Abstract
Background
Health service areas are essential for planning, policy and managing public health interventions. In this study, we delineate health service areas from routinely collected health data as a robust geographic basis for presenting access to maternal care indicators.
Methods
A zone design algorithm was adapted to delineate health service areas through a cross-sectional, ecological study design. Health sub-districts were merged into health service areas such that patient flows across boundaries were minimised. Delineated zones and existing administrative boundaries were used to provide estimates of access to maternal health services. We analysed secondary data comprising routinely collected health records from 32,921 women attending 27 hospitals to give birth, spatial demographic data, a service provision assessment on the quality of maternal healthcare and health sub-district boundaries from Eastern Region, Ghana.
Results
Clear patterns of cross border movement to give birth emerged from the analysis, but more women originated closer to the hospitals. After merging the 250 sub-districts in 33 districts, 11 health service areas were created. The minimum percent of internal flows of women giving birth within any health service area was 97.4%. Because the newly delineated boundaries are more “natural” and sensitive to observed flow patterns, when we calculated areal indicator estimates, they showed a marked improvement over the existing administrative boundaries, with the inclusion of a hospital in every health service area.
Conclusion
Health planning can be improved by using routine health data to delineate natural catchment health districts. In addition, data-driven geographic boundaries derived from public health events will improve areal health indicator estimates, planning and interventions.
Similar content being viewed by others
Background
Demarcating geographic areas from patient travel is essential for health policy, planning, and research [1]. Health service managers use spatial tools to plan health services, identify gaps in service provision, prioritise areas with poor access, measure service coverage and allocate resources [2]. In some countries, such as Uganda and Ghana, district league tables based on these boundaries have formed the basis for health systems performance assessment [3, 4]. Health catchments can be natural, reflecting patient choice, or mandated, reflecting regulation of health service delivery [5]. For instance, general practices follow mandated catchments in the UK because patients must live within practice boundaries [6]. However, some countries, including Ghana, have natural catchments because patients can use any health facility. While supply is fixed within a district, significant flows of cross-border service users can change the demand for services [7] and affect management priorities and planning needs. Identifying catchments is vital for measuring coverage, access, improving quality and planning [8,9,10]. Therefore, zone design approaches can help by sub-dividing large regions or merging small areas into health service areas, or even changing boundaries altogether.
A health service area (HSA) is a geographic unit where most of the trips to use routine health services start and end internally within that geographic unit, making it relatively self-contained [11]. HSAs improve quality of care and provide insights into service utilisation patterns and access to care by supporting areal health indicator reports [8,9,10, 12, 13]. Additionally, health service area demarcations can be used for health systems programming. However, planning health services within district boundaries can be problematic, particularly in districts with overutilised hospitals or without secondary care facilities.
The Travel-To-Work-Area algorithm (TTWA) is one of the approaches for delineating zones [14]. The TTWA has been used to delineate labour market [14], retail [15] and health service areas [16, 17]. It was applied to admissions to develop health service areas [17] and general practice affiliations data for local health planning purposes [16]. The TTWA is useful for zone design because it creates non-overlapping zones by maximising internal flows and minimising flows between zones.
For birthing services, reaching health facilities promptly in times of need and emergency is crucial for promoting women’s health, and preventing maternal mortality and disability [18]. Furthermore, a functioning referral system includes effective communication between service providers to guarantee timely quality care [19]. Inadequate coordination and communication between health facilities during referrals can lead to adverse outcomes for women and their babies [20, 21]. Health professionals within a hospital network need knowledge of the nearest available quality secondary care to prepare for life-saving emergencies adequately. Information on available resources can be shared between collaborating health facilities within a HSA.
Access to maternal health service indicators can be calculated using HSA demarcations [9]. For instance, the World Health Organisation (WHO) recommends five (four basic and one comprehensive) emergency obstetric care facilities per half a million population within a geographical area [22]. In terms of staff based at these crucial health facilities, at least 22.8 skilled health workers (midwives, nurses, doctors) per 10,000 population threshold are recommended. This benchmark has more recently been revised upwards to 33.45 skilled health workers per 10,000 population [23]. A set of key suggested indicators measuring performance against staffing benchmarks, facility benchmarks, health outcome measures, and quality markers can be estimated using the HSA and administrative boundaries. Therefore, geographic boundaries play a fundamental role in robust reporting of areal statistics to improve maternal health quality.
