Abstract
Background
Given the increasing prevalence of the physician burnout, this study provides new insights into the antecedents driving burnout and turnover intent. By introducing the concept of physician fortitude, we develop a valid and statistically-reliable measure that increases our understanding of these issues.
Methods
A two-sample design was employed. Using a sample of 909 physicians, Advanced Practice Providers (APPs) and healthcare leaders, exploratory factor analysis was employed to create a 12-item fortitude scale. In the second study, using a sample of 212 of practicing physicians, APPs and healthcare leaders, bivariate and tetrachoric correlations, and ordinary least square regression modeling were able to establish reliability and validity.
Results
The fortitude scale shows sufficient reliability. Moreover, we found significant support for convergent and criterion-related validity. Fortitude was significantly related to all three subdimensions of burnout, including emotional exhaustion (r = -.62, p < .01), depersonalization (r = -.70, p < .01) and personal accomplishment (r = .65, p < .01), and turnover intent (r = -.55, p < .01). Moreover, the fortitude measure explained more variance in all three subdimensions of burnout and turnover intent compared to common measures, including grit, hardiness, mental toughness and resilience (p < .01).
Conclusions
Results from this study empirically demonstrate that fortitude is significantly related to burnout, and turnover intent. This new fortitude measure adds a new perspective to assist in the development of more effective interventions. Opportunities for future research are discussed.
Similar content being viewed by others
Background
For nearly thirty years, researchers have sought to understand the antecedents and consequences of physician burnout, yet the problem continues. Notably, Shanafelt et al., found that 62.8% of physicians had at least one manifestation of burnout in 2021, compared with 45.5% in 2011 [1]. Consequently, patients have a higher likelihood of being treated by a burned-out physician today than one who is not [1, 2]. This is associated with decreased quality of care, medical errors, poor patient satisfaction, and limited patient access [3, 4]. Moreover, beyond the human cost of burnout on individuals, the financial cost of burnout related turnover on the healthcare system is estimated to be $2.6 to $6.3 billion (USD) a year, or $7,600 (USD) per employed physician [5]. Clearly more research needs to be conducted to understand the antecedents of physician burnout and turnover so that more effective strategies can be developed to address this growing problem.
Overview of physician burnout
Existing research on physician burnout has primarily examined two sets of drivers, intrinsic personality traits and extrinsic work environments. Intrinsic personality traits such as high neuroticism, low agreeableness and low conscientiousness as measured by the Big 5 Inventory have been associated with an increased risk of burnout [6]. Likewise, extrinsic work environmental factors such as excessive workload, poor work-life balance, low autonomy and systemic barriers all contribute to burnout and intent to leave. [7, 8].
Much recent research focused on the importance of the work environment has led to interventions to improve physician wellbeing [9,10,11,12]. However, in a recent meta-analysis of 38 randomized trials using different interventions focused on improving physician burnout, results suggested these efforts did not result in meaningful impacts on clinical burnout [13]. Furthermore, the authors suggest that a more nuanced understanding of the causes of burnout is needed to develop more effective interventions. Similarly, Cataputo et al., looked at interventions focused on mitigating work-related stress in healthcare using cognitive behavioral therapy, relaxation therapy; and interventions focused on the organization. They concluded that individual-level interventions were beneficial over the short term, but organizational-level intervention failed to show any benefit in reducing burnout [14]. Although these studies have provided important insights into physician burnout, there are still significant opportunities to extend these findings.
Consequently, a critical question to consider is while it is estimated that up to 50% of physicians are suffering from burnout at any one time, why do 50% of physicians in presumably similar circumstances not burnout? One possible explanation may be that individuals can perceive their work environment very differently. In a study of UK house officers, differences in self-reported trainee stress levels were shown to be related to individual differences within the doctors themselves and not organizational factors present or the administrative structure of hospitals [15]. Furthermore, in a separate study, researchers determined how doctors perceived their workplace climate and workload can be partially predicted by trait measures of personality taken five years earlier [16]. That is not to say that factors such as work environment and systemic factors are unimportant but suggests that there is a need to build upon this past empirical research to increase our collective understanding of how an individual’s perspective and attitude may contribute to their unique responses to environmental stressors in healthcare.
