Abstract
Background
To ensure a safe patient discharge from hospital it is necessary to transfer all relevant information in a discharge summary (DS). The aim of this study was to evaluate a bundle of measures to improve the DS for physicians, nurses and patients.
Methods
In a double-blind, randomized, controlled trial, four different versions of DS (2 original, 2 revised) were tested with physicians, nurses and patients. We used an evaluation sheet (Case report form, CRF) with a 6-point Likert scale (1 = completely agree; 6 = strongly disagree).
Results
In total, 441 participants (physicians n = 146, nurses n = 140, patients n = 155) were included in the study. Overall, the two revised DS received significant better ratings than the original DS (original 2.8 ± 0.8 vs. revised 2.1 ± 0.9, p < 0.001). Detailed results for the main domains are structured DS (original 1.9 ± 0.9 vs. revised 2.2 ± 1.3, p = 0.015), content (original 2.7 ± 0.9 vs revised 2.0 ± 0.9, p < 0.001) and comprehensibility (original 3.8 ± 1.2vs. revised 2.3 ± 1.2, p < 0.001).
Conclusion
With simple measures like avoiding abbreviations and describing indications or therapies with fixed contents, the DS can be significantly improved for physicians, nurses and patients at the same time.
Trial registration
First registration 13/11/2020 NCT04628728 at www.clinicaltrials.gov, Update 15/03/2023.
Key messages
1. To ensure a safe patient discharge from hospital it is necessary to transfer all relevant information in a discharge summary (DS).
2. Several issues related to the medical DS have already been identified delayed transmission of the DS to the subsequently treating physician and others, low quality or lack of information, lack of consistent formats, lack of patient understanding, and inadequate training for medical students in writing medical DS.
3. It would also be necessary that the patients understand the DS; - or at least receive therapeutically relevant care information in form of a patient-directed DS.
4. With simple measures like avoiding abbreviations and describing fixed content, the DS can be significantly improved for patients, physicians, and nurses at the same time.
5. The DS should become a patient‐centred tool ensuring that improved communication and understanding between healthcare professionals, patients and relatives succeeds.
Similar content being viewed by others
Introduction
To ensure a safe patient discharge from hospital it is necessary to transfer all relevant information in a discharge summary (DS). It is known that poor-quality discharge communications, orally and written, can lead to adverse outcomes, such as preventable readmissions [1, 2]. Moreover, there can be a negative impact on further patient care and health outcomes [3, 4].
Several issues related to the medical DS have already been identified in a review such as delayed transmission of the DS to the subsequently treating physician and others, low quality or lack of information, lack of consistent formats, lack of patient understanding, and inadequate training for medical students in writing medical DS [5].
Moreover, the use of unexplained abbreviations of medical terms may influence effective communication with all involved parties (physicians, nurses, patients and relatives) and cause relevant information to go unnoticed [6].
According to Austrian law, every patient must receive a medical DS at discharge and patients are owners of their written DS [7]. Therefore, it would also be necessary that the patients understand the DS;—or at least receive therapeutically relevant care information in form of a patient-directed DS. A study by Lin et al. [8] showed, that a simple patient-directed DS at discharge significantly improved the patient’s understanding of their illness and post discharge recommendations.
As part of preliminary projects, we have been working on the topic of communication and information in healthcare and especially on the improvement of the medical DS. In this present trial (GO-SAFE – safe discharge from hospital), existing DS of a University Hospital were analysed. First, we summarized general risks regarding medical discharge information in a review. The results of this systematic literature research indicate notable risk factors relating to the medical DS [5]. Secondly, physicians (n = 1060) in Styria were asked which content is important to them, what contribution the current DS is making to promote the individual health literacy of patients and for whom it is important [9]. The DS should (for the most part) satisfy the needs of physicians, nurses and patients for effective discharge communication. This was also shown in preliminary survey of inpatients conducted at regular intervals in the University Hospital in Graz demonstrated that patients frequently lacked clarity about their post-discharge treatment, therapy, and medication options. Thirdly, 100 DS were systematically analysed according to their content and strengths and weaknesses [6]. We have identified a significant issue with important items being missing in the DS as comprehensive medication history and clear recommendations for future medication. Furthermore, unclear abbreviations were regularly used. Fourth, timely delivery to doctor and patient was verified.
