Abstract
Background
Multimorbidity of non-communicable diseases (NCDs) is increasingly prevalent among older adults around the world, leading a higher risk of household catastrophic health expenditure (CHE). As current powerful evidence was insufficient, we aimed to estimate the association between multimorbidity of NCDs and the risk of CHE in China.
Methods
We designed a cohort study using data investigated in 2011–2018 from the China Health and Retirement Longitudinal Study, which is a nationally-representative study covering 150 counties of 28 provinces in China. We used mean ± standard deviation (SD) and frequencies and percentages to describe baseline characteristics. Person χ2 test was employed to compare the differences of baseline characteristics between households with and without multimorbidity. Lorenz curve and concentration index were used to measure the socioeconomic inequalities of CHE incidence. Cox proportional hazards models were applied to estimate adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) for the association between multimorbidity and CHE.
Results
Among 17,708 participants, 17,182 individuals were included for the descriptive analysis of the prevalence of multimorbidity in 2011, and 13,299 individuals (8029 households) met inclusion criteria and were included in the final analysis with a median of 83 (interquartile range: 25–84) person-months of follow-up. 45.1% (7752/17,182) individuals and 56.9% (4571/8029) households had multimorbidity at baseline. Participants with higher family economic level (aOR = 0.91, 95% CI: 0.86–0.97) had lower multimorbidity prevalence than those with lowest family economic level. 82.1% of participants with multimorbidity did not make use of outpatient care. The CHE incidence was more concentrated among participants with higher socioeconomic status (SES) with a concentration index of 0.059. The risk of CHE was 19% (aHR = 1.19, 95% CI: 1.16–1.22) higher for each additional NCD.
Conclusions
Approximately half of middle-aged and older adults in China had multimorbidity, causing a 19% higher risk of CHE for each additional NCD. Early interventions for preventing multimorbidity among people with low SES could be intensified to protect older adults from financial hardship. In addition, concerted efforts are needed to increase patients’ rational healthcare utilization and strengthen current medical security for people with high SES to reduce economic disparities in CHE.
Similar content being viewed by others
Background
In 2015, 17 goals for ending poverty, protecting the planet and improving the health of everyone everywhere, which are widely known as the Sustainable Development Goals (SDGs), were adopted by the United Nations [1]. Universal health coverage (UHC) is a main content of SDG target 3.8, which aims for all people to have access to the health services they need, when and where they need them, without financial hardship [2]. According to the World Health Organization (WHO), monitoring progress towards UHC should focus on 2 parts: how many people can receive essential quality health services and how much household income people spend on health. For the latter, catastrophic health expenditure (CHE), which is defined as out-of-pocket health expenditure exceeding a specific proportion of household financial capability, is a broadly used indicator despite inconsistent thresholds and denominators among studies [3].
To promote process towards UHC, the Chinese government introduced a series of policies. In the early 2000s, China developed three insurance programs: Urban Employee Basic Medical Insurance (UEBMI) for the employed urban population, the New Rural Cooperative Medical Scheme (NRCMS) for rural residents, and Urban Resident Basic Medical Insurance (URBMI) for urban residents who are unemployed or self-employed. In April 2009, China launched a major health care reform that included increasing financial investment to expand insurance coverage and intensify the development of basic medical institutions [4]. Since 2013, catastrophic medical insurance, which was introduced in 2012 and focused on providing supplementary coverage for patients with URBMI and the NRCMS, has covered more than 1 billion people, and benefited over 11 million people [5]. In 2016, President Xi Jinping announced Healthy China 2030, the country’s long-term health sector strategy for a healthy population in all aspects [6].
As early as2011, almost all people in China were insured by one of the abovementioned three social health insurance programs. After10 years of health care reform, China made substantial progress towards UHC, with a steady downward trend in the proportion of households with CHE during 2010–2018. [7] However, as non-communicable diseases (NCDs) are increasingly prevalent in China, additional medical needs and health expenditures are needed [8]. Using data from a national population-based screening project, Lu et al. [9] found that 44.7% of 1,738,886 participants in China had hypertension, only half of them were aware of their diagnosis, and only 7.2% had achieved control. Another nationally representative survey revealed that the estimated prevalence of diagnosed diabetes in China was 10.9% (95% confidence interval (CI): 10.4-11.5%) in 2013 and 12.4% (95% CI: 11.8-13.0%) in 2018, absolute increase of 1.4% (95% CI: 0.7-2.2%), and only 32.9% (95% CI: 30.9-34.8%) of individuals reported being treated [10]. Hence, further-integrated efforts need be made to consolidate current achievements and promote UHC.