Extant literature has yielded a significant amount of research assessing the relationship between intra-personal attributes with burnout and/or turnover across multiple professions. Specifically, there is a growing body of research that has demonstrated how grit [17,18,19], self-efficacy [20], hardiness [21,22,23], resilience [24, 25], mental toughness [26, 27] and hope [28, 29] individually mitigate the relationship between environmental stressors and burnout-related phenomena in healthcare and many other professions. While these unique individual attributes have proven to be beneficial, we believe there is a significant opportunity to integrate these constructs to develop a more holistic understanding of how individuals use all of these attributes to respond to their unique work-related stressors.
Integration of concepts
There have been previous attempts to integrate the abovementioned attributes. The limited literature on fortitude shows promise as a unifying construct [30,31,32]. However, this body of research has been studied using different definitions, antecedents and outcome measures. For example, Pretorius et al. defined fortitude as an attitude to manage stress and stay well. He postulated that this strength derives from an appraisal of the self, the family and support from others. Their 20 item Fortitude Questionnaire (FORQ) was tested and validated in undergraduate psychology students [31]. Henttonen et al. attempted to measure fortitude by developing a scale based on the Finnish cultural attribute of sisu, defined as determination and resoluteness in the face of adversity. They combined multiple intrapersonal attributes with personality traits to develop a 18-item scale in a general working population [30]. Similarly, VanTongeren et al. developed a validated measure for spiritual fortitude. Their measure includes items for spiritual enterprise, spiritual endurance and redemptive purpose and was validated in a volunteer population [32].
While there has been significant value from the fortitude research, its applicability and generalizability to physician burnout and turnover is limited. To advance the literature and extend our understanding of physician burnout, there is a need to arrive at a more precise definition relevant to healthcare. Subsequently, we suggest fortitude to be an interpersonal attitudinal attribute that enables one to succeed under repeated pressure and stress. Therefore, the purpose of this study is to gain new insights into burnout and turnover by investigating fortitude in healthcare and developing a statistically valid and reliable scale.
Methods
To assess the potential impact of physician fortitude on burnout and turnover intent, we drew on previous research that has focused on explaining how individuals overcome adversity. We employed a two-sample design to establish content validity, internal consistency, empirical reliability, unidimensionality, convergent validity and ultimately criterion-related validity. Surveys were approved by the University of Illinois College of Medicine Institutional Review Board. Informed consent was attained by all survey participants prior to completion of the survey.
Item generation
To ensure we met the psychometric assumptions proposed by our latent construct we define as fortitude, we used a deductive approach [33]. Grounded in extant literatures that have shown empirical promise regarding how individuals experience and ultimately overcome adversity, seven specific areas of research were identified. Specifically, we drew on grit, hardiness, mental toughness, resilience, hope, optimism and self-efficacy to generate a potential list of items for our integrative fortitude construct. Based on commonalities across these dimensions, 64 potential items were identified. We then engaged 73 physicians and non-physician healthcare leaders in 13 focus groups to provide feedback on the suitability of the potential items in a healthcare context. Based on relevancy, these focus groups reduced the potential list of survey items to 45.
Next, we ensured sufficient interrater reliability to evaluate internal consistency of potential items for the fortitude scale [34]. A panel of five academic researchers actively engaged in burnout and turnover research were queried and asked to match potential survey items with the fortitude construct. Crocker and Algina define a minimum value greater than 0.70 to be acceptable for consistency estimates of interrater reliability [35]. Consequently, if an item had an interrater reliability value that did not meet the 0.70 threshold, it was deleted as a possible item for the fortitude scale. This resulted in an interrater reliability 0.88. Results from the interrater reliability assessment yielded 34 potential items.
