Abstract
Background
Late antenatal care initiation is linked to a higher risk of maternal death. Women who do not start ANC at an early stage may experience the effects of pregnancy-related health difficulties, as well as long-term health issues and pregnancy complications. Therefore, our study aimed to determine the prevalence of late initiation of antenatal care and associated factors among pregnant women in Jimma Zone public Hospitals.
Methods
A facility-based cross-sectional study design was employed in Jimma zone public hospitals from February 1 up to 30 March 2020 and 409 pregnant women were participated in the study by using a systematic random sampling method. Structured questionnaire was used to collect data that contain socio demographic variables, socio cultural variables, pregnancy related factors and predisposing factor related variables. The data was entered into EPI data version 3.1 and exported to SPSS version 20 for statistical analysis. Binary and multivariable logistic regression analysis were performed by using 95%CI and significance was declared at P < 0.05.
Result
Forty-eight percent of pregnant women were initiated their first ANC late. Primary education (AOR = 0.242; 95% CI, 0.071–0.828) and college diploma and above was (AOR = 0.142; 95% CI, 0.040- 0.511), mothers with an unplanned pregnancy (AOR = 11.290; 95%CI, 4.109–31.023), time taken to arrive the health facility greater than sixty (60) minutes (AOR = 8.285; 95% CI, 2.794–24.564) and inadequate knowledge about ANC service (AOR = 4.181; 95%CI, 1.693–10.348) were associated with late first Antenatal care initiating.
Conclusion
The prevalence of late initiation of ANC still remains a major public health concern in the study area. Level of education, unplanned pregnancy, distance from house to health facility, and lack of understanding about ANC services were all found to be significant variables in late ANC starting. As a result, healthcare workers can provide ongoing health education on the need of starting antenatal care visits early to avoid unfavorable pregnancy outcomes by considering all identified factors.
Similar content being viewed by others
Introduction
Antenatal care (ANC) is a type of care given to pregnant women and is considered a key maternal service in improving a wide range of health outcomes for women and newborns. The Antenatal Care (ANC) model recommended by the World Health Organization (WHO) calls for a minimum of eight ANC visits, with the first one occurring during the first trimester [1]. ANC initiation period is defined differently in different countries; European countries consider it a late ANC initiation if it occurs after the first trimester, while Pakistan considers it a late ANC initiation if it occurs after 24 weeks of gestation [2, 3]. Late ANC initiation, on the other hand, is defined in Ethiopia as a pregnant woman visiting for the first time after 16 weeks of pregnancy [4].
Implementing appropriate ANC services and evidence-based techniques during ANC at the suggested period can benefit both the mother and the fetus. They also promote maternal nutrition, give health education, and help to avert obstetric emergencies and other life-threatening situations. This is also an appropriate time for women to begin planning for birth and newborn care [5,6,7,8].
In the year 2001, the WHO issued guidance on a new model of ANC called goal-oriented or focused ANC, for implementation in developing countries [9]. In low-risk pregnancies, WHO recommends four antenatal care visits with evidence-based content prescribed for each: the first during the first trimester; the second around week 26; the third around week 32; and the fourth and final visit between weeks 36 and 38 [9, 10].
The late ANC initiation magnitude is different for countries. The lowest among European countries was 2% for Poland, and the highest was 33% for Malta [11]. In Pakistan, 71% of women received late antenatal care [12]. According to the Ethiopian Demographic Health Survey (EDHS, 2016), 80% of women had their first ANC visit after 16 weeks of gestational age [5]. Late initiation of ANC is a significant risk factor for maternal mortality. Women who do not begin ANC at an early stage may experience the effects of pregnancy-related health conditions, as well as long-term health problems and complications related to pregnancy [7, 13].
Every day, over 800 women die from complications connected to pregnancy and childbirth around the world, with Sub-Saharan Africa, which includes Ethiopia, accounting for over 66% of those deaths. According to the World Health Organization (WHO), 11,000 maternal deaths occurred in Ethiopia in 2015 during pregnancy, childbirth, and the postpartum period [14]. Postpartum hemorrhage, sepsis, pre-eclampsia, eclampsia, and delivery complications are the leading causes of maternal mortality in Ethiopia [2]. Despite the fact that the majority of maternal deaths are preventable, many women lack access to evidence-based interventions including antenatal care (ANC) during pregnancy and related services during labor and the postpartum period due to poverty, a lack of awareness, and cultural aspects [11].