The problem with using government administrative boundaries to measure health indicators such as the physician-to-population ratio is the magnitude of cross-district use of health services [9]. In Ghana, health planning and other public health management activities are limited to government administrative boundaries. However, service use goes across district boundaries as clients move from one district to another for services [24]. Therefore, midwife-to-population ratios and other maternal health access indicators could misrepresent the demand for services.
Almost all studies delineating HSAs using admissions data are in high-income countries [8, 9, 13, 25]. Meanwhile, the increasing availability of individual-level routine health data in low-income settings with electronic health systems can aid such studies [26]. Although some studies have estimated catchment areas around individual health facilities for malaria and other infectious diseases, these statistical methods are not optimised for zoning HSAs because the catchments are drawn around individual health facilities [27,28,29]. Also, they focus on travel times and care-seeking behaviour rather than developing HSAs for reporting health service performance indicators. However, evidence from high-income countries suggests that contiguous zones formed by grouping health facilities using patient flows are well suited for healthcare planning [25]. Despite the advantages of this approach, no existing studies demarcated HSAs in low and middle income countries (LMIC) using patient flows. A study in Ghana divided one district into sub-districts with network analysis [30].
This study aims to delineate HSAs using routine birth admission data. Also, the study examines to what extent the TTWA method can be adapted to design zones using patient flows to secondary health care facilities. In doing so, we merge highly connected health facility zones to form HSAs. Subsequently, the creation of HSAs allows this study to estimate maternal health indicators for planning and to improve maternal health services within the study area.
Methods
Data
Data documenting births of 32,921 women from 27 hospitals in the Eastern region, Ghana, from 1st January to 31st December 2017 were used to analyse women’s travel to give birth. The Ghana Health Service (GHS) collects birth data using book registers. Midwives record details of a woman into these registers when they give birth in a health facility. Information collected includes the woman’s residential address, age, parity, complications, birth outcomes and other relevant maternal health information.
Subsequently, the data is entered into the electronic District Health Information Management System (DHIMS). First, the women are counted and reported as monthly aggregates. Secondly, the individual records as they appear in the register are also captured in the DHIMS system. Currently, only hospitals enter the individual women’s data into the DHIMS, as health centres use paper registers only. The individual records transferred from paper to electronic registers at hospitals can differ from routine aggregate reports. The two key variables used in this analysis are the woman’s community of residence and the health facility she gave birth in.
District and sub-district boundaries from the GHS were included in the analysis. In the GHS, sub-districts are the lowest administrative areal unit and are formed by a group of health facilities and communities. We used WorldPop gridded (100 m by 100 m) estimated population, the number of midwives in health facilities, and the spatial distribution of the hospitals to estimate access to adequately staffed birthing services. The WorldPop group produces the population estimates by disaggregating census data into 100 square meter grids within built settlements using Random Forest machine learning methods [31].
In order to construct indicators that provide a good measure of human resource availability and quality of care, data were collected for this study in September 2021. An emergency obstetric and newborn care (EmONC) service provision assessment survey (SPA) was conducted. The survey data was used to determine if hospitals provided care to the level of Comprehensive Emergency Obstetric and Newborn Care (CEmONC). A hospital is classified as CEmONC ready if they administered parenteral antibiotics, uterotonics, parenteral anticonvulsants, removed placenta manually, removed retained products, performed assisted vaginal delivery, neonatal resuscitation, caesarean section and blood transfusion in the last 3 months [22]. CEmONC designated health facilities are supposed to be ready for all major obstetric complications, including the need for surgery and blood transfusion.
Birthing mobility patterns
We used a list of place names with geographic coordinates from the GHS to locate the residential towns of the women. However, we could not find some addresses due to spelling errors, unavailable town names or address mismatches. The town names were manually matched with the reference list as automated geocoding performs poorly because official standardised address lists are unavailable in Ghana [32]. The geographic locations of the hospitals were collected during the SPA.
The flows of women initially captured between residential communities and hospitals were aggregated to sub-districts. The aggregation was carried out for two reasons: to reduce the complexity of flows and, secondly, to be consistent with the geographic unit used for delineating HSAs in subsequent analysis. For mappings, only flows of six or more women between sub-districts were shown to avoid graphical complexity [33].
Zoning health service areas
The TTWA zoning method used in this study is a criteria-based zoning process originally used to delineate labour market [14] and retail [15] areas from flow data. The TTWA was used to analyse labour markets delineated to have the majority of people living and working within the zones generated. Similarly, this study utilises it to create health service areas where people live and use birthing services in an area. The building block for our zoning analysis is sub-districts, which were merged into larger areal units. Sub-districts without any facilities reporting births were first merged to a nearby one within the same district. Figure 1 shows the steps involved in developing the HSAs, implemented via Visual Basic within a Microsoft Access database.