Data reduction, reliability and unidimensionality
To further reduce potential items, in our first study (study 1) we collected data from a sample of 909 practicing physicians, APPs and healthcare leaders from a large U.S. healthcare system. Respondents were asked to rate the degree to which each statement accurately described their own individual attributes on the 34 items using a seven-point Likert Scale, where 1 = strongly disagree and 7 = strongly agree. A seven-point Likert Scale was used, as this is most consistent with the literatures we used to develop our potential list of items.
Results from study 1 provided initial evidence of reliability, construct validity and unidimensionality. Exploratory factor analysis (EFA) was used to assess potential items. Given the data were normally distributed, a maximum likelihood extraction method and Varimax rotation were used [36]. We were able to identify potential items that had individual factor loadings greater than 0.70. This yielded a 12-item scale measuring fortitude in healthcare (HCF-12). Example items include “I am excited about working on achieving my goals,” “I am determined to succeed in achieving my goals,” “I am passionate about the work I do.”
The EFA provided initial support for the unidimensionality of a single factor for the HCF-12 scale, as well as initial construct validity. Specifically, scree plots indicated unidimensionality for our HCF-12 measure. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was 0.88, well above the suggested threshold of 0.5 [37], and Bartlett’s test of sphericity was significant (p < 0.05). Initial reliability was encouraging, yielding a Cronbach alpha of 0.89.
Convergent and criterion-related validity
After finding encouraging evidence of reliability and unidimensionality, we collected data from a second sample (study 2) to measure convergent validity and criterion-related validity. The survey in study 2 was sent to practicing physicians and healthcare leaders (n = 212). Similar to Study 1, we found encouraging reliability with a Cronbach’s alpha = 0.93. Measures for internal consistency and factor loadings of the 12 items in the HCF-12 for Study 2 can be seen in Table 1.
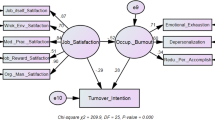
To test for convergent validity, Study 2 included the HCF-12 scale and scales grit [17], hardiness [21], resilience [24], mental toughness [27]. To establish criterion-related validity, the survey also included scales for all three subdimensions of burnout (emotional exhaustion, depersonalization, and personal achievement [38], and turnover intent [39], as previous literature has shown that chronic burnout leads to turnover [40,41,42]. Additionally, based on focus-group insights, control variables were added including age, gender, race, hours worked and call burden. Note that reliabilities for all scales used in Study 2 are included in Table 2.
Given the HCF-12 draws on attitudinal measures specifically related to stressors, including grit, hardiness, resilience and mental toughness, we would expect strong relationships among these variables. To assess convergent validity, we used correlational analyses. We found significant correlations between fortitude and hardiness (r = 0.28, p < 0.01) and resilience (r = 0.71, p < 0.01). However, there were not significant relationships between our fortitude measure with grit or mental toughness. To assess criterion-related validity, we would expect that the HCF-12 measure to be negatively related to burnout and turnover intent. Fortitude was significantly related all three subdimensions of burnout, specifically emotional exhaustion (r = -0.62, p < 0.01), depersonalization (r = -0.70, p < 0.01) and personal accomplishment (r = 0.65, p < 0.01), and turnover intent (r = -0.55, p < 0.01). Given that fortitude was significantly related to all of these constructs in the predicted directions, this provides strong initial evidence for criterion-related validity.
Findings and results
Based on encouraging results regarding reliability and validities of the HCF-12, this creates a platform that allows us to compare fortitude with the scales currently recognized as antecedents in the extant burnout and turnover-intent literatures. Subsequently, we used ordinary least-squared (OLS) regression modeling to test significance levels and explained variance to compared the HCF-12 to grit, hardiness, mental toughness and resilience based on data from the 212 respondents in study 2,
Sample characteristics
Of the 212 respondents who completed the survey, 76% were female, 21% were male and 3% preferred not to answer. For race, 91% of respondents were White, 5% were Asian, 2% were Hispanic and 2% were Black. The average age of respondents was 47.4 years old; they worked an average of 51.3 h per week and worked for an average of 8.8 years in the current hospital system. Finally, in terms of their role, respondents were asked if they were a physician leader (26%), a non-physician leader (49%) or a practicing clinician (29%).