With ageing of population, the prevalence of multimorbidity (defined as the coexistence of 2 or more NCDs in one person) is increasing among older adults. In a systematic review, the median prevalence of multimorbidity was 30.7% among all people in China, and it was about half of the prevalence among older adults [11,12,13]. Such a severe disease burden directly triggers a high amount of medical expenditure and CHE incidence. A national study conducted in China found that for each additional chronic disease, the risk of CHE increased by 39% (odds ratio (OR) = 1.39, 95% CI: 1.31–1.47). [14] Similarly, in a Chinese population-based panel study, the likelihood of CHE events increased with the number of NCDs (OR = 1.29, 95% CI: 1.26–1.32). [15] Therefore, the burden of multimorbidity in the older population is an urgent point that needs to be considered to reduce CHE, and to solve this problem needs more evidence about the effect of multimorbidity on CHE. However, current related results were obtained from cross-sectional studies with limited data, which cannot provide stronger facts about the association between multimorbidity and CHE or the long-term impacts of multimorbidity on CHE. Moreover, they did not analyze the socioeconomic inequalities of CHE incidence [14,15,16,17].
This study aimed to estimate the association of multimorbidity with CHE incidence among middle-aged and older adults through a population-based cohort study design using all wave data (2011, 2013, 2015, and 2018) from the China Health and Retirement Longitudinal Study (CHARLS).
Methods
Study design and participants
CHARLS is a nationally representative survey implemented by the National School of Development of Peking University of the middle-aged and older population of China, including individuals aged ≥ 45 years [18]. Considering the sample lost during follow-up and the long period of investigation, CHARLS included some people aged < 45 years if they met the inclusion criteria as a reserved sample for future interviews. The baseline survey was conducted between June 2011 and March 2012 and ultimately included 17,708 eligible participants from 150 counties of 28 provinces in China. CHARLS respondents were followed up every 2 years via face-to-face interviews with a structured questionnaire that included individual and family components. In the family component of the questionnaire, CHARLS selected one individual randomly from each household as the main respondent. Details about the design of CHARLS have been published elsewhere [18]. All data were openly available from the official CHARLS website (http://charls.pku.edu.cn/). The Biomedical Ethics Review Committee of Peking University approved CHARLS (ethical approval number IRB00001052-11015), and all subjects provided written informed consent before enrolment.
We designed a population-based cohort study using data from all waves (2011, 2013, 2015, and 2018) of CHARLS. The exposure at baseline was the number of NCDs, and the outcome was the onset of CHE. The participants were followed up until they had CHE onset or the interview ended. Among 17,708 participants selected in baseline survey, we excluded those who aged < 45 years (n = 415), had CHE at baseline (n = 2449), were lost to follow-up (n = 1501), and had missing data on baseline characteristics (n = 44). In addition, 5270 participants who were not the main respondents of households were excluded from the main household-related analysis. Finally, a total of 13,299 individuals and 8029 households (main respondents) were included in this study (Fig. 1). After excluding those aged < 45 years (N = 415) and those who had missing data on baseline characteristics (N = 111), 17,182 individuals were included in the analysis of the association between baseline characteristics and multimorbidity.
Measures of multimorbidity
In this study, we described multimorbidity as the cooccurrence of at least 2 chronic NCDs in the same person. We ascertained 14 self-reported diagnosed chronic disorders to measure multimorbidity by asking “Have you been diagnosed with the following conditions by a doctor: hypertension, dyslipidemia, diabetes or high blood sugar, cancer or malignant tumor, chronic lung diseases, liver disease, heart diseases, stroke, kidney disease, stomach or other digestive disease, psychiatric problems, memory-related diseases, arthritis or rheumatism, or asthma?”. We counted the number of NCDs from the answers of participants, and divided participants into 2 groups: those with multimorbidity (> 1 NCD) and those without multimorbidity (0 or 1 NCD).
