) predominantly healthy. In line with existing literature [16, 18] and given the evidence that fruits, vegetables, and fatty fish are associated with a healthier cardiometabolic profile [28], we included the following retail outlets as healthy food outlets: retail outlets for potatoes, vegetables, and fruit (SBI code 47.21); retail outlets for natural foods and reform articles (e.g., Ekoplaza) (SBI code 47.29.2); marketplace for potatoes, vegetables, and fruit (SBI code 47.81.1); retail outlets for selling fish (SBI code 47.23); supermarkets and similar retail outlets with a general assortment of foods (SBI code 47.11). Supermarkets are also generally considered a source of healthy foods in the literature [16], even though they also offer unhealthy foods. We defined physical activity facilities as facilities that (1) require an access fee and (2) are meant exclusively for individuals to exercise. Further details about the definitions are provided elsewhere [29] and in Additional file 1: Table S1.
Additionally, we linked participants’ neighbourhood codes to Statistics Netherlands 2012 neighbourhood data [30]. We determined neighbourhood boundaries using official administrative definitions from Statistics Netherlands [31]. Based on these boundaries, a neighbourhood in the Netherlands covered a median (IQR) surface of 84 (35–289) hectares and contained a median (IQR) of 660 (180–1,850) residents.
Exposure
Based on the linkage with LISA data, we computed the number of fast-food outlets within a straight-line 1-kilometre (km) distance of participants’ residential addresses. We opted for an absolute rather than a relative measure of fast-food outlet presence, as relative measures are more difficult to interpret and to translate into policies on the food environment [32]. The 1 km-density was based on a previous study in the Dutch context that found strongest associations with BMI for 1 km-density, rather than proximity and density of other ranges [29]. Moreover, the distance of 1 km is equal to a 10- to 15-minute walk for an average adult, and has been linked to food shopping behaviours [33]. We did not observe a linear relation between the number of fast-food outlets within 1 km and BMI in our data. Therefore, we categorised the number of fast-food outlets into null, one, or at least two fast-food outlets within 1 km. This categorisation reflects being present versus being absent, and allows for further assessment when multiple fast-food outlets are present within 1 km. Splitting the group of participants with at least two fast-food outlets within 1 km into more categories was not opted for, as a study on the Dutch context found that going from null to one fast-food outlet was associated with changes in BMI, but that an increase in fast-food outlets was not associated with changes in BMI when multiple fast-food outlets in the environment were available already [13]. We computed this variable using address points in QGIS v3.4.2 (match rate 99.6%).
Outcomes
BMI (in kilogram(kg)/metre(m)2) was based on objectively measured weight (in kg) and height (in centimetre(cm)), without shoes and heavy clothing, during a physical examination at the Lifelines research study site.
Moderators
We determined neighbourhood socio-economic status (NSES) based on the linkage with Statistics Netherlands, and measured it as a composite score of: (1) the average value of a house per 1,000 euros, (2) the percentage of owner-occupied houses, (3) the mean net disposable monthly income, and (4) the percentage of individuals aged 15–65 years receiving assistance benefits. We opted for these indicators to create a multidimensional NSES score, reflecting the financial, housing, and work situation in a neighbourhood [34]. After reversing the fourth indicator, we aggregated all indicators into one z-standardized score using principal component analysis. Loadings of the separate indicators on the NSES variable were all 0.80 or higher. The NSES variable was z-standardised and divided into tertiles (low, middle and high NSES).
The number of healthy food outlets within 1 km of the residential address was based on the linkage with LISA data and categorized into null, one and at least two healthy food outlets within 1 km of the residential address.
Mediators
The frequency of fast-food consumption was measured with the question: ‘If you have eaten ready-to-eat meals in the past month, how often did you eat meals from fast-food restaurants (e.g. McDonalds, Burger King or KFC)?’ with the following answer options: ‘never’, ‘sometimes’, ‘often’, and ‘always’. Since only a relatively small proportion of participants responded with ‘often’ (4.1%) or ‘always’ (1.8%), we merged these two categories with the response option ‘sometimes’. The amount of fat intake was based on a 110-item Food Frequency Questionnaire (FFQ) [28] to assess past-month food intake, and on a Dutch food composition database [35]. We measured the amount of fat intake as the number of grams of fat/1,000 kcal, as FFQ’s can be used to accurately estimate only relative intakes of certain foods over other types of foods [28]. Further details about the measurement of fat intake in Lifelines are provided elsewhere [28, 36].
