Abstract
Background
Commercial geospatial data resources are frequently used to understand healthcare utilisation. Although there is widespread evidence of a digital divide for other digital resources and infra-structure, it is unclear how commercial geospatial data resources are distributed relative to health need.
Methods
To examine the distribution of commercial geospatial data resources relative to health needs, we assembled coverage and quality metrics for commercial geocoding, neighbourhood characterisation, and travel time calculation resources for 183 countries. We developed a country-level, composite index of commercial geospatial data quality/availability and examined its distribution relative to age-standardised all-cause and cause specific (for three main causes of death) mortality using two inequality metrics, the slope index of inequality and relative concentration index. In two sub-national case studies, we also examined geocoding success rates versus area deprivation by district in Eastern Region, Ghana and Lagos State, Nigeria.
Results
Internationally, commercial geospatial data resources were inversely related to all-cause mortality. This relationship was more pronounced when examining mortality due to communicable diseases. Commercial geospatial data resources for calculating patient travel times were more equitably distributed relative to health need than resources for characterising neighbourhoods or geocoding patient addresses. Countries such as South Africa have comparatively high commercial geospatial data availability despite high mortality, whilst countries such as South Korea have comparatively low data availability and low mortality. Sub-nationally, evidence was mixed as to whether geocoding success was lowest in more deprived districts.
Conclusions
To our knowledge, this is the first global analysis of commercial geospatial data resources in relation to health outcomes. In countries such as South Africa where there is high mortality but also comparatively rich commercial geospatial data, these data resources are a potential resource for examining healthcare utilisation that requires further evaluation. In countries such as Sierra Leone where there is high mortality but minimal commercial geospatial data, alternative approaches such as open data use are needed in quantifying patient travel times, geocoding patient addresses, and characterising patients’ neighbourhoods.
Similar content being viewed by others
Background
Sustainable Development Goal (SDG) 3, Target 3.8 seeks to ‘achieve universal health coverage, including financial risk protection, access to quality essential health-care services…for all’ [1], with a similar target 3.7 seeking to deliver universal maternal healthcare coverage. GIS has been proposed as an integrative information and communication technology tool for accelerating progress towards universal health coverage (UHC) [2]. Informed decision-making is central to achieving UHC and spatial analysis enables precise identification of health needs to inform system strengthening interventions and can help to identify localised gaps in service provision, masked by national or provincial averages [2]. Supporting UHC has been proposed as a means of reducing mortality. For example, increasing the proportion of births attended by a skilled birth attendant at primary healthcare facilities can contribute to reduced maternal mortality [3].
To realise the potential of GIS, it has been argued that the health sector has to ‘geoenable’ its health information systems [2]. ‘Geoenabling’ entails putting in place the necessary governance structures, technical capacity, guidelines, standards, protocols, technology and core data to harness GIS’ potential. Thus, a management structure that provides sufficient funding to underpin GIS adoption, resources for creating and maintaining health information systems, and an underlying national spatial data infrastructure are all prerequisites for GIS uptake in the health sector. Awareness of GIS use in healthcare planning remains low even in developed countries [4], where within the UK National Health Service its use remains largely restricted to mapping.
Here, we focus on one such potential barrier to GIS uptake in the health sector, namely the availability of core data. In representing population demand for healthcare and examining patient interactions with healthcare facilities, the use of several key commercial geospatial resources has become widespread in many developed countries. These geospatial resources include reference data sets and tools for geocoding the residential addresses of patients presenting at healthcare facilities [5, 6], and transportation data that enable patient travel times to be computed from place of residence to facility [7, 8]. They also include area statistics and geodemographic data sets, which provide insights into neighbourhood characteristics that may be associated with healthcare demand and utilisation [9,10,11].
Although such data resources are generally available in high income countries, in many low and middle income countries (LMICs), such data may be patchy in coverage, imprecise, or lacking altogether. Furthermore, in developed countries, national spatial data infra-structures (SDIs) typically enable national mapping and statistical agencies to maintain address databases or dwelling frameworks, and thereby construct small area statistics. In LMICs, however, barriers relating to the global digital divide such as lack of financial resources, insufficient leadership and governance, poor internet bandwidth [12], lack of trained personnel, lack of vendor support, and power dynamics over information release all inhibit SDI development [13]. Even where open data initiatives exist as in the example of Kenya, such resources may still remain limited [14], although there is evidence [15, 16] that coverage of the world’s largest open geospatial database, OpenStreetMap (OSM), is rapidly expanding in many LMICs.
Over 30 years ago, an ‘inverse care law’ was first identified by Hart [17], which highlighted the frequently encountered perverse relationship between healthcare provision and need. Since then, there have been numerous studies that have quantified greater healthcare provision among areas of low need and lower healthcare provision in areas of high need [18,19,20,21], confirming this phenomenon in many settings. It is unclear whether data for planning healthcare delivery follow a similar pattern.