Measures of household catastrophic health expenditure
Participants in CHARLS were asked about their use of outpatient care during the past month, inpatient care during the past year, and self-medication during the past month. The out-of-pocket (OOP) expenditure for each kind of medical service was reported by individuals. We multiplied the monthly spending by 12 to calculate the yearly OOP expenditure of outpatient care and self-medication for each participant. Then we calculated the self-medical OOP expenditure for each participant as the sum of the annual OOP expenditures of outpatient care, inpatient care, and self-medication and added it to their spouses’ as household medical OOP expenditure. In this study, a household with CHE was defined as having a household medical OOP expenditure exceeding 40% of the household’s capacity to pay (defined as the total household expenditure minus household food expenditure). [3] The annual household food expenditure was calculated as the weekly meal expenses divided by 7 and then multiplied by 365, and the annual total household expenditure was calculated as the sum of monthly basic expenditures (daily used commodities and necessities, communication, transportation, fuel, and so on) multiplied by 12 plus yearly special expenditures (clothing, travelling, education, furniture, and so on).
Covariates
To control for potential confounders in the association between multimorbidity and CHE, we included the following variables as covariates: gender (male, female), age group (45–54, 55–64, ≥ 65 years), marital status (married, other), education (illiterate/semiliterate, primary school, middle school, high school and above), insurance (no insurance, UEBMI, URBMI, NRCMS, other), outpatient services (yes, no), inpatient services (yes, no), family size (1–2, 3–4, ≥ 5), residence (urban, rural), family economic level (four classes), and socioeconomic development level (four classes).
Outpatient and inpatient services were identified by the questions “Have you visited a hospital or clinic center for outpatient care in the last month?” and “Have you received inpatient care in the past year?”. The family economic level was classified by the quartiles of household annual income (lowest: <4000 yuan; lower: 4000–16,799 yuan; higher: 16,800–38,399 yuan; highest: ≥38,400 yuan). The socioeconomic development level was identified by the quartiles of 2011 per capita gross regional product (GRP, lowest: <27,250 yuan; lower: 27,250–33,232 yuan; higher: 33,232–48,200 yuan; highest: ≥48,201 yuan), which were obtained from the 2011 China Statistical Yearbook [19].
Statistical analysis
We described baseline characteristics using means ± standard deviations (SDs) for continuous variables and frequencies and percentages for categorical variables. To compare the distributional differences in the characteristics of household heads with and without multimorbidity, we used the Pearson χ2 test.
The concentration index (C) and Lorenz curve were applied to evaluate the socioeconomic inequalities in CHE incidence. In this study, socioeconomic inequality was defined by dividing annual family income into quartiles (lowest, lower, higher, highest). C (ranging between − 1 and 1) is defined as twice the area between the concentration curve and the line of equality and can be calculated by the following formula:
where h refers to the health outcome (CHE), µ is the mean of h, and r denotes the fractional rank of individuals in family income quartiles. If C took a negative value, in this study, it indicated that CHE events are more concentrated among poor people. Conversely, if C was a positive value, it indicated that CHE events were more concentrated among rich people [20]. The Lorenz curve was plotted by the cumulative percentage of CHE incidence (Y-axis) against the cumulative percentage of the population ranked by family income (X-axis).
At the individual level, a logistic regression model was employed to estimate the adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for the association of baseline characteristics (gender, age group, marital status, education, insurance, family size, residence, family income level, and socioeconomic development level) with multimorbidity (with and without). At the household level, we applied univariate and multivariate Cox proportional hazards models to estimate the hazard ratios (HRs) and 95% CIs for the effect of multimorbidity on household CHE. In the multivariate Cox proportional hazards model, we adjusted for all the covariates, including gender, age group, marital status, education, insurance, outpatient services, inpatient services, family size, residence, family economic level, and socioeconomic development level.