Potential confounders
Analyses were adjusted for individual-level and neighbourhood-level potential confounders. Individual-level potential confounders included: sex; age (in years); partner status (having a partner or not); highest level of completed education (low [less than primary education, primary education, or lower secondary education], middle [upper secondary education or post-secondary non-tertiary education], and high [short-cycle tertiary education, bachelor or equivalent education, master or equivalent education, doctoral or equivalent education] based on the International Standard Classification of Education [37]); weekly working hours (0, 1–11, 12–19, 20–31, or ≥ 32 h); net monthly income (middle value of categories <€750 [set to €500], €750-€1,000, subsequent 500-euro intervals until €3,500, and >€3,500 [set to €3,750], divided by the square root of individuals living from that income [38]); density of physical activity facilities within 1 km (based on the LISA data); household size (number of individuals living in the household); density of healthy food outlets within 1 km; and occupational prestige (based on the Standard International Occupational Prestige Scale (SIOPS) [39]). Neighbourhood-level potential confounders were address density (number of addresses/km2) and NSES, as based on the linkage with Statistics Netherlands. For mediation analyses, we additionally included (1) occupational and (2) non-occupational moderate-to-vigorous physical activity (MVPA) based on the Short Questionnaire to Assess Health-enhancing physical activity (SQUASH) questionnaire [40], as physical activity may influence diet and BMI, but is unlikely to influence the presence of fast-food outlets. Occupational and non-occupational MVPA were treated separately as they are differentially associated with BMI [41].
Statistical analysis
We imputed missing data using Multiple Imputation by Chained Equations with Multilevel Data (MICEMD), accounting for clustered data within neighbourhoods. Based on statistical recommendations [42], we created 10 imputed datasets.
To investigate associations between the presence of fast-food outlets and BMI, we performed multivariable multilevel linear regression analyses to account for clustered data within neighbourhoods. We adjusted for the potential confounders listed above, and reported effect sizes and 95% confidence intervals. To examine moderation by NSES and healthy food outlets, we assessed their two-way interaction terms with fast-food outlet presence on BMI and tested the model fit (Akaike Information Criterion (AIC)) for models with and without these interaction terms. If one of the interaction terms had a p-value < 0.10 [43]) or model fit improved meaningfully (i.e., at least 2 points lower AIC in the model with interaction terms [44]), we presented stratified analyses for NSES and/or healthy food outlet presence. In addition, we reasoned that the association between fast-food outlet presence and BMI may be especially pronounced in low NSES areas with few healthy food outlets. Therefore, we tested three-way interaction terms between fast-food outlet presence, NSES, and healthy food outlet presence, and tested the AIC for models with and without these interaction terms. If one of the three-way interaction terms had a p-value < 0.10 or model fit improved meaningfully (i.e., at least 2 points lower AIC in the model with interaction terms), we presented stratified analyses by level of NSES and number of healthy food outlets.
To examine mediation through the frequency of fast-food consumption and the amount of fat intake, we performed mediation analyses using causal mediation methods [45]. Multilevel models were used to estimate paths. We incorporated interactions between exposure and mediators [46], as associations between the presence of fast-food outlets and BMI may be weaker among individuals who never consume fast-food [47] or fatty foods. In the mediation analyses we adjusted for all potential confounders of the main analyses. In the mediator-outcome paths we additionally adjusted for (1) occupational and (2) non-occupational MVPA.
To evaluate the robustness of the results we conducted three sensitivity analyses. First, we repeated the analyses with waist-to-height ratio as the outcome. Although BMI is a common weight status outcome in the literature and is quick and easy to assess, BMI-based measures are criticised for not adequately reflecting fat mass and regional fat distribution [48]. As a result, using BMI may introduce the risk of misclassifying participants as being overweight or obese, while the elevated BMI is due to, for instance, higher muscle mass. Waist-to-height ratio more accurately reflects fat mass [49] and central adiposity, and is less susceptible to misclassification than BMI [50]. Also, waist-to-height ratio more accurately predicts chronic disease occurrence [51] and all-cause mortality [48]. Second, we repeated the analysis with only those participants recruited after January 1st, 2012 (N = 79,697), to examine the potential influence of a temporal mismatch between the measurement of exposure (2012) and outcome (2006–2013). Third, we repeated the mediation analysis by taking the frequency of fast-food consumption categorically instead of dichotomously. This allowed us to distinguish between individuals that ‘never’, ‘sometimes’, ‘often’, or ‘always’ consume fast-food.