The women were first assigned to the hospital they used. Where women in a subdistrict used more than one hospital, they were assigned to the hospital that received the most flows from that subdistrict to form the first set of zones. Then, the self-containment or localisation index was calculated (Step 1) to determine which zone will be merged in the next step. Next, demand and supply-side self-containment are calculated from patient flows (Step 2). Demand-side self-containment is calculated as the number of internal flows starting and ending within a zone as a proportion of all flows ending in the zone. In contrast, supply-side self-containment comprises internal flows as a proportion of all flows originating in a zone. The zone with the minimum demand or supply-side self-containment is the candidate for merging.
The next step (Step 3) calculates the connectance (connectivity strength) between zones [15] to identify the zone with the highest connectance (Step 4). The connectance flows are calculated between the zone with the lowest self-containment in step two and all other zones. In Step 5, we merged the least self-contained zone in Step 2 with the best connected in Step 4. This analysis used the connectance flow function (Eq. 1) by Pratt and colleagues [15] derived from Coombes [34]:
Where Cij is the connectance flows between zone i and zone j.
Tij are the flows from zone i to zone j.
Tji are the opposite from zone j to zone i.
The sum of flows at the origin ∑iTij contains internal flows from i to i.
The sum of flows at the destination ∑jTij contains internal flows from j to j.
The sum of reverse flows at the origin ∑iTji contains internal flows from i to i.
The sum of reverse flows at the destination ∑jTji includes internal flows from j to j.
Steps one to five are repeated until a minimum self-containment criterion is met. Zones were only progressively merged. They were not dissolved as implemented in the original TTWA process.
The minimum supply/demand self-containment threshold for all zones to qualify as an HSA was set at 96%. The self-containment was high because the initial self-containment was high (70.5%), and a high value optimises health services planning by limiting cross border patient movement in the output zones.
The final step used manual interventions to make all zones contiguous. There were instances where most of the women in a sub-district attended the regional hospital or a hospital farther away, resulting in an outlier island zone. These inconsistent zones were corrected by assigning them to the nearby zone with the highest contiguity to ensure homogeneity.
Henceforth, the study introduces new terminology and refers to HSAs as Natural Catchment Health Districts (NCHD) as it differentiates them from HSAs delineated from mandatory catchments. NCHD and Zones are used interchangeably.
A simpler comparable set of zones were delineated to assess the effect of scale on self-containment. The flows were assigned to the destinations where most women went to give birth from a sub-district. The zone with the smallest supply-side self-containment was a candidate for merging. The candidate zone was merged to the contiguous zone with the least supply-side self-containment. The process was repeated until a comparable number of zones was achieved.
Health planning indicators
Geographic access indicators were calculated using municipal and district assembly boundaries (MDA) and NCHD. MDAs are the government geographical boundaries for local governance. Two indicators of access to birthing services were calculated for each geographic boundary using the 2021 service provision assessment survey and gridded population data:
-
1.
The number of CEmONC hospitals per 100,000 population
-
2.
The number of midwives per 10,000 population
Although the most appropriate indicators of geographic access are travel time to health facilities [5], the analysis used a provider to population ratio. Provider to population ratio is suitable because it is the primary indicator health managers use, simple to calculate and a recommended benchmark by the WHO [23, 35].
Results
Women’s journeys to give birth in secondary care facilities
There were 32,921 (80.6%) individual birth records of the 40,856 aggregated counts in the DHIMS database (Fig. 2). Geographic coordinates of the residential communities were successfully identified for 30,838 (93.7%) of women with individual records. However, there was no substantial variation in the proportion of records by facility ownership (government, private, faith-based) and availability of geographic coordinates. The 30,838 women analysed came from 1015 residential communities in 250 sub-districts and gave birth in 27 hospitals. The number of women making journeys from a residential community to a hospital pair ranged from one to 1726.
On average, there were less than 30 births per residential community in 2017 and a median of 7 births [Inter Quartile Range IQR = 20, (2 to 22)], but this skewed distribution has a few communities with many more births. The total births at the top 50 residential communities ranged from 115 to 2002. Private and faith-based hospitals saw fewer women than public hospitals (Fig. 3A). Inter-regional users from the Greater Accra area (women who crossed regional boundaries from the national capital city) represented more than one quarter (26%) of women from the top 10 residential communities. The agreement between aggregated and individual reports are compared in Fig. 3B. There was a 97.1% correlation between the aggregated and individual reports in DHIMS. Non-reporting hospitals were mainly private.