Methods
Aims
In this paper, we aim to quantify the extent to which the same perverse relationship with health needs applies to geospatial data availability as with healthcare provision. We explore two scales through a cross-sectional, ecological study design. We firstly examine the relationship between geospatial data availability and health need as measured by all-cause mortality and mortality due to three groups of causes, globally at national level. We then consider the relationship between health need and geospatial data availability in two sub-national case studies from Ghana and Nigeria.
Data
At international level, we examine the availability, by country, of three sets of commercial data resources that are central to understanding population demand for healthcare and spatial patterns of healthcare utilisation. These are geocoding tools for locating patients’ residences; transportation network resources for computing patient travel from place of residence to health facility; and area statistics for characterising the neighbourhoods where patients live. We excluded other commercial geospatial data resources not directly related to healthcare-seeking behaviour, such as remotely sensed imagery. To identify such resources, we used the search strategy in Additional file 1: Table S1. We included only geospatial data resources that met the following criteria:
-
Related to more than five countries, thereby having an international rather than national or regional remit
-
Were not derived exclusively from open data and were provided as a commercial service
-
Did not duplicate data resources already included in our analysis (for example where there were several APIs based on the same underlying data resource)
-
Provided published statements of data availability or quality by country.
Where necessary, we contacted data providers to request permission to use data availability or quality statements in our analysis, only including those where such permission was granted. The geospatial resources that met all these criteria were included in our analysis are shown in Table 1 (Additional file 1: Tables S2–S4 documents data resources that were excluded and reasons for this).
Alongside these resources, we used all-cause mortality by country for the most recent period (2000–2015) reported by the World Health Organisation (WHO) [22], as a general health outcome measure and thereby metric of healthcare need. We also separately examined the major WHO categorization of mortality: non-communicable diseases; injuries; communicable diseases, maternal, perinatal, and nutritional conditions for 183 countries.
Analysis
International analysis
National mortality data from WHO were age-standardised to account for differences in population structure between countries. As dependent territories are not reported separately in WHO mortality data, these were excluded from our analysis.
We then generated commercial geospatial resource indicators by country as follows:
-
Geocoding resources Since the published level of geocoding availability and quality via the Google Application Programming Interface (API) scarcely varied by country, we used the geocoding precision levels published by Pitney Bowes, TomTom, MapBox, Loqate, and the Environmental Systems Research Institute (ESRI).
-
Resources for computing patient travel times To characterise availability and quality of resources for computing travel times via the Google API, we generated a composite index by summing reported data availability for cycling directions, walking directions, driving directions, speed limits and availability of a traffic layer. Each of these was scored as two for ‘good quality and availability’, one for ‘approximate data quality and availability’ and zero otherwise. ESRI/HERE data quality and availability was characterised by six levels, based on availability of traffic and speed limit data, and completeness of street network coverage, whilst TomTom resources were characterised by availability of traffic flows, traffic incidents, and online routing. We separately recorded the availability of a traffic layer via MapBox and availability of routing for car travel only or car travel and public transport via iGeoloise TravelTime.
-
Area statistics for characterising patients’ neighbourhoods To quantify availability of neighbourhood statistics by country, we computed three measures. Firstly, as a measure of spatial data disaggregation, we used the mean population per areal unit (lower mean populations indicate a higher level of spatial disaggregation) in Michael Bauer data sets. Where no data were available from this provider for a given country, we used the national 2015 population estimate from the WHO mortality database. Secondly, for the most detailed geography available in the Michael Bauer data, we counted the number of areal attributes available per country, setting this to zero where no data were available. Finally, for each country, we identified whether only one or both the geodemographic classifications (i.e. CAMEO Worldwide and Mosaic Global) were available, alongside availability of Maptitude demographic data.
To examine the availability of these geospatial resources relative to healthcare need, as measured by standardised all-cause mortality and cause-specific mortality, we computed relative concentration indices and slope indices of inequality [23] for each of these measures of geospatial data availability using a tool from Public Health England [24]. In this context, the slope index of inequality measured the change in mortality relative to ranked geospatial data availability/quality, whilst the relative concentration index measured the mortality gradient against relative geospatial data availability/quality.
We also created a composite index of commercial geospatial resource quality/availability (geospatial resource index) by combining these various indicators. For each of the three index domains (geocoding resources, patient travel, and neighbourhood characterisation), we ranked each country from highest to lowest based on each of the above indicators, then summed these ranks, dividing the total by the maximum possible summed rank to give an index for each domain between 0 and 1. To avoid the index being dominated by indicator availability at domain level, we then summed the three domain index values. We regressed logged standardised mortality against the geospatial resource index, identifying as outliers in terms of data availability those countries with studentised residuals greater than two. We also calculated the correlation of the geospatial resource index with the percentage of internet users and gross domestic product (GDP) per capita for 2016 in each country [25].