Based on this preliminary work, we have established quality criteria for a good DS. The main objective of this double-blind, randomized, controlled trial was to evaluate measures to improve the DS for physicians, nurses, and patients as the target groups of the document.
Methods
Pre-trial
In a randomized, controlled, participant-blind trial we tested two conventional DS (one surgical DS, one internal medicine DS) and revised versions of these DS. Medical undergraduates were randomized into two groups (original vs. revised) and asked to assess the assigned letter for the 3 domains i) structure, ii) content, and iii) patient-friendliness. We used an evaluation sheet (Case report form, CRF) with a 6-point Likert scale (1 = completely agree; 6 = strongly disagree): The results of the CRF were compared using the Mann-Whitney-U-Test with a p < 0.05 being the level of significance. In total, 74 undergraduates participated in the study [10]. Based on the pre-study the main study was designed.
Main trial
In the main trial, two randomly selected original written DS (Department of Internal Medicine – Division of Gastroenterology and Department of Surgery—Division of Plastic, Aesthetic and Reconstructive Surgery, Medical University of Graz) with a minimum length of two pages were selected by a member of an independent department (University Hospital Graz—Controlling). DS were revised with the following 5 key principles: i) short sentences, ii) no unexplained abbreviations, iii) large font size, iv) avoidance of technical terms (especially with the recommendations), and v) no more than 4 pages of length. The DS head was identical in both letters. Patient's data were blackened in the same way in both letters. The main structure in the revised DS was according to the guidelines of the final version of the HL7 Implementation Guide for discharge letters for ELGA [11]. Based on this HL7 Implementation Guide a DS must contain the following sub-headings:
-
Reason for admission
-
Discharge diagnosis, secondary diagnoses
-
Diagnostic and therapeutic measures
-
Recommended medication – including tradename, active substance, route of administration, prescription, and dosage
-
Therapeutic recommendations
-
Information on possible allergies, intolerances, and individual risk factors (e.g., miscellaneous implants)
-
Summary of diagnostic findings
-
Anamnesis (optional)
A detailed prescription can be found in the supplement (supplement Table 1).
Missing content, e.g., information on allergies, was added according to the given structure. The design of re-worked DS was identical to the specifications of the University Hospital Graz to make it difficult to distinguish between the original and revised DS versions.
Evaluation sheet (Case report form)
For the evaluation process, an evaluation sheet (CRF) with 3 main domains was used: i) structure, ii) content, and iii) patient-friendliness. Every section could be rated on a 6-point Likert scale (1 = completely agree, 6 = strongly disagree). The global indicator, along with the three main domains, is computed by averaging their respective items. Thus, the scale once again falls between 1 and 6, with lower scores indicating better outcomes. The evaluation sheet can be found in the supplement (supplement CRF).
Study design
The four documents (2 original DS, 2 revised DS) were tested randomly and double-blind. One of the four versions of the DS was randomly distributed to each participant in a closed envelope. Neither the participant nor the examiner knew who got which version. The target groups were physicians, nurses, and patients. Unblinding took place during the statistical analysis. A detailed description can be found in Fig. 1.
Participants and recruitment process
Based on our pre-study it was planned to recruit a minimum of 61 participants per group over a period of 3 months (June to August 2019). If a participant agreed to take part in the study, the participant was randomly allocated to one of the four groups and received the selected version of the DS and an evaluation sheet. The evaluation sheet was returned in a sealed envelope.
Physicians
Physicians were recruited from four different departments (Department of Surgery; Department of Internal Medicine; Department of Ear, Nose and Throat, Department of Psychiatry) at the University Hospital of Graz. The physicians received verbal information from a trained physician. Inclusion criteria were to be a trained physician and willingness to participate.
Nurses
Nurses were recruited by the management of Volkshilfe Steiermark, a large nursing home institution. They received verbal information from a trained head nurse. Inclusion criteria were to be a trained nurse and willingness to participate.
Patients
Patients were recruited from two Departments (Department of Internal Medicine – Division of Gastroenterology and Department of Surgery—Division of Plastic, Aesthetic and Reconstructive Surgery) at the University Hospital of Graz. Patients received verbal information from a trained physician as well as an informed consent form.