A The number of women giving birth by hospitals in Eastern Region, Ghana, 2017, based on individual-level birth register records. B Individual versus aggregate records reported in DHIMS in Eastern Region, Ghana, 2017; the red line shows expected 100% correlation between the individual and aggregated data
Women moved between and within MDAs to give birth (Fig. 4). The number of women travelling to give birth decreased with increasing distance to hospitals as larger flows lived closer to the hospitals. Afram plains areas, surrounded by the lake, had a highly localised movement pattern. Women from the Central, Volta and Greater Accra regions used nearby hospitals in the Eastern Region. However, the most substantial inter-regional flows were women from Greater Accra, primarily using Nsawam hospital. Almost half [2894 (48%)] of the women giving birth at Nsawam hospital were from Accra.
Delineation of natural catchment health districts
Based on the women’s flow patterns and connectivity between the hospitals, 11 natural catchment health districts (NCHD) emerged from the 250 sub-districts (Fig. 5A). The zones vary from 473 km2 (zone 7) to 4669 km2 (zone 6). The Afram plains area (zone 6), surrounded by Lake Volta, was highly self-contained without connecting to other zones through all iterations. Each NCHD covered at least two or more districts. There were an average of six administrative districts in each NCHD. The only district split between three zones (Ayensuano) does not have a hospital. The final self-containment was high, with 97.4% to 99.% of journeys starting and ending within the output zones (Fig. 5B). The merging of zones in each iteration increased the self-containment. Similarly, the difference between the internal flows for all output zones and each output zone decreased anytime zones were merged. The self-containment for the comparable zones (Fig. 6) ranged from 71 to 100% for each output zone and 91% altogether.
Access to birthing service indicators by MDA versus NCHD
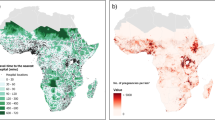
Figure 7 shows the geographical distribution of hospitals providing CEmONC services and the midwife-population ratio. Of the 33 MDA areas in the Eastern region, 12 (36%) did not have a hospital, and 10 districts (30%) had hospitals that were not ready to provide CEmONC (Fig. 7A). Most of the remaining 11 districts either had one or two CEmONC hospitals per 100,000 population. When zoned, all NCHDs had hospitals, but two were without CEmONC (Fig. 7B).
There were marginal variations between the number of hospitals and midwives attending to pregnancies across the region. Although there was only one public hospital in some districts (e.g. Nkawkaw), the number of midwives was high (Fig. 7C). There were two or more hospitals in two districts. There were an average of five and 15 midwives per 10,000 population in MDA and NCHD, respectively. Only one district and three NCHDs meet the 22.8 per 10,000 population WHO threshold.
Discussion
This study presents the first analysis delineating NCHD using birth data from routine health records. Likewise, it provides the first insights into delineating NCHDs from flow data in Ghana and any LMIC setting. The study merged catchments of 27 hospitals in 33 administrative districts to 11 zones using birthing records. The minimum proportion of internal flows of women giving birth within these zones was 97.4%. Accra’s interregional flows to the Eastern region were prominent in all districts sharing a border with Accra, especially Nsawam. This study introduced a new term, NCHD, specific to health service areas or zones delineated from natural flow patterns.
Implications for maternal health planning and policy
In Ghana and many other LMICs, district boundaries are used across all government sectors such as agriculture, education, and local government. While this MDA structure harmonises boundaries for all government sectors and fosters cross-sectoral cohesion at the district level, they are not optimised for any particular government sector. Indeed, population size and political considerations have played the most part in shaping district boundaries [36]. There are mismatches between the MDAs and the distributions of hospitals because not every MDA boundary contains a district hospital. There are similarly no hospitals within some second-level administrative boundaries elsewhere in Ghana and Sub-Saharan Africa [37]. Furthermore, since the MDAs are not designed to capture a group of health facilities and the population attending those facilities, they are problematic as a basis for areal health indicators.
The NCHDs address the mismatched distribution of hospitals versus MDAs. First, the NCHDs impact the calculation of indicators and positively address mismatch challenges associated with MDAs by providing a more robust basis for calculating indicators. The high self-containment in NCHDs ensures that areal health indicators reflect the attending population. Likewise, indicators such as mortality rates, caesarean sections, skilled birth rates and other estimates are reasonable because every NCHD has a hospital. The results reveal NCHDs with inadequate human resources and poor emergency obstetric care. When these quality care and human resource challenges are addressed, they could improve the skilled birth coverage in Ghana [38, 39].
