Abstract
Background
The Dixon-Woods et al. Candidacy Framework, a valuable tool since its 2006 introduction, has been widely utilized to analyze access to various services in diverse contexts, including healthcare. This social constructionist approach examines micro, meso, and macro influences on access, offering concrete explanations for access challenges rooted in socially patterned influences. This study employed the Candidacy Framework to explore the experiences of individuals living with rheumatoid arthritis (RA) and their formal care providers. The investigation extended to assessing supports and innovations in RA diagnosis and management, particularly in primary care.
Methods
This systematic review is a Critical Interpretive Synthesis (CIS) of qualitative and mixed methods literature. The CIS aimed to generate theory from identified constructs across the reviewed literature. The study found alignment between the seven dimensions of the Candidacy Framework and key themes emerging from the data. Notably absent from the framework was an eighth dimension, identified as the “embodied relational self.” This dimension, central to the model, prompted the proposal of a revised framework specific to healthcare for chronic conditions.
Results
The CIS revealed that the eight dimensions, including the embodied relational self, provided a comprehensive understanding of the experiences and perspectives of individuals with RA and their care providers. The proposed Candidacy 2.0 (Chronic Condition (CC)) model demonstrated how integrating approaches like Intersectionality, concordance, and recursivity enhanced the framework when the embodied self was central.
Conclusions
The study concludes that while the original Candidacy Framework serves as a robust foundation, a revised version, Candidacy 2.0 (CC), is warranted for chronic conditions. The addition of the embodied relational self dimension enriches the model, accommodating the complexities of accessing healthcare for chronic conditions.
Trial Registration
This study did not involve a health care intervention on human participants, and as such, trial registration is not applicable. However, our review is registered with the Open Science Framework at https://doi.org/10.17605/OSF.IO/ASX5C.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Access barriers for people with chronic conditions can result in delays in diagnosis, treatment, and management. These barriers can directly impact a patient’s ability to receive timely and appropriate care and increase healthcare costs [1, 2]. Although theoretical frameworks exist to guide health and community care for chronic conditions (e.g., [3]), the process of attaining a diagnosis and ongoing care for chronic conditions across the micro-to macro continuum is less well understood. The Candidacy Framework is a theoretical model that has the potential to deepen our understanding of the process of gaining access to diverse health and social services needed by people living with chronic conditions. Our study applied the Candidacy Framework to systematically examine the experiences of people living with Rheumatoid Arthritis (RA), a common chronic autoimmune disease, to comprehensively analyze barriers and facilitators in accessing a diagnosis and healthcare services [4].
Dixon-Woods et al. [4] developed the framework from an extensive scoping review and a Critical Interpretive Synthesis (CIS) of the literature on access to care by marginalized populations. O’Brien et al. [5] have since demonstrated that the framework is applicable to a wider population base of people with chronic conditions. We argue, however, that while the Candidacy Framework is an excellent starting point, a more comprehensive theory of access must also incorporate an intersectional lens and a phenomenological understanding of identity and its influences on access.
The Candidacy Framework conceptualizes healthcare access as a dynamic process wherein candidacy for care is constructed between those needing and providing services [4, 6]. This multi-level approach includes individual (patient, practitioner), interpersonal, institutional, and infrastructural factors [7], operationalized as seven distinct yet overlapping dimensions with which individuals are likely to engage in an iterative manner [6, 8].
According to Dixon-Woods et al. [4], and depicted in Fig. 1, establishing access is a fluid process that entails [1] identification of the need for care, [2] finding a way to it, (3&4) presenting a claim for it to service providers who judge its credibility, and [5] accepting or rejecting resultant offers. The ‘openness’ and compatibility of the system [6] and local operating conditions [7] are also salient, reflecting the broader organizational and socio-political or environmental conditions that influence claims to candidacy throughout a process of negotiation [7]. Application of Candidacy dimensions generates concrete and testable explanations of access challenges, which can reveal socially patterned influences underlying seemingly individual behaviours [7, 9, 10].
The Candidacy Framework has been used to analyze access to a broad range of medical and non-medical services, including those for chronic conditions such as dementia [11], fibromyalgia [12], comorbid obesity [7], diabetes [13, 14], coronary heart disease [13], multiple sclerosis [15], mental health problems [16, 17], osteoarthritis [5], and asthma and other ‘long-term conditions’ [14]. Collectively, these works have demonstrated that gaining access to a diagnosis and receiving appropriate ongoing care for chronic conditions, comorbidities and adverse effects of treatment is key to achieving positive health and social outcomes. These studies also underscore the explanatory power of the original Candidacy Framework but have inevitably suggested refinements that are not always acknowledged in subsequent applications of the framework, although some trends are apparent.
Using RA as an exemplar for an augmented Candidacy framework, we discuss the implications of our findings for an interdisciplinary understanding of access to chronic conditions, particularly those that are complex and difficult to diagnose. Drawing upon prior applications of the Candidacy Framework to analyses of primary data and systematic reviews, we propose an expanded version that seeks to capture these additional dimensions: Candidacy 2.0 (Chronic Conditions [CC]).
RA affects approximately 0.5% of the world’s population, and its prevalence is increasing globally [18]. Prevalence rates are higher in industrialized countries (e.g., Canada: 0.65–0.78%) and among women [18]. RA affects multiple joints, causing pain, swelling, stiffness, warmth, redness, fatigue, weakness, and loss of range of motion. Rheumatoid nodules may develop under the skin near the affected joints and may cause functional and/or cosmetic concerns. Systematic inflammation associated with RA may affect other organs, including nerves, eyes, skin, lungs, or heart. Symptoms vary from person to person and can come and go, with periods of more active disease commonly referred to as flare-ups. The target of treatment is disease remission; however, treatment is often complex and needs frequent reassessment to achieve this goal [19]. RA can thus have a significant impact on patients’ quality of life due to pain, stiffness, and swelling, as well as fatigue, reduced mobility, and functional disability, reduced ability to work and premature mortality, yet many gaps in care remain due in part to inconsistencies with current treatment guidelines [20].
Methodology: critical interpretive synthesis (CIS)
Our study aimed to explore healthcare access experiences of people living with Rheumatoid Arthritis (PlwRA) through the Candidacy Framework [4]. Despite qualitative studies offering valuable insights into complex issues, they comprise only 1% of research in top-tier rheumatology journals [21]. To address this gap, we conducted a systematic review using Critical Interpretive Synthesis methodology [4], focusing on qualitative and mixed-methods literature on RA care access. This approach allowed us to capture in-depth perspectives of both RA patients and their care providers, offering insights that quantitative studies alone might miss. Qualitative methods, such as interviews and focus groups, are uniquely suited to explore the nuanced, contextual aspects of patient experiences [22]. Our review also examined supports and innovations in RA diagnosis and management, particularly in primary care settings.
A CIS differs from a conventional systematic review by emphasizing the inclusion of diverse study types, beyond randomized controlled trials, to capture a broader range of evidence [4]. CIS incorporates a more interpretive and reflexive approach, encouraging researchers to critically engage with the context and complexities of the included studies. Unlike traditional systematic reviews that focus on aggregating quantitative data, CIS prioritizes the synthesis of qualitative and quantitative evidence, allowing for a more nuanced understanding of the research topic. Additionally, CIS places a greater emphasis on exploring underlying mechanisms and contextual factors, promoting a deeper and more holistic analysis of the subject matter.
A CIS improves on the meta-ethnographic approach [23, 24] typically employed in reviews of qualitative literature (1) by utilizing systematic review search strategies, and (2) by seeking to produce more generalizable theoretical conclusions, rather than a simple synopsis of the literature reviewed [4, 25]. This is achieved by an inductive approach to analysis that integrates different theoretical categories to achieve deeper understanding of the topic of interest [25]. Thus, while the review focuses on the literature on RA access, this informs a more general theory of access to care for multiple chronic conditions.
Search and sampling process
Within a CIS, question formulation, source search and selection, and analysis are dynamic and iterative processes [25]. The search and sampling process involves selecting a set of guided topics, iteratively identifying ‘probably relevant articles’ through a range of searching strategies that are ‘fit for purpose’, and sampling purposively relative to an emerging theory [4].
Articles reporting qualitative and mixed method studies were identified from multiple database searches in Medline (OVID) and CINAHL by a health sciences librarian using the terms detailed in Appendix A: Search Terms (see supplementary file 1) and based on our inclusion criteria (Table 1). The data bases were searched from their date of inception to search dates ranging from April 12, 2020, to June 13, 2022. Dixon-Woods et al. [4] advocate for refining database searches in critical interpretive synthesis to ensure relevance to guiding questions. This iterative approach aligns with CIS’s flexible nature, allowing researchers to adapt their strategy as understanding evolves and focus on obtaining the most pertinent literature for theoretical development. Thus, searches were added and refined to better reflect the breadth of articles needed to comprehensively understand all dimensions of access, e.g., to address a paucity of references to allied health professionals.