Statistical methods
The items in the main domains of the survey were rated from the categories ‘completely agree’ (score 1) to ‘strongly disagree’ (score 6). Indicators, which are defined as the mean of subsets of the items, were descriptively analysed using means and standard deviations. A subgroup analysis was carried out to determine possible gender-specific differences. Differences between the two groups, the original and revised DS, were determined by t-Test. A p-value of < 0.05 was considered significant. All analyses were performed using R (version 3.6.1).
Ethics statement
The Ethics Committee of the Medical University of Graz approved this study (EK 30–178 ex 17/18).
Reporting
The research and reporting methodology followed the SQUIRE 2.0 [12] and CONSORT guidelines.
Results
In total, 441 participants (physicians n = 146, nurses n = 140 and patients n = 155) were included in the study. A detailed description can be found in Table 1.
For each group, the numbers of participants were randomly assigned to the DS, allocated to groups and subgroups, and were analysed for the primary outcome.
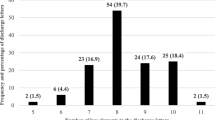
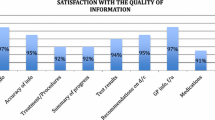
Overall, the two revised DS received significant better ratings (global indicator include all domains) than the original DS (original n = 224; 2.8 ± 0.8 vs. revised n = 217; 2.1 ± 0.9, p < 0.001). Detailed results for the main domains were structure (original 1.9 ± 0.9 vs. revised 2.2 ± 1.3, p = 0.015), content (original 2.7 ± 0.9 vs. revised 2.0 ± 0.9, p < 0.001) and comprehensibility (original 3.8 ± 1.2 vs. revised 2.3 ± 1.2, p < 0.001). Details can be found in Table 2 and Fig. 2.
Results by groups
Physicians
Physicians rated the global indicator for the original “surgery” DS (2.6 ± 0.7) significantly worse than the revised “surgery” DS (2.2 ± 0.7). Physicians rated the global indicator for the original “internal medicine” DS (2.6 ± 0.7) and for the revised “internal medicine” DS (2.4 ± 0.9) almost equally. A striking difference was the topic of structure in the new version of “surgery” DS (original 1.9 ± 1.0 vs. revised 2.7 ± 1.3) and “internal medicine” DS (original 1.8 ± 0.9 vs. revised 3.1 ± 1.5).
Nurses
Nursing staff rated the global indicator of the original “surgery” DS (2.7 ± 0.7) significantly worse than the revised “surgery” DS (2.0 ± 1.0). Nurses rated the global indicator of the original “internal medicine” DS (2.8 ± 0.7) significantly worse than the revised “internal medicine” DS (1.7 ± 0.7).
Patients
Patients rated the global indicator of the original “surgery” DS (2.7 ± 0.8) significantly worse than the revised “surgery” DS (2.0 ± 0.70). Patients rated the global indicator of the original “internal medicine” DS (3.2 ± 1.0) significantly worse than the revised “internal medicine” DS (2.1 ± 1.2).
An overview can be found in Table 3 and Fig. 3.
Results by gender
Female participants (global indicator) rated the original DS (2.8 ± 0.8) and the revised DS (2.0 ± 0.9) DS. Male participants (global indicator) rated the original DS (2.8 ± 0.8) and the revised (2.2 ± 0.8) DS.
An overview can be found in Table 4 and Fig. 4.
Discussion
Overall, the study evaluated a bundle of measures to improve the DS for physicians, nurses and patients. The findings of the evaluation can be considered an expression of the opinions of the respective groups with their own experiences. It is worth noting that, to date, no comparable study has been conducted using the same methodology. In this trial we found out that the revised DS reached significantly better ratings than the original ones.
Results showed that the original DS received already good ratings, but with simple measurements, like short sentences, no use of unexplained abbreviations, large font size, avoidance of technical terms (especially within the recommendations for health-promoting behaviour) in a standardized structure with no more than 4 pages length there could be a significant improvement. Beside these formal aspects it is also important to ensure that the discharge summary is given to the patient at discharge and that it is sent at the appropriate time to the further treating physician. Moreover, the importance of this topic should be highlighted in education and training.
The Patient Oriented Discharge Summary (PODS) is an individualized discharge tool designed with patient and family engagement that contains five sections of information that are actionable and useful for patients and families [13].
Patients, as the primary owners of their DS, rated the revised version significantly better. Since many people in Austria have a mediocre health literacy, it seems particularly important to formulate certain contents of the DS, such as instructions and further recommendations, in a way that is particularly comprehensible to the patients [14]. To communicate “about” rather than “with” patients still reflects historical behavior but is no longer deemed appropriate [9].