Topography likely influences movement patterns and NCHDs. For instance, the Afram plains area surrounded by the Volta lake had no connectivity with other districts, as did the mountainous Akwapim North with its unsurfaced roads in some communities, forming one zone. The influence of topography on access to care should be considered when upgrading hospitals or improving the quality of maternal health. If service quality in these hospitals is inadequate, women would struggle to access alternative, higher quality hospitals. They might give birth at home since poor roads and the inability to cross rivers are risk factors for home births in rural Ghana [40].
The NCHD zones may be helpful in the organisation of health professional teams. High connectance values are likely to reflect patient choice and referral patterns. For example, hospitals within the same NCHD are likely to be referring women between neighbouring hospitals in emergency cases. Maternal health quality improvement projects based on collaborating health teams increased skilled birth uptake in Ghana [41]. Thus, if health professionals were geographically grouped into teams within the zones, this might further improve referrals and promote continuity of care. A new GHS “network of practice” initiative could also benefit from our zoning approach to group health facilities [42]. The initiative aims to group health facilities to collaborate, share resources, improve referrals, and provide technical and operational support.
Implementing the NCHDs could be challenging considering resource allocation structures and the political landscape. In Ghana, financial, human, material and other resources are mainly allocated to regions and districts [43]. Thus, funding NCHDs could be problematic as they are not part of the administrative and governance structures of the GHS. However, this could be addressed by organising capacity building via the NCHD clusters and developing resource sharing mechanisms among districts within NCHDs. Furthermore, local government authorities might not support NCHD-driven programming as it does not align with electoral boundaries where they campaign for votes.
Methodological implications for zone design and limitations
The low number of flows between many origin-destination pairs, the large number of residential communities and few hospitals affected the converging of the automated TTWA approach. The automating challenge shows that zoning applications can be contextual depending on the setting, data source and service that generated the data. Haynes and colleagues [8] observed that zone design can be challenging for rare diseases that generate no or fewer data from some parts of the study area. Whilst births are not rare, few women gave birth in many parts of the study area. Hence, the nature of our data may explain difficulties applying an existing automated tool [15].
Whilst findings are specific to attendance for childbirth, the methods in this study could be applied to other health events with patient residential and hospital addresses. Levels of self-containment for birth attendance might be similar to other events as residents are likely to use the secondary level hospitals in their NCHD rather than cross over to others. In Ghana, when seeking non-emergency care that is available at primary facilities for scabies, patients travel to hospitals in a pattern broadly comparable with the flows in Fig. 4 [44]. Thus, the NCHD zones based on hospital use patterns are likely to remain highly self-contained in the presence of shorter trips to primary health centres.
Aggregating flows from small areas into larger areas typically increases self-containment, the number of journeys starting and ending within a zone. Thus greater self-containment would be expected for flows based on NCHDs relative to MDAs, given that the former are larger zones. However, since NCHDs had greater self-containment than similar zones of comparable size, this suggests the TTWA algorithm effectively delineated groups of facilities and the populations they serve (Fig. 6).
There were manual interventions used here to make zones contiguous. Alternative methods overcome this shortfall by enforcing spatial contiguity in automated approaches [8]. Relative to aggregate data, individual data were incomplete in some hospitals. However, the correlation between aggregated and individual data has improved compared with a previous study from the same area [24]. The impact of private health facilities on the NCHD is likely to be low because there is no district served by private facilities only; birthing services are free in public facilities; and only 6% of women gave birth in private health facilities in the Eastern region [45]. Journeys to primary care facilities were not included in this study. However, they are likely to be shorter and highly localised. Therefore, primary care flows are unlikely to affect the NCHDs substantially. Future studies could use data from different years to improve record completeness and include private facilities. Since we did not incorporate attendance by Eastern region residents in neighbouring regions’ facilities, this study did not account for edge effects, the tendency for cross-boundary healthcare access to impact geographical accessibility measures [46]. A nationwide analysis could resolve or minimise the edge effect resulting from inter-regional movement.
Transferability and future research
NCHDs could be regularly updated as movement patterns evolve, since the routine health data is continuously available to health managers. The open-source District Health Information Systems (DHIS) for routine health data management is widely implemented in many LMICs, especially across Africa [26]. The widespread DHIS presents the opportunity to scale up or replicate this study in other countries. However, the mix of public, private and faith-based healthcare providers varies across African countries [47] and private health facility integration within DHIS reporting is limited in some countries [48]. Thus, health system fragmentation in some countries, national health insurance systems influencing choice of facility, and country-specific data availability constraints could limit the replication ot this study elsewhere in Africa.