Results
We included 149,617 participants from 3,509 neighbourhoods. The mean (sd) BMI was 26.1 (4.3) kg/m2. The mean (sd) age was 44.8 (13.1), and 57.7% of the participants were female. The percentages of participants with null, one or at least two fast-food outlets within 1 km of the residential address were 22.3%, 13.4%, and 64.2%, respectively (Table 1).
Association between the presence of fast-food outlets and body Mass Index
Participants who had one fast-food outlet within 1 km of their residential address had a higher BMI than participants with no fast-food outlets within a 1 km radius (BMI: B = 0.11, 95% CI: 0.01, 0.21; Table 2). Participants with two or more fast-food outlets within 1 km did not have a higher BMI than participants with no fast-food outlets within the same radius (BMI: B = 0.10, 95% CI: -0.01, 0.20; Table 2).
The p-value of interaction terms were 0.06 for fast-food outlet presence and NSES (two-way interaction), 0.16 for fast-food outlet presence and healthy food outlet presence (two-way interaction), and 0.01 for fast-food outlet presence, NSES, and healthy food outlet presence (three-way interaction). None of the models with interaction terms had a better fit than models without interaction terms based on the AIC.
Association between the presence of fast-food outlets and Body Mass Index, stratified by neighbourhood socioeconomic status (NSES)
The median (interquartile range (IQR)) number of fast-food outlets within 1 km in neighbourhoods of low, middle, and high SES were 7 (3–17), 2 (1–5), and 1 (0–4), respectively (Additional file 1: Table S2). The mean (sd) BMI of participants living in neighbourhoods of low, middle, and high SES was 26.3 (4.7), 26.1 (4.3), and 25.8 (4.1), respectively. Participants from neighbourhoods with low SES also had a lower income and reported more often a low educational level than participants from neighbourhoods with middle and high SES (Additional file 1: Table S2). Participants living in low SES neighbourhoods with at least two fast-food outlets within 1 km of their residential address had a higher BMI (BMI: B = 0.29, 95% CI: 0.01, 0.57; Fig. 1) than participants in low SES neighbourhoods with no fast-food outlet within 1 km of their residential address. The density of fast-food outlets was not associated with BMI among participants with middle NSES. In high SES neighbourhoods, fast-food outlet density within 1 km was borderline associated with BMI, with weaker effect sizes than in low SES neighbourhoods (B = 0.14, 95% CI: 0.00, 0.28; p = 0.07; Fig. 1).
Associations between the presence of fast-food outlets and Body Mass Index, stratified for participants living in neighbourhoods with low, middle, and high socio-economic status (based on: (1) average value of a house per 1,000 euros; (2) percentage of owner-occupied houses; (3) mean net disposable monthly income; and (4) percentage of individuals aged 15–65 years receiving assistance benefits). Associations were adjusted for age, sex, partner status, highest level of completed education, weekly working hours, income, number of physical activity facilities within 1 km, household size, number of healthy food outlets within 1 km, occupational prestige, and address density. Note: bold numbers represent associations with p < 0.05
Association between the presence of fast-food outlets and Body Mass Index, stratified by neighbourhood socioeconomic status (NSES) and the presence of healthy food outlets
For participants with low NSES, the association between the presence of fast-food outlets and BMI was not attenuated by the availability of healthy food outlets within 1 km of their residential address (Fig. 2). To the contrary, the association between the presence of fast-food outlets and BMI among participants with low NSES was more pronounced if at least two healthy food outlets were available within 1 km of their residential address (B = 0.75, 95% CI: 0.19, 1.31; Fig. 2). For participants with middle or high NSES, a clear moderation pattern by the presence of healthy food outlets within 1 km was lacking (Additional file 1: Table S5).
Association between the presence of fast-food outlets and Body Mass Index for participants living in low SES neighbourhoods, stratified according to number of healthy food outlets within 1 km. Associations were adjusted for age, sex, partner status, highest level of completed education, weekly working hours, income, number of physical activity facilities within 1 km, household size, occupational prestige, and address density. Note: bold numbers represent associations with p < 0.05
Mediation through frequency of fast-food consumption and amount of fat intake
Among participants with low NSES with at least two healthy food outlets within 1 km, associations between the presence of fast-food outlets and BMI were partly (for 3.1%) explained by the amount of fat intake, but not by the frequency of fast-food consumption (Fig. 3 and Additional file 1: Table S3). These participants who lived with at least two fast-food outlets within 1 km had a higher fat intake than those who had no fast-food outlet within 1 km (B = 1.34 g/1,000 kcal, 95% CI: 0.27, 2.42). Subsequently, higher fat intake was associated with a higher BMI (per g/1,000 kcal: B = 0.02, 95% CI: 0.01, 0.02).