The evaluation of the DS was not uniform in all areas. Physicians rated the new structure in the DS significantly worse than in the original DS. Prior to the implementation of the electronic fever chart and standardised structure, the different clinics had employed varying formats for discharge summaries in Austria. General changes in the usual structure were sometimes not perceived as pleasant. However, the universal structure of the DS is specified by ELGA and now mandatory.
Nurses rated the revised DS significantly better as well. A good transfer of knowledge and information to the nursing staff is in general particularly relevant because nurses care for patients in their homes or nursing homes.
A future recommendation could therefore be, that all professional groups have a joint DS [15]. Poor information and communication between the professional groups, patients and relatives during the discharge process is a risk to patient safety, and further research could investigate this impact. As far as possible, the DS should be adapted to the needs of the addressees. Great attention must be paid to the use of resources. Electronic documentation and Artificial Intelligence can contribute to this [16,17,18].
In practice there are examples of “own” patient DS [8, 19, 20]. The DS should become a patient‐centred tool ensuring that improved communication and understanding between healthcare professionals, patients and relatives succeeds. Many positive effects, such as increased patient satisfaction, increased understanding and a greater patient involvement, were shown [21]. This should be achieved without reducing the medically relevant content.
Strengths and limitations of the study
A strength of this study was the design of the trial as all stakeholders namely patients, physicians, and nurses were involved. The newly developed DS can support them all at the same time. However, the study does not allow to verify whether the revised discharge letters actually contribute to better patient care.
There are some limitations in this study. First, the physicians may have noticed that there are differences to the letters from their own department. However, this bias is negligible since each University hospital has different formats and structures at the University Hospital of Graz. Basically, only the letterhead was uniform across the clinic. Secondly, in this study, we only examined and revised two randomly selected DS.
Conclusions
The aim of this study was to evaluate a bundle of measures to improve the DS for physicians, patients, and nurses. It can be stated that across all groups, the revised version of the DS received significant better ratings by all participants. Only the item of structure, which is mandatory by ELGA regulations, received a poorer rating in the new version exclusively from the physicians surveyed. To summarize, small improvements can make a difference for all groups at the same time.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Contact details: Magdalena Hoffmann. Medical University of Graz, Auenbruggerplatz 29/4, 8036 Graz, Austria, Email: Magdalena.hoffmann@medunigraz.at, Telephone: + 43 316 385 80,804.
Abbreviations
- DS:
-
Discharge Summary
- e.g.:
-
Exempli gratia
- ELGA:
-
“Elektronische Gesundheitsakte” – Austrian Electronic Health Records
- IQR:
-
Interquartile ranges
- CRF:
-
Case Repot Form
- SQUIRE:
-
Standards for Quality Improvement Reporting Excellence
- PODS:
-
Patient Oriented Discharge Summary
- IT :
-
Information Technology
References
Groene RO, Orrego C, Suñol R, Barach P, Groene O. ‘It’s like two worlds apart’: an analysis of vulnerable patient handover practices at discharge from hospital. https://doi.org/10.1136/bmjqs-2012-001174.
Lorenzati B, Quaranta C, Perotto M, Tartaglino B, Lauria G. Discharge communication is an important underestimated problem in emergency department. Intern Emerg Med. 2016;11:157–8.
Moore C, Mcginn T, Halm E. Tying up loose ends discharging patients with unresolved medical issues. 2007. https://jamanetwork.com/.
Perren A, et al. Omitted and unjustified medications in the discharge summary. Qual Saf Heal Care. 2009;18:205–8.
Schwarz CM, et al. A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients’ safety. BMC Health Serv Res. 2019. https://doi.org/10.1186/s12913-019-3989-1.
Schwarz CM, et al. Structure, content, unsafe abbreviations, and completeness of discharge summaries: A retrospective analysis in a University Hospital in Austria. J Eval Clin Pract. 2021. https://doi.org/10.1111/jep.13533.
Kuranstaltengesetz Kundmachungsorgan, K. Krankenanstalten- u. Kuranstaltengesetz § 24. vol. 124. 2009. Access on https://www.ris.bka.gv.at/.
Lin R, et al. Effect of a patient-directed discharge letter on patient understanding of their hospitalisation. Intern Med J. 2014;44:851–7.