To examine the robustness of estimations for the impact of multimorbidity on CHE, we performed three sensitivity analyses. First, we replaced the definition of CHE as household-medical OOP expenditure exceeding 25% of total household expenditure with the WHO definition. Second, we changed the original selected main respondents in households with 2 eligible respondents to the 5270 excluded participants and used the same fully-adjusted model. Third, we used the nighttime light level (divided into four classes according to the quartiles of 2011 province-level mean nighttime light intensity [21]) to indicate socioeconomic development rather than GRP.
To explore the possible different effects of the number of NCDs on CHE incidence among subpopulations, the analysis was stratified by age group, insurance, residence, family economic level, and socioeconomic development level, using the same fully-adjusted model but with the stratified variable removed.
Considering the national representativeness, multistage probability proportional to size (PPS) sampling and nonresponse rate of CHARLS, all data included in the analyses were weighted per the sampling probabilities [22]. All analyses were conducted in R 4.2.1 (R Core Team, Vienna, Austria). A two-side P value less than 0.05 was considered to be significant.
Results
Baseline individual characteristics and prevalence of multimorbidity
Among all 17,182 participants, the mean (SD) age was 59.4 (9.9) years. A total of 8364 (48.7%) participants were male, 14,948 (87.0%) were married or partnered, and only 1154 (6.7%) participants had no medical insurance. A total of 10,261 (59.7%) participants lived in rural areas, and 10,988 (64.0%) had more than 2 family members (Table 1). Weighted proportions were similar to unweighted results (Table S1).
At baseline, among a total of 17,182 participants, 7752 (45.1%) individuals had multimorbidity, and the weighted prevalence of multimorbidity was 44.3%. Logistic regression models revealed that participants with higher family economic level (aOR = 0.91, 95% CI: 0.86–0.97) had lower multimorbidity prevalence than those with lowest family economic level, and participants with lower (aOR = 0.81, 95% CI: 0.76–0.86) and highest (aOR = 0.90, 95% CI: 0.85–0.97) economic development levels were also less likely to have multimorbidity (Table 1).
Baseline household characteristics in the cohort study
Of the 10,257 households in CHARLS, 8029 households met all the inclusion criteria of this study. A total of 1134 (14.1%) and 505 (6.3%) household heads had outpatient and inpatient care at baseline, respectively. 4850 (60.4%) households were in rural areas, and 5266 (65.6%) households had more than 2 family members (Table 2).
In total 4571 (59.2%) households were defined as with multimorbidity because at least 1 member in this family had more than 1 NCD, and the weighted prevalence of multimorbidity among households was 56.6% (Table S2). 82.1% of household heads with multimorbidity did not make use of outpatient care in the last year (Table 2). Except for residence and family economic level, the distribution of baseline characteristics between households with multimorbidity and those without multimorbidity were significantly different (all p value < 0.05; Table 2).
CHE incidence and its socioeconomic disparities
Of 8029 households, during a median of 83 (interquartile range: 25–84) person-months of follow-up, up to 4260 households had CHE events, with an incidence rate of 8.5 per 1,000 person-months. The cumulative number of CHE events was 1521 (incidence rate: 6.6 per 1,000 person-month) for households without multimorbidity and 2739 (incidence rate: 10.2 per 1,000 person-months) for households with multimorbidity.
As depicted in Fig. 2, the Lorenz curve of CHE incidence was under the equal line with a concentration index of 0.059, which indicated that CHE events were more concentrated among people with higher socioeconomic status (pro-rich).
Lorenz curve of catastrophic health expenditure incidence. Notes: The Lorenz curve of catastrophic health expenditure incidence lay below the equal line with a concentration index of 0.059, which revealed that catastrophic health expenditure was concentrated in people with higher socioeconomic status
Association of multimorbidity with the risk of CHE
Both univariate and multivariate models revealed that a higher number of NCDs was significantly associated with an increased risk of CHE (Table 3 and Table S3). In the unadjusted model, the likelihood of CHE increased by 20% for each additional NCD (crude HR = 1.20, 95% CI: 1.17–1.23). In the fully adjusted model, an additional NCD led to a 19% increased risk of CHE (aHR = 1.19, 95% CI: 1.16–1.22).
