Abstract
Background
Rural residents in the United States face disproportionately poorer health outcomes compared to urban residents. This study aims to establish a continuous rural-urban measure for the 306 hospital referral regions (HRRs) in the U.S. and to investigate the relationship between the proportion of rural population served in each HRR and health outcomes, healthcare spending and utilization, and access to and quality of primary care.
Methods
Cross-sectional analysis using data from The Dartmouth Atlas and the U.S. Census. The sample is limited to fee-for-service Medicare beneficiaries aged 65–99 years and living during 2015. The primary outcomes were measured at the HRR-level: mortality rates, Medicare reimbursements, percent Medicare enrollees who have at least one visit to a primary care physician, diabetic hemoglobin A1c testing rates, and mammography rates. We calculate a population-weighted rural proportion and population-weighted area deprivation index (ADI) for each HRR by aggregating zip-code level data.
Results
The most rural quartile of HRRs had significantly greater mean mortality rate of 4.50%, compared to 3.95% in most urban quartile of HRRs (p < 0.001). Increasing rural proportion was associated with decreasing price-adjusted Medicare reimbursements. In the multivariate, linear regression model, increasing area deprivation (ADI) was associated with increasing rates of mortality and greater utilization.
Conclusion
Disparities in rural mortality are driven by sociodemographic disadvantage, rather than the quality of care provided at hospitals serving rural areas. After accounting for sociodemographic disadvantage, rural areas achieve similar quality of primary care in measured domains at an overall lower cost.
Similar content being viewed by others
Introduction
In the United States, people living in rural areas face disproportionately poorer health outcomes compared to those living in urban areas [1,2,3]. Individuals in rural areas have higher rates of morbidity, mortality, smoking, obesity, and opiate-use disorder compared to their urban counterparts [4]. Differences in socioeconomic and demographic factors such as income, education, employment, race/ethnicity distribution, primary care physician supply, and health insurance status across rural and urban areas have been used to explain the disparity in rural health outcomes [1, 5].
Mortality rates in rural compared with urban areas differ across states, with the highest rural mortality disparities in Virginia, Florida, and California, while Wyoming, Colorado, and Montana have lower mortality rates in rural compared with urban areas [5]. These finding suggest that there are regional factors that impact differences in mortality between rural and urban dwellers. Prior research in rural-urban health disparities have used data at the state, county, or national level, but these units of analysis may not capture where rural populations are receiving healthcare services or account for geographic patterns of healthcare utilization [6]. For example, people within the same state may receive major surgical procedures in their neighboring state or county, or there may be two major centers within one state that provide varying quality of care and serve different populations. Using a geographic-based measure of where individuals are accessing care incorporates the nuances of quality of healthcare received at a given hospital into the analysis of rural-urban disparities and provides a better understanding of drivers of the established variation in rural-urban disparities across regions of the U.S.
Hospital Referral Regions (HRRs) are 306 geographic areas created by the Dartmouth Atlas project to characterize where Medicare recipients are admitted for tertiary care. HRRs provide a more accurate measure of where the population within a certain region access inpatient healthcare services compared to other units of analyses based on county or state boundaries [7]. HRRs have not previously been given a rural-urban designation. This study has two aims: first, to establish a rural-urban measure for the 306 HRRs based on the rural/urban designations of populations they serve, and second, to use the rural-urban HRR measure to analyze health disparities, including an investigation into whether mortality differences are correlated with differences across regions in price-adjusted Medicare reimbursements, as well as quality of and access to primary care. By conducting rural-urban comparisons using HRRs, this study aims to better understand the drivers of previously established rural health disparities and to investigate whether health outcomes in rural areas differ due to population-level characteristics such as income, education, and employment, or the quality of care available to rural populations [7].
Methods
Study population
This study is limited to fee-for-service U.S. Medicare beneficiaries aged 65–99 years. Beneficiaries who die during the study year are excluded.
Hospital Referral Regions
Hospital referral regions (HRRs) represent the healthcare market for a tertiary hospital. To designate HRRs, the Dartmouth Atlas project assigned 5-digit zip codes to smaller units called Hospital Service Areas (HSAs), based on the hospital where the plurality of Medicare beneficiaries who reside within that zip code are hospitalized. The Dartmouth Atlas then aggregates HSAs into larger-area HRRs based on where the Medicare enrollees within that HSA access major cardiovascular procedures or neurosurgery [8]. There are 3,436 HSAs and 306 HRRs in the U.S. Medicare Advantage are only included in mortality outcome measures, and are not included in Medicare reimbursement measures as Medicare Advantage is a Health Maintenance Organization (HMO) and not fee-for-service so cannot be included in the analysis. We used the MABLE-14 crosswalk geographic database to create a custom data set with zip codes, HRR, and total populations of each zip code [9].
