Abstract
Background
Physical rehabilitation is often prescribed immediately following a neurological event or a neurological diagnosis. However, many individuals require physical rehabilitation after hospital discharge. The purpose of this scoping review was to determine the amount of physical rehabilitation that individuals living in the community with neurological conditions receive to understand current global practices and assess gaps in research and service use.
Methods
This scoping review included observational studies that 1) involved adults living with a neurological condition, and 2) quantified the amount of rehabilitation being received in the community or outpatient hospital setting. Only literature published in English was considered. MEDLINE, EMBASE, AMED, CINAHL, Cochrane Library, and PEDro databases were searched from inception. Two independent reviewers screened titles and abstracts, followed by full texts, and data extraction. Mean annual hours of rehabilitation was estimated based on the amount of rehabilitation reported in the included studies.
Results
Overall, 18 studies were included after screen 14,698 articles. The estimated mean annual hours of rehabilitation varied greatly (4.9 to 155.1 h), with individuals with spinal cord injury and stroke receiving the greatest number of hours. Participants typically received more physical therapy than occupational therapy (difference range: 1 to 22 h/year). Lastly, only one study included individuals with progressive neurological conditions, highlighting a research gap.
Discussion
The amount of rehabilitation received by individuals with neurological conditions living in the community varies greatly. With such a wide range of time spent in rehabilitation, it is likely that the amount of rehabilitation being received by most individuals in the community is insufficient to improve function and quality of life. Future work should identify the barriers to accessing rehabilitation resources in the community and how much rehabilitation is needed to observe functional improvements.
Similar content being viewed by others
Background
Physical rehabilitation, such as physical and occupation therapy, is commonly prescribed following the diagnosis of a neurological condition or the occurrence of a neurological event. The goal of physical rehabilitation is to optimize physical functioning so people can continue to complete tasks that are important to them, as independently and safety as possible. More specifically, physical therapy typically views movement on a continuum while considering the physical, pathological, social, and psychological aspects [1]. Common therapeutic activities include transfer and gait training, strength exercises, and balance training [2]. Conversely, occupational therapy focuses on improving independence with activities of daily living using an approach that incorporates both physical and mental health [3]. The practice of occupational therapy involves tasks such as prescribing adaptive equipment, optimizing activities of daily living, and practicing fine motor tasks. Common tasks performed in occupational therapy may include problem solving, reaching to grasp a cup, and minimizing stimulation in public spaces. Despite approximately 0.5–2 h per day being spent on physical rehabilitation during inpatient rehabilitation [4,5,6], persistent physical impairments in neurological populations are often present long-term such as spasticity, pain, muscle weakness, and fatigue [7,8,9]. Accordingly, many individuals require ongoing physical rehabilitation after discharge from inpatient rehabilitation hospitals.
Quality of life – which may be one of the most important self-perceived measure of function – has been shown to improve with access to physical rehabilitation in the community setting [10]. The community setting can be operationalized as visiting an outpatient clinic, a community centre, or being visited in-home by a healthcare practitioner. Outpatient clinic use is more common than receiving services in-home [11]. Betterment in many of these functional domains can impact quality of life [12, 13], therefore highlighting the benefits of physical rehabilitation for individuals living with neurological conditions in the community. Outpatient programs have been shown to results in a manifold of improvements to functional independence, balance, and mobility [14,15,16].
Individuals with long-term neurological conditions have qualitatively reported that their physical rehabilitative needs are not met [17]. However, to our knowledge, no review has evaluated how much time is spent in physical rehabilitation following chronic neurological impairment, to better understand this gap in care quantitatively. It is important to understand current global practices to first gauge the current norms in the field of neurological rehabilitation. By assessing this data, we can then work towards determining the optimal time needed to improve physical function and provide recommendations for insurance companies or hospitals and direct future research studies and programs. Therefore, the purpose of this scoping review was to identify and describe studies that characterize the amount of outpatient or community physical rehabilitation received by those living with neurological conditions. The goal of this work is to inform future guidelines for community rehabilitation and provide a baseline amount of therapy for interventions targeting these populations.
Methods
Search strategy
This scoping review was conducted according to the guidelines presented in the PRISMA Extension for Scoping Reviews [18]. A protocol paper has been previously submitted for the present scoping review (Saumur et al., submitted). In brief, following a search of review registries to determine no similar review is currently in progress, an initial search strategy was developed in MEDLINE (Additional file 1) with the assistance of a research librarian surrounding the concepts of ‘Rehabilitation’, ‘Neurological Populations’, and ‘Time Factors’. The search strategy was then translated for application in Ovid Embase, Ovid Allied and Complementary Medicine (AMED), EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus. The searches for journal articles in all databases were conducted on December 17th, 2020.