Results of causal mediation analyses to investigate mediation through frequency of fast-food consumption and amount of fat intake in the association between the presence of fast-food outlets and Body Mass Index, in a subgroup of participants living in low SES neighbourhoods with at least two healthy food outlets within 1 km (N = 39,717). Associations were adjusted for age, sex, partner status, highest level of completed education, weekly working hours, income, number of physical activity facilities within 1 km, household size, number of healthy food outlets within 1 km, neighbourhood socio-economic status, occupational prestige, and address density. In the mediator-outcome associations, we also adjusted for occupational and non-occupational moderate-to-vigorous physical activity. Note: bold numbers represent associations with p < 0.05
Sensitivity analyses
Repeating the analyses with waist-to-height ratio as outcome did not affect the conclusions (Additional file 1: Table S6-S8). Furthermore, repeating the analysis with only the 79,697 participants recruited from January 1st, 2012 did not affect the conclusions (Additional file 1: Table S9-S10). Also, the findings of the mediation analysis were not affected by taking the frequency of fast-food consumption categorically instead of dichotomously (Additional file 1: Table S11).
Discussion
This study indicates that individuals living in low SES neighbourhoods with at least two fast-food outlets within 1 km of their residential address have a higher BMI than individuals with no fast-food outlet within the same radius. Rather than being attenuated by the presence of healthy food outlets, these associations were only more pronounced. The amount of fat intake, but not the frequency of fast-food consumption, explained only a limited part of the association between the presence of fast-food outlets and BMI.
The current study emphasizes the role of fast-food outlets in inequalities between individuals living in neighbourhoods with a different socioeconomic status. First, the number of fast-food outlets itself was substantially higher in low SES neighbourhoods than in high SES neighbourhoods: the median (IQR) number of fast-food outlets within 1 km for participants with low, middle, or high NSES was 7 (3–17), 2 (1–5), and 1 (0–4), respectively. This is in line with several other studies that found more fast-food outlets to be present in low NSES areas [52]. Second, the mean BMI was higher among participants from low NSES areas (26.3 kg/m2) than among participants with middle (26.1 kg/m2) or high NSES (25.8 kg/m2). Third, although we also saw a borderline significant association between fast-food outlet presence and BMI in high NSES areas, the strongest effect sizes of fast-food outlet presence on BMI were observed in low NSES areas. This may be because low SES neighbourhoods have less social capital [53] and more positive social norms that encourage eating fast-food [54]. In low SES neighbourhoods, we found effect sizes up to 0.75 of fast-food outlet presence on BMI, averaging a higher weight of 2.30 kg for a Dutch adult of average height (i.e., an average of 1.75 metre (m) for males and females combined [55]). By examining the role of SES on neighbourhood level, this study may provide a tangible platform for conducting public health interventions and contribute to a better reach of such interventions towards vulnerable groups [56].
Remarkably, associations between the presence of fast-food outlets and BMI in low SES neighbourhoods were more pronounced with increasing availability of healthy food outlets (at least two). This may suggest that healthy food outlets do not buffer the potentially unhealthy impact of fast-food outlets. On the one hand, this finding may be the result of our inclusion of supermarkets in the definition of healthy food outlets. Although in the literature supermarkets are typically considered as healthy food outlets [16,17,18,19], they also offer a wide range of unhealthy foods [57]. Even more, a study found that 71% of all promoted food products in supermarkets in the Netherlands do not contribute to a healthy diet [58]. On the other hand, this finding may be explained by self-licensing dietary behaviours [59]: healthy food outlet shopping could be used as a psychological ‘license’ to consume fast-food. Also, low SES neighbourhoods with many healthy food outlets may at the same time be urbanised areas with easy access to all types of foods. In such areas, snacking patterns may be more common [60].
Associations between the presence of fast-food outlets and BMI were only modestly explained by the amount of fat intake. The high amounts of fat in fast-food meals [22] may explain these observed mediation effects. The associations were not explained by the frequency of fast-food consumption. A reason for this could be that only a small proportion (5.9%) of individuals indicated that they ‘often’ or ‘always’ consumed fast-food. Furthermore, we did not take into account the amount of fast-food consumed. We can also not rule out differential misclassification, as the frequency of fast-food consumption was based on self-report: individuals with a higher BMI may have given socially desirable answers, and underreported their frequency of fast-food consumption [60].