In three sensitivity analyses, the significant association between multimorbidity and CHE incidence did not change when the definition of CHE was replaced as household-medical OOP expenditure exceeding 25% of total household expenditure by the WHO definition; or when the original selected main respondents in households with 2 eligible respondents were changed to the 5270 excluded ones; or when the socioeconomic development level was indicated by nighttime light level rather than GRP (Table 3).
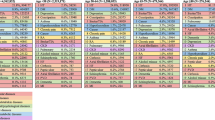
In subgroup analyses, except for household heads with URBMI, the negative effect of multimorbidity on CHE incidence did not appear to be modified by baseline characteristics, including gender, age, family size, residence, family economic level, or economic development level (all p values < 0.05; Fig. 3).
Subgroup analyses of the association between multimorbidity and risk of catastrophic health expenditure. Notes: aHR: adjusted hazard ratio; CI: confident interval; UEBMI: urban employee basic medical insurance; URBMI: urban resident basic medical insurance; NRCMS: new rural cooperative medical scheme. *Per 1000 person-months; † estimation of association between number of NCDs and risk of catastrophic health expenditure
Discussion
To our knowledge, this study is the first to explore and quantify the effect of multimorbidity on long-term CHE through a cohort study design. We found that multimorbidity was common among Chinese people aged 45 years and above, family economic level and socioeconomic development level were related to multimorbidity, CHE events were more concentrated among people with higher socioeconomic status, and multimorbidity was associated with an increased risk of long-term CHE incidence.
This study showed that the weighted prevalence of multimorbidity among middle-aged and older adults in China was 44.3% in 2011, which was lower than that in 3 other studies that also used data from CHARLS [12, 13, 23]. The gaps between our results and their results can be explained by differences in the included survey year and population age structure: the prevalence of multimorbidity was reported as 52.2% in 2011 (people aged ≥ 45 years with data on physical activity), 63.4% in 2015 (people aged ≥ 45 years), and 65.6% in 2018 (people aged ≥ 60 years) [12, 13, 23]. An upward trend in multimorbidity prevalence appeared with increasing age or year through data from CHARLS. Given that an NCD might not be resolved, the probability of multimorbid conditions increases with age.
We found that people with higher family economic level had a lower multimorbidity prevalence than those with lowest family economic level, and participants with lower and highest economic development levels were also less likely to have multimorbidity. People with lower socioeconomic status had higher multimorbidity prevalence, which was similar to the findings of other studies despite various indicators for defining socioeconomic status [24, 25]. People with lower socioeconomic status may have poor health literacy and unhealthy lifestyles (such as smoking and unhealthy diets), increasing the risk of NCDs and further resulting in multimorbidity [26, 27]. A systematic review revealed that people in lower socioeconomic groups had a significantly higher prevalence of tobacco and alcohol use, also they consumed less fruit, vegetables, fish and other healthy foods than people in high socioeconomic groups [26]. Additionally, people with low socioeconomic level might have less use of medical care. Zhao et al. [15] found that people in the highest expenditure group had a 20% increased number of outpatient visits than people in the lowest expenditure group. Another national study in Korea also demonstrated that the highest socioeconomic group had 58% higher healthcare utilization than other socioeconomic groups [28]. In view of this, more proactive interventions such as health education might be directed towards people in low socioeconomic groups to strengthen the prevention and management of multimorbidity.
From the analysis at the household level, we found that the percentages of households with multimorbidy that used outpatient care and inpatient care were 17.9% and 8.3%, respectively, which were almost twice those of households without multimorbidity (9.2% for outpatient care and 3.6% for inpatient care). A couple of studies drew the conclusions that because of deteriorating health conditions, multimorbidity accounted for more consultations in primary care, more frequent outpatient visits and longer lengths of inpatient stays [29,30,31]. Notably, 82.1% of participants with multimorbidity did not make use of outpatient care in the last month in our study. Because the regular management of NCDs in primary health care in China allows doctors to prescribe more than one month worth of drugs (i.e., prescription refills) for patients with stable chronic conditions [32, 33], the participantis included in our study might have visited clinics before the investigation month or planned to go to primary health insitutions after the investigation month. In addition, some individuals were unable to seek medical care for financial reasons. Insufficient treatment directly contributes to poor control of multimorbidity, leading to more severe health outcomes, which might require high medical costs to both households and society. To improve patients’ conditions and avoid financial hardship, concerted efforts from related health institutions could be made to increase patients’ rational healthcare utilization.