Hoffmann M, et al. Attitudes of physicians towards target groups and content of the discharge summary: a cross-sectional analysis in Styria. Austria BMJ Open. 2019;9: e034857.
Smolle C, et al. Design and preliminary evaluation of a newly designed patient-friendly discharge letter – a randomized, controlled participant-blind trial. BMC Health Serv Res. 2021;21:450.
ELGA GmbH. ELGA CDA Implementierungsleitfäden HL7 Implementation Guide for CDA®R2: Entlassungsbrief (Ärztlich). 2017. https://www.elga.gv.at/fileadmin/user_upload/Dokumente_PDF_MP4/CDA/Implementierungsleitfaeden/Leitfaeden_2017_02/HL7_Implementation_Guide_for_CDA_R2_-_Entlassungsbrief_AErztlich_2.06.2.pdf. Accessed 23 Feb 2023.
Ogrinc, G. et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. J. Contin. Educ. Nurs. (2015) doi: 10.3928/00220124-20151020-02.
Hahn-Goldberg S, et al. Implementation, spread and impact of the Patient Oriented Discharge Summary (PODS) across Ontario hospitals: a mixed methods evaluation. BMC Health Serv Res. 2021. https://doi.org/10.1186/s12913-021-06374-8.
Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. https://doi.org/10.1186/1471-2458-12-80.
Carlsson E, Ehnfors M, Ehrenberg A. Multidisciplinary recording and continuity of care for stroke patients with eating difficulties. J Interprof Care. 2010. https://doi.org/10.3109/13561820903011976.
Dean SM, Gilmore-Bykovskyi A, Buchanan J, Ehlenfeldt B, Kind AJH. Design and Hospitalwide Implementation of a Standardized Discharge Summary in an Electronic Health Record. Jt Comm J Qual Patient Saf. 2016. https://doi.org/10.1016/S1553-7250(16)30107-6.
Callen JL, Alderton M, McIntosh J. Evaluation of electronic discharge summaries: A comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77:613–20.
Murphy SF, et al. Electronic discharge summary and prescription: improving communication between hospital and primary care. Ir J Med Sci. 2017. https://doi.org/10.1007/s11845-016-1397-7.
Hahn-Goldberg S, et al. Implementing Patient-Oriented Discharge Summaries (PODS): A Multisite Pilot Across Early Adopter Hospitals. Healthc Q. 2016. https://doi.org/10.12927/hcq.2016.24610.
Patientenbriefe wirken: Ergebnisbericht zum Forschungsprojekt "Mehr Gesundheitskompetenz durch Patientenbriefe". https://washabich.de/aktuelles/319/Patientenbriefe-wirken. Accessed 24 Feb 2023.
VanSuch M, Naessens JM, Stroebel RJ, Huddleston JM, Williams AR. Effect of discharge instructions on readmission of hospitalised patients with heart failure: Do all of the Joint Commission on Accreditation of Healthcare Organizations heart failure core measures reflect better care? Qual Saf Heal Care. 2006;15:414–7.
Acknowledgements
Special thanks go to David Lippitsch, Alexandra Winter and Lydia Jantscher for the support with Evasys. Our thanks also go to all study participants as well as the Styrian Health Fund (Gesundheitsfonds Steiermark), Volkshilfe Steiermark, the Medical University of Graz and the University Hospital Graz.
Funding
This work was supported by the Medical University of Graz and the University Hospital of Graz as well as by the Gesundheitsfonds Steiermark.
Author information
Authors and Affiliations
Contributions
Guarantor: CMS, MH. Study concept and design: CMS, MH, VG, LK, GS. Acquisition of data: CS, SF, AT, AK, MH. Analysis and interpretation of pooled data: MH, CS, AB. Drafting of the manuscript: CMS, MH, SF. Critical revision of the manuscript for important intellectual content: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects. The Ethics Committee of the Medical University of Graz approved this study (EK 30–178 ex 17/18).
Consent for publication
All authors confirmed the publication in its present form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Schwarz, C.M., Hoffmann, M., Smolle, C. et al. Patient-centered discharge summaries to support safety and individual health literacy: a double-blind randomized controlled trial in Austria. BMC Health Serv Res 24, 789 (2024). https://doi.org/10.1186/s12913-024-11183-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11183-w