Area Deprivation Index
Area deprivation index (ADI) is a measure of socioeconomic disadvantage derived from the American Community Survey assigned as a national ranking from 1 to 100, where 100 is most deprived, based on a cumulative measure of income, education, employment, and housing quality in a given census block-group/neighborhood. We use the national rankings of ADI assigned at the zip code level. Higher national rankings of ADI correspond to greater levels of disadvantage [10].
Outcome variables
Medicare reimbursements, mortality rates, and primary care access and quality data are publicly available from the Dartmouth Atlas Project website [11]. Price-adjusted Medicare reimbursements are a measure of health care utilization, and were calculated from a 20% Medicare sample using diagnostic-related group (DRG) pricing and adjusted based on variation in Medicare reimbursement by region from 2017 [6]. Mortality rates were measured among 2017 Medicare beneficiaries. Primary care access was calculated as a rate with the number of Medicare beneficiaries with at least 1 primary care visit (in 2015) divided by the total number of beneficiaries in the given region from the 20% Medicare sample. Quality of primary care was determined by proportion of diabetic enrollees who receive a hemoglobin A1c test and proportion of eligible women who receive mammograms [12].
Data aggregation
Rural-urban commuting area (RUCA) codes assign a value 1–10 to each zip code (1 representing most urban, 10 most rural) and are determined by measures of population density, urbanization, and daily commuting from the 2010 decennial census data from the United States Department of Agriculture Economic Research Service [13]. We merged the RUCA-zip code, HRR-zip code, and ADI-zip code data sets based on zip code to create a single dataset with an identified HRR, ADI, total population, and RUCA code for each zip code. We collapsed the dataset on HRR, creating a total population residing within each RUCA code in the HRR, the sum total population of the HRR, and a population-weighted measure of ADI equal to the zip code ADI multiplied by the zip code population divided by total population of the HRR.
Calculating rural proportion
For each HRR, we calculated a proportion value for RUCA codes 1–10 based on the proportion of the population of that HRR that lives within each RUCA code. We used the Health Resources Services Administration (HRSA) definition of rural as RUCA codes 4–10 and urban as RUCA codes 1–3 and created a population-weighted measure of rural and urban based on the total population in the rural and urban RUCA code groupings.
Analysis
We examined the linear correlation between rural proportion and ADI using Spearman’s rank correlation coefficient. We then compared unadjusted summary measures of our outcomes in the quartile with the most rural HRRs to the quartile with the most urban (least rural) HRRs, assessing significant differences in groups using a two-sample t-test. We performed univariate and multivariate linear regression analyses to investigate the relationship between rural proportion and our outcomes measures. The data met the assumptions for t-test and multivariable linear regression. The fully-adjusted linear regression model included rural proportion and ADI. We determined significance at the p = 0.05 level. Data was analyzed using Stata version 16.0. (Statacorps, 2017) [14].
Results
Rural proportion measure and area deprivation index
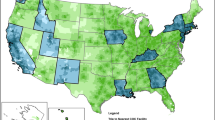
The 306 U.S. HRRs were assigned a measure of proportion rurality ranging from 0 to 1. Figure 1 shows the proportion rurality measure for each HRR represented by color density. The median proportion rurality was 0.207. Population-weighted ADI for each HRR ranges from 12.0 to 81.5, with a median of 57.1. The relationship between rural proportion and ADI is shown in Fig. 2, Spearman’s ρ = 0.49 (p < 0.001).