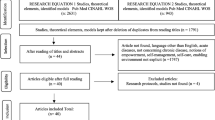
A total of 1244 articles were identified through database searches (see Fig. 2). An additional five articles were identified by experts on our team, after their review of our list of articles to be screened in full. Team members include PlwRA, primary care physicians, and rheumatologists as well as researchers with backgrounds in physiotherapy, social epidemiology, health services research, and medical anthropology. Database-identified references were imported into Covidence [26] and reviewed by two investigators (AP and SK) until all conflicts in classification (i.e., include or exclude for full-text screening) were resolved. Following Dixon-Woods and colleagues [4], we prioritized papers based on relevance rather than specific study types or strict methodological standards, aiming to include a wide variety of papers at the conceptual level. While our priority was to review the qualitative literature that focuses on patient experience we chose to include three highly relevant review articles [27,28,29] and four quantitative studies [30,31,32,33] that addressed, to a degree, gaps in understanding in the qualitative record. We set a low inclusion threshold, excluding only fatally flawed papers. The concept of “fatally flawed” as a criterion for excluding articles in a CIS refers to studies with severe methodological deficiencies. These include lacking clear aims, having an inappropriate research design, failing to explain its process clearly, providing insufficient data to support conclusions, or using an inadequate or poorly explained analysis method [4]. Such flaws significantly undermine a study’s credibility and contribution to the synthesis. In our study, this judgement occurred primarily at the abstract screening stage, although 20 articles were excluded for this reason at the full article screening phase (denoted as ‘wrong study design’ in Fig. 2).
Of the 1093 abstracts reviewed, 307 articles were deemed eligible for full-text screening (by SK) of which 10 could not be retrieved. 111 articles were subsequently excluded, as detailed in Fig. 2. The exclusion process was in fact iterative since nine of the articles excluded were withdrawn during the analysis phase within NVivo, when their lack of fit with our guiding questions and inclusion criteria became apparent. Ultimately, any study deemed unlikely to contribute to our development of a theory that answers the guiding questions was excluded. In accordance with PRISMA guidelines, these articles were subcategorized in the flow chart as wrong population, language, setting, outcomes, etc.). ‘Wrong setting’ refers to contexts outside of the scope of enquiry relevant to a North American context (e.g., a discussion of patient experiences of Traditional Chinese Medicine care for RA in China). ‘Wrong outcomes’ indicates that the study did not specifically report on either the health and health care experiences of people with RA. One article was a protected PDF that did not allow for text selection and coding in NVivo. Since it was a marginally relevant study, we chose to exclude it. Studies with mixed populations were included if patients with RA were part of the study sample. Another 76 articles were demoted to a secondary list because their focus was not on experience. Ultimately, our sample included 110 multidisciplinary articles employing diverse theoretical approaches (see Appendix C in supplementary file 2, a framework summation of methodological features of sampled literature).
Through the process of familiarization with the materials and consultation with our advisory panel (five people living with RA across Canada)Footnote 1 and RA experts on our team, we refined our overarching question into the five guiding topics that ultimately determined the selection of articles included in the review (Table 2). Our topics were further informed by the Candidacy Framework for understanding access to healthcare services.
Data analysis
The inductive approach of a CIS consists of several phases. The first phase of the analysis is the development of a synthesizing argument through reciprocal translational analysis, which involves the translation of different concepts into each other [4]. Two studies often discuss the same construct using different terms or use a common term to which each study ascribes a different meaning. Thematically coding all sources of evidence using qualitative data management software, QSR NVivo 12®, facilitated this process. SK led the analytic phase but met regularly with the research team’s CIS subcommittee comprised of the remaining authors. Emergent codes and interpretations were discussed with and contextualized by this group and were refined accordingly.
All categories and the nodes within them are listed and described in a codebook (Appendix B, supplementary file 1). The analysis employed both deductive and inductive coding methods. Deductive coding was guided by the Candidacy Framework, which provided a structured lens for examining access to healthcare services. Inductive coding emerged organically from the interview data, allowing new themes and insights to surface. The inductive nodes were ultimately grouped as subnodes of each of the Guiding Topics. Two additional node families—‘healthcare provider roles’ and ‘treatment effects’—were created to accommodate relevant topics that did not fit comfortably within any of the Guiding Topics. Most extracts of pertinent text were coded at multiple nodes, which allows for explorations of associations among them using the Matrix feature of NVivo 12®. For example, the Guiding Questions nodes are often coded as well with Candidacy Framework nodes which allows us to discern which dimensions of Candidacy are most salient for each of the Guiding Questions.
Our reciprocal translational analysis generated an aggregative synthesis of the reviewed literature, although it is distinct from most aggregative reviews in that each article is viewed more as a “repository of concepts” than a source of data per se [34]. We provide both a condensed review of the dominant themes in tabular form as well as a detailed and cited account of these themes in supplementary file 1.
The next phase of CIS analysis—refutational synthesis—involves characterizing and explaining the contradictions between constructs in different studies (e.g., in terms of different study approaches, conceptual assumptions). To facilitate ready access to study details that could explain such discrepancies we created a ‘Methodology’ code category that included the subnodes data collection method, limitations, location of study, sample size, study question or purpose, target population of study, and theory or framework. Using the “framework” feature in NVivo 12®, we generated a tabular summary of these details for each study that could be readily checked to potentially explain anomalies in our findings or as a resource for others (supplementary file 2).
The final phase is the lines-of-argument synthesis, which aims to create a comprehensive explanatory proposition suggested by the data [4]. This final interpretation is grounded in the constructs included in the reviewed materials, and seeks to identify and reconcile the most influential themes that represent the combined data [35]. This process ensures a robust and well-supported understanding of the phenomenon under study. Coding text at both Candidacy nodes and Guiding Questions subnodes systematically connected the ideas more specific to the RA experience represented by the Guiding Questions to the dimensions of access described by the Candidacy Framework and identified what was missing in this framework.
Results: making sense of access to RA care through a candidacy lens and beyond
The Candidacy Framework offered a relatively inclusive ecological approach that served as a useful starting point for the development of lines of argument that broke down the process of access to RA care into seven dimensions of access. All seven dimensions could be identified in the literature, but some were more thoroughly explored than others, pointing to opportunities for additional inquiry into these areas. Our interpretations were derived from text coded in NVivo 12® at different dimensions of Candidacy, many of which were co-coded with the themes emerging as important in association with each of the Guiding Questions (presented as Findings in supplementary document 1).
However, the explanations associated with the different dimensions of Candidacy for limitations to access did not suffice to explain findings that linked the bilateral relationship between illness and identity to access challenges. We recognized the need to augment the Candidacy Framework dimensions with insights from phenomenological and intersectional theories. The following interpretation of the CIS analysis will include a consideration of the intersectional, relational and embodied self to enhance the explanatory power of Candidacy as a theory of access.
Identification of RA
The first step in securing access to care is recognition of the need to seek out medical attention. A common pattern emerged in all studies that focused on initial help seeking whereby symptoms were rationalized in relation to preceding events or current conditions, such as an accident, pregnancy, too much or too little exercise, exposure to heat or cold, consuming certain foods, comorbidities, changes in medication, and so on [29, 36,37,38,39,40]. At some point, however, these explanations no longer accounted for the persistence or evolution of symptoms, and medical advice was sought [40]. Alternatively, some explanations of symptoms, such as a curse, were culture-specific and could prompt consultation of non-medical (e.g., religious) practitioners, or remedial actions such as prayer or a change in diet that further delayed consultation [29, 39, 41]. Importantly, family members could be instrumental in either advising recourse to alternative explanations and remedies or persuading the afflicted person to seek medical advice [42,43,44].
Regardless, delays in consultation due to failure to recognize the symptoms of RA were attributed in retrospect to a lack of knowledge: “had they known when they developed their symptoms what they knew once they had been diagnosed with RA, they would have consulted much earlier” (43, see also 29). Numerous studies reported that laypeople have little if any knowledge of RA and are unaware that it is a serious degenerative disorder requiring aggressive treatment to prevent irreparable damage [29, 40, 45,46,47,48]. Similarly, failure to recognize the symptoms of foot problems associated with RA, as well as confusion around who to consult or how to access podiatry services resulted in delayed access and potential damage [49,50,51]. Ultimately, the evidence pointed to the inadequacy of information available to the public about RA, its expression, and treatment [43, 46, 48, 50, 52]. Primary care practitioners who were asked to comment on the viability of campaigns to promote rapid help-seeking behaviour at the onset of RA were nonetheless wary of the impact of a poorly designed campaign on their workload and the possibility that false presentations would “‘clog up’ the referral pathway for genuine cases of RA” [53].
Navigation to services
Navigation through a Candidacy lens refers to the process of finding appropriate services and physically navigating to them. Navigation challenges were rarely and only superficially addressed in the reviewed literature. Once they had identified the need for medical attention, participants in most studies consulted their primary care physicians, with variable success in securing a referral to a rheumatologist [29, 36, 54, 55]. Of note were reports of “proactive” patients who had been able to find information on the internet and self-advocate for referrals or shorter wait-times, sometimes through recourse to private care [36, 39, 55,56,57]. While not explicitly explored in these studies, the ability of some to more effectively navigate the system invokes Bourdieu’s notion of social capital whereby symbolic power is gained by some actors due to their access to higher levels of economic, cultural and symbolic capital (e.g., income, education, familiarity with the healthcare system) in different social spaces [58]. Navigating to other specialists identified by PlwRA as important to their care, such as podiatrists and psychologists, was just as challenging [59]. Barriers identified were a lack of information about their roles, the lack of clear pathways to care, and the limited availability of RA-informed specialists [51, 60]. Barber et al. [61] recommended the development of a peer navigation system to expedite information gathering about the disease or the healthcare system.
Appearances and adjudications (the patient-care provider interaction)
Once a PlwRA has successfully navigated to a care provider they need to present their symptoms in a manner that precipitates some kind of offer, such as a referral, screening, or treatment. These ‘appearances’ are often difficult to identify without reference to the adjudications or decisions made by the care provider positioned to make such offers. Adjudications are based in part on the clarity of the claim to care made by the PlwRA, but the provider’s own training and biases also play a role.