Descriptive statistics
Means, standard deviations, reliability scores, and bivariate correlations can be seen in Table 2. Note that reliabilities for all scales met the minimum threshold of 0.70 (with the exceptions of hardiness) and the HCF-12 had the highest reliability score of 0.93. Also note that the fortitude measure was significantly related to all three subdimensions of burnout and turnover intent, providing encouraging support for the consideration of the new scale.
Ordinary least squares regression results
In order to compare the HCF-12 with existing measures, regression analyses were performed. Specifically, in Tables 3–6, fortitude, grit, hardiness, mental toughness and resilience were all regressed on turnover intent and the three subdimensions of burnout, namely emotional exhaustion, depersonalization and personal accomplishment.
In Table 3, all five scales were negatively related with turnover intent. Specifically, fortitude (β = -0.55), grit (β = -0.23) hardiness (β = -0.31), mental toughness (β = -0.27) and resilience (β = -0.28) were all statistically significant (p < 0.01). Note that there was a statistically significant difference in explained variance between fortitude and all of the other measures (p < 0.01). The adjusted R2 for fortitude was 0.30 compared to grit (0.04), hardiness (0.09), mental toughness (0.06) and resilience (0.07).
In Table 4, all five scales were negatively related with the burnout subdimension of emotional exhaustion. Specifically, fortitude (β = -0.62), grit (β = -0.35) hardiness (β = -0.56), mental toughness (β = -0.45) and resilience (β = -0.38) were all statistically significant (p < 0.01). Note that there was a statistically significant difference in explained variance between fortitude and all of the other measures (p < 0.01). The adjusted R2 for fortitude was 0.39 compared to grit (0.12), hardiness (0.32), mental toughness (0.29) and resilience (0.15).
In Table 5, all five scales were negatively related with the burnout subdimension of depersonalization. Specifically, fortitude (β = -0.69), grit (β = -0.36) hardiness (β = -0.50), mental toughness (β = -0.47) and resilience (β = -0.40) were all statistically significant (p < 0.01). Note that there was a statistically significant difference in explained variance between fortitude and all of the other measures (p < 0.01). The adjusted R2 for fortitude was 0.48 compared to grit (0.13), hardiness (0.25), mental toughness (0.22) and resilience (0.16).
In Table 6, all five scales were positively related with the burnout subdimension of personal accomplishment. Specifically, fortitude (β = 0.65), grit (β = 0.41) hardiness (β = 0.49), mental toughness (β = 0.49) and resilience (β = 0.59) were all statistically significant (p < 0.01). Note that there was a statistically significant difference in explained variance between fortitude and all of the other measures (p < 0.01). The adjusted R2 for fortitude was 0.42 compared to grit (0.16), hardiness (0.23), mental toughness (0.23) and resilience (0.34).
In summary, fortitude explained significantly more variance in turnover intent, emotional exhaustion, depersonalization and personal accomplishment than any of the existing measures.
Discussion
The primary focus of this research was to investigate the potential use of a new fortitude scale to increase our understanding of antecedents to physician burnout and turnover intent. Results from this study provide encouraging evidence that the integration of grit, hardiness, mental toughness and resilience, in a latent the construct defined as fortitude, provides new insights into understanding how the combination of these intrapersonal attributes contribute to physician burnout and turnover intent. Our proposed HCF-12 scale exhibited encouraging findings to support the psychometric properties of a physician fortitude scale. Specifically, based on a two-study design, we were able to establish content validity, unidimensionality, empirical reliability, convergent validity and criterion-related validity. Moreover, we were able to show that the HCF-12 resulted in significantly higher levels of explained variances for all three subdimensions of burnout and turnover intent when compared to all existing scales found in the extant literature. Consequently, findings from our study provide additional insights into understanding physician burnout and turnover intent. Specifically, our findings make several contributions.