One of the strategies used to reduce maternal mortality was timely and high-quality antenatal care [8]. The predictors associated with late initiation of antenatal care varied across studies, including residence, education of the pregnant woman, husband's occupation, parity and being planned, women who had no previous obstetrical complications, and those who lived far away from health care facilities, among others [8, 11, 12]. In order to decrease child and maternal mortality, it is critical to know the time of the first ANC visit for pregnant women and the factors affecting it. Therefore, this study aimed to measure the prevalence and factors associated with late initiation of ANC at Jimma Zone Public Hospitals.
Method and materials
Study setting and design
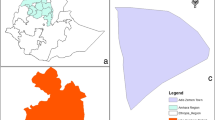
A facility-based cross-sectional study design was carried out from February 1 to 30, 2020 in Jimma zone public hospitals. The zone has eight public hospitals, two private hospitals, and 120 health centers. Of the eight governmental hospitals, one is a referral hospital, three are general hospitals, and four are primary hospitals. The source and study population were all pregnant women who attended selected public hospitals of the ANC clinic and participant who were selected for the study during the data collection period from the sampled hospitals respectively. All pregnant women who were initiated into ANC were included, and who were severely ill and who attended their first ANC visits in other health facilities were excluded.
Sample size determination and sampling technique
A single population proportion formula was used assuming a 95% confidence interval and a 59% prevalence (P) of receiving ANC [15] and a precision of 5% between the sample and the 10% non- response rate, thus a total of 409 pregnant women were required for the study. Simple random sampling techniques were used to select the hospitals. Of the total of eight hospitals found in the Jimma zone, four (Jimma University medical center, Agaro general hospital, Seka primary hospital, and Shenen Gibe general hospital) were selected for the study. Finally, proportional allocation to sample size of each hospital was done, all eligible study participants were selected from each hospital till the allocated sample size was reached by systematic random sampling with kth interval values. (Fig. 1).
Data collection tools and personnel
An interviewer-administered structured questionnaire was adapted through reviewing existing literature which encompasses information related to socio-demographic characteristics, pregnancy-related variables, socio-cultural variables, and predisposing factors [16, 17]. Data were collected by trained data collectors using pretested and structured questioners. The questionnaires were prepared in English, then translated into the languages of both Afaan Oromo (the language spoken by the local residents) and Amharic versions (the official language of Ethiopians), and retranslated back to English by experts to ensure consistency. Face-to-face interviews were used to collect data; gestational age was estimated by asking about the last normal menstrual period, and if respondents were unable to recall their gestation age, further informed consent was obtained to access medical records. Two days of training were given by the principal investigator, which focused on the objective of the study to create a common understanding of the questionnaires. A pretest was conducted among 20 pregnant women in the Limu Genet Primary hospital. After the pretest, the necessary correction was made.
Study variables
Dependent Variable was late initiation of ANC and the independent variables were Socio-demographic variables such as (age, educational status, marital status, and occupation of respondents’, house Income and residence), Socio-cultural variables (religion, family support, advice from significant others, Decision-making and Husbands Educational status), Pregnancy related variables (number of delivery, gravidity, abortion history), Types of pregnancy and means of recognizing pregnancy and Predisposing factors (Knowledge of pregnant women related to ANC visits, and pregnancy related health problem).
Operational definitions
Antenatal care:-is the care given to pregnant women so that they have safe pregnancy and healthy baby.
Late initiation of ANC
Pregnant women were considered late ANC initiated at first visit, when they came to health facility after 16 weeks of gestational age.
Inadequate knowledge
Respondents were categorized as inadequate knowledge about ANC service, if they scored below to the mean knowledge score questions of about ANC service (34), otherwise adequate knowledge.
Planned pregnancy
A pregnancy which is consciously desired and planned by a couple
Data processing and analysis
The completed questionnaire was coded and entered into a data entry template in EPI-DATA version 3.1, then exported to SPSS version 20 for analysis. Descriptive statistics like frequencies, cross-tabulation, graphs, and percentages were employed. The goodness of fit was checked with the Hosmer–Lemeshow test (p = 0.35). Multicollinearity was checked by examining the variance inflation factor. In the bi-variable logistic regression analysis, p-values of less than 0.25 were used to select the candidate variables for multivariable logistic regression analysis. An adjusted odds ratio (AOR) with a 95% CI was used to determine the predictor of the outcome variable independently and to show the strength of an association. A p-value of less than 0.5 were considered as statistically significant.