Strengths of this study include its use of objectively measured BMI, its large sample size, and the overall representativeness of the study sample [24]. Moreover, the study sample came from a large rather than narrow geographical area (e.g., a city). However, this study also has limitations. Firstly, as the results are based on cross-sectional data, we cannot exclude the possibility of reverse causation. For instance, fast-food outlets may have opened selectively in areas where BMI is higher or where fast-food meals or fatty foods are consumed more often. Therefore, we cannot draw firm conclusions about the causal relationship between the presence of fast-food outlets and BMI and underlying causal mechanisms. Longitudinal studies, and particularly natural experiments, are needed to strengthen the evidence regarding the impact of the presence of fast-food outlets on BMI. Secondly, we cannot rule out the effect of fast-food delivery services, even though before 2014 the use of these services was less common than today [52]. This may have led to underestimated associations in the current study. Thirdly, we relied on straight-line distances instead of street-network distances to compute the presence of fast-food outlets. Even though there is evidence that straight-line and street-network distances correlate highly [61], this correlation may have been weaker in rural areas where a part of the Lifelines participants reside. Fourthly, even though we adjusted for address density in our analyses, we cannot rule out that results from this observational study are affected by address density due to residual confounding. In urban areas, fast-food outlets are more ubiquitous, while the average BMI is lower [29].
This study provides a deeper understanding of the role of the presence of fast-food outlets in BMI, who might be most affected, and how the presence of fast-food outlets may influence BMI. We hope that our results can be used by policy-makers to create healthier food environments. In the future, longitudinal studies are needed to strengthen the evidence on how the presence of fast-food outlets affects changes in BMI over time. Moreover, future studies should examine overweight and obesity using systems dynamics approaches. Such approaches model overweight and obesity as part of a complex system [62,63,64], and could thereby move beyond bivariate exposure-outcome associations.
Conclusions
We found that among individuals living in low SES neighbourhoods, the presence of fast-food outlets is associated with objectively measured BMI. These associations were not buffered by the presence of healthy food outlets and only modestly explained by the amount of fat intake. Our results may provide a stepping stone toward understanding the widespread pandemic of overweight and obesity, and how the fast-food environment may contribute to health inequalities.
Availability of data and materials
Researchers can apply for the data and biomaterial through a proposal submitted to the LifeLines Cohort Study. For more information, we refer to www.lifelines.nl.
Abbreviations
- BMI:
-
Body Mass Index
- cm:
-
centimetre
- FFQ:
-
Food Frequency Questionnaire
- IQR:
-
Interquartile range
- kg:
-
kilogram
- km:
-
kilometre
- m:
-
metre
- LISA:
-
Landelijk Informatiesysteem van Arbeidsplaatsen
- MICEMD:
-
Multiple Imputation by Chained Equations with multilevel data
- NSES:
-
Neighbourhood socio-economic status
- sd:
-
standard deviation
- SIOPS:
-
Standard International Occupational Prestige Scale
- SQUASH:
-
Short Questionnaire to Assess Health-enhancing physical activity
References
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944–53.
WHO. Obesity and overweight. 2018. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/#.Ws9xsurfnf1.mendeley. Accessed 12 Apr 2018.
Dobbs R, Manyika J, Chui JWM, Lund S. Overcoming obesity: An initial economic analysis. 2014. Available from: https://www.mckinsey.com/~/media/McKinsey/Business%20Functions/Economic%20Studies%20TEMP/Our%20Insights/How%20the%20world%20could%20better%20fight%20obesity/MGI_Overcoming_obesity_Executive_summary.ashx. Accessed 28 Jun 2022.
Gamba RJ, Schuchter J, Rutt C, Seto EYW. Measuring the food environment and its effects on obesity in the United States: a systematic review of methods and results. J Community Health. 2015;40(3):464–75.
Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9(6):535–47.
Mackenbach JD, Rutter H, Compernolle S, Glonti K, Oppert J-M, Charreire H, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233.
Jia P, Cheng X, Xue H, Wang Y. Applications of geographic information systems (GIS) data and methods in obesity-related research. Obes Rev. 2017;18(4):400–11.
Bennett WL, Wilson RF, Zhang A, Tseng E, Knapp EA, Kharrazi H, et al. Methods for Evaluating Natural Experiments in Obesity: A Systematic Review. Ann Intern Med. 2018;168(11):791–800.
Goris AH, Westerterp-Plantenga MS, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr. 2000;71(1):130–4.