Study selection & screening
Articles were uploaded to Covidence (Covidence, Victoria, Australia) where they were initially deduplicated. Articles were then screened for eligibility. Articles were included if they met the following criteria: 1) adults 18 years of age or older; 2) living in the community with a neurological condition defined as traumatic brain injury, multiple sclerosis, spinal cord injury, stroke, and Parkinson’s disease [19, 20]; 3) used an observational study design, 4) reported the amount of rehabilitation received; 5) published in English; and 6) have abstract and full text available in a peer-reviewed journal. Experimental studies, systematic/scoping reviews, and gray literature such as newspaper articles, reports, and dissertations were not included.
Two reviewers independently reviewed all deduplicated titles and abstracts to determine which articles to include for full text screening. If consensus could not be achieved between the two reviewers, the other team members were consulted to determine the article’s eligibility. During full text screening, two reviewers independently assessed the potential articles for their eligibility. If the article was not included, a reason was provided based on the inclusion criteria. The same procedures as title and abstract screening were used in the event of reviewer disagreement. Once full texts were selected for study inclusion, backwards citation tracking was conducted to consult the references of included studies for additional articles.
Data extraction & analysis
Following full text screening, data extraction was performed based on a standardized, piloted extraction form developed by the research team. Data extracted included: year and country published in; study design and objectives; population and patient demographics included in the article; method of data collection; time spent in rehabilitation; and type of rehabilitation. The two primary reviewers independently extracted the data for each study and an additional team member cross-referenced the two data extraction forms with the included journal article. The collected data were then summarized using descriptive statistics (mean and standard deviation or median and interquartile range, accordingly) and presented in tabular and graphical forms. Annual time spent in rehabilitation was estimated in hours for each study based on the information provided. One hour was allocated for each session in the event that number of sessions was reported based on previous research, which has shown that 1 session is approximately 1h on average [21].
Results
Included studies
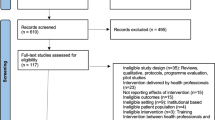
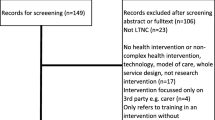
A PRISMA diagram outlining the screening process can be found in Fig. 1. In brief, following deduplication, 14,698 articles were initially assessed for eligibility. Following title and abstract screening, 88 articles were selected for full text review. Of these 88 articles, 18 were included in this review. The main reasons for articles being excluded were due to the outcomes reported (58.6%, e.g., no mention of time spent in rehabilitation); study design (12.9%, e.g., experimental design); and poster or conference abstract (10.0%).
Study Demographics
Table 1 outlines the main objectives, study design, and participant demographics of the included studies. Most studies were conducted in the United States (n = 6) or the United Kingdom (n = 4). No research was found prior to 1990 in the literature, with an incremental increase in the presence of these studies over the last three decades (Fig. 2).
The most commonly used data collection tools to evaluate the amount of time in physical rehabilitation were questionnaires, interviews, and surveys (n = 6); medical charts or electronic patient record (n = 5); health claims data (n = 3). Some studies used a variety of methods to gather this information (n = 2), or custom data collection sheets (n = 2) were also implemented in some studies.
Stroke was by far the most common condition studied (n = 13), with SCI (n = 2), TBI (n = 2), and multiple long-term neurological conditions (n = 1) also being evaluated. Chronicity of the condition varied from immediately following hospital discharge until 40 years post-injury. Half of the studies distinguished between occupational and physical therapy (n = 9), and the rest of the studies grouped all types of physical rehabilitation (n = 9).
Time spent in rehabilitation
The estimated mean annual hours spent in rehabilitation ranged from 4.9 h in mild TBI [22] to 155.1 h in chronic stroke [23] (Table 2). On average, SCI and stroke received the most hours of rehabilitation (Fig. 3). In general, participants received more physical therapy than occupational therapy, regardless of condition (9 of 10 studies; Fig. 4). Regarding location of services, two of four studies found that patients utilized more in-home services compared to outpatient services [24, 25], whereas two studies found that more time was spent in outpatient services [23, 26].
Estimated mean annual hours reported for each physical rehabilitation service, separated by neurological condition. Misc Neuro included stroke, traumatic brain injury, other acquired brain injury, spinal cord injury, peripheral neuropathy, and progressive long-term neurological conditions [26]
Discussion
The purpose of this study was to identify and describe studies that characterize the amount of outpatient or community physical rehabilitation received by those living with neurological conditions. We found that the amount of physical rehabilitation received by individuals with neurological conditions living in the community varied greatly. Those with spinal cord injury and stroke received a greater number of hours on average regardless of service and the majority of studies were conducted within the first year following injury. In general, however, more time was spent in physical therapy than occupational therapy.