Sub-national case studies
To examine sub-national geospatial commercial resource availability and quality, two sub-national case studies were conducted, one in Eastern Region, Ghana and the other in Lagos State, Nigeria. Both focussed on success rates for geocoding facility locations (health facilities and schools respectively). In the absence of robust district-level mortality estimates, both studies examined geocoding success rates relative to area deprivation at administrative level 2 (districts in Ghana or local government areas in Nigeria). In this context, we consider area deprivation to reflect ‘an area’s potential for health risk from ecological concentration of poverty, unemployment, economic disinvestment, and social disorganisation’ [26].
In Eastern Region, 984 health facility place-names from 25 districts were obtained from the Ghana Health Service routine data repository (DHIMS2) and geocoded via an interface to the Google Maps API Version 2 [27]. Geocoding success was measured as the proportion of facilities per district for which a location within Eastern Region was returned. District deprivation was assessed firstly via the 2017 UNICEF District League Table (DLT) [28], a composite index of district development based on indicators of education, sanitation, rural water, health, security and governance. Secondly, district deprivation was also assessed via a bespoke district deprivation index. The bespoke deprivation index was created from 12 indicators representing six domains: information access, education, energy, employment, water and sanitation, and living conditions, adapting an approach used in South Africa [29]. Indicators values were drawn from 2010 census data [30]. Within each domain, each indicator was standardised by conversion to a z-score, with z-scores averaged for each domain. The average scores for the six domains were then summed to give a composite deprivation score.
Similarly, in Lagos State 310 schools, both private and public, from 20 Local Government Areas (LGAs) were obtained from online news media [31]. These were then geocoded using the Google Maps API Version 2 via BatchGeo [32]. A deprivation index with the same six domains as Ghana was created for the LGAs, but with 9 indicators drawn from 2006 census data acquired from the National Population Commission. These were then standardised and combined using the same method as for Eastern Region. For both case studies, geocoding success per district/LGA was then plotted against deprivation. Relative concentration indices and slope indices of inequality were computed for district-level geocoding success rates versus the deprivation measures.
Results
Characteristics of commercial geospatial data resources
Table 2 summarises the availability and precision of commercial geospatial resources for the 183 countries for which data were available in the WHO mortality database. There is considerable international variation in each indicator’s availability, with for example both predictive and live traffic data underpinning ESRI’s drive-time calculations in 11 countries, but conversely only partial coverage of the major road network being available in 24 countries. Similarly, market and demographic statistics were available for areas with average populations of less than a thousand in some countries, but over ten million in others.
International inequality in access to commercial geospatial data resources
Table 3 shows two health inequality metrics, the relative concentration index and slope index of inequality, for national all-cause mortality versus international availability and quality of various commercial geospatial data resources. Slope index of inequality values indicate the effect on all-cause mortality of moving from the most data-poor country to the most data-rich. Negative concentration indices suggest mortality is concentrated among data-poor populations, whilst zero indicates no mortality gradient relative to geospatial data. Slope indices of inequality were significantly different from zero for most sources of commercial geospatial data considered, suggesting significant health inequalities for most resources. However, levels of inequality were lower for resources for computing patient travel times than for resources for geocoding patient addresses or characterising patients’ areas of residence. For example, concentration indices for ESRI’s geocoding service and population size of Michael Bauer’s areal units were − 0.14 and − 0.12 respectively, whereas concentration indices for Google and ESRI’s patient travel resources were less than − 0.07.
Table 4 shows the inequality metrics broken down by the WHO cause-specific mortality categorization. As indicated by the concentration index values differing from zero, measured inequalities were greatest for the communicable disease group and lowest for non-communicable diseases, both for the overall index and for the geocoding and neighbourhood characterisation domains. Concentration index values and therefore measured inequality were closer to zero for the patient travel domain, as with all-cause mortality.
International geospatial resource index
Figure 1 shows the international geospatial resource index (illustrating quality/availability of commercial geospatial data resources for healthcare planning). According to the composite index, the quality/availability is generally high in the Americas, Australasia and Europe, but low in Africa and south Asia. However, some data providers document potentially valuable geospatial resources for healthcare planning in countries with high mortality, particularly in west and southern Africa. For example, a traffic layer is available via Google and interpolated street address level geocoding is documented by Pitney Bowes for Nigeria, both potentially valuable in understanding patient travel.

(based on a Winkel-Tripel projection. Portions of this graphic are modifications based on work created and shared by Google and thematicmapping.org and used according to terms described in the Creative Commons 3.0 Attribution License. Used with permission. Copyright © 2017 Esri, ArcGIS Online, HERE, Increment P, GlobeTech and the GIS User Community. All rights reserved. © 2017 Michael Bauer Research GmbH, © TomTom 2018)
An index of commercial geospatial resource quality/availability for healthcare planning by country
The geospatial resource index was strongly correlated with the percentage of internet users per country in 2016 (r = 0.77, p < 0.001, n = 183) and to a lesser extent with GDP per capita (r = 0.68, p < 0.001, n = 174). Several African countries such as South Africa and Mozambique had comparatively high geospatial data availability/quality scores given GDP, whilst several of the Gulf States (e.g. Qatar, United Arab Emirates) and smaller island states (e.g. Iceland, the Seychelles) had comparatively low index values given their GDP per capita. Similar patterns were observable for index values versus internet use.