Appearances or presentation of RA symptoms
Evidence on appearances of people seeking diagnosis or care from gatekeepers such as primary care physicians underscored the relevance of considerations of social capital and reflected the importance of considering sampling bias. In some studies, participants saw themselves as team members engaged in a bilateral relationship with their physicians in which the PlwRA’s expertise of their own bodies was on a par with the physician’s professional expertise [47, 62]. Confident ‘expert’ patients were more likely to access information on the internet and request blood tests for RA and hence secured a diagnosis or referral to a rheumatologist more expediently [36, 55]. The confidence needed to assume the role of expert patient sometimes derived from prior familiarity with RA [36]. Firth et al. [51] maintained, however, that patient education could also build self-efficacy to develop PlwRAs’ confidence to proactively seek solutions. Given the common expectation that the ‘Expert Patient’ can self-manage their disease, Townsend et al. [52] suggested that the failure to adequately inform patients about RA is ethically problematic; without adequate knowledge or support, the potential for benefits is limited, whereas the likelihood of harm is increased.
Subsequent to diagnosis, Laires et al. [46] found that many PlwRA had limited awareness of treatment options and typically had a passive relationship with their physicians characterized by unilateral decision making. PlwRA, healthcare professionals, and decision-makers participating in a focus group identified those with lower SES as being less assertive in their relationships with physicians and therefore less likely to gain a prompt referral [45]. More passive patients hesitated to raise their concerns about sources of pain or discomfort needing treatment for fear of being ‘a nuisance’ or because they viewed themselves as a ‘coper’ or ‘stoic’ and preferred not to ‘complain’ [42, 50, 63, 64]. Flurey et al’s [63] study of British men with RA highlighted the gendered nature of stoicism among them. However, the culturally-mediated and cohort-specific nature of this orientation is also salient [65, 66]. Some studies found that past experiences of sexist or racist treatment by healthcare providers influenced the presentation and healthcare preferences of PlwRA [64, 67]. To address such constraints, studies recommended that healthcare providers afford their patients sufficient time to express themselves, pay attention to patient context and increase patients’ health literacy [68, 69].
Adjudications
Access to RA care may be influenced by the biases of primary care providers, or patients’ anticipation of such biases based on prior experience. Some biases were widely shared by providers and patients alike. For example, several studies found that primary care providers were less likely to suspect RA, an inflammatory arthritis, as a possible diagnosis among younger patients because ‘arthritis’ is perceived as a normal part of aging and is not associated with the young; this view also prevented them from taking a proactive approach to the symptoms of RA in older patients [45, 54, 55]. The scarcity of or distant location from specialists and other resources also inhibited some primary care practitioners from referring patients to them [45, 70, 71]. Patients who were overweight or consumed excessive alcohol delayed medical consultations in anticipation of the physician’s attribution of their symptoms to their behaviours, which triggered feelings of guilt [29, 40].
Thurston et al. [67] reported that healthcare providers who did not regularly work with Indigenous patients attributed their perceived lack of buy-in to medical treatment of their RA to a lack of education about the value of specialists and their services. However, the evidence pointed instead to the historical treatment of Indigenous peoples that has undermined their trust in Western institutions, and cultural constraints such as family obligations that prevented Indigenous PlwRA from attending appointments or establishing concordance with treatment plans [67, 69, 72].
The most frequently reported cause of treatment delays, according to PlwRA, was a gatekeeper—usually a primary care provider—who lacked the expertise, time or consideration to recognize their signs and symptoms of RA [36, 39, 46, 50, 64, 70, 73,74,75,76,77]. Lopatina et al. [78] have advocated for improved access to information and resources on RA for primary care practitioners to this end. Some studies emphasized that delays occurred because primary care physicians viewed themselves as gatekeepers to scarce secondary services and, hence, to integrated care [71, 73]. Some authors advocated for the greater availability or awareness of diagnostic tools [46, 73, 76]. More commonly, though, patients identified the importance of physicians who took a person-centred approach that resulted in better health outcomes. This entailed the affordance of mutual respect through bilateral communication and inclusion in treatment decisions; such physicians saw them in the context of their whole lives, not just in terms of their disease [42, 52, 61, 62, 64, 67, 69, 71, 75, 79,80,81].
Acceptance and resistance of offers (diagnosis, screening, treatment)
So far, we have seen ample evidence of the Candidacy Framework premise that “accomplishing access to healthcare requires considerable work on the part of users, and the amount, difficulty, and complexity of that work may operate as barriers to receipt of care” [4]. Ultimately, people seeking care aim to secure an offer of some kind. This may be a prescription, a treatment plan, a referral to a specialist or for screening. Yet receipt of an offer does not guarantee access because the ability or willingness to accept the offer may depend on a great many factors such as proximity, affordability, and cultural congruence. This dimension of Candidacy was by far the most densely coded. Of the nodes cross-coded with this dimension, ‘medications’ and ‘exercise and physiotherapy programs’ were most populated.
Medications
The pain and disability experienced by PlwRA, especially during flares, was reported as extreme to the extent that some had contemplated suicide [59, 60, 76], and the relief that the appropriate prescription of DMARDS and/or biologics can bring was described as ‘dramatic’ and life-changing’ across multiple studies [80, 82,83,84,85,86]. Thus, the offer of therapeutic drugs for RA is typically accepted, albeit with some reservations: “Most felt or had been told that they had no choice other than to take potentially toxic drugs to alleviate their symptoms or to slow down the deterioration of their chronic condition” [64].
Yet arriving at the point of relief was often a long and painful process of trial and error to find the right combination of medications ([75],e.g., [87])—there was no ‘one size fits all’—which, in turn, took a toll on the PlwRA’s mental health [60]. PlwRA for whom effective medication had all but eradicated their symptoms hesitated to taper or temporarily discontinue it to resolve an infection, for fear that the intensity of the flares could increase and the drug would no longer be as effective upon resumption [49, 88,89,90], although in principle, they were willing to try. While some temporarily opted out of taking DMARDS and biologics due to their incompatibility with their reproductive goals [91], others had relinquished the possibility of conceiving because they felt unable to cope without these medications [60].
Adherence to pharmaceutical treatment for RA was highly variable, ranging from 30 to 80% [33, 92]. Multiple studies explained non-adherence in terms of the burden of administration and monitoring DMARD/biologic treatment, which required a considerable commitment from PlwRA [44, 71, 91, 93,94,95]. Side effects of the drugs were also found to negatively the PlwRA’s wellbeing and add another level of healthcare complication [44, 68, 84], (e.g., [91, 96, 97]). Ultimately, the extent to which PlwRA perceived their medications to be helpful or harmful exerted the greatest influence on their acceptance or resistance to treatment [92, 93]. Some had tried multiple medications with limited or no relief or recovery of their prior capacity and quality of life [54, 84, 86, 94, 96, 97], or the effectiveness of any treatment was short-lived [44]. It should be noted, however, that the introduction of new more efficacious treatments has decreased the risk of negative outcomes such as joint arthroplasty, excess mortality or adverse pregnancy outcomes following parental exposure to DMARDs [98,99,100].
Considerable evidence points to resistance as partial rather than absolute. Most commonly, PlwRA decided to ‘take control’ of their disease by varying the dose according to their perceived need, periodically abstaining from certain medications [38, 63, 64, 92], or utilizing complementary and alternative medicine or over-the-counter drugs [29, 38, 43, 44, 54, 59, 64, 67, 92, 93, 97, 101,102,103]. Studies found that the understanding of the mechanism of action of DMARDs and biologics, was often poorly understood by PlwRA; in particular, they did not understand the preventive value of the medications [38, 93]. Moreover, they did not understand the harms of long-term use of glucocorticoids like Prednisone [38, 91]. A patient-initiated self‐monitoring service for PlwRA on methotrexate was well received in the UK, in large part because the training they received to prepare them to monitor and initiate the drug themselves “increased their knowledge of arthritis, their treatment, the reasons for regular testing and the meaning of test results” and thus “enabled them to gain a sense of control and ownership over their arthritis” [95]. This speaks to the importance of the provision of person-centred information and education to address harmful misconceptions.
Exercise and physiotherapy programs
Engagement in exercise programs benefitted PlwRA physically and psychologically and contributed to participants’ empowerment and their ability to manage RA [104, 105]. However, exercise programs tailored to the needs of PlwRA were reportedly scarce [61] and many home exercise programs were viewed as boring and difficult to prioritize [106].
Studies of RA-tailored exercise programs have identified some key components that increase uptake and maintenance of an exercise routine. These include expert person-centred guidance, flexibility, and sensitivity to and accommodation of RA-specific limitations.
Successful programs were typically moderated by a physiotherapist or other exercise professional with the expertise to guide participants through the challenges of pain or fatigue, even when the program was largely participant-led [104, 107]. This guidance was especially important for those unfamiliar with exercise [108], but was also valued for broad-based feedback and back-up, particularly when participants needed to adjust their routines or increase their exercise load [105, 109, 110]. Professionals who took a person-centred approach, recognized the need for PlwRA to feel heard, and adopted a holistic approach to symptom management were especially valued [108,109,110,111].
Flexibility in programming was appreciated by PlwRA and took many forms. Some programs were customized so PlwRA could exercise at home and fit the exercises into their normal routines [104, 108]; being able to modify exercises to their own pace, limitations, and goals (which may vary on a daily basis contingent on disease activity), was also important (104, 108, 110, 111). PlwRA were often afraid to participate in exercise if they believed it would cause pain or they may not be able to get in and out of exercise positions, and adherence to exercise programs often waned as participants experienced flares, fluctuating symptoms or medication changes [104, 105, 111]. Programming must therefore be sensitive to these fears and adapted accordingly.