First, our findings extend previous fortitude research that showed the combination of different psychological antecedents of well-being provide additional insights beyond single constructs alone. Specifically, Pretorius et al. derived their measure from the constructs of hardiness, sense of cohesion and potency and found that fortitude, defined as the strength to manage stress and to stay well, was significantly related to students’ well-being and distress [31]. Similarly, Henttonen et al. combined attributes of mental toughness, grit, hardiness, resilience, hope and self-efficacy with personality traits and studied the effects of beneficial and harmful sisu on the happiness and wellbeing of survey participants [30]. Likewise, VanTongeren et. al. developed a unique scale for spiritual fortitude which predicted variance in meaning in life, spiritual well-being, religious coping and adversity-related anxiety [32]. Our study and the Healthcare Fortitude Scale (HF-12) extends these studies conceptually and relies on well-established constructs and validated instruments. Furthermore, we validate this scale so that it is applicable to healthcare workers.
Second, our findings support and extend research examining the impact of resilience on burnout [24, 25]. In a study by Roslen et. al. the authors contend the concept of resilience has unfortunately been used interchangeably with mental toughness, hardiness, and grit, adding to confusion in the literature [43]. Stoffel and Cain likewise state that it is often difficult to tell whether the constructs of resilience, grit, hardiness and mental toughness are distinct from each other as some authors use these terms interchangeably [44]. Consequently, by combining these concepts using the HCF-12, our findings support and extend this research by empirically demonstrating that an elevated concept of fortitude is a better and more precise construct than an expanded definition of resilience. Furthermore, our fortitude measure explains more variance than any of the individual concepts, including resilience alone, proving that the combination of constructs is better than any single one alone.
Third, the findings from this study may help to change the conversation regarding physician burnout and turnover intent. Our work suggests that the interpersonal attribute of fortitude leads to decreased burnout and turnover intent. Moreover, fortitude can be viewed as attitudinal and therefore malleable when compared to personality traits. Subsequently, it may help explain the interaction between each individual and their work environment. As such, interventions that are mindful of empowering individuals to develop fortitude in addition to changes in the work environment may lead to faster progress in mitigating this important issue in healthcare.
Limitations and future research
We recognize potential limitations of the current study. First, we used a cross-sectional sample, collected at one point in time. Second, we recognize the possibility of common-methods bias, even though cross-sectional sampling is considered an acceptable method of collecting perceptual data [45].
Future research should strive to obtain longitudinal data and sources of secondary data to improve criterion-related validity. Likewise, future research on fortitude may want to consider the impact of fortitude on organizational context measures, such as perceived supervisor support (PSS) and organizational culture. It may not be the environment or the person alone, but the interaction between the adequacy of the multiple skills and attributes of the individual with ever evolving demands of the environment that contributes to wellbeing. Given the encouraging measures of validity and reliability of the HCF-12, future research can also test the moderating and mediating roles of fortitude on the relationship between work stress and burnout, work stress and turnover intent and burnout and turnover intent. Finally, this research was performed on a U.S.-based sample. Future research can assess fortitude among physicians in other countries to increase generalizability.
Conclusion
This study represents the first attempt to define and measure fortitude using a U.S.-based sample in a healthcare environment. Moreover, this study develops a valid, reliable and generalizable scale that extends our understanding of antecedents that lead to physician burnout and turnover intent. As a malleable attribute, fortitude also provides new opportunities for targeted intervention strategies to improve physician wellbeing.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Shanafelt TD, West CP, Dyrbye LN, Trockel M, Tutty M, Wang H, Carlasare LE, Sinsky C. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clin Proc. 2022;97(12):2248–58 Elsevier.
Ortega MV, Hidrue MK, Lehrhoff SR, Ellis DB, Sisodia RC, Curry WT, Del Carmen MG, Wasfy JH. Patterns in physician burnout in a stable-linked cohort. JAMA Netw Open. 2023;6(10):e2336745-.
Li CJ, Shah YB, Harness ED, Goldberg ZN, Nash DB. Physician burnout and medical errors: exploring the relationship, cost, and solutions. Am J Med Qual. 2023;38(4):196–202.
Williams ES, Rathert C, Buttigieg SC. The personal and professional consequences of physician burnout: a systematic review of the literature. Med Care Res Rev. 2020;77(5):371–86.
Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, Fiscus LC, Trockel M, Goh J. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784–90.
Brown PA, Slater M, Lofters A. Personality and burnout among primary care physicians: an international study. Psychol Res Behav Manag. 2019;18:169–77.
Meredith LS, Bouskill K, Chang J, Larkin J, Motala A, Hempel S. Predictors of burnout among US healthcare providers: a systematic review. BMJ Open. 2022;12(8):e054243.
Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129–46 Elsevier.
Greep NC, Woolhandler S, Himmelstein D. Physician Burnout: Fix the Doctor or Fix the System? Am J Med. 2022;135(4):416–7.
Kruse CS, Mileski M, Dray G, Johnson Z, Shaw C, Shirodkar H. Physician burnout and the electronic health record leading up to and during the first year of COVID-19: systematic review. J Med Internet Res. 2022;24(3):e36200.
Speicher LL, Francis D. Improving employee experience: reducing burnout, decreasing turnover and building well-being. Clin Gastroenterol Hepatol. 2023;21(1):11–4.
West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–29.
Haslam A, Tuia J, Miller SL, Prasad V. Systematic review and meta-analysis of randomized trials testing interventions to reduce physician burnout. Am J Med. 2023;137:249–257.e1. https://doi.org/10.1016/j.amjmed.2023.10.003.
Catapano P, Cipolla S, Sampogna G, Perris F, Luciano M, Catapano F, Fiorillo A. Organizational and individual interventions for managing work-related stress in healthcare professionals: a systematic review. Medicina. 2023;59(10):1866.
McManus IC, Winder B, Paice E. How consultants, hospitals, trusts and deaneries affect pre-registration house officer posts: a multilevel model. Med Educ. 2002;36(1):35–44.
McManus IC, Keeling A, Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: a twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2(1):1–2.
Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92(6):1087.
Lee DH, Reasoner K, Lee D. Grit: what is it and why does it matter in medicine? Postgrad Med J. 2023;99(1172):535–41.
Shakir HJ, Cappuzzo JM, Shallwani H, Kwasnicki A, Bullis C, Wang J, Hess RM, Levy EI. Relationship of grit and resilience to burnout among US neurosurgery residents. World Neurosurg. 2020;1(134):e224–36.
Miyawaki Y, Sada KE, Shidahara K, Nawachi S, Asano Y, Katayama Y, Hayashi K, Katsuyama E, Katsuyama T, Takano-Narazaki M, Matsumoto Y. The Association of Grit With Burnout Components (Professional Efficacy, Exhaustion, and Cynicism) Among Academic Rheumatologists: The TRUMP: 2: SLE Study. J Clin Rheumatol. 2023;29(6):268–74.
Kobasa SC. Stressful life events, personality, and health: an inquiry into hardiness. J Pers Soc Psychol. 1979;37(1):1.
Ladstätter F, Cooper-Thomas HD, Moreno-Jiménez B, Ponsoda V, Song S, Garrosa E. Deciphering hardiness: differential relationships of novelty seeker, rigid control, and hardy profiles on nurses’ burnout and their effects. Nurs Adv Health Care. 2018;2(1):1–8.
Vagni M, Maiorano T, Giostra V, Pajardi D, Bartone P. Emergency stress, hardiness, coping strategies and burnout in health care and emergency response workers during the COVID-19 pandemic. Front Psychol. 2022;21(13):918788.
Britt TW, Shen W, Sinclair RR, Grossman MR, Klieger DM. How much do we really know about employee resilience? Ind Organ Psychol. 2016;9(2):378–404.
Siu OL, Hui CH, Phillips DR, Lin L, Wong TW, Shi K. A study of resiliency among Chinese health care workers: Capacity to cope with workplace stress. J Res Pers. 2009;43(5):770–6.
Jones G, Hanton S, Connaughton D. A framework of mental toughness in the world’s best performers. Sport Psychol. 2007;21(2):243–64.