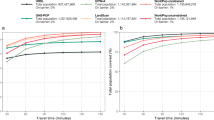
Figure 2 shows the distribution of standardised all-cause mortality in relation to the geospatial resource index. As anticipated from the deprivation indicators above, the pattern of all-cause mortality broadly follows geospatial resource quality/availability. Several outliers are labelled in Fig. 2. Countries with low all-cause mortality and low commercial geospatial data resources were typically either small island states such as Malta and the Maldives, or states with strict controls on international transfers of national data, such as South Korea and Cuba. South Africa was notable for its high all-cause mortality but comparatively high commercial geospatial resource availability, with similar outliers being in southern or west Africa.

(labelled countries were identified as outliers. Portions of this graphic are modifications based on work created and shared by Google and used according to terms described in the Creative Commons 3.0 Attribution License. Used with permission. Copyright © 2017 Esri, ArcGIS Online, HERE, Increment P, GlobeTech and the GIS User Community. All rights reserved. © 2017 Michael Bauer Research GmbH; © TomTom 2018)
Age-standardised all-cause mortality for 2015 versus a an index of commercial geospatial resource quality/availability; b ranked availability of Google Maps travel time resources
Sub-national case studies
Figure 3 shows the relationship between geocoding success rate and deprivation, in Lagos State and Eastern Region, with no clear relationship emerging overall. Geocoding success rates were low for health facilities in Eastern Region, but much higher for schools in Lagos State. In Eastern Region, districts such as East Akim and Birim Central had high success rates although their deprivation score was close to the average. Further exploration revealed these two districts had the highest number of hospitals (4 each) in the region and hospitals had the highest geocoding success rate (70.6%) compared with other health facility types. Likewise, the regional capital of New Juaben with 3 hospitals, was least deprived and had a high geocoding success rate. In Nigeria, two LGAs containing a small number of schools, Badagry and Ibeju-Lekki, were more deprived and had lower geocoding success rates, particularly influencing the observed relationship between deprivation and geocoding success.
Table 5 shows inequality metrics for geocoding success rates versus area deprivation at the LGA or district level in Lagos State, Nigeria, and Eastern Region, Ghana. There was no evidence of inequality in geocoding success relative to area deprivation in Lagos State, as indicated by the concentration index of zero. In Ghana, evidence for lower geocoding success in more deprived areas was mixed. When the DLT was used to measure area deprivation, confidence intervals for the slope index of inequality straddled zero, indicating no significant inequality. When the bespoke area deprivation index was used, the slope index of inequality was significantly different from zero.
Discussion
To our knowledge, our analysis is the first to examine global patterns of commercial geospatial data availability in relation to health outcomes. As observed with healthcare services, both internationally and for two sub-national case studies, these data are inversely correlated with health need, as measured by mortality and deprivation respectively. This disparity in geospatial data availability is more pronounced for mortality due to communicable diseases. Such data are thus frequently unavailable for planning healthcare provision or geocoding cases for widespread communicable diseases such as malaria. The availability of commercial geospatial data resources broadly follows the same pattern as that identified in analyses of the global digital divide, with for example sub-Saharan Africa being the world region lagging furthest behind North America in internet users [33] and Africa having the lowest Information and Communication Technology Development Index [34]. The pattern of outliers is somewhat different to these more general analyses of the global digital divide, however. For example, an assessment of digitalisation relative to GDP per capita [35] indicated lower than anticipated digitalisation in Oman and Kuwait but higher digitalisation in South Korea. We observed the same relationship for the Gulf States in relation to our commercial geospatial index but low international availability of commercial geospatial data in South Korea. However, because of restrictions on the export of mappable data out of the country, South Korea has previously been reported as lacking data from major providers such as Google [36].
In the absence of such commercial tools, and where sufficient capacity exists, researchers in LMICs have resorted to alternative strategies for geocoding data, computing drive-times, and characterising patients’ places of residence. Where the human resources, infrastructure, and tools exist, one geocoding strategy is to rely on open data, particularly OSM, as has been attempted in Thailand and Mozambique for healthcare management [37, 38]. Elsewhere, a study in Yemen, relied on direct measurement of drive-times taken on specific routes [39]. A Kenyan study explored participatory mapping and use of local landmarks as strategies for geocoding patient addresses [40], whilst in a Mexican study, a software application was developed that allowed patients to identify their place of residence through interpretation of Google Earth and StreetView imagery [41]. In Cote d’Ivoire, aggregated call record data from mobile phones have been used to develop a proxy for regional socio-economic indicators [42], whilst in Accra, vegetation metrics derived from QuickBird satellite imagery were correlated with a slum index [43]. Without such innovative geocoding or neighbourhood characterisation strategies, there is potential for misclassification of neighbourhood characteristics [44] and environmental exposures [45] when analysing LMIC patient data using inexact geocodes or areal statistics relating to large populations.