Permeability of the healthcare system
Permeability invokes the metaphor of the passage of fluid through material, with slower transmission representing the more stringent qualifications of candidacy (e.g., the need for a referral, lack of cultural alignment) needed to gain access to the healthcare system, and rapid transmission representing easier processes of access [4]. In our sample, evidence of healthcare system impermeability was primarily found in accounts of untimely delivery of care that disrupted continuity. New models of care were proposed to increase system permeability.
The benefits and challenges of different approaches aimed at increasing system permeability according to the reviewed literature are summarized in Table 3. These characteristics were often reported in combination.
Local operating conditions
The final dimension of Candidacy considers local influences on the ability of the person needing access to services that may extend beyond the healthcare system [4]. There is ample evidence in the reviewed literature that access to care for RA is especially compromised for those living in rural and remote areas, in which people who are low-income and Indigenous populations in Canada are disproportionately represented [61, 72].
Primarily, access in remote areas was found to be limited because of the absence or low representation of all types of healthcare providers from primary care providers to rheumatologists as well as other specialists and allied health professionals to whom access is needed for optimal care of RA [32, 45, 46, 61]. As a result, PlwRA faced long drives to access these services. For example, more than half the PlwRA in rural and northern Saskatchewan (a Canadian prairie province) had to drive an hour or more to access primary care providers, Physical Therapy (PT) and Occupational Therapy (OT), pharmacies, labs and medical imaging facilities, and > 25% travelled 4 + hours to see a rheumatologist [32]. In addition to distance, factors such as weather, road conditions and maintenance, a lack of transportation and the need to arrange childcare compromised PlwRAs’ ability to access care [32].
PlwRA also had to absorb multiple out-of-pocket costs for fuel or other transportation, childcare, overnight accommodation, etc. Some PT and OT services external to hospitals or outpatient services were also not covered by medical insurance for many, hence affordability of care was a barrier despite Canada’s universal healthcare coverage [32, 75]. Also missing in these communities are resources such as community pools or rehabilitation centres needed for optimal RA care [45]. The availability of potential solutions to address access limitations in these communities, such as traveling clinics, telehealth, and patient travel grants was found to vary by province. The viability of each was hampered by lack of available staff, lack of patient buy-in, and low cost-effectiveness, respectively [61].
Even outside of rural and remote areas, local influences can affect access to care. Hand et al. [27] noted that access to services could be compromised for low-income seniors when cost-saving policies resulted in housing that was poorly situated (e.g., on a hill, near a highway, far from services). These authors also reported that despite protective policies, employers did not always cooperate with accommodations for modified working arrangements to facilitate a PlwRA’s ability to return to work.
Beyond candidacy – the embodied self
Candidacy focuses on the negotiation of access at micro, meso and macro levels, but none of its dimensions fully capture how the identities of PlwRA are challenged by illness experiences and the ways in which access is consequently compromised. This understanding emerges from our sample, in part, because of the phenomenological/phenomenographic approach adopted by 18 of the reviewed studies, for which the focus was on meaning-making. Yet evidence of the same is found across studies with diverse methodological approaches. These findings speak to Kleinman’s [117] emphasis on the importance of understanding illness as an embodied experience, rather than just a set of symptoms or diagnostic criteria. Kleinman argued that illness is not just a matter of biological dysfunction but is also shaped by a person’s cultural and social context, as well as their own subjective experiences and meanings. Similarly, Bury [118], who conducted his research with PlwRA, viewed chronic illness as a biological disruption, in the face of which people were forced to reappraise their selfhood as intimately bound to the body. To this, Goodacre [119] added the importance of the social interpretation of self. Both Charmaz [120] and Ratcliffe [121], influenced by Merleau-Ponty, spoke to the loss of identity and self that could arise from bodily disruptions. A profound sense of loss is apparent in PlwRA’s accounts of flares or the effects of pain, deformity and immobilization caused by RA in which not only the body but the mind and sense of self are profoundly affected by the illness (e.g., [28, 31, 37, 49, 60, 68, 83, 86, 91, 94, 107, 109, 122]).
Consistent with Martin’s [123] work on how women’s culturally-informed and gendered identities are affected by illness, and sources of women’s power in the body discussed by Chrisler et al. [124], women with RA in several studies detailed identity compromises. Illness affected their appearance and sexuality (e.g., [49, 109, 125]). It also hindered gendered roles like housework, food preparation, and childcare [76, 85, 126,127,128,129]. Yet, some studies reported women exhibiting stoicism [55] and facing peer exclusion [87], akin to patterns more commonly found among men [63]. This highlights the importance of adopting an intersectional approach, wherein identities (e.g., age, gender, SES, rural/urban residence) and concomitant experiences of social domination are seen as intertwined with a compounding effect [130, 131].
Additionally, the identities of PlwRA could be supported or undermined by members of their social networks. People who understood their challenges and offered necessary support, without undermining the PlwRA’s self-determination, promoted their identity and facilitated coping [27, 37, 83, 128, 129]. Others undermined their sense of self and personal value by dismissing their suffering or assuming control over them [60, 83, 102, 108, 128, 129, 132].
A PlwRA’s selfhood must therefore be understood in relation to their embodiment of illness (RA and comorbidities), their intersections of identity (e.g., gender, SES, age) and the nature of their relationships with close others. In the studies reviewed, the PlwRA’s selfhood primarily undermined access through the effect of identity loss on their mental health, expressed variously as embarrassment, shame, and loss of self-esteem, power and control [31, 60, 133], which in turn led to self-isolation and societal withdrawal [37, 57, 59, 68, 91, 134]. PlwRA were thus impeded from seeking the help they needed, which could further undermine their mental and physical health [28, 63, 85, 94, 109, 127]. Kristiansen and Antoft [135] reported on a program for PlwRA that overlooked the debilitating effect of RA on self-esteem and thus further undermined it. “Narratives of chaos” created by illness in relation to identity, as theorized by Frank [136], were also evident in the efforts of some PlwRA to ‘gain control’ of their illness and hence their sense of self by resisting or modifying treatment [38, 63, 64, 91, 132]. Some supplemented or replaced biomedical treatments with complementary and alternative medicines (CAM) in ways that were detrimental to their health [59, 97, 103]. While CAM use can indicate patient engagement and a proactive stance to treatment, it sometimes reflected an uninformed approach to medication resistance. Other such examples were suspending medication while on vacation to permit greater alcohol intake [63] or substituting medication with unconventional remedies (e.g., horse liniment) [44] that delayed access and compromised health outcomes.
To summarize, we illustrate in Table 4 the seven dimensions of Candidacy plus the embodied self with brief descriptions, based on our CIS, of factors that promote (✔) and limit (✘) candidacy in each.
Discussion: extending a theory of access to care for chronic conditions: candidacy 2.0 (CC)
Previous applications of the Candidacy Framework have suggested the addition of supplementary constructs to enhance the theory. Most notable among them are recursivity [137] and concordance [138], the importance of intersectionality theory [139] and the relational nature of negotiations of candidacy [10]. Our findings not only support inclusion of these concepts, the centrality of the embodied self in the model facilitates their integration as components rather than adjuncts of candidacy and suggests the need for an enhanced Candidacy 2.0 model.
Selfhood can be challenged by chronic disease, comorbidities and treatments that may have severe side-effects. A person’s identity facilitates their creation of meaning, which is a central tenet of mental health [140]. The relationship between illness and selfhood can be cyclical when challenges to selfhood due to pain, disability or extreme fatigue, for example, result in deteriorating mental health. This, in turn, has a bidirectional relationship with social isolation and withdrawal [141, 142].
Yet the self is not a blank slate: rather it is composed of multiple intersecting identities that are more or less privileged in the societal context in which the person living with a chronic condition is embedded [141, 143]. The compounding effect of these identities and societal expectations of and responses to them shapes the extent to which illness-related changes to physical features, sexuality, or the roles that people perform are important to them and the meanings that they ascribe to their illness and its effect on their selfhood [144, 145]. In parallel with Mackenzie et al. [139], we identified the positive or negative influence of intersecting identities on the ability of people to establish candidacy in the articles reviewed for the CIS, especially in the dimensions of navigation and appearances. The addition of an intersectional lens facilitates a more nuanced understanding of help-seeking behaviours and acceptance or rejection of treatment: gender matters in its own right, for example, but it also interacts with other identities and social determinants of health to influence these behaviours [143]. Intersectional awareness achieved through the integration of candidacy and intersectionality also offers policy makers and practitioners “a means of enhancing knowledge of how the political becomes enacted in the personal” [139].
Intersecting identities also influence the extent to which a person is likely to reach ‘concordance’ (i.e., agreement with care providers about the problem and best solutions) and engage in shared decision-making with them [138]. The importance of concordance in the establishment of candidacy has been recognized in multiple studies [16, 17] and corresponds well with the original construct of permeability whereby “the service provider’s alignment with service users, including personality, gender, and ethno-linguistic characteristics” facilitates access at the organizational level [11]. However it is only when intersectionality and candidacy are united that we can fully appreciate how “discordant healthcare encounters are not simply a manifestation of essential cultural differences between the two parties but are shaped by factors that emanate from a complex interplay of historical and contemporary discourses, inequitable structures, multiple intersecting identities and past experiences” [146]. In the CIS sample, this is illustrated most clearly with reference to experiences of access to RA care by Indigenous people, immigrants and refugees, the frail elderly and people who are low-income or live in rural and remote areas; importantly, people are often marginalized by the intersection of two or more of these identities [67, 69, 72].