Lin Y, Clough PJ, Welch J, Papageorgiou KA. Individual differences in mental toughness associate with academic performance and income. Pers Individ Differ. 2017;15(113):178–83.
Passmore S, Hemming E, McIntosh HC, Hellman CM. The relationship between hope, meaning in work, secondary traumatic stress, and burnout among child abuse pediatric clinicians. Perm J. 2020;24:19.087.
Vetter MH, Vetter MK, Fowler J. Resilience, hope and flourishing are inversely associated with burnout among members of the Society for Gynecologic Oncology. Gynecol Oncol Rep. 2018;1(25):52–5.
Henttonen P, Määttänen I, Makkonen E, Honka A, Seppälä V, Närväinen J, García-Velázquez R, Airaksinen J, Jokela M, Lahti EE. A measure for assessment of beneficial and harmful fortitude: development and initial validation of the Sisu Scale. Heliyon. 2022;8(11):e11483.
Pretorius TB, Padmanabhanunni A. The dynamics of appraisal: a review of 20 years of research using the Fortitude Questionnaire. South Afr J Psychol. 2021;51(1):158–74.
Van Tongeren DR, Aten JD, McElroy S, Davis DE, Shannonhouse L, Davis EB, Hook JN. Development and validation of a measure of spiritual fortitude. Psychol Trauma Theory Res Pract Policy. 2019;11(6):588.
Hinkin TR. A review of scale development practices in the study of organizations. J Manag. 1995;21(5):967–88.
Carmines EG, Zeller RA. Reliability and Validity Assessment. Quantitative applications in the social sciences. Beverly Hills, London: Sage Publications; 1979. no. 07–017.
Crocker L, Algina J. Introduction to classical and modern test theory. Holt, Rinehart and Winston, 6277 Sea Harbor Drive, Orlando, FL 32887; 1986.
Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. 1999;4(3):272.
Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39(1):31–6.
Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto: Consulting Psychologists Press; 1996.
Lim VK, Chen D, Aw SS, Tan M. Unemployed and exhausted? Job-search fatigue and reemployment quality. J Vocat Behav. 2016;1(92):68–78.
Hamidi MS, Bohman B, Sandborg C, Smith-Coggins R, De Vries P, Albert MS, Murphy ML, Welle D, Trockel MT. Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res. 2018;18:1–8.
Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and health care workforce turnover. Ann Fam Med. 2019;17(1):36–41.
Rabatin J, Williams E, Baier Manwell L, Schwartz MD, Brown RL, Linzer M. Predictors and outcomes of burnout in primary care physicians. J Prim Care Community Health. 2016;7(1):41–3.
Roslan NS, Yusoff MS, Morgan K, Razak AA, Shauki NI. Evolution of Resilience Construct, Its Distinction with Hardiness, Mental Toughness, Work Engagement and Grit, and Implications to Future Healthcare Research. Educ Med J. 2022;14(1).
Stoffel JM, Cain J. Review of grit and resilience literature within health professions education. Am J Pharm Educ. 2018;82(2):6150.
Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psycho. 2003;88(5):879.
Acknowledgements
The authors have no acknowledgements.
Funding
The authors have no sources of funding to declare.
Author information
Authors and Affiliations
Contributions
LW and SH both wrote the main manuscript and (1) ensure that original data/original figures/materials/code upon which the submission is based are preserved following best practices in the field so that they are retrievable for reanalysis; (2) confirm that data/figures/materials/code presentation accurately reflects the original; and (3) foresee and minimize obstacles to the sharing of data/materials/code described in the work. Both authors were involved in writing every section of the manuscript. LW performed the statistical analyses. SH created all tables and figures. Neither author utilized any editorial services when writing this manuscript. All information is original. Both authors reviewed the final manuscript before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved in accordance of the Declaration of Helsinki by The University of Illinois Institutional Review Board (IRB), including protocol, consent to participate (IRB number is 1952792).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Weinzimmer, L., Hippler, S. New insights into physician burnout and turnover intent: a validated measure of physician fortitude. BMC Health Serv Res 24, 748 (2024). https://doi.org/10.1186/s12913-024-11186-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11186-7