Result
Socio-demographic characteristics of the study participants
A total of 409(100%) clients were included in the interview, yielding 100% response rate. The mean age was 27 ± 4.22 years. Among the study participant 84.6% of them were married, 10.8% were single, and more than one-third of the respondents, 36.4%, were housewives. The majority of the respondents, 68.45% were urban residents and 70.9% had 1500 ETB (44.12 US dollars) (Table 1).
Timing of first ANC booking of the study participants
The prevalence of pregnant women who has late initiated their first ANC (after 16 week) age was 48%. Among the pregnant women, 21.5% reported the reason for the specific time for the first ANC visit. They did not know the right time and its purpose. Among the participants 25.6% of the respondents who had been to the late initiation of ANC were between the age groups of 25 and 29 years old. Pregnant women attend their first ANC was 44.7% at the recommended time (16 weeks) (Fig. 2).
Knowledge of study participant on ANC Service
Out of 409 respondents, 57% and 39% were to prevent potential health problems and regular medical and nursing care during ANC contact respectively. Pregnant women have adequate knowledge, 139(34%), because they obtain the above mean score: 45.83%. Of the total participants, 270 (66%) respondents have inadequate knowledge because they obtained below the mean score of ANC and the mean score of < 45.83% (Table 2).
Predisposing and socio-cultural factors among pregnant women regarding their health care seeking to attend ANC
One-third of the pregnant women (31.3%) responded that they had ANC follow-up during the preceding pregnancy and about (34.2%) participants were responded as experienced a health problem during the preceding pregnancy. Among the participants 64.8% of them were participated in decision-making process about their health care were decided jointly with husband followed by women alone was 28.1%. (Table 3).
Factors significantly associated with late initiation of antenatal care
Women who reported arriving at the health facility in more than sixty (60) minutes were more than eight times more likely to start ANC recently than those who reported arriving in less than sixty minutes (AOR = 8.26455; 95%CI, 2.929–25.514). Pregnant women who perceived that the current pregnancy was not wanted or unplanned (AOR = 11.290; 95%; CI, 4.109–31.023) were 11 times more likely to start their ANC late compared to those women who wanted the pregnancy. Pregnant women who have inadequate knowledge about ANC service have been (AOR = 4.186; 95%CI, 1.693–10.348) 4 times more likely to start their ANC lately than those who have adequate knowledge. Pregnant mothers who had two children (AOR = 5.964; 95% CI, 1.733–20.526) were six times more likely to begin ANC late than those who had three or more children (Table 4).
Discussion
Our study pointed out that 48% respondents initiated first ANC contact beyond the recommended time. That is almost consistent with the study done in Adigrat Town and Tigray, Ethiopia, (51.8%) [17], and Dilla Town governmental health institutions (50.3%) [18].
The prevalence of pregnant women who initiated late ANC in Jimma Zone (48%) was higher than in Debre Markos town, North West Ethiopia (33.4%) [11].This might be due to socio-cultural differences and difference in awareness creation regarding ANC initiation and difference in accessibility of health facilities. It is also higher than the report of the study in Cameroon (44.0%) [19]. This might be due to the difference in socio-economic level attention and educational background among the study populations in the case of Cameroon.
In the current study the prevalence of late ANC in pregnant women was lower than in Arbaminch town (82.6%) [20], northern Ethiopian pregnant women (59.4%) [15], in the central zone of Tigray Region, Ethiopia(85.67%) [21], and in Gondar Town, North West Ethiopia (64.9%) [22]. This might be due to the difference in the commitment of the providers in awareness-creation since the facilities are in the same country that is guided by the same minister of health and the availability of alternative hospitals in the town. It also lower than in South Africa (51%) [2] and Malaysia (56.2%) [16]. It might due to difference in research conducted time and using of updated guidelines.