Intersections of identity also influence the degree of agency that people can exercise. As Chase et al. [6] point out, Dixon-Woods et al. [4] originally conceived of the establishment of candidacy as a ‘negotiation’ between patients and healthcare providers, but this underestimates the power differentials between them that can undermine the agency of people at marginalized intersections of identity, effectively foreclosing any true negotiation and reducing candidacy. For example, asylum seekers who encountered discriminatory and unjust treatment when applying for services were subsequently more likely to pay out of pocket and showed greater reluctance to seek further help or even information [6]. Similarly, in the articles reviewed for our CIS, we saw multiple examples of curtailed interaction with health professionals due to diminished trust arising from what were seen as biased adjudications rooted in power differentials between healthcare providers and PlwRA at marginalized intersections of identity (e.g., low SES, Indigenous, etc.). This phenomenon is identified as ‘recursivity’ [137]: “the interdependency between a user’s experiences of health services and her/his future actions in regards [sic.] to health and help seeking” [16]. Thus “the key determinants of patient choice of healthcare are social and diachronic” [14]. The outcome of reduced candidacy due to negative recursivity in the CIS data and in Koehn et al’s dementia study [11] was most apparent in people’s resistance to offers but was also seen in their interactions with healthcare providers (appearances and adjudications). For example, Machin et al. [81] suggested that PlwRA’s perception of their primary care practitioner as too busy and primarily focused on physical over mental health provoked anxiety and recursively prevented them from discussing mood or seeking assistance to locate mental health resources in subsequent consultations.
The connection of recursivity to the embodied self was illustrated by Flurey et al. [63] who reported that the selfhood of men living with RA, already diminished by their inability to work and perform other roles central to their masculinity, was further degraded when physicians did not take their medical complaints seriously. In response they sought to recover some sense of control by reducing medications, and engaging in excessive exercise or alcohol consumption, and only consulted the physician as a last resort. The permeability of services is also implicated in recursivity as illustrated by Hunter et al.’s [14] finding that people with ‘long-term conditions’ are frequent users of emergency care services for illness exacerbations because they provide the most expedient access to needed care and technology. Dixon-Woods et al. [4] have described emergency care as the most permeable healthcare service which, as a result, tends to be utilized more frequently by the most vulnerable members of society, thus underscoring the importance of the inclusion of an intersectional lens. These examples further emphasize Kovandžić et al.’s [17] point that recursivity is important because it unites the concepts of access to and utilization of healthcare services. Rather than viewing recursivity and candidacy as separate processes [14, 16, 17], we propose that recursivity be understood as an integral component of the process of establishing candidacy that reflects the relative agency of people living with chronic conditions at different intersections of identity as they attempt to negotiate access across its different dimensions.
Another key element to arise from the articles included in this CIS is the potential for family, friends, and the broader social network of the person with a chronic condition to either promote or undermine their self-determination and personal value. The notion of an interdependent or sociocentric self, whereby the self is viewed “not in terms of one’s independence from others, but rather by one’s connection to them” [147] is more commonly attributed to non-Eurocentric cultures, yet examples of this interdependence between PlwRA and their social networks abound throughout our CIS sample. The influence of the social network on candidacy is also apparent in other analyses utilizing the framework. For example, family members who may have more social capital than the person with a chronic condition, particularly dementia, are more likely to identify the need to seek medical attention, facilitate navigation to care, and convey observed symptoms to family physicians and other gatekeepers [11, 14]. Accordingly, we propose that the embodied self or personhood conceived as central to the Candidacy 2.0 model is necessarily understood as relational.
The centrality of the intersectional relational self in the enhanced model also makes sense in relation to the abundance of evidence that person-centred interactions, information, and service configuration are key to addressing many of the access challenges faced by PlwRA and, we would argue, people living with chronic conditions in general. Candidacy 2.0 provides a strong explanatory framework that maps out why this is the case. Focusing attention on selfhood in the Candidacy model further reinforces the importance of understanding movement through the dimensions of access as iterative, not only because the need for care among people with chronic conditions is ongoing, but because, as Saari [140] reminds us, “meaning systems must be constantly maintained and amended so that the content will fit with the context and experience of the present. The processes of the self must therefore be active in creating and altering meaning throughout life.” This in turn serves as a reminder to those designing and delivering person-centred systems and care that the ‘person’ is not a static entity, and their values, needs and goals of care may well shift over time.
Figure 3 depicts the movement of the intersectional relational self through each dimension of candidacy. Appearances and adjudications are inextricably linked, while permeability is characterized as a barrier with variable holes through which some of the offers made by gatekeepers (adjudicators) will pass. Offers such as referrals, medications or screening are depicted by the small balls that need to be accepted by the self and be compatible with the organizational framework represented by permeability and wider environment or local conditions. Concordance and recursivity are integral to the framework and are most often salient to the dimensions they touch in the diagram. The outcome is ideally access, but different resources may require an iterative process to obtain and for some, the obstacles represented by the accumulated dimensions may defeat access.
Limitations
The CIS is a very flexible approach to systematic synthesis, which can be both a strength and a weakness. This critical approach draws on the reviewer’s expertise in the field on the one hand and responds to the knowledge needs of the research team, on the other. In this sense, it is not entirely reproducible [35]. SK, the first author, was primarily responsible for data analysis for which task she drew on her considerable expertise in access to health care and theoretical approaches to illness experience. She consulted frequently with the remaining authors whose expertise in RA and primary care provision strengthened the validity of her interpretations. To remain accountable, the authors of a CIS must demonstrate both systematicity (soundness of execution) and transparency (explicitness of reporting), for which Depraetere and colleagues (25) have developed seven evaluative criteria that distinguish a CIS. Most important among them are (1) Data-extraction method for identifying themes/concepts, (2) Formulation of a synthesizing argument, (3) Inclusion of qualitative and quantitative research results, and (4) Flexible inclusion criteria. We believe that all criteria in this list have been met. While most sources were qualitative to address the deficit in comprehensive studies of RA access experience, eleven were mixed methods with a quantitative component, four were quantitative, and three were review articles.
Conclusions
Adoption of the CIS methodology using the lens of the Candidacy Framework to review literature focused on the experiences of people living with a chronic condition (specifically RA) has generated a rich analysis of the challenges and complexity of access to care for RA. Perhaps more importantly, this analysis has identified the key phenomenological dimension of embodied selfhood that is missing in the original formulation of Candidacy. The importance of this central concept is reinforced when considered in relation to other applications of Candidacy, particularly those concerned with access to care for chronic conditions. Modifications suggested by these studies underscore the importance of considering the intersectional and relational self as integral to an enhanced version of the framework.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Data availability
Data is provided within the manuscript or supplementary information files.
Notes
Advisory committee members continue to be involved with the overall programme of RA research but did not feel equipped to contribute to the CIS given their lack of familiarity with academic literature.
References
Barber CE, Lacaille D, Croxford R, Barnabe C, Marshall DA, Abrahamowicz M, et al. Investigating associations between access to rheumatology care, treatment, continuous care and healthcare utilization and costs among older individuals with RA. J Rheumatol. 2023;50(5):617–24.
Davtyan A, Lee JJY, Eder L, Hawker GA, Luo J, Barber CEH, et al. The effects of continuity of rheumatology care on emergency department utilization and hospitalizations for individuals with early rheumatoid arthritis: a population-based study. J Rheumatol. 2023;50(6):748–53. https://doi.org/10.3899/jrheum.220996.
Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7(1):73–82.
Dixon-Woods M, Cavers D, Agarwal MS, Annandale E, Arthur T, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35.
O’Brien P, Bunzli S, Ayton D, Dowsey MM, Gunn J, Manski-Nankervis JA. What are the patient factors that impact on decisions to progress to total knee replacement? A qualitative study involving patients with knee osteoarthritis. BMJ Open. 2019;9(9):e031310.
Chase LE, Cleveland J, Beatson J, Rousseau C. The gap between entitlement and access to healthcare: an analysis of candidacy in the help-seeking trajectories of asylum seekers in Montreal. Soc Sci Med. 2017;182:52–9.
Blane DN, Macdonald S, O’Donnell CA. What works and why in the identification and referral of adults with comorbid obesity in primary care: a realist review. Obes Rev. 2020;21(4):e12979.
Mackenzie M, Conway E, Hastings A, Munro M, O’Donnell C. Is ‘candidacy’ a useful concept for understanding journeys through public services? A critical interpretive literature synthesis. Soc Policy Admin. 2013;47(7):806–25.
Klassen AC, Smith KC, Shariff-Marco S, Juon HS. A healthy mistrust: how worldview relates to attitudes about breast cancer screening in a cross-sectional survey of low-income women. Int J Equity Health. 2008;7(1):5–24.
Koehn S. Negotiating candidacy: ethnic minority seniors’ access to care. Ageing Soc. 2009;29(4):585–608.
Koehn S, Badger M, McCleary L, Cohen C, Drummond N. Negotiating access to a diagnosis of dementia: implications for policies in health and social care. Dement - Lond. 2016;15(6):1436–56.
Wilson N, Beasley MJ, Pope C, Dulake D, Moir LJ, Hollick RJ, et al. UK healthcare services for people with fibromyalgia: results from two web-based national surveys (the PACFiND study). BMC Health Serv Res. 2022;22(1):989.
Garrett CR, Gask LL, Hays R, Cherrington A, Bundy C, Dickens C, et al. Accessing primary health care: a meta-ethnography of the experiences of British south Asian patients with diabetes, coronary heart disease or a mental health problem. Chronic Illn. 2012;8(2):135–55.
Hunter C, Chew-Graham C, Langer S, Stenhoff A, Drinkwater J, Guthrie E, et al. A qualitative study of patient choices in using emergency health care for long-term conditions: the importance of candidacy and recursivity. Patient Educ Couns. 2013;93(2):335–41.