International organisations have invested heavily in geospatial infra-structure, capacity-building, and technology to address this paucity of commercial data and its affordability in low-resource settings. The WHO for example has developed AccessMod to estimate patient travel times to health facilities via a cost surface approach [46]. Because of limited access to software and technical GIS skills, WHO also developed the HealthMapper software, which packages public domain spatial databases with a user-friendly interface to broaden uptake of GIS for healthcare planning. HealthMapper has been used in schistosomiasis control [47] and prioritising areas for filariasis elimination [48]. More recently, Measure Evaluation have supported health management information systems by developing the Place Mapping plug-in for QGIS to ease handling and display of point data sets [49] and provided guidance on diagnosing positional errors [50].
We found less conclusive evidence that geocoding success rates were lower in deprived areas when considering the two sub-national case studies of Lagos State, Nigeria and Eastern Region, Ghana. There was no evidence of inequality in geocoding success in Lagos State, but mixed evidence of such inequality in Eastern Region. However, elsewhere an apparent inverse relationship between geocoding outcomes and area deprivation has been observed at local level in other LMICs. A study in the Brazilian city of Belo Horizonte, for example, found that geocoding precision via the Google geocoding API was lower in slum areas than in formal urban neighbourhoods [51]. In response to this issue, the What3Words georeferencing system, which uses an algorithm to assign three words as a unique, human-friendly georeference to each of 57 trillion grid squares globally, has been used to locate addresses in Brazilian favelas lacking conventional addressing systems [52].
Our findings are subject to several limitations. Our study assumes that the data provider’s published country coverage information is an accurate reflection of geospatial data availability and precision across all countries. In reality, export of geospatial data from one country to another may be restricted by trade embargos, as has previously happened with satellite imagery exports to India for example [53], and where commercial geospatial data are available internationally, they may be unaffordable within the national health sector. In assessing the international availability of geodemographic classifications, we focussed on two major international data providers only, potentially omitting smaller data providers operating in individual countries. However, a recent study of the international availability of geodemographic classifications [54] showed very similar patterns to that found here. Computed inequality indices are also likely to be lower for metrics of geospatial data availability and precision based on a small number of ordinal classes (e.g. for geodemographic data availability), than metrics on a ratio scale (e.g. mean population per areal unit). In our sub-national case studies, geocoding success rates for higher tier facilities (e.g. hospitals or large secondary schools) may be higher than for lower tier facilities (e.g. primary care facilities such as Community-Based Health Planning and Services compounds). Since such facilities are more often found in urban areas, such heterogeneity in facility type may lead to an over-estimate of inequality in geocoding resource access.
Given the rapid pace of change in the geospatial data sector, this analysis could be repeated in the future to monitor rapidly changing data availability in relation to health outcomes. We have only considered the relationship between commercial geospatial resources and mortality, but geospatial resource availability could also be examined in relation to underlying drivers of health outcomes, such as country income levels, internet access, and relevant government policies, or in relation to measures relevant for other sectors (such as infrastructure). There would also be scope to combine the country-level results presented here on commercial geospatial data with recent assessments of OSM completeness by country [15, 16]. These studies, based on stratified assessment of OSM road completeness [16] or saturation of user contributions [15], suggest that global commercial geospatial resources and OSM completeness patterns are somewhat different, with for example, China and Egypt having low OSM completeness [16]. The potential utility of commercial geospatial data resources for healthcare planning could also be explored through a case study country (e.g. South Africa), deliberately selected because of its high mortality and high geospatial data availability.
The comparatively richer commercial resources in west and southern African countries such as Nigeria and South Africa merit further investigation for healthcare planning in these countries, subject to sufficient funds being available to support their use in a given project.
In contrast to analyses from elsewhere [51], our sub-national analyses in Lagos State suggested only limited evidence that geocoding success was lower in deprived areas. Our inconclusive results may be because the large areal units we used to assess deprivation may mask localised pockets of deprivation, which have been identified via previous work in Accra [55]. In our analysis, we implicitly use geocoding success rates to assess spatial variation in the Google Maps API reference data set and geocoding algorithm performance. However, geocoding success also depends on the quality of the input address data [56] and this will have been affected by local variations in service provision tiers, language of place-names and place-name aliases in our Nigerian and Ghanaian case studies. Furthermore, in our two case studies, success rates in geocoding service locations in Eastern Region, Ghana, and Lagos State, Nigeria were very different, despite identical documented levels of geocoding service precision. Despite their growing potential, this suggests careful evaluation of such resources is needed prior to their application to healthcare management.
In many other countries with high mortality, commercial geospatial data availability was very low. By examining commercial geospatial resource availability alongside OSM completeness [16], such countries could be targeted via non-profit initiatives to increase the availability of open geospatial data availability, such as those undertaken through OSM-based volunteer mapping initiatives by humanitarian organisations [57, 58]. Whilst commercial geospatial resource availability may improve in these countries in the future, in the interim, there remains a need for innovative solutions to geocoding outpatient data, estimating patient travel times and characterising neighbourhoods in such countries as described above.