Pregnant women who are educated are 75% more likely to have started ANC early compared to those who cannot read and write, and pregnant women who have a college diploma or higher are 85% more likely to have started ANC early compared to those who cannot read and write. This finding was consistent with the report of the study conducted in Dilla town governmental health institutions, illiteracy [18], Addis Ababa, Ethiopia, to eighth grade or below [13] and Debre Markos town, North West Ethiopia had, no formal education [11]. The studies found that higher levels of education of the mothers were less associated with late ANC initiation. This is probably due to the fact that education allows mothers to develop greater confidence to make better choices and to make decisions regarding their health as well as their children's. It is also more likely that educated women demand higher quality service and pay more attention to their health to ensure better health for themselves.
Pregnant women with an unplanned pregnancy (AOR = 11.290; 95%CI, 4.109–31.023) were 11.3 times more likely to start their ANC late compared to those women with planned pregnancies. It is consistent with the study conducted in Arba Minch Town and Arba Minch District, Gamo Gofa Zone, South Ethiopia with unplanned pregnancy [19], in Dilla town governmental health institutions, unplanned pregnancy [18], Debre Markos town [11] and Addis Ababa [13]. It is also consistent with the study conducted in Malaysia with unplanned pregnancy [16] and in South Africa unplanned pregnancy [2].
Women who reported arriving at the health facility in more than sixty (60) minutes were 8.28 times more likely to start ANC early than those who reported arriving in less than sixty (60) minutes. This finding was consistent with the report of study results conducted in Malaysia [15] and Cameroon [19].
Women with inadequate knowledge were four times less likely to begin ANC early than those with adequate knowledge. This finding was consistent with the report of study results conducted in the central zone of the Tigray Region, Ethiopia [21], and northern Ethiopian pregnant women [22]. Report of study conducted in Mekelle City [23] were also in line with result of study.
Pregnant women who had two children were six times more likely to begin ANC late than those who had three or more children. It is consistent with the report of study results conducted in Malaysia [16].
Limitations of the study
The study only considers pregnant women attending public hospitals. As a result, a significant number of pregnant women who attended private health institutions and not visited health facility were overlooked. There is recall bias related to their gestational age, and we have tried to reduce it by asking about some memorable national holidays and reviewing their medical records information like ultrasound investigation.
Conclusion
In the study area, late antenatal care initiation is a still high and serious public health issue. Educational status, unplanned pregnancy, time taken to get to a health facility, and inadequate knowledge of ANC services were affect the outcome variable. As a result, health care workers can provide ongoing health education on the need of starting antenatal care visits early to avoid unfavorable pregnancy outcomes. The hospital managers and the zonal health office should work together to raise knowledge about the advantages of starting ANC as soon as possible for both the mother and the fetus by considering the identified factor. Making the service more accessible to mothers who must travel long distances is also preferable.
Availability of data and materials
Data will be available upon request from the corresponding author.
Abbreviations
- ANC:
-
Antenatal care
- CI:
-
Confidence Interval
- EDHS:
-
Ethiopian demographic Health survey
- WHO:
-
World Health Organization
- USD:
-
USA Dollar
References
WHO. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience : Summary Highlights and Key Messages from the World Health Organization ’ s 2016 Global Recommendations for Routine Antenatal Care. 2018;10(January):1–10.
Ebonwu J, Mumbauer A, Uys M, Wainberg ML, Medina- AWainberg ML, Medina A. Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa : A cross-sectional study. PLoS One. 2018;13(3):e0191903. https://doi.org/10.1371/journal.pone.0191903.
STATISTICS WH. Health-related Millennium Development Goals. 2015;
Ethiopia FDR of, Health M of. Health Sector Development Programme IV 2010/11 – 2014/15. 2014;(October 2010).
EDHS. Ethiopian Demographic Health Survey. 2016.
Ethiopia FDR of, Health M of. Antenatal Care, Part 1 Blended Learning Module for the Health Extension Programme.
Agency CS, Ababa A. Ethiopia Mini Demographic and Health Survey. 2014;(August).
Tesfaye G, Loxton D, Chojenta C, Semahegn A, Smith R. Delayed initiation of antenatal care and associated factors in Ethiopia : a systematic review and meta-analysis. Reproductive Health; 2017;
Carroli G, Villar J, Piaggio G, Khan-neelofur D, Gülmezoglu M, Mugford M, et al. WHO systematic review of randomised controlled trials of routine antenatal care. 2001;357:1565–70.