Methley AM, Chew-Graham CA, Cheraghi-Sohi S, Campbell SM. A qualitative study of patient and professional perspectives of healthcare services for multiple sclerosis: implications for service development and policy. Health Soc Care Community. 2017;25(3):848–57.
Bristow K, Edwards S, Funnel E, Fisher L, Gask L, Dowrick C, et al. Help seeking and access to primary care for people from hard-to-reach groups with common mental health problems. Int J Fam Med. 2011;10:490634.
Kovandžić M, Chew-Graham C, Reeve J, Edwards S, Peters S, Edge D, et al. Access to primary mental health care for hard-to-reach groups: from ‘silent suffering’to ‘making it work’. Soc Sci Med. 2011;72(5):763–72.
Finckh A, Gilbert B, Hodkinson B, Bae SC, Thomas R, Deane KD, et al. Global epidemiology of rheumatoid arthritis. Nat Rev Rheumatol. 2022;18(10):591–602.
The Arthritis Society. Rheumatoid arthritis - symptoms, causes, diagnosis & treatments. 2017. https://arthritis.ca/about-arthritis/arthritis-types-(a-z)/types/rheumatoid-arthritis
Lacaille D, Anis AH, Guh DP, Esdaile JM. Gaps in care for rheumatoid arthritis: a population study. Arthritis Care Res. 2005;53(2):241–8.
Kelly A, Tymms K, Fallon K, Sumpton D, Tugwell P, Tunnicliffe D, et al. Qualitative research in rheumatology: an overview of methods and contributions to practice and policy. J Rheumatol. 2021;48(1):6–15.
Huberman M, Miles MB. The qualitative researcher’s companion. Sage. 2002;426.
Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess. 2011;15(43):1–164.
Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. Newbury Park, CA: Sage; 1988.
Depraetere J, Vandeviver C, Keygnaert I, Beken TV. The critical interpretive synthesis: an assessment of reporting practices. Int J Soc Res Methodol. 2020;0(0):1–21.
Veritas Health Innovation. Covidence systematic review software. Australia: Melbourne; 2021.
Hand CL, Wilkins S, Letts LJ, Law MC. Renegotiating environments to achieve participation: a metasynthesis of qualitative chronic disease research. Can J Occup Ther. 2013;80(4):251–62.
Poh LW, He HG, Lee CSC, Cheung PP, Chan WCS. An integrative review of experiences of patients with rheumatoid arthritis. Int Nurs Rev. 2015;62(2):231–47.
Stack RJ, Shaw K, Mallen C, Herron-Marx S, Horne R, Raza K. Delays in help seeking at the onset of the symptoms of rheumatoid arthritis: a systematic synthesis of qualitative literature. Ann Rheum Dis. 2012;71(4):493–7.
Bernatsky S, Feldman D, Shrier I, Toupin K, Haggerty J, Tousignant P, et al. Care pathways in early rheumatoid arthritis. Can Fam Physician. 2006;52(11):1444–5.
Dures E, Almeida C, Caesley J, Peterson A, Ambler N, Morris M, et al. Patient preferences for psychological support in inflammatory arthritis: a multicentre survey. Ann Rheum Dis. 2016;75(1):142–7.
Nair BV, Schuler R, Stewart S, Taylor-Gjevre RM. Self-reported barriers to healthcare access for rheumatoid arthritis patients in rural and Northern Saskatchewan: a mixed methods study. Musculoskelet Care. 2016;14(4):243–51.
Kvien TK, Balsa A, Betteridge N, Buch MH, Durez P, Favalli EG, et al. Considerations for improving quality of care of patients with rheumatoid arthritis and associated comorbidities. RMD Open. 2020;6(2):e001211.
Carboni C, Wehrens R, van der Veen R, de Bont A. Conceptualizing the digitalization of healthcare work: a metaphor-based critical interpretive synthesis. Soc Sci Med. 2022;292:114572.
Dixon-Woods M. Synthesising qualitative and quantitative evidence. Powerpoint slides presented at University of Leicester; 2012; http://www.evidencebasedpublichealth.de/download/Dixon-Woods%20Systematic%20reviews%20of%20qualitative%20and%20mixed%20studies.pdf
De Cock D, Van der Elst K, Stouten V, Peerboom D, Joly J, Westhovens R, et al. The perspective of patients with early rheumatoid arthritis on the journey from symptom onset until referral to a rheumatologist. Rheum Adv Prac. 2019;3(2):rkz035.
Flurey CA, Morris M, Richards P, Hughes R, Hewlett S. It’s like a juggling act: rheumatoid arthritis patient perspectives on daily life and flare while on current treatment regimes. Rheumatology (Oxford). 2014;53(4):696–703.
Kobue B, Moch S, Watermeyer J. It’s so hard taking pills when you don’t know what they’re for: a qualitative study of patients’ medicine taking behaviours and conceptualisation of medicines in the context of rheumatoid arthritis. BMC Health Serv Res. 2017;17(1):303.
Oliver S. Exploring the healthcare journey of patients with rheumatoid arthritis: a mapping project – implications for practice. Musculoskelet Care. 2008;6(4):247–66.
Sheppard J, Kumar K, Buckley CD, Shaw KL, Raza K. I just thought it was normal aches and pains: a qualitative study of decision-making processes in patients with early rheumatoid arthritis. Rheumatology (Oxford). 2008;47(10):1577–82.
Kumar K, Peters S, Barton A. Rheumatoid arthritis patient perceptions on the value of predictive testing for treatments: a qualitative study. BMC Musculoskelet Disord. 2016;17(1):1–6.
Chilton F, Bradley E, Mitchell T. Lost time. Patients with early inflammatory/rheumatoid arthritis and their experiences of delays in primary care. Musculoskelet Care. 2021;19(4):495–503.
Kumar K, Daley E, Khattak F, Buckley CD, Raza K. The influence of ethnicity on the extent of, and reasons underlying, delay in general practitioner consultation in patients with RA. Rheumatology (Oxford). 2010;49:1005–12.
Rao JK, Arick R, Mihaliak K, Weinberger M. Using focus groups to understand arthritis patients’ perceptions about unconventional therapy. Arthritis Care Res. 1998;11(4):253–60.
Bernatsky S, Feldman D, De Civita M, Haggerty J, Tousignant P, Legare J, et al. Optimal care for rheumatoid arthritis: a focus group study. Clin Rheumatol. 2010;29(6):645–57.
Laires PA, Mesquita R, Veloso L, Martins AP, Cernadas R, Fonseca JE. Patient’s access to healthcare and treatment in rheumatoid arthritis: the views of stakeholders in Portugal. BMC Musculoskelet Disord. 2013;14(100968565):279.
Mølbæk K, Hørslev-Petersen K, Primdahl J. Diagnostic delay in rheumatoid arthritis: a qualitative study of symptom interpretation before the first visit to the doctor. Musculoskelet Care. 2016;14(1):26–36.
Simons G, Belcher J, Morton C, Kumar K, Falahee M, Mallen CD, et al. Symptom recognition and perceived urgency of help-seeking for rheumatoid arthritis and other diseases in the general public: a mixed method approach. Arthritis Care Res. 2017;69(5):633–41.
Blake A, Mandy PJ, Stew G. Factors influencing the patient with rheumatoid arthritis in their decision to seek podiatry. Musculoskelet Care. 2013;11(4):218–28.
de Souza S, Williams R, Lempp H. Patient and clinician views on the quality of foot health care for rheumatoid arthritis outpatients: a mixed methods service evaluation. J Foot Ankle Res. 2016;9(101471610):1.
Firth J, Nelson A, Briggs M, Gorecki C. Experiences of healthcare provision for foot ulceration occurring in people with rheumatoid arthritis. Musculoskelet Care. 2013;11(3):159–67.
Townsend A, Adam P, Cox SM, Li LC. Everyday ethics and help-seeking in early rheumatoid arthritis. Chronic Illn. 2010;6(3):171–82.
Stack RJ, van Tuyl LHD, Sloots M, van de Stadt LA, Hoogland W, Maat B, et al. Symptom complexes in patients with seropositive arthralgia and in patients newly diagnosed with rheumatoid arthritis: a qualitative exploration of symptom development. Rheumatology (Oxford). 2014;53(9):1646–53.
Nyman CS, Lutzen K. Caring needs of patients with rheumatoid arthritis. Nurs Sci Q. 1999;12(2):164–9.
Townsend A, Backman CL, Adam P, Li LC. Women’s accounts of help-seeking in early rheumatoid arthritis from symptom onset to diagnosis. Chronic Illn. 2014;10(4):259–72.
Brand C, Claydon-Platt K, McColl G, Bucknall T. Meeting the needs of people diagnosed with rheumatoid arthritis: an analysis of patient-reported experience. J Nurs Healthc Chronic Illn. 2010;2(1):75–83.
Graham AS, Williams AE. Foot Health Education for People with rheumatoid arthritis: … a game of Chance… - a Survey of patients’ experiences. Musculoskelet Care. 2016;14(1):37–46.
Siisiainen M. Two concepts of social capital: Bourdieu vs. Putnam. Int J Contemp Sociol. 2003;40(2):183–204.
Poh LW, He HG, Chan WCS, Lee CSC, Lahiri M, Mak A, et al. Experiences of patients with rheumatoid arthritis: a qualitative study. Clin Nurs Res. 2017;26(3):373–93.
Park JYE, Howren AM, Davidson E, De Vera MA. Insights on mental health when living with rheumatoid arthritis: a descriptive qualitative study of threads on the Reddit website. BMC Rheumatol. 2020;4(1):62.