Mason KE, Pearce N, Cummins S. Do neighbourhood characteristics act together to influence BMI? A cross-sectional study of urban parks and takeaway/fast-food stores as modifiers of the effect of physical activity facilities. Soc Sci Med. 2020;261:113242.
Algren MH, Bak CK, Berg-Beckhoff G, Andersen PT. Health-Risk Behaviour in Deprived Neighbourhoods Compared with Non-Deprived Neighbourhoods: A Systematic Literature Review of Quantitative Observational Studies. PLoS One. 2015;10(10):e0139297.
Green MA, Hobbs M, Ding D, Widener M, Murray J, Reece L, et al. The Association between Fast Food Outlets and Overweight in Adolescents Is Confounded by Neighbourhood Deprivation: A Longitudinal Analysis of the Millennium Cohort Study. Int J Environ Res Public Health. 2021;18(24):13212.
Mölenberg FJM, Mackenbach JD, Poelman MP, Santos S, Burdorf A, van Lenthe FJ. Socioeconomic inequalities in the food environment and body composition among school-aged children: a fixed-effects analysis. Int J Obes. 2021;45(12):2554–61.
Burgoine T, Forouhi NG, Griffin SJ, Brage S, Wareham NJ, Monsivais P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am J Clin Nutr. 2016;103(6):1540–7.
Burgoine T, Sarkar C, Webster CJ, Monsivais P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: evidence from 51,361 UK Biobank participants. Int J Behav Nutr Phys Act. 2018;15(1):71.
Pinho MGM, Mackenbach JD, Oppert J-M, Charreire H, Bárdos H, Rutter H, et al. Exploring absolute and relative measures of exposure to food environments in relation to dietary patterns among European adults. Public Health Nutr. 2019;22(6):1037–47.
Clary CM, Ramos Y, Shareck M, Kestens Y. Should we use absolute or relative measures when assessing foodscape exposure in relation to fruit and vegetable intake? Evidence from a wide-scale Canadian study. Prev Med (Baltim). 2015;71:83–7.
Stark JH, Neckerman K, Lovasi GS, Konty K, Quinn J, Arno P, et al. Neighbourhood food environments and body mass index among New York City adults. J Epidemiol Community Health. 2013;67(9):736–42.
Woodruff RC, Raskind IG, Harris DM, Gazmararian JA, Kramer M, Haardorfer R, et al. The dietary impact of introducing new retailers of fruits and vegetables into a community: results from a systematic review. Public Health Nutr. 2018;21(5):981–91.
van Rongen S, Poelman MP, Thornton L, Abbott G, Lu M, Kamphuis CBM, et al. Neighbourhood fast food exposure and consumption: the mediating role of neighbourhood social norms. Int J Behav Nutr Phys Act. 2020;17(1):61.
Mackenbach JD, Charreire H, Glonti K, Bárdos H, Rutter H, Compernolle S, et al. Exploring the Relation of Spatial Access to Fast Food Outlets With Body Weight: A Mediation Analysis. Environ Behav. 2018;51(4):401–30.
Bowman SA, Vinyard BT. Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23(2):163–8.
Scholtens S, Smidt N, Swertz MA, Bakker SJ, Dotinga A, Vonk JM. Cohort profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol. 2015;44(4):1172-80.
Klijs B, Scholtens S, Mandemakers JJ, Snieder H, Stolk RP, Smidt N. Representativeness of the LifeLines Cohort Study. PLoS One. 2015;10(9):e0137203.
Zijlema WL, Smidt N, Klijs B, Morley DW, Gulliver J, de Hoogh K, et al. The LifeLines Cohort Study: a resource providing new opportunities for environmental epidemiology. Arch Public Heal. 2016;74(1):32.
Scholtens G, van Gessel-Dabekaussen AAMW. Werk en vestigingen in Nederland. 2018. Available from: https://www.cbs.nl/nl-nl/achtergrond/2018/05/werk-en-vestigingen-in-nederland. Accessed 7 Jul 2021.
Mackenbach JD, Charreire H, Glonti K, Bárdos H, Rutter H, Compernolle S, et al. Exploring the Relation of Spatial Access to Fast Food Outlets With Body Weight: A Mediation Analysis. Environ Behav. 2018;51(4):401–30.