In addition, we found that CHE events were more concentrated among people with higher socioeconomic status, which was consistent with the findings of some studies but contrary to the findings of others [34, 35]. Given the definition of CHE, it can be summarized that both OOP medical expenditure and family financial capacity can determine the onset of CHE. Therefore, on the one hand, as shown in some studies, people with lower socioeconomic status may be more likely to incur CHE with lower income for calculating CHE. On the other hand, people with higher socioeconomic status might seek health services more frequently without worrying about medical expenditure, contributing to a lager molecule for calculating CHE. Several studies revealed that both health services distribution and utilization were concentrated among people with higher socioeconomic status [4, 36]. These people were prone to overuse high-quality tertiary hospitals with poor quality primary health care, which are distributed mostly in urban areas and require higher costs with lower reimbursement ratios [4]. Notably, a series of policies in China for decreasing the financial risk of health care were introduced with emphasis on rural populations, most with lower socioeconomic status, such as catastrophic health insurance, medical assistance, and basic life assistance [5, 37].
Our results also showed that the risk of long-term household CHE events was 19% higher for each additional NCD, which was consistent with other cross-sectional studies [14, 15]. Due to incurability, multimorbidity requires more long-term health care of reasonable quality (more frequent outpatient or inpatient visits and longer length of inpatient stays) for both primary and secondary health care services, which directly increases medical expenditure [15, 38, 39]. Considering that the early onset of NCDs increases the possibility for multimorbidity in later life, lifecycle management of multimorbidity for reducing CHE should be prioritized, including integrated activities for primary prevention of NCDs at early ages, timely control of the early state of NCDs, and efficient treatment for each NCD to delay the progression to disability and death.
The first strength of this study was its population-based cohort design, which provided more powerful evidence about the association of multimorbidity with CHE than current published cross-sectional studies [14,15,16,17]. Second, our study included more information because it used all wave data (2011–2018) from CHARLS with a longer time span than other studies that used only 1 wave of data [14,15,16,17]. Third, we focused on the socioeconomic inequities of CHE incidence in addition to the association of multimorbidity with CHE, which introduced new concerns and distinct emphasis on health policies among different populations. However, there are still several limitations in our study. First, survivor bias may exist in our cohort study because some households that had CHE at baseline were excluded, which might underestimate the CHE incidence, as the remaining sample might be less likely to have CHE. Second, data for measuring CHE, including medical expenditures, total expenditures, and food expenditures, were obtained from oral answers, which might lead to recall bias. Third, although the judgement of multimorbidity was conducted by asking participants if whether they had doctor-diagnosed NCDs, there might be inconsistencies with the real conditions because of different diagnostic procedures between doctors.
Conclusions
Approximately half of middle-aged and older adults in China had multimorbidity, and the risk of long-term household CHE events was 19% higher for each additional NCD. Integrated management and interventions for preventing multimorbidity could be intensified, especially in older populations with low socioeconomic status. In addition, concerted efforts to increase patients’ rational healthcare utilization, provide high-quality primary care, and strengthen medical security for people with high socioeconomic status might be made to advance progress towards UHC in China.
Data availability
All waves’ data from the CHARLS can be downloaded from the CHARLS official website (http://charls.pku.edu.cn/).