Subsequent studies should analyse routine data for other health outcomes. Our analysis shows how routine health data collected electronically via health information systems can be used for monitoring local service delivery progress [49], strengthening the case for investment in such systems [50]. Subsequent studies could also explore how the use of boundaries designed from patient flows affects health systems performance assessment systems. National systems such as Uganda’s district league table have been criticised as lacking a robust statistical basis [3], and similar methods are used in Ghana [4]. The use of more appropriate boundaries could address some of these criticisms [51]. Pregnancy and childbirth-related risk perceptions influence choice of place for antenatal care, obstetric emergencies and normal birth in Ghana [52]. Also, service availability will drive patterns as nearby primary facilities treating fevers or diarrhoea might not provide birthing services, but bypassing could be prevalent even for non-emergency cases such as scabies [44]. Therefore, the variations in patient travel for different services should be investigated in future studies as patterns for in/outpatient, emergencies/non-emergencies, communicable/non-communicable diseases, and other public health events are likely to differ, forming different zones.
Conclusions
This study presents the first insights into applying zone design methods to maternal health birthing services using routine health data. The resultant NCHD zones were used to measure access to maternal health care. By design, most trips for birthing services start and end within NCHD, making the population denominators more stable. The TTWA algorithm had to be tailored to the available data mainly due to the number of health facilities and frequency of trips in the study area, compared with high-income country settings where the algorithm was previously used. Notwithstanding, the methodology has potential for scale-up nationally and elsewhere in Sub-Saharan Africa, particularly as investments in routine health systems continue and increasing availability of individual transactional data captured through the DHIS or other electronic health systems. This study is highly relevant to strategies by the GHS to develop health service areas.
Availability of data and materials
The demographic dataset analysed during the current study is openly available in the WoldPop repository, https://www.worldpop.org/
The service provision assessment dataset analysed during the current study are available from the correspondent author on reasonable requst.
The birth datasets analysed during the current study are not publicly available due to confidentiality and data licencing restrictions from the Ghana Health Service. They can be obtained from the Ghana Health Service (https://www.ghs.gov.gh/contact-us) with reasonable request.
Abbreviations
- HAS:
-
Health service area
- TTWA:
-
Travel to work areas
- WHO:
-
World Health Organisation
- LMIC:
-
Low and middle income countries
- GHS:
-
Ghana Health Service
- DHIMS:
-
District Health information Management Systems
- SPA:
-
Service provision assessment
- NCHD:
-
Natural catchment health district
- MDA:
-
Municipal and district assembly
- DHIS:
-
District Health Information Systems
References
Kilaru AS, Wiebe DJ, Karp DN, Love J, Kallan MJ, Carr BG. Do Hospital service areas and hospital referral regions define discrete health care populations? Med Care. 2015;53(6):510–6.
Robin TA, Khan MA, Kabir N, Rahaman ST, Karim A, Mannan II, et al. Using spatial analysis and GIS to improve planning and resource allocation in a rural district of Bangladesh. BMJ Glob Health. 2019;4(Suppl 5):e000832.
KirungaTashobya C, Ssengooba F, Nabyonga-Orem J, Bataringaya J, Macq J, Marchal B, et al. A critique of the Uganda district league table using a normative health system performance assessment framework. BMC Health Serv Res. 2018;18(1):355.
NDPC, UNICEF. 2020 District league table: Generating evidence for addressing unequal access to services and development opportunities for children. 2020.
Cromley EK, McLafferty SL. GIS and public health. New York: Guilford Press; 2011.
NHS. Registering with a GP surgery outside the area you live 2018. Available from: https://www.nhs.uk/nhs-services/gps/registering-with-a-gp-outside-your-area/. [updated 28-11-2018].
Putri NK, Wulandari RD, Syahansyah RJ, Grépin KA. Determinants of out-of-district health facility bypassing in East Java, Indonesia. Int Health. 2021;13:545–54.
Haynes AG, Wertli MM, Aujesky D. Automated delineation of hospital service areas as a new tool for health care planning. Health Serv Res. 2020;55(3):469–75.
Makuc DM, Haglund B, Ingram DD, Kleinman JC, Feldman JJ. The use of health service areas for measuring provider availability. J Rural Health. 1991;7:347–56.