Barber CEH, Lacaille D, Hall M, Bohm V, Li LC, Barnabe C, et al. Priorities for high-quality care in rheumatoid arthritis: results of patient, health professional, and policy maker perspectives. J Rheumatol. 2021;48(4):486–94.
Ahlmen M, Nordenskiold U, Archenholtz B, Thyberg I, Ronnqvist R, Linden L, et al. Rheumatology outcomes: the patient’s perspective. A multicentre focus group interview study of Swedish rheumatoid arthritis patients. Rheumatology (Oxford). 2005;44(1):105–10.
Flurey CA, Hewlett S, Rodham K, White A, Noddings R, Kirwan JR. You obviously just have to put on a brave face: a qualitative study of the experiences and coping styles of men with rheumatoid arthritis. Arthritis Care Res. 2017;69(3):330–7.
Lempp H, Scott DL, Kingsley GH. Patients’ views on the quality of health care for rheumatoid arthritis. Rheumatol. 2006;45(12):1522–8.
Clarke LH, Bennett E. You learn to live with all the things that are wrong with you’: gender and the experience of multiple chronic conditions in later life. Ageing Soc. 2013;33(2):342–60.
Galdas P, Cheater F, Marshall P. What is the role of masculinity in white and south Asian men’s decisions to seek medical help for cardiac chest pain? J Health Serv Res Policy. 2007;12(4):223–9.
Thurston WE, Coupal S, Jones CA, Crowshoe LF, Marshall DA, Homik J, et al. Discordant indigenous and provider frames explain challenges in improving access to arthritis care: a qualitative study using constructivist grounded theory. Int J Equity Health. 2014;13(1):46.
Hendry GJ, Gibson KA, Pile K, Taylor L, Du Toit V, Burns J, et al. They just scraped off the calluses: a mixed methods exploration of foot care access and provision for people with rheumatoid arthritis in south-western Sydney, Australia. J Foot Ankle Res. 2013;6(1):34.
Loyola-Sanchez A, Pelaez-Ballestas I, Crowshoe L, Lacaille D, Henderson R, Rame A, et al. There are still a lot of things that I need: a qualitative study exploring opportunities to improve the health services of First Nations people with arthritis seen at an on-reserve outreach rheumatology clinic. BMC Health Serv Res. 2020;20(1):1076.
Dando C, Bacon D, Borthwick A, Bowen C. Stakeholder views of podiatry services in the UK for people living with arthritis: a qualitative study. J Foot Ankle Res. 2020;13(1):58.
Pollard LC, Graves H, Scott DL, Kingsley GH, Lempp H. Perceived barriers to integrated care in rheumatoid arthritis: views of recipients and providers of care in an inner-city setting. BMC Musculoskelet Disord. 2011;12(100968565):19.
Pianarosa E, Hazlewood GS, Thomas M, Hsiao R, Barnabe C. Supporting equity in Rheumatoid Arthritis outcomes in Canada: Population-specific factors in patient-centered care. J Rheumatol. 2021;48(12):1793–802.
Baymler Lundberg AS, Esbensen BA, Jensen MB, Hauge EM, de Thurah A. Facilitators and barriers in diagnosing rheumatoid arthritis as described by general practitioners: a Danish study based on focus group interviews. Scand J Prim Health Care. 2021;39(2):222–9.
Graham AS, Hammond A, Williams AE. Foot health education for people with rheumatoid arthritis: the practitioner’s perspective. J Foot Ankle Res. 2012;5(1):2.
Hartford W, Backman CL, Li LC, McQuitty S, McKinnon A, Kherani R, et al. Networks of care: a social network perspective of distributed multidisciplinary care for people with inflammatory arthritis. ACR Open Rheumatol. 2022;4(1):40–56.
Hewlett S, Sanderson T, May J, Alten R, Bingham CO 3rd, Cross M, et al. I’m hurting, I want to kill myself: rheumatoid arthritis flare is more than a high joint count–an international patient perspective on flare where medical help is sought. Rheumatology (Oxford). 2012;51(1):69–76.
Pollard TM, Carlin LE, Bhopal R, Unwin N, White M, Fischbacher C. Social networks and coronary heart disease risk factors in South asians and europeans in the UK. Ethn Health. 2003;8(3):263–75.
Lopatina E, Miller JL, Teare SR, Marlett NJ, Patel J, Barber CEH, et al. The voice of patients in system redesign: a case study of redesigning a centralized system for intake of referrals from primary care to rheumatologists for patients with suspected rheumatoid arthritis. Health Expect. 2019;22(3):348–63.
Abdelhamid AS, Mooney J, Walker AA, Barton G, MacGregor AJ, Scott DGI, et al. An evaluation of rheumatology practitioner outreach clinics: a qualitative study. BMC Health Serv Res. 2012;12(101088677):119.
Landgren E, Bremander A, Lindqvist E, Nylander M, Larsson I. Patients’ perceptions of person-centered care in early rheumatoid arthritis: a qualitative study. ACR Open Rheumatol. 2021;3(11):788–95.
Machin A, Hider S, Dale N, Chew-Graham C. Improving recognition of anxiety and depression in rheumatoid arthritis: a qualitative study in a community clinic. Br J Gen Pract. 2017;67(661):e531–7.
Cefai E, Balzan D, Mercieca C, Borg A. Patients’ perspective of a dedicated biologic clinic for inflammatory arthritis. J Health Care Qual Assur. 2019;32(5):879–86.
Dubouloz CJ, Vallerand J, Laporte D, Ashe B, Hall M. Occupational performance modification and personal change among clients receiving rehabilitation services for rheumatoid arthritis. Aust Occup th J. 2008;55(1):30–8.
Linden C, Bjorklund A. Living with rheumatoid arthritis and experiencing everyday life with TNF-alpha blockers. Scand J OccupTher. 2010;17(4):326–34.
Ottenvall Hammar I, Hakansson C. The importance for daily occupations of perceiving good health: perceptions among women with rheumatic diseases. Scand J Occup Ther. 2013;20(2):82–92.
Sanders L, Donovan-Hall M, Borthwick A, Bowen CJ. Experiences of mobility for people living with rheumatoid arthritis who are receiving biologic drug therapy: implications for podiatry services. J Foot Ankle Res. 2017;10(101471610):14.
Bergstrom M, Ahlstrand I, Thyberg I, Falkmer T, Borsbo B, Bjork M. Like the worst toothache you’ve had - how people with rheumatoid arthritis describe and manage pain. Scand J Occup Ther. 2017;24(6):468–76.
Chan SJ, Stamp LK, Liebergreen N, Ndukwe H, Marra C, Treharne GJ. Tapering biologic therapy for rheumatoid arthritis: a qualitative study of patient perspectives. Patient. 2020;13(2):225–34.
Hazlewood GS, Loyola-Sanchez A, Bykerk V, Hull PM, Marshall D, Pham T et al. Patient and rheumatologist perspectives on tapering DMARDs in rheumatoid arthritis: a qualitative study. Rheumatology (Oxford). 2021;(100883501, ddb).
Hewlett S, Haig-Ferguson A, Rose-Parfitt E, Halls S, Freke S, Creamer P. Dose reduction of biologic therapy in inflammatory arthritis: a qualitative study of patients’ perceptions and needs. Musculoskelet Care. 2019;17(1):63–71.
Fair BS. Contrasts in patients’ and providers’ explanations of rheumatoid arthritis. J Nurs Scholarsh. 2003;35(4):339–44.
Brandstetter S, Hertig S, Loss J, Ehrenstein B, Apfelbacher C. The lesser of two evils… views of persons with rheumatoid arthritis on medication adherence: a qualitative study. Psychol Health. 2016;31(6):675–92.
Loyola-Sanchez A, Hazlewood G, Crowshoe L, Linkert T, Hull PM, Marshall D, et al. Qualitative study of treatment preferences for rheumatoid arthritis and pharmacotherapy acceptance: indigenous patient perspectives. Arthritis Care Res. 2020;72(4):544–52.
McArthur MA, Birt L, Goodacre L. Better but not best: a qualitative exploration of the experiences of occupational gain for people with inflammatory arthritis receiving anti-TNFalpha treatment. Disabil Rehabil. 2015;37(10):854–63.
McBain H, Newman S, Shipley M, Olaleye A, Moore S. Experiences of a patient-initiated self‐monitoring service in inflammatory arthritis: a qualitative exploration. Musculoskelet Care. 2018;16(2):278–86.
Prothero L, Georgopoulou S, Galloway J, Williams R, Bosworth A, Lempp H. Patients’ and carers’ views and expectations about intensive management for moderate rheumatoid arthritis: a qualitative study. Psychol Health Med. 2016;21(8):918–25.
Rose G. Why do patients with rheumatoid arthritis use complementary therapies? Musculoskelet Care. 2006;4(2):101–15.
Lacaille D, Avina-Zubieta JA, Sayre EC, Abrahamowicz M. Improvement in 5-year mortality in incident rheumatoid arthritis compared with the general population—closing the mortality gap. Ann Rheum Dis. 2017;76(6):1057–63.
Nguyen H, Ahmed K, Luo W, Flint J, Giles I. A systematic review of the safety of non-TNF inhibitor biologic and targeted synthetic drugs in rheumatic disease in pregnancy. Semin Arthritis Rheum. 2021;51(6):1205–17.
Zhou VY, Lacaille D, Lu N, Kopec JA, Garbuz DS, Qian Y, et al. Has the incidence of total joint arthroplasty in rheumatoid arthritis decreased in the era of biologics use? A population-based cohort study. Rheumatology (Oxford). 2022;61(5):1819–30.