Abbreviations
- SDGs:
-
The Sustainable Development Goals
- UHC:
-
Universal health coverage
- WHO:
-
The World Health Organization
- CHE:
-
Catastrophic health expenditure
- UEBMI:
-
The Urban Employee Basic Medical Insurance
- NRCMS:
-
The New Rural Cooperative Medical Scheme
- URBMI:
-
The Urban Resident Basic Medical Insurance
- NCDs:
-
Non-communicable diseases
- CHARLS:
-
The China Health and Retirement Longitudinal Study
- OOP:
-
Out-of-pocket
- C:
-
Concentration index
- aORs:
-
Adjusted odds ratios
- CIs:
-
Confident intervals
- aHRs:
-
Adjusted hazard ratios
- GRP:
-
Gross regional product
References
UN. Sustainable Development Goals: 17 Goals to Transform our World [cited 2022-11-10]. Available from: https://www.un.org/en/exhibits/page/sdgs-17-goals-transform-world.
WHO. Universal Health Coverage 2022 [cited 2022-11-06]. Available from: https://www.who.int/health-topics/universal-health-coverage#tab=tab_1.
Cylus J, Thomson S, Evetovits T. Catastrophic health spending in Europe: equity and policy implications of different calculation methods. Bull World Health Organ. 2018;96(9):599–609.
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–204.
Li H, Jiang L. Catastrophic medical insurance in China. Lancet. 2017;390(10104):1724–5.
The CPC Central Committee and The State Council. Outline of the Healthy China 2030 Plan 2016 [cited 2022-11-13]. Available from: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm.
Liu C, Liu ZM, Nicholas S, Wang J. Trends and determinants of catastrophic health expenditure in China 2010–2018: a national panel data analysis. BMC Health Serv Res. 2021;21(1):526.
Fang EF, Xie C, Schenkel JA, Wu C, Long Q, Cui H et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64:101174.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE million persons project). Lancet. 2017;390(10112):2549–58.
Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–506.
Zhang X, Padhi A, Wei T, Xiong S, Yu J, Ye P, et al. Community prevalence and dyad disease pattern of multimorbidity in China and India: a systematic review. BMJ Glob Health. 2022;7(9):e008880.
He L, Biddle SJH, Lee JT, Duolikun N, Zhang L, Wang Z, et al. The prevalence of multimorbidity and its association with physical activity and sleep duration in middle aged and elderly adults: a longitudinal analysis from China. Int J Behav Nutr Phys Act. 2021;18(1):77.
Zhang Q, Han X, Zhao X, Wang Y. Multimorbidity patterns and associated factors in older Chinese: results from the China health and retirement longitudinal study. BMC Geriatr. 2022;22(1):470.
Fu Y, Chen M, Si L. Multimorbidity and catastrophic health expenditure among patients with diabetes in China: a nationwide population-based study. BMJ Glob Health. 2022;7(2):e007714.
Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. 2020;8(6):e840–9.
Jing Z, Li J, Fu PP, Wang Y, Yuan Y, Zhao D, et al. Catastrophic health expenditure among single empty-nest elderly with multimorbidity in rural Shandong, China: the effect of co-occurrence of frailty. Int J Equity Health. 2021;20(1):23.
Zhao Y, Zhang P, Oldenburg B, Hall T, Lu S, Haregu TN, et al. The impact of mental and physical multimorbidity on healthcare utilization and health spending in China: a nationwide longitudinal population-based study. Int J Geriatr Psychiatry. 2021;36(4):500–10.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
National Bureau of Statistics of the People’s Republic of China. CHINA STATISTICAL YEARBOOK 2011, 2011. pp 47.
O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. Washington: World Bank Institute; 2008 [cited 2022-11-20]. [World Bank Publications]. Available from: https://openknowledge.worldbank.org/handle/10986/6896.
Chen Z, Yu B, Yang C, Zhou Y, Yao S, Qian X, et al. An extended time-series (2000–2018) of global NPP-VIIRS-like nighttime light data. Volume V3. ed: Harvard Dataverse; 2020.
Zhao Y, Strauss J, Yang G, Hu P, Hu Y, Lei X et al. China Health and Retirement Longitudinal Study: 2011–2012 National Baseline Users’ Guide. 2013. [cited 2022-11-01]. Available from: http://charls.pku.edu.cn/wenjian/jixiandiaochashujuyonghushiyongshouce2013-04-07.pdf.
La DTV, Zhao Y, Arokiasamy P, Atun R, Mercer S, Marthias T, et al. Multimorbidity and out-of-pocket expenditure for medicines in China and India. BMJ Glob Health. 2022;7(11):e007724.