Schroeck FR, Kaufman SR, Jacobs BL, Skolarus TA, Hollingsworth JM, Shahinian VB, et al. Regional variation in quality of prostate cancer care. J Urol. 2014;191(4):957–63.
Makuc DM, et al. Health service areas for the United States National Center for Health Statistics. Vital Health Stat. 1991;112(2).
Bullen N, Moon G, Jones K. Defining localities for health planning: a GIS approach. Soc Sci Med. 1996;42(6):801–16.
Widmer M, Matter P, Staub L, Schoeni-Affolter F, Busato A. Regional variation in orthopedic surgery in Switzerland. Health Place. 2009;15(3):791–8.
Coombes MG, Green AE, Openshaw S. An efficient algorithm to generate official statistical reporting areas: the case of the 1984 travel-to-work areas revision in Britain. J Oper Res Soc. 1986;37(10):943–53.
Pratt MD, Wright JA, Cockings S, Sterland I. Delineating retail conurbations: a rules-based algorithmic approach. J Retail Consum Serv. 2014;21(5):667–75.
Shortt NK, Moore A, Coombes M, Wymer C. Defining regions for locality health care planning: a multidimensional approach. Soc Sci Med. 2005;60(12):2715–27.
Jia P. Developing a flow-based spatial algorithm to delineate hospital service areas. Appl Geogr. 2016;75:137–43.
Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9(1):34.
WHO. Standards for improving quality of maternal and newborn care in health facilities. 2016.
Afari H, Hirschhorn LR, Michaelis A, Barker P, Sodzi-Tettey S. Quality improvement in emergency obstetric referrals: qualitative study of provider perspectives in Assin north district, Ghana. BMJ Open. 2014;4(5):e005052.
Harahap NC, Handayani PW, Hidayanto AN. Barriers and technologies of maternal and neonatal referral system in developing countries: a narrative review. Inform Med Unlocked. 2019;15:100–84.
Bailey P, Lobis S, Maine D, Fortney JA. Monitoring emergency obstetric care: a handbook. Geneva: World Health Organization; 2009.
WHO. A universal truth: no health without a workforce. Geneva: World Health Organisation (WHO) Report; 2013. p. 1–104.
Dotse-Gborgbortsi W, Dwomoh D, Alegana V, Hill A, Tatem AJ, Wright J. The influence of distance and quality on utilisation of birthing services at health facilities in eastern region, Ghana. BMJ Glob Health. 2020;4(Suppl 5):e002020.
Klauss G, Staub L, Widmer M, Busato A. Hospital service areas–a new tool for health care planning in Switzerland. BMC Health Serv Res. 2005;5(1):1–15.
University of Oslo. DHIS in action 2021. Available from: https://dhis2.org/in-action/.
Alegana VA, Khazenzi C, Akech SO, Snow RW. Estimating hospital catchments from in-patient admission records: a spatial statistical approach applied to malaria. Sci Rep. 2020;10(1):1–11.
Alegana VA, Wright JA, Pentrina U, Noor AM, Snow RW, Atkinson PM. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int J Health Geogr. 2012;11(1):6.
Zinszer K, Charland K, Kigozi R, Dorsey G, Kamya MR, Buckeridge DL. Determining health-care facility catchment areas in Uganda using data on malaria-related visits. Bull World Health Organ. 2014;92:178–86.
Kofie RY, Møller-Jensen L. Towards a framework for delineating sub-districts for primary health care administration in rural Ghana: a case study using GIS. Nor Geogr Tidsskr. 2001;55(1):26–33.
Bondarenko M, Kerr D, Sorichetta A, Tatem A. Census/projection-disaggregated gridded population datasets for 51 countries across sub-Saharan Africa in 2020 using building footprints. 2020.
Dotse-Gborgbortsi W, Wardrop N, Adewole A, Thomas MLH, Wright J. A cross-sectional ecological analysis of international and sub-national health inequalities in commercial geospatial resource availability. Int J Health Geogr. 2018;17(1):14.
Rae A. Flow-data analysis with geographical information systems: a visual approach. Environ and Plan B Plan Design. 2011;38(5):776–94.
Coombes M, Ons. 1991-based travel-to-work areas. London: ONS London; 1998.
WHO. The global health observatory, explore a world of data; Density of midwives 2021. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3112.
Resnick D. Democracy, decentralization, and district proliferation: the case of Ghana. Polit Geogr. 2017;59:47–60.
Wigley AS, Tejedor-Garavito N, Alegana V, Carioli A, Ruktanonchai CW, Pezzulo C, et al. Measuring the availability and geographical accessibility of maternal health services across sub-Saharan Africa. BMC Med. 2020;18(1):237.