Conclusions
To our knowledge, our analysis is the first to examine global patterns of commercial geospatial data availability in relation to health outcomes. The relationship observed between commercial geospatial resource availability and health needs suggests LMICs still have inadequate geospatial resources for the type of granular analysis needed to drive the SDG agenda surrounding UHC. This inequality in data availability is more pronounced for mortality due to communicable diseases than for all-cause mortality. There were some outliers, however: several west and southern African countries such as Nigeria and South Africa had comparatively high geospatial data availability and high mortality. In contrast, there were several countries with low mortality and comparatively geospatial data availability, often island states (e.g. the Maldives) or those with policy restrictions on geospatial data (e.g. South Korea). This analysis thus suggests some resources, particularly those for quantifying patient travel times, are penetrating countries with high all-cause mortality. In countries such as South Africa and Nigeria where there is high mortality but also comparatively rich commercial geospatial data, these data are a potential resource for examining healthcare utilisation that requires further evaluation. In countries such as Sierra Leone where there is high mortality but minimal commercial geospatial data, alternative approaches, for example based on open data such as OSM, are needed in quantifying patient travel times, geocoding patient addresses, and characterising patients’ neighbourhoods.
In many instances, our examination of patterns of commercial geospatial availability confirms other studies of global digitalisation, with for example lower levels of digitalisation in the Gulf States for a given level of GDP per capita. However, even where this is comparatively high availability of relevant commercial geospatial data availability, this alleviates just one barrier among many that inhibit uptake of GIS in healthcare planning. Beyond increasing the availability of core data, further investments are needed in technical capacity-building, awareness-raising, guidelines, standards and protocols if the potential of such data is to be realised within the health sector.
Abbreviations
- API:
-
Application Programming Interface
- DLT:
-
District League Table
- DHIMS:
-
District Health Information Systems
- ESRI:
-
Environmental Systems Research Institute
- GDP:
-
gross domestic product
- LGA:
-
local government area
- LMICs:
-
low and middle-income countries
- OSM:
-
OpenStreetMap
- SDGs:
-
Sustainable Development Goals
- SDI:
-
spatial data infra-structure
- UHC:
-
universal health coverage
- WHO:
-
World Health Organisation
References
United Nations. Sustainable development goal 3: ensure healthy lives and promote well-being for all at all ages. New York: Department of Economic and Social Affairs; 2018 [cited 2018 18 April 2018]. https://sustainabledevelopment.un.org/sdg3.
Roth S, Landry M, Ebener S, Marcelo A, Kijsanayotin B, Parry J. The geography of universal health coverage: why geographic information systems are needed to ensure equitable access to quality healthcare. Manila: Asian Development Bank; 2016.
Campbell O, Graham W. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):7–13.
Shaw N. Geographical information systems and health: current state and future directions. Healthc Inf Res. 2012;18(2):88–96.
Rosu A, Chen DM. An improved approach for geocoding Canadian postal code-based data in health-related studies. Can Geogr Geogr Can. 2016;60(2):270–81.
Edwards SE, Strauss B, Miranda ML. Geocoding large population-level administrative datasets at highly resolved spatial scales. Trans GIS. 2014;18(4):586–603.
Sharma DK, Vangaveti VN, Larkins S. Geographical access to radiation therapy in North Queensland: a retrospective analysis of patient travel to radiation therapy before and after the opening of an additional radiotherapy facility. Rural Remote Health. 2016;16(1):3640.
Chu S, Boxer R, Madison P, Kleinman L, Skolarus T, Altman L, et al. Veterans affairs telemedicine: bringing urologic care to remote clinics. Urology. 2015;86(2):255–60.
Nnoaham KE, Frater A, Roderick P, Moon G, Halloran S. Do geodemographic typologies explain variations in uptake in colorectal cancer screening? An assessment using routine screening data in the south of England. J Public Health. 2010;32(4):572–81.
Grubesic TH, Miller JA, Murray AT. Geospatial and geodemographic insights for diabetes in the United States. Appl Geogr. 2014;55:117–26.
Petersen J, Gibin M, Longley P, Mateos P, Atkinson P, Ashby D. Geodemographics as a tool for targeting neighbourhoods in public health campaigns. J Geogr Syst. 2011;13(2):173–92.
Hilbert M. The bad news is that the digital access divide is here to stay: domestically installed bandwidths among 172 countries for 1986–2014. Telecommun Policy. 2016;40(6):15.
Bishop ID, Escobar FJ, Karuppannan S, Williamson IP, Yates PM, Suwarnarat K, et al. Spatial data infrastructures for cities in developing countries—lessons from the Bangkok experience. Cities. 2000;17(2):85–96.