Pathirana TI, Jackson CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. 2018;42(2):186–94.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, Wickramasinghe K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5(3):e277–89.
Yen FS, Lo YR, Hwu CM, Hsu CC. Early-onset type 2 diabetes < 60 years and risk of vascular complications. Diabetes Res Clin Pract. 2021;182:109129.
Kim J, Kim B, Kim DH, Kim Y, Rajaguru V. Association between Socioeconomic Status and Healthcare utilization for children with allergic Diseases: Korean National Health and Nutritional Examination Survey (2015–2019). Healthc (Basel). 2023;11(4):492.
Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61(582):e12–21.
Skinner HG, Coffey R, Jones J, Heslin KC, Moy E. The effects of multiple chronic conditions on hospitalization costs and utilization for ambulatory care sensitive conditions in the United States: a nationally representative cross-sectional study. BMC Health Serv Res. 2016;16:77.
Frølich A, Ghith N, Schiøtz M, Jacobsen R, Stockmarr A. Multimorbidity, healthcare utilization and socioeconomic status: a register-based study in Denmark. PLoS ONE. 2019;14(8):e0214183.
Li H, Huang T, Shen P, Lin H, Guan X, Shi L. Effects of prescription refills use on Healthcare Service utilization and Healthcare cost in hypertensive patients. Chin J Pharmacoepidemiol. 2022;31(7):474–80. (in Chinese).
National Health Commission of PRC. Long-term prescription management standard. 2021. [cited 2023-03-23]. Avaliable form: http://www.gov.cn/zhengce/zhengceku/2021-08/13/content_5631140.htm. (in Chinese)
Zhao Y, Oldenburg B, Mahal A, Lin Y, Tang S, Liu X. Trends and socio-economic disparities in catastrophic health expenditure and health impoverishment in China: 2010 to 2016. Trop Med Int Health. 2020;25(2):236–47.
Njagi P, Arsenijevic J, Groot W. Decomposition of changes in socioeconomic inequalities in catastrophic health expenditure in Kenya. PLoS ONE. 2020;15(12):e0244428.
Ni X, Li Z, Li X, Zhang X, Bai G, Liu Y, et al. Socioeconomic inequalities in cancer incidence and access to health services among children and adolescents in China: a cross-sectional study. Lancet. 2022;400(10357):1020–32.
Wang B, Li Q. Roles of medical assistance in the system of Medical Insurance. Chin Health Econ. 2006;25(1):40–3. (in Chinese).
Jankovic J, Mirkovic M, Jovic-Vranes A, Santric-Milicevic M, Terzic-Supic Z. Association between non-communicable disease multimorbidity and health care utilization in a middle-income country: population-based study. Public Health. 2018;155:35–42.
Marthias T, Anindya K, Ng N, McPake B, Atun R, Arfyanto H, et al. Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: a population-based panel data analysis study. BMJ Open. 2021;11(2):e041870.
Acknowledgements
We appreciate all members in the CHARLS for providing data and training in using the database. We also thank all the interviewers, respondents, and volunteers in the survey. And all authors acknowledge the helpful advice by the editors and reviewers.
Funding
This study was supported by the National Natural Science Foundation of China (grant number 72122001).
The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. Y.W. and J.L. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization, J.L.; Methodology, Y.W., M.D., AND C.Q.; Software, Y.W. AND J.L.; Validation, Q.L. AND W.Y.; Formal Analysis, Y.W.; Writing–Original Draft Preparation, Y.W.; Writing – Review & Editing, Y.W., W.L., J.L. AND M.L.; Visualization, Y.W., and J.L.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The CHARLS was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Biomedical Ethics Review Committee of Peking University (protocol code IRB00001052-11015). And informed consent was obtained from all subjects involved in the CHARLS.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Du, M., Qin, C. et al. Associations among socioeconomic status, multimorbidity of non-communicable diseases, and the risk of household catastrophic health expenditure in China: a population-based cohort study. BMC Health Serv Res 23, 403 (2023). https://doi.org/10.1186/s12913-023-09391-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09391-x