Brien SB, Leydon GM, Lewith G. Homeopathy enables rheumatoid arthritis patients to cope with their chronic ill health: a qualitative study of patient’s perceptions of the homeopathic consultation. Patient Educ Couns. 2012;89(3):507–16.
Pati S, Sahoo KC, Samal M, Jena S, Mahapatra P, Sutar D, et al. Care-seeking pathways, care challenges, and coping experiences of rural women living with rheumatoid arthritis in Odisha, India. Prim Health Care Res Dev. 2019;20(100897390):e83.
Squire R. Living well with rheumatoid arthritis. Musculoskelet Care. 2012;10(3):127–34.
Bearne LM, Manning VL, Choy E, Scott DL, Hurley MV. Participants’ experiences of an education, self-management and upper extremity eXercise training for people with rheumatoid arthritis programme (EXTRA). Physiotherapy. 2017;103(4):430–8.
Nichols VP, Williamson E, Toye F, Lamb SE. A longitudinal, qualitative study exploring sustained adherence to a hand exercise programme for rheumatoid arthritis evaluated in the SARAH trial. Disabil Rehabil. 2017;39(18):1856–63.
Swardh E, Biguet G, Opava CH. Views on exercise maintenance: variations among patients with rheumatoid arthritis. Phys Ther. 2008;88(9):1049–60.
Larkin L, Gallagher S, Fraser A, Kennedy N. If a joint is hot it’s not the time: health professionals’ views on developing an intervention to promote physical activity in rheumatoid arthritis. Disabil Rehabil. 2017;39(11):1106–13.
Feldthusen C, Mannerkorpi K. Factors of importance for reducing fatigue in persons with rheumatoid arthritis: a qualitative interview study. BMJ Open. 2019;9(5):e028719.
Josefsson KA, Gard G. Women’s experiences of sexual health when living with rheumatoid arthritis–an explorative qualitative study. BMC Musculoskelet Disord. 2010;11(100968565):240.
Lange E, Palstam A, Gjertsson I, Mannerkorpi K. Aspects of exercise with person-centred guidance influencing the transition to independent exercise: a qualitative interview study among older adults with rheumatoid arthritis. Eur Rev Aging Phys Act. 2019;16:4.
Ward L, Treharne GJ, Stebbings S. The suitability of yoga as a potential therapeutic intervention for rheumatoid arthritis: a focus group approach. Musculoskelet Care. 2011;9(4):211–21.
Feddersen H, Kristiansen TM, Andersen PT, Hørslev-Petersen K, Primdahl J. Interactions between women with rheumatoid arthritis and nurses during outpatient consultations: a qualitative study. Musculoskelet Care. 2019;17(4):363–71.
McCulloch L, Borthwick A, Redmond A, Edwards K, Pinedo-Villanueva R, Prieto-Alhambra D, et al. UK podiatrists’ experiences of podiatry services for people living with arthritis: a qualitative investigation. J Foot Ankle Res. 2018;11(101471610):27.
Moerbeke A, Magdelijns F, Cleutjens F, Boonen A, Onna M. Development and evaluation of a clinic for Elderly patients with rheumatoid arthritis and multimorbidity: a pilot study. ACR Open Rheumatol. 2021;3(1):34–40.
Carr ECJ, Ortiz MM, Patel JN, Barber CEH, Katz S, Robert J, et al. Models of Arthritis Care: A systems-level evaluation of acceptability as a dimension of Quality of Care. J Rheumatol. 2020;47(9):1431–9.
MacKay C, Veinot P, Badley EM. Characteristics of evolving models of care for arthritis: a key informant study. BMC Health Serv Res. 2008;8(101088677):147.
Kleinman A. The illness narratives: suffering, healing, and the human condition. Cambridge: Basic Book; 1988.
Bury M. Chronic illness as biographical disruption. Sociol Health Illn. 1982;4(2):167–82.
Goodacre L. Women’s perceptions on managing chronic arthritis. Br J OccupTher. 2006;69(1):7–14.
Charmaz K. Stories and silences: disclosures and self in chronic illness. Qual Inq. 2002;8(3):302–28.
Ratcliffe M. Towards a phenomenology of grief: insights from Merleau-Ponty. Eur J Philos. 2020;28(3):657–69.
Niedermann K, Hammond A, Forster A, de Bie R. Perceived benefits and barriers to joint protection among people with rheumatoid arthritis and occupational therapists. A mixed methods study. Musculoskelet Care. 2010;8(3):143–56.
Martin E. The woman in the body: a Cultural Analysis of Reproduction. Beacon Press; 2001. p. 316.
Chrisler JC, Rossini M, Newton JR. Older Women, Power, and the body. In: Muhlbauer V, Chrisler JC, Denmark FL, editors. Women and aging: an International, Intersectional Power Perspective. Cham: Springer International Publishing; 2015. pp. 9–30.
Tehan PE, Morpeth T, Williams AE, Dalbeth N, Rome K. Come and live with my feet and you’ll understand - a qualitative study exploring the experiences of retail footwear in women with rheumatoid arthritis. J Foot Ankle Res. 2019;12(101471610):15.
Grant M. Mothers with arthritis, Child Care and Occupational Therapy: insight through Case studies. Br J OccupTher. 2001;64(7):322–9.
Gustafsson K, Andersson I, Andersson J, Fjellstrom C, Sidenvall B. Older women’s perceptions of independence versus dependence in food-related work. Public Health Nurs. 2003;20(3):237–47.
Kostova Z, Caiata-Zufferey M, Schulz PJ. The impact of social support on the acceptance process among RA patients: a qualitative study. Psychol Health. 2014;29(11):1283–302.
Lütze U, Archenholtz B. The impact of arthritis on daily life with the patient perspective in focus. Scand J Caring Sci. 2007;21(1):64–70.
Crenshaw K. A primer on Intersectionality. Volume 11. New York: African American Policy Forum; 2009.
Winker G, Degele N. Intersectionality as multi-level analysis: dealing with social inequality. Eur J Women’s Stud. 2011;18(1):51–66.
Ward V, Hill J, Hale C, Bird H, Quinn H, Thorpe R. Patient priorities of care in rheumatology outpatient clinics: a qualitative study. Musculoskelet Care. 2007;5(4):216–28.
Radford S, Carr M, Hehir M, Davis B, Robertson L, Cockshott Z, et al. It’s quite hard to grasp the enormity of it: perceived needs of people upon diagnosis of rheumatoid arthritis. Musculoskelet Care. 2008;6(3):155–67.
Firth J, Nelson EA, Briggs M, Gorecki C. A qualitative study to explore the impact of foot ulceration on health-related quality of life in patients with rheumatoid arthritis. Int J Nurs Stud. 2011;48(11):1401–8.
Kristiansen TM, Antoft R. Patient education as a status passage in life - an ethnographic study exploring participation in a Danish group based patient education programme. Soc Sci Med. 2016;158(ut9):34–42.
Frank AW. The wounded storyteller: body, illness & ethics. University of Chicago Press; 2013. p. 280.
Rogers AE, Hassell K, Nicolaas G. Demanding patients: analysing the use of primary care. Open University; 1999. (The State of Health series).
Stevenson F, Scambler G. The relationship between medicine and the public: the challenge of concordance. Health. 2005;9(1):5–21.
MacKenzie M, Conway E, Hastings A, Munro M, O’Donnell C. Intersections and multiple candidacies: exploring connections between two theoretical perspectives on domestic abuse and their implications for practicing policy. Soc Policy Soc. 2015;14(1):43–62.
Saari C. Identity complexity as an indicator of health. Clin Soc Work J. 1993;21(1):11–24.
Erving CL, Frazier C. The association between multiple chronic conditions and depressive symptoms: intersectional distinctions by race, nativity, and gender. J Health Soc Behav. 2021;62(4):599–617.
Hwang J, Wang L, Siever J, Medico TD, Jones CA. Loneliness and social isolation among older adults in a community exercise program: a qualitative study. Aging Ment Health. 2019;23(6):736–42.
Hankivsky O. Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med. 2012;74(11):1712–20.
Clarke LH, Griffin M. Failing bodies: body image and multiple chronic conditions in later life. Qual Health Res. 2008;18(8):1084–95.
Porter T, Ong BN, Sanders T. Living with multimorbidity? The lived experience of multiple chronic conditions in later life. Health. 2020;24(6):701–18.
Depares J, Culley L. Healthcare encounters between asylum seekers and health professionals in Maltese primary care. J Res Nurs. 2022;27(3):275–87.
Khoshkar L. Toward an interdependent conception of the self: implications for Canadian policy reform. The Canadian Society for Study of Practical Ethics / Société Canadienne Pour L’étude De L’éthique Appliquée. — SCEEA. 2019;15–40.
Acknowledgements
The authors would like to express a sincere thank you to Nikoletta Wood for the creation of the graphics for the Candidacy 2.0 framework model, and to all of the members of the advisory committee, composed of people living with RA, who provided support and insight in the development of the research questions.
Funding
The authors would also like to convey their gratitude to The Arthritis Society Canada for the support through the Strategic Operating Grant 20 − 0000000018 SOG, and to Mitacs for the.
support through an Accelerate Postdoctoral Fellowship.
Author information
Authors and Affiliations
Contributions
SK and AP reviewed articles for inclusion. SK analyzed the included articles. All authors (SK, CAJ, CB, LJ, AP, CL, ND) were involved in writing, reviewing, and approving the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Koehn, S., Jones, C.A., Barber, C. et al. Candidacy 2.0 (CC) – an enhanced theory of access to healthcare for chronic conditions: lessons from a critical interpretive synthesis on access to rheumatoid arthritis care. BMC Health Serv Res 24, 986 (2024). https://doi.org/10.1186/s12913-024-11438-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11438-6