WHO. 2016 WHO Antenatal Care Guidelines Malaria in Pregnancy Frequently Asked Questions ( FAQ ). 2018;(March):1–6.
Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos. BMC Pregnancy and Childbirth; 2018;1–8.
Tola W, Negash E, Sileshi T, Id NW. Late initiation of antenatal care and associated factors among pregnant women attending antenatal clinic of Ilu Ababor Zone , southwest Ethiopia : A cross-sectional study. 2021;1–11.
Gebrekidan K, Worku A. Factors associated with late ANC initiation among pregnant women in select public health centers of Addis Ababa , Ethiopia : unmatched case – control study design. 2017;223–30.
Belayneh T, Adefris M, Andargie G. Previous early antenatal service utilization improves timely booking: Cross-sectional study at university of Gondar Hospital, northwest Ethiopia. J Pregnancy. 2014;2014.
Wolde F, Mulaw Z, Zena T, Biadgo B, Limenih MA. Determinants of late initiation for antenatal care follow up : the case of northern Ethiopian pregnant women. BMC Res Notes. BioMed Central; 2018;1–7.
Aung TZ, Oo WM, Khaing W, Lwin N, Dar HT. Late initiation of antenatal care and its determinants: a hospital-based cross-sectional study. Int J Community Med Public Heal. 2016; 3(4):900–5.21.
Lerebo W, Kidanu A, Tsadik M. Magnitude and Associated Factors of Late Booking for Antenatal Care in Public Health Centers of Adigrat Town, Tigray. Ethiopia Clinics Mother Child Health. 2015;12:171. https://doi.org/10.4172/2090-7214.1000171.
Girum T. Alternative & Integrative Medicine Assessment of Timing of First Antenatal Care Visit and Associated Factors Among Pregnant Women Attending Antenatal Care in Dilla Town Governmental. Institutions, Heal. 2016;5(3).
Tolefac PN, Halle-ekane GE, Agbor VN, Sama CB, Ngwasiri C, Tebeu PM. Why do pregnant women present late for their first antenatal care consultation in Cameroon ? Maternal Health, Neonatology and Perinatology; 2017;1–6.
Gebremeskel F, Dibaba Y, Admassu B. Timing of First Antenatal Care Attendance and Associated Factors among Pregnant Women in Arba Minch Town and Arba Minch District , Gamo Gofa Zone , South Ethiopia. 2015;2015.
Grum T, Brhane E. Magnitude and factors associated with late antenatal care booking on first visit among pregnant women in public health centers in central zone of Tigray Region , Ethiopia : A cross sectional study. 2018;1–9.
Gudayu TW, Woldeyohannes SM, Abdo AA. Timing and factors associated with first antenatal care booking among pregnant mothers in Gondar Town; North West Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):287.
Fisseha G, Miruts G, Tekie M, Michael AW, Yemane D, Gerezigiher T. Predictors of Timing of First Antenatal Care Booking at Public Health Centers in Mekelle City. Northern Ethiopia. 2015;3(3):55–60.
Acknowledgements
We would like to thank Jimma University of institute of health for supporting this project. We also thank the study participants, data collectors and those who had contribution to this study.
Funding
This work was supported by Jimma University.
Author information
Authors and Affiliations
Contributions
N.G and F.T were involved in designing the study, drafting the proposal, data collection, analysis, and writing up the first draft of the manuscript. K.F and D.A Reviewed and reanalyzed the data set and reviewed the manuscript and references to get the final version. All authors agreed with the final format of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted after obtaining ethical clearance from Jimma University, Institute of Health (IRB reference number were IHRPGD/a/2019, Research Ethics Committee and letter of support from town health office. Formal Permission paper was given to health facilities and responsible persons in each health institution accordingly. Written informed consent was obtained from all participates prior to their participation with informing the purpose, benefits, confidentiality of the information, and voluntary nature of participation in the study. Name and other personal identifiers were not recorded to maintain confidentiality. “All the protocol was performed in accordance with the relevant guideline and regulation.”
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tadele, F., Getachew, N., Fentie, K. et al. Late initiation of antenatal care and associated factors among pregnant women in Jimma Zone Public Hospitals, Southwest Ethiopia, 2020. BMC Health Serv Res 22, 632 (2022). https://doi.org/10.1186/s12913-022-08055-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08055-6