Dotse-Gborgbortsi W, Tatem AJ, Alegana V, Utazi CE, Ruktanonchai CW, Wright J. Spatial inequalities in skilled attendance at birth in Ghana: a multilevel analysis integrating health facility databases with household survey data. Tropical Med Int Health. 2020;25(9):1044–54.
Nesbitt RC, Lohela TJ, Soremekun S, Vesel L, Manu A, Okyere E, et al. The influence of distance and quality of care on place of delivery in rural Ghana. Sci Rep. 2016;6:30291.
Adatara P, Strumpher J, Ricks E. Exploring the reasons why women prefer to give birth at home in rural northern Ghana: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):500.
Singh K, Brodish P, Speizer I, Barker P, Amenga-Etego I, Dasoberi I, et al. Can a quality improvement project impact maternal and child health outcomes at scale in northern Ghana? Health Res Policy Syst. 2016;14(1):45.
Ministry of Health. Ghana health sector 2021 programme of work. 2021.
Ensor T, Dakpallah G, Osei D. Geographic resource allocation in the health sector of Ghana. 2001.
Boateng LA, The Ghana Southampton Scabies Research Partnership. Healthcare-seeking behaviour in reporting of scabies and skin infections in Ghana: a review of reported cases. Trans R Soc Trop Med Hyg. 2020;114(11):830–7.
Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF. Ghana maternal health survey 2017. Accra: GSS, GHS, and ICF; 2018.
Gao F, Kihal W, Le Meur N, Souris M, Deguen S. Does the edge effect impact on the measure of spatial accessibility to healthcare providers? Int J Health Geogr. 2017;16(1):46.
Whyle EB, Olivier J. Models of public–private engagement for health services delivery and financing in southern Africa: a systematic review. Health Policy Plan. 2016;31(10):1515–29.
Muhoza P, Tine R, Faye A, Gaye I, Zeger SL, Diaw A, et al. A data quality assessment of the first four years of malaria reporting in the Senegal DHIS2, 2014–2017. BMC Health Serv Res. 2022;22(1):18.
Boerma T, Victora CG, Sabin ML, Simpson PJ. Reaching all women, children, and adolescents with essential health interventions by 2030. British Medical Journal Publishing Group; 2020.
AbouZahr C, Boerma T. Health information systems: the foundations of public health. Bull World Health Organ. 2005;83:578–83.
Maïga A, Jiwani SS, Mutua MK, Porth TA, Taylor CM, Asiki G, et al. Generating statistics from health facility data: the state of routine health information systems in eastern and southern Africa. BMJ Glob Health. 2019;4(5):e001849.
Dako-Gyeke P, Aikins M, Aryeetey R, McCough L, Adongo PB. The influence of socio-cultural interpretations of pregnancy threats on health-seeking behavior among pregnant women in urban Accra, Ghana. BMC Pregnancy Childbirth. 2013;13(1):211.
Acknowledgements
This work was supported by the Economic and Social Research Council [grant number ES/P000673/1]. VA is supported by a Wellcome Trust Fellowship [number 211208]. We are thankful to the Ghana Health Service for making routine health data available and supporting service provision assessment surveys.
Funding
The study was funded by the Economic and Social Research Council (ESRC), UK [grant number ES/P000673/1]. The funder had no role in the design, data collection, analysis, interpretation of data and writing of the manuscript. The researchers were independent with no influence from the ESRC.
Author information
Authors and Affiliations
Contributions
WDG and JW conceptualised and designed the study, WDG analysed the data and wrote the original draft manuscript; JW, AJT, ZM, VA and AO supervised the analysis and reporting. All authors revised and edited the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the University of Southampton (Ref: 54949.A1 and 54944) and the Ghana Health Service ethics review committee (Ref: GHS-ERC008/05/20). Informed consent was obtained from all participants in the service provision assessment. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
AO at the time of the study is the Deputy Director General of the Ghana Health Service. The Ghana Health Service generates and owns the birth data analysed in this study and is responsible for healthcare delivery in Ghana. WDG previously worked with the Ghana Health Service as a public health information officer until 2017. The other authors have no interests to declare.
There are no financial interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dotse-Gborgbortsi, W., Tatem, A.J., Matthews, Z. et al. Delineating natural catchment health districts with routinely collected health data from women’s travel to give birth in Ghana. BMC Health Serv Res 22, 772 (2022). https://doi.org/10.1186/s12913-022-08125-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08125-9