Williams S, Marcello E, Klopp JM. Toward open source Kenya: creating and sharing a GIS database of Nairobi. Ann Assoc Am Geogr. 2014;104(1):114–30.
Grochenig S, Brunauer R, Rehr K. Digging into the history of VGI data-sets: results from a worldwide study on OpenStreetMap mapping activity. J Locat Based Serv. 2014;8(3):198–210.
Barrington-Leigh C, Millard-Ball A. The world’s user-generated road map is more than 80% complete. PLoS ONE. 2017;12(8):e0180698.
Hart JT. The inverse care law. Lancet. 1971;297(7696):8.
McLean G, Guthrie B, Mercer SW, Watt GCM. General practice funding underpins the persistence of the inverse care law: cross-sectional study in Scotland. Br J Gen Pract. 2015;65(641):E799–805.
Tansley G, Stewart BT, Gyedu A, Boakye G, Lewis D, Hoogerboord M, et al. The correlation between poverty and access to essential surgical care in Ghana: a geospatial analysis. World J Surg. 2017;41(3):639–43.
Chavehpour Y, Rashidian A, Raghfar H, Sefiddashti SE, Maroofi A. ‘Seeking affluent neighbourhoods?’ A time-trend analysis of geographical distribution of hospitals in the Megacity of Tehran. Health Policy Plan. 2017;32(5):669–75.
Wright J, Martin D, Cockings S, Polack C. Overall Quality of Outcomes Framework scores lower in practices in deprived areas. Br J Gen Pract. 2006;56(525):277–9.
World Health Organization. Global health estimates 2015: deaths by cause, age, sex, by country and by region, 2000–2015. In: World Health Organization, editor. Geneva: World Health Organization; 2016.
Regidor E. Methods for measuring health inequalities: part 2. J Epidemiol Community Health. 2004;58:4.
Public Health England. Excel tool for calculating various inequality measures, such as Slope Index of Inequality and Concentration Index. March 2014 ed. Redditch: Public Health England; 2014.
World Bank. World Bank Open Data Washington DC: World Bank; 2018 [17 April 2018]. https://data.worldbank.org/.
Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socio-economic status. Epidemiology. 1997;8(1):42–7.
Aanensen D. spatialepidemiology.net London: Imperial College; 2018 [29 March 2018]. http://www.spatialepidemiology.net/.
UNICEF, CDD Ghana. Ghana’s District League Table. New York: UNICEF; 2017.
Wright G, Barnes H, Noble M, Dawes A. The South African index of multiple deprivation for children 2001 at datazone level. Pretoria: Department of Social Development; 2009.
Ghana Statistical Service. 2010 Population and housing census, Eastern region analytical report; 2013.
Anuoluwap B. List of registered schools in Lagos State Lagos: MySchoolNews; 2018 [29 March 2018]. https://9jaskulnews.blogspot.co.uk.
BatchGeo. BatchGeo Vancouver: BatchGeo; 2018 [29 March 2018]. https://batchgeo.com/.
Robison KK, Crenshaw EM. Reevaluating the global digital divide: socio-demographic and conflict barriers to the internet revolution. Sociol Inq. 2010;80(1):34–62.
International Telecommunications Union. Measuring the information society report 2015. Geneva: International Telecommunications Union; 2015.
Billon M, Lera-Lopez F, Marco R. Differences in digitalization levels: a multivariate analysis studying the global digital divide. Rev World Econ. 2010;146(1):39–73.
Associated Press. No driving directions: Google, South Korean Can’t Reach Map Deal VOA News; 2016 [cited 2017 31 Oct 2017]. https://www.voanews.com/a/google-maps-data-south-korea/3602188.html.
Makanga PT, Schuurman N, Sacoor C, Boene H, Von Dadelszen P, Firoz T. Guidelines for creating framework data for GIS analysis in low- and middle-income countries. Can Geogr Geogr Can. 2016;60(3):320–32.
Ferguson WJ, Kemp K, Kost G. Using a geographic information system to enhance patient access to point-of-care diagnostics in a limited-resource setting. Int J Health Geogr. 2016;15:10.
Al-Taiar A, Clark A, Longenecker JC, Whitty CJM. Physical accessibility and utilization of health services in Yemen. Int J Health Geogr. 2010;9:38.
Stresman GH, Stevenson JC, Owaga C, Marube E, Anyango C, Drakeley C, et al. Validation of three geolocation strategies for health-facility attendees for research and public health surveillance in a rural setting in western Kenya. Epidemiol Infect. 2014;142(9):1978–89.
Beletsky L, Arredondo J, Werb D, Vera A, Abramovitz D, Amon JJ, et al. Utilization of Google enterprise tools to georeference survey data among hard-to-reach groups: strategic application in international settings. Int J Health Geogr. 2016;15:24.
Mao H, Shuai X, Ahn Y-Y, Bollen J. Quantifying socio-economic indicators in developing countries from mobile phone communication data: applications to Côte d’Ivoire. EPJ Data Sci. 2015;4:15.