Proportion of population that is designated as rural within each of the 306 Hospital Referral Regions in the U.S. Figure 1 was created using a Stata program created by Dr. Michael Stepner [26]
Unadjusted results
The most rural quartile HRRs had significantly greater mean population-weighted ADI of 61.7 (95%CI: 59.5, 64.0) compared with 41.6 (95% CI: 37.7, 45.4) in the most urban quartile and the most rural quartile had significantly greater age, sex, race adjusted percent mortality of 4.50% (95%CI: 4.40%, 4.59%) compared to 3.95% (95% CI: 3.84%, 4.06%) in the most urban quartile HRRs. The rural quartile HRRs had lower total and price-adjusted Medicare reimbursements of $9,506 (95%CI: $9,324, $9,969) and $10,049 (95%CI: $9,777, $10,322), respectively, compared to the total and price adjusted Medicare reimbursements in the most urban quartile HRRs of $11,180 (95% CI: $10,895, $11,466) and $10,694 (95% CI: $10,427, $10,962), respectively. In the measures of primary care access and quality, the most rural quartile of HRRs had a greater percentage of Medicare enrollees who have at least one primary care visit, with 80.8% (95% CI: 79.9%, 81.7%) compared to 77.4% (95% CI: 76.2%, 78.6%) for the most urban quartile. The other measures of primary care quality, the percent of diabetic enrollees receiving hemoglobin A1c tests and the percent of eligible female enrollees receiving mammograms, did not differ significantly between the most rural and urban HRRs (Table 1).
Linear regression analysis
In the univariate analysis, increasing rural proportion from entirely urban (rural proportion = 0) to entirely rural (rural proportion = 1) is associated with an increase in 0.70% point (95% CI: 0.49, 0.92) increase in mortality, adjusted for age, sex, and race and an increase in the percentage of eligible Medicare enrollees who receive an annual primary care visit (4.4% points; 95% CI: 2.4%, 6.5%). Increasing ADI was associated with a 0.02% point increase in age, sex, and race adjusted mortality (95% CI: 0.02%, 0.03%) and an increase in percentage of eligible Medicare enrollees who receive an annual primary care visit (0.14%; 95% CI: 0.11%, 0.17%). Rural proportion was negatively associated with price-adjusted Medicare reimbursement (-$970; 95% CI: -$1519, -$422) while ADI was positively associated with price-adjusted Medicare reimbursement ($32.13; 95% CI: $23.92, $40.36). Rural proportion and ADI were not significantly associated with percent of diabetic enrollees who receive hemoglobin A1c test nor percent of eligible female enrollees who receive mammograms (Table 2).
When we included ADI in the multivariate linear regression model (Table 2), the association between rural proportion and mortality became non-significant and ADI had a significant, positive association with increased mortality (0.03%; 95% CI: 0.02%, 0.03%). Both ADI and proportion rurality were significantly associated with price-adjusted Medicare reimbursement, increasing ADI was associated with greater spending ($48.2; 95% CI: $40.0, $56.4) and increasing rural proportion was associated with less spending (-$2273; 95% CI: -$2782, -$1763).
Discussion
Our study demonstrates that HRRs serving more rural populations experience a greater burden of socioeconomic disadvantage. The multivariate regression analysis shows that the one-year mortality rate among Medicare beneficiaries more strongly associated with socioeconomic deprivation within HRRs, rather than the rurality of the region. This suggests the increased mortality in rural areas is mediated by characteristics of the population and area: economic opportunity, education, employment, and housing, rather than the quality of care provided in the region for the HRR or the geographic characteristics that are inherent to rural living.
These findings are consistent with the conclusions of Long et al., 2018, who show that median income and percent in poverty are the primary drivers of disparities in rural mortality, rather than rural status, at the county level [3]. Our analysis adds to this previous work by incorporating where rural populations are receiving their healthcare, and we show that HRRs serving more rural populations have greater burden of sociodemographic deprivation which appears to be driving the adverse health outcomes in these more rural HRRs. Compared to their urban counterparts in 2018, 14.5% fewer rural residents hold bachelor’s degrees; rural individuals make, on average, $7,600 less per year; and there are 7.6% fewer adults in the labor force in rural areas [15, 16]. These data align with our findings of a positive correlation between rurality and ADI which we believe are contributing to disparities in rural mortality.
In Deaths of Despair, Case and Deaton (2020) discuss possible mechanisms by which income, education, and employment drive mortality disparities. They note education is protective against preventable diseases because information about disease prevention is more accessible to those with more education. Individuals age 25 and older with less than a Bachelor’s degree (BA) are four-times as likely to be current smokers and have higher rates of obesity (33% vs. 25%) compared those with a BA or more education [17]. Case and Deaton discuss the rise in “deaths of despair”, which refer to death caused by alcohol, drug-use, and suicide. Rates of deaths of despair are higher among those who are less educated compared to those with a 4-year degree, and in areas with higher rates of unemployment [17].