Vinke PC, Corpeleijn E, Dekker LH, Jacobs DRJ, Navis G, Kromhout D. Development of the food-based Lifelines Diet Score (LLDS) and its application in 129,369 Lifelines participants. Eur J Clin Nutr. 2018;72(8):1111–9.
van Erpecum CL, van Zon SKR, Bültmann U, Smidt N. The association between fast-food outlet proximity and density and Body Mass Index: Findings from 147,027 Lifelines Cohort Study participants. Prev Med (Baltim). 2022;155:106915.
Scholtens G. Kerncijfers wijken en buurten. 2012. Available from: https://www.cbs.nl/nl-nl/maatwerk/2011/48/kerncijfers-wijken-en-buurten-2012. Accessed 22 Oct 2018
Statistics Netherlands. Wijk- en buurtkaart 2012. 2015. Available from: https://www.cbs.nl/nl-nl/dossier/nederland-regionaal/geografische-data/wijk-en-buurtkaart-2012. Accessed 28 Jun 2021.
Thornton LE, Lamb KE, White SR. The use and misuse of ratio and proportion exposure measures in food environment research. Int J Behav Nutr Phys Act. 2020;17(1):118.
Maguire ER, Burgoine T, Monsivais P. Area deprivation and the food environment over time: A repeated cross-sectional study on takeaway outlet density and supermarket presence in Norfolk, UK, 1990–2008. Health Place. 2015;33:142–7.
Mohammed SH, Habtewold TD, Birhanu MM, Sissay TA, Tegegne BS, Abuzerr S, et al. Neighbourhood socioeconomic status and overweight/obesity: a systematic review and meta-analysis of epidemiological studies. BMJ Open. 2019;9(11):e028238.
Dutch Intitute for Public Health and the Environment. Nieuwe NEVO-tabel 2011 beschikbaar. 2011. Available from: https://www.rivm.nl/Documenten_en_publicaties/Algemeen_Actueel/Nieuwsberichten/2011/Nieuwe_NEVO_tabel_2011_beschikbaar. Accessed 24 Oct 2018.
Brouwer-Brolsma EM, Perenboom C, Sluik D, van de Wiel A, Geelen A, Feskens EJ, et al. Development and external validation of the “Flower-FFQ”: a FFQ designed for the Lifelines Cohort Study. Public Health Nutr. 2022;25(2):225–36.
Statistics Netherlands. Standaard Onderwijsindeling 2016. 2020. Available from: https://www.cbs.nl/nl-nl/onze-diensten/methoden/classificaties/onderwijs-en-beroepen/standaard-onderwijsindeling--soi--/standaard-onderwijsindeling-2016. Accessed 1 Feb 2021.
Klijs B, Kibele EUB, Ellwardt L, Zuidersma M, Stolk RP, Wittek RPM, et al. Neighborhood income and major depressive disorder in a large Dutch population: results from the LifeLines Cohort study. BMC Public Health. 2016;16(1):773.
Treiman DJ. Occupational prestige in comparative perspective. 1st ed. New York: Academic; 1977.
de Hollander EL, Zwart L, de Vries SI, Wendel-Vos W. The SQUASH was a more valid tool than the OBiN for categorizing adults according to the Dutch physical activity and the combined guideline. J Clin Epidemiol. 2012;65(1):73–81.
Byambasukh O, Vinke P, Kromhout D, Navis G, Corpeleijn E. Physical activity and 4-year changes in body weight in 52,498 non-obese people: the Lifelines cohort. Int J Behav Nutr Phys Act. 2021;18(1):75.
Bodner TE. What Improves with Increased Missing Data Imputations? Struct Equ Model. 2008;15(4):651–75.
Vivot A, Boutron I, Béraud-Chaulet G, Zeitoun J-D, Ravaud P, Porcher R. Evidence for Treatment-by-Biomarker interaction for FDA-approved Oncology Drugs with Required Pharmacogenomic Biomarker Testing. Sci Rep. 2017;7(1):6882.
Burnham KP, Anderson DR. Multimodel inference: understanding AIC and BIC in model selection. Sociol Methods Res. 2004;33(2):261–304.
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. mediation: R Package for Causal Mediation Analysis. J Stat Softw. 2014;59(5):1–38.
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–34.
Mason KE, Pearce N, Cummins S. Associations between fast food and physical activity environments and adiposity in mid-life: cross-sectional, observational evidence from UK Biobank. Lancet Public Heal. 2018;3(1):e24–33.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ. 2020;370:m3324.
Swainson MG, Batterham AM, Tsakirides C, Rutherford ZH, Hind K. Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLoS One. 2017;12(5):e0177175–e0177175.