Weeks JR, Hill A, Stow D, Getis A, Fugate D. Can we spot a neighborhood from the air? Defining neighborhood structure in Accra, Ghana. GeoJournal. 2007;69(1–2):9–22.
Ribeiro AI, Olhero A, Teixeira H, Magalhaes A, Pina MF. Tools for address georeferencing—limitations and opportunities every public health professional should be aware of. PLoS ONE. 2014;9(12):e114130.
Mazumdar S, Rushton G, Smith BJ, Zimmerman DL, Donham KJ. Geocoding accuracy and the recovery of relationships between environmental exposures and health. Int J Health Geogr. 2008;7:13.
Ray N, Ebener S. AccessMod 3.0: computing geographic coverage and accessibility to healthcare services using anisotropic movement of patients. Int J Health Geogr. 2008;7:63.
Chammartin F, Hurlimann E, Raso G, N’Goran E, Utzinger J, Vounatsou P. Statistical methodological issues in mapping historical schistosomiasis survey data. Acta Trop. 2013;128(2):345–52.
Ngwira B, Tambala P, Perez A, Bowie C, Molyneux D. The geographical distribution of lymphatic filariasis infection in Malawi. Filaria J. 2007;6:12.
Evaluation Measure. The place mapping tool: a plug-in for QGIS. Chapel Hill: University of North Carolina; 2017.
Measure Evaluation. Overview: spatial quality anomalies diagnosis (SQUAD) tool for QGIS. Chapel Hill, North Carolina: University of North Carolina, 2018 April 2018. Report No.
Davis CA, de Alencar RO. Evaluation of the quality of an online geocoding resource in the context of a large Brazilian city. Trans GIS. 2011;15(6):851–68.
Jones G. Human friendly coordinates. Geoinformatics. 2015;18(5):10–2.
Nagendra N. Industry participation in India’s space program: current trends and perspectives for the future. Int J Space Politics Policy. 2016;14(2–3):237–55.
Ojo A. Geodemographic classification systems for the developing world: the case of Nigeria and the Philippines. Sheffield: University of Sheffield; 2010.
Aggrey-Korsah E, Oppong J. Researching urban slum health in Nima, a slum in Accra. In: Weeks JR, Hill A, Stoler J, editors. Spatial inequalities: health, poverty and place in Accra, Ghana. Dordrecht: Springer; 2013. p. 109–24.
Zanderbergen P. Geocoding quality and implications for spatial analysis. Geogr Compass. 2009;3(2):647–80.
de Albuquerque JP, Herfort B, Eckle M. The tasks of the crowd: a typology of tasks in geographic information crowdsourcing and a case study in Humanitarian mapping. Remote Sens. 2016;8(10):859.
Givoni M. Between micro mappers and missing maps: digital humanitarianism and the politics of material participation in disaster response. Environ Plan D Soc Space. 2016;34(6):1025–43.
Authors’ contributions
WD, AA, NW, and JW designed the study. AA prepared and analysed the Nigerian case study data, WD prepared and analysed the Ghanaian case study data, and JW and MT prepared and analysed the international data sets. WD and JW drafted the manuscript, which was reviewed by all other authors. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The mortality and Google-derived datasets analysed during the current study are available in the WHO Global Health Organisation repository at http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html and the Google Maps Application Programming Interfaces documentation, https://developers.google.com/maps/coverage. Data concerning the percentage of internet users per country and GDP per country are available as open data from https://data.worldbank.org/ . The other web documentation that supports the findings of this study are available from ESRI, Pitney Bowes, MapBox, TomTom and Michael Bauer but restrictions apply to the availability of these web pages, which were used under license or with permission for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the data providers. The deprivation datasets for Ghana are in the 2010 Population and housing census analytical reports available online for download, whilst names of healthcare facilities were provided with permission by Ghana Health Services. The District League Table data for Ghana are available for download from UNICEF Ghana and the Ghana Centre for Democratic Development: http://www.unicef.org/ghana/. 2006 census data for Nigeria were acquired under licence from the National Population Commission, whilst school names are available at https://9jaskulnews.blogspot.co.uk.
Consent for publication
Not applicable.
Ethics approval and consent to participate
As all human subjects data were aggregated to the district or national level and anonymised, the need for ethical approval was waived under the current policy of the Ethics Committee Faculty of Social, Human, and Mathematical Sciences, University of Southampton.
Funding
WD is a Commonwealth Scholar, and was funded by the UK government and University of Southampton. MT’s contribution to the paper was supported by the Economic and Social Research Council (Grant No. ES/P000673/1). Neither funding body had a role in the design of the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1.
Search strategy for identifying relevant commercial geospatial data resources and details of data resources excluded from the analysis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dotse-Gborgbortsi, W., Wardrop, N., Adewole, A. et al. A cross-sectional ecological analysis of international and sub-national health inequalities in commercial geospatial resource availability. Int J Health Geogr 17, 14 (2018). https://doi.org/10.1186/s12942-018-0134-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12942-018-0134-z