Additionally, we show that rural proportion is associated with lower overall healthcare utilization as measured by price-adjusted Medicare reimbursements and this relationship is not confounded by the level of sociodemographic disadvantage. This finding could be explained by higher rates of annual primary care visits in rural HRRs which leads to decreased downstream healthcare utilization and decreased overall Medicare spending [18, 19]. Our results suggest that more rural HRRs spend less per Medicare enrollee, and are able to achieve similar outcomes on select measures compared more urban HRRs, as shown by the lack of a significant difference in primary care quality and mortality by rurality when adjusted for ADI. This work contributes to a body of research in geographic variations in healthcare, pioneered by Wennberg and Fisher, that show that Medicare enrollees in higher-spending regions receive more care, but do not have better quality of– or access to– care, health outcomes, and satisfaction, compared to lower spending regions [18,19,20,21].
Further, Chandra and Skinner (2012) show that there are categories of hospital procedures that are costly and yield uncertain clinical value with variable benefits to patient quality of life [22]. These procedures, such as percutaneous coronary intervention (PCI), knee arthroscopy, and aggressive treatment for end-stage cancer, often require expensive infrastructure, technology, and specialized physicians, more commonly found in urban and academic medical centers. Colla et al. (2015) found that HRRs with higher per-capita spending had higher use of low-value services and greater ratios of specialists to primary care providers [23]. Rural clinics and hospitals experience lower patient volume, have fewer specialists, and have fewer expensive medical devices and technologies (such as robotic surgery, proton beam therapy), and are likely utilizing fewer low-value services, which could contribute to decreased spending and utilization in rural areas. One possible explanation for the lower utilization in more rural-serving HRRs with similar healthcare outcomes and quality compared to urban-serving HRRs is the discrepancy in technology and infrastructure between rural and urban hospitals. Further research is needed to investigate rates of expensive procedures, low-value procedures, and utilization patterns in HRRs serving rural vs. urban populations.
This study has several limitations, and the most important aspect is the single-year cross sectional analysis. Second, HRRs accurately localize care for approximately 88% of Medicare beneficiaries based on geographic locations, but that leaves a portion of beneficiaries who reside within HRR boundaries who do not receive their care at the given tertiary care center [24]. Third, we use one definition of rurality based on RUCA codes designated by HRSA. There may be other ways to measure rural populations at the zip code level which could yield different measures for proportion rurality in the areas served by HRRs [25]. Finally, we used ADI as a measure of sociodemographic deprivation, a composite measure of income, education, employment, and housing quality. As such, this analysis is not able to distinguish which factors are the primary drivers of the relationship between ADI and rurality and mortality. Further investigation is needed to see which ADI components are driving the association with rurality in order to impact rural disparities in mortality.
Disparities in rural mortality are driven by sociodemographic disadvantage in rural regions rather than the quality of healthcare available to rural populations. After adjusting for sociodemographic deprivation, we find that HRRs serving rural populations have comparable outcomes and primary care quality with less per capita Medicare spending.
Data availability
The datasets generated during and/or analyzed during the current study are available in the Dartmouth Atlas data repository, https://data.dartmouthatlas.org/.[11]
Abbreviations
- HRR:
-
Hospital referral region
- HSA:
-
hospital service area
- RUCA:
-
rural-urban commuting area
- ADI:
-
area deprivation index
References
Eberhardt MS, Pamuk ER. The Importance of Place of Residence: Examining Health in Rural and Nonrural Areas. Am J Public Health. 2004;94(10):1682–6. doi:https://doi.org/10.2105/AJPH.94.10.1682.
James WL. All Rural Places Are Not Created Equal: Revisiting the Rural Mortality Penalty in the United States. Am J Public Health. 2014;104(11):2122–9. doi:https://doi.org/10.2105/AJPH.2014.301989.
Long AS, Hanlon AL, Pellegrin KL. Socioeconomic variables explain rural disparities in US mortality rates: Implications for rural health research and policy. SSM Popul Health. 2018;6:72–4. doi:https://doi.org/10.1016/j.ssmph.2018.08.009.
National Healthcare Quality. and Disparities Report Chartbook on Rural Health Care.:58.
Gong G, Phillips SG, Hudson C, Curti D, Philips BU. Higher US Rural Mortality Rates Linked To Socioeconomic Status, Physician Shortages, And Lack Of Health Insurance. Health Aff. 2019;38(12):2003–10. doi:https://doi.org/10.1377/hlthaff.2019.00722.
Skinner JS, Gottlieb DJ, Carmichael D, Bronner KK. A New Series of Medicare Expenditure Measures by Hospital Referral Region: 2003–2008.:8.