Ljungvall Å, Gerdtham UG, Lindblad U. Misreporting and misclassification: implications for socioeconomic disparities in body-mass index and obesity. Eur J Heal Econ. 2015;16(1):5–20.
Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A Comparison of Adiposity Measures as Predictors of All-cause Mortality: The Melbourne Collaborative Cohort Study. Obesity. 2007;15(4):994–1003.
Pinho MGM, Mackenbach JD, den Braver NR, Beulens JJW, Brug J, Lakerveld J. Recent changes in the Dutch foodscape: socioeconomic and urban-rural differences. Int J Behav Nutr Phys Act. 2020;17(1):43.
Glonti K, Mackenbach JD, Ng J, Lakerveld J, Oppert J-M, Bardos H, et al. Psychosocial environment: definitions, measures and associations with weight status–a systematic review. Obes Rev. 2016;17 Suppl 1:81–95.
Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–45.
Statistics Netherlands. Dutch population taller and heavier. 2012. Available from: https://www.cbs.nl/en-gb/news/2012/49/dutch-population-taller-and-heavier. Accessed 28 Jun 2022.
Zhu Y, Duan M-J, Riphagen IJ, Minovic I, Mierau JO, Carrero J-J, et al. Separate and combined effects of individual and neighbourhood socio-economic disadvantage on health-related lifestyle risk factors: a multilevel analysis. Int J Epidemiol. 2021;50(6):1959–69.
Charlton EL, Kahkonen LA, Sacks G, Cameron AJ. Supermarkets and unhealthy food marketing: An international comparison of the content of supermarket catalogues/circulars. Prev Med (Baltim). 2015;81:168–73.
Hendriksen A, Jansen R, Dijkstra SC, Huitink M, Seidell JC, Poelman MP. How healthy and processed are foods and drinks promoted in supermarket sales flyers? A cross-sectional study in the Netherlands. Public Health Nutr. 2021;24(10):3000–8.
Prinsen S, Evers C, de Ridder DTD. Justified indulgence: self-licensing effects on caloric consumption. Psychol Health. 2019;34(1):24–43.
Dekker LH, Rijnks RH, Strijker D, Navis GJ. A spatial analysis of dietary patterns in a large representative population in the north of The Netherlands – the Lifelines cohort study. Int J Behav Nutr Phys Act. 2017;14(1):166.
Burgoine T, Alvanides S, Lake AA. Creating “obesogenic realities”; do our methodological choices make a difference when measuring the food environment? Int J Health Geogr. 2013;12:33.
Waterlander WE, Singh A, Altenburg T, Dijkstra C, Luna Pinzon A, Anselma M, et al. Understanding obesity-related behaviors in youth from a systems dynamics perspective: The use of causal loop diagrams. Obes Rev. 2021;22(7):e13185.
Sawyer ADM, van Lenthe F, Kamphuis CBM, Terragni L, Roos G, Poelman MP, et al. Dynamics of the complex food environment underlying dietary intake in low-income groups: a systems map of associations extracted from a systematic umbrella literature review. Int J Behav Nutr Phys Act. 2021;18(1):96.
Luna Pinzon A, Stronks K, Dijkstra C, Renders C, Altenburg T, den Hertog K, et al. The ENCOMPASS framework: a practical guide for the evaluation of public health programmes in complex adaptive systems. Int J Behav Nutr Phys Act. 2022;19(1):33.
Acknowledgements
The authors wish to acknowledge the services of the Lifelines Cohort Study, the contributing research centres delivering data to Lifelines, and all the study participants.
Funding
The Lifelines initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG), Groningen University and the Provinces in the North of the Netherlands (Drenthe, Friesland, Groningen).
Author information
Authors and Affiliations
Contributions
All authors were involved in designing the study. CLE performed the data management and statistical analysis. All authors were involved in interpreting the data, and critically revised, read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants filled out an informed consent form before they received an invitation for the physical examination. The Lifelines Cohort Study is conducted according to the principles of the Declaration of Helsinki, and was approved by the medical ethical committee of the University Medical Center Groningen, The Netherlands.
Consent for publication
Not applicable.
Competing interests
The authors declare to have no potential conflict of interest with respect to the research, authorship, and publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Erpecum, CP.L., van Zon, S.K., Bültmann, U. et al. The association between the presence of fast-food outlets and BMI: the role of neighbourhood socio-economic status, healthy food outlets, and dietary factors. BMC Public Health 22, 1432 (2022). https://doi.org/10.1186/s12889-022-13826-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13826-1