Baicker K, Chandra A, Skinner J. Geographic Variation in Health Care and the Problem of Measuring Racial Disparities. Perspect Biol Med. 2005;48(1):42–53. doi:https://doi.org/10.1353/pbm.2005.0020.
FAQ. Dartmouth Atlas of Health Care. Accessed October 15. 2020. https://www.dartmouthatlas.org/faq/.
Geocorr 2014 - MCDC. Accessed November 20. 2020. https://mcdc.missouri.edu/applications/geocorr2014.html.
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible — The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–8. doi:https://doi.org/10.1056/NEJMp1802313.
Dartmouth Atlas DATA. Accessed May 20. 2021. https://data.dartmouthatlas.org/.
Goodman DC, Brownlee S, Chang CH, Fisher ES. Regional and Racial Variation in Primary Care and the Quality of Care among Medicare Beneficiaries. The Dartmouth Institute for Health Policy & Clinical Practice;:36.
USDA ERS - Rural-Urban Commuting Area Codes. Accessed October 30. 2020. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.
StataCorp. Stata Statistical Software: Release 15. College Station. TX: StataCorp LLC; 2017.
USDA ERS - Rural Education. Accessed April 17. 2021. https://www.ers.usda.gov/topics/rural-economy-population/employment-education/rural-education/.
USDA ERS - Rural Employment and Unemployment. Accessed April 17. 2021. https://www.ers.usda.gov/topics/rural-economy-population/employment-education/rural-employment-and-unemployment/.
Case A, Deaton A. Deaths of Dispair and the Future of Capitalism. Princeton University Press; 2020.
Mark DH, Gottlieb MS, Zellner BB, Chetty VK, Midtling JE. Medicare costs in urban areas and the supply of primary care physicians. J Fam Pract. 1996;43(1):33–9.
Baicker K, Chandra A. Medicare, Spending. The Physician Workforce, And Beneficiaries’ Quality Of Care. Health Aff. 2004;23(Suppl1):W4–184. doi:https://doi.org/10.1377/hlthaff.W4.184.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder ÉL. The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care. Ann Intern Med. 2003;138(4):273–87. doi:https://doi.org/10.7326/0003-4819-138-4-200302180-00006.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder ÉL. The Implications of Regional Variations in Medicare Spending. Part 2: Health Outcomes and Satisfaction with Care. Ann Intern Med. 2003;138(4):288–98. doi:https://doi.org/10.7326/0003-4819-138-4-200302180-00007.
Chandra A, Skinner J. Technology Growth and Expenditure Growth in Health Care. J Econ Lit. 2012;50(3):645–80. doi:https://doi.org/10.1257/jel.50.3.645.
Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing wisely: prevalence and correlates of low-value health care services in the United States. J Gen Intern Med. 2015;30(2):221–8. doi:https://doi.org/10.1007/s11606-014-3070-z.
Kilaru AS, Wiebe DJ, Karp DN, Love J, Kallan MJ, Carr BG. Do Hospital Service Areas and Hospital Referral Regions Define Discrete Health Care Populations? Med Care. 2015;53(6):510–6. doi:https://doi.org/10.1097/MLR.0000000000000356.
Onega T, Weiss JE, Alford-Teaster J, Goodrich M, Eliassen MS, Kim SJ. Concordance of Rural-Urban Self-identity and ZIP Code-Derived Rural-Urban Commuting Area (RUCA) Designation. J Rural Health. 2020;36(2):274–80. doi:https://doi.org/10.1111/jrh.12364.
maptile: Geography templates. Accessed February 4. 2021. https://michaelstepner.com/maptile/geographies/.
Acknowledgements
The Dartmouth Institute for Health Policy and Clinical Practice MPH students and faculty who supported this project.
Funding
This work was supported by the National Institutes of Health (NCI R01 CA248470-01).
Author information
Authors and Affiliations
Contributions
LS analyzed and interpreted data and drafted the manuscript. SW provided contributions to analytical design, interpretation of data, and revised the manuscript. CC provided contributions to analytical design, interpretation of data, and revised the manuscript. All authors approved the submitted version and have agreed to be accountable for their contributions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. This paper has not been subject to CBO’s regular review and editing process. The views expressed here should not be interpreted as CBO’s.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Skinner, L., Wong, S. & Colla, C. Rethinking rurality: using hospital referral regions to investigate rural-urban health outcomes. BMC Health Serv Res 22, 1312 (2022). https://doi.org/10.1186/s12913-022-08649-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08649-0