The first main finding in this study was that individuals who experienced a spinal cord injury or stroke received a greater number of rehabilitation hours while living in the community compared to other populations. Reasons why these populations would receive more rehabilitation than other populations, such as traumatic brain injury are unclear; however, it does not appear to be linked with severity of injury as Homaifer and colleagues (2009) reported that the amount of rehabilitation received by those with mild traumatic brain injury was greater than those with moderate/severe injury beyond 10 years post-injury [22]. These findings may suggest that severity of impairment is not a key factor in service use for those living in the community; however, studies that directly compare functional severity with service use are needed.
A second main finding of this review was that the vast majority of studies reported increased hours spent in physical therapy compared to occupational therapy (ranging between 1 and 22 annual hours difference in those studies which reported greater physical therapy use). There are a few potential reasons for the finding. Firstly, there are approximately 37% more registered physical therapists than occupational therapists [27]. The availability of staff and resources likely explains this difference in service utilization in those with neurological impairments. In addition, there is some overlap in the roles of occupational and physical therapists [28], despite these roles being functionally quite distinct. For example, both professions may use strengthening exercises to improve physical function of the hand; however, the goal to implement these exercises may different (i.e., physical therapy – improve hand strength so can hold onto a walker; occupational therapy – improve hand strength so can dress oneself) [29]. However, many individuals may not know this difference between roles, and individuals in the community may be inclined to receive whichever service is readily available to them, regardless of the goal. It is important that individuals understand the difference between these types of physical rehabilitation so that their appropriate needs can be met. Indeed, therapists have reported factors such as lack of professional role clarity and restricted multidisciplinary team working as key barriers to providing community-based rehabilitation [30]. Taken together, this research highlights the importance of role clarity, accessibility, and perceived value as key factors influencing the amount of rehabilitation individuals participate in in the community.
With respect to the location of services, results were split with half of the studies finding patients utilized more in-home services compared to outpatient services [24, 25], whereas half found that more time was spent in outpatient services [23, 26]. This contrasts work by Godwin et al., (2011) which has shown that time spent in outpatient rehabilitation is more than three times that of in-home services. It is worth noting however, that the aforementioned study calculated rehabilitation utilization based on healthcare costs which likely impacted the findings. Furthermore, the utilization of resources available in the community likely differs by region and depends on features related to access such as distance to the nearest hospital or the equipment required. Therefore, while the location of rehabilitation used in the community may vary, a one-size-all approach should not be used when comparing patient needs and the resources available.
Despite our findings demonstrating that people with neurological diagnoses commonly do receive some physical rehabilitation after discharge from hospital inpatient units, the amount of rehabilitation received is likely insufficient. Research indicates many people continue to have disability long-term following diagnosis, and evidence shows that failure to access occupational and physical therapy is associated with continued issues following a brain injury [31, 32]. Furthermore, the evidence is clear that ongoing rehabilitation services do help long term [15]. However, patients frequently discuss short-term barriers to community rehabilitation such as problems ambulating and the inconvenience of attending sessions as well as long-term barriers related to finances and lack of interest or perceived need [33]. We also acknowledge that presently, access to these resources is limited. For example, in the United States, fewer than 10% of individuals living in the community with a stroke access occupational and physical therapy [34]. Thus, understanding the barriers to accessing the resources and how much rehabilitation is needed to observe functional improvements is critical.
Where do we go from here?
The present scoping review highlighted various gaps in the literature pertaining to physical rehabilitation use in those with neurological conditions living in the community. Firstly, while we sought out to study individuals with discrete and progressive neurological conditions, we did not identify any studies on those with a degenerative condition with the exception of Jackson et al., (2014) which included various neurological conditions including 21 subjects (5%) with progressive long-term neurological conditions. It is important to note that the focus of rehabilitation differs between these two disease types. Rehabilitation for degenerative neurological disorders aims to manage the condition and slow the decline of physical function by developing compensatory strategies and increasing support over time [35]. Conversely, after a traumatic or ischemic event, rehabilitation focuses on reducing disability following the acute event to pre-injury functional capacities [36, 37]. Since treatment goals may differ between these groups, access to resources and tracking of these populations likely also differs. This can be appreciated by the lack of research pertaining to those with degenerative neurological conditions living in the community.
Furthermore, while studies did not track service use over time within the same cohort of subjects, it will be important for researchers to track service use longitudinally in order to further understand these trends and factors that affect them. As most of the studies included in this review focused on the first year following injury, there remains a large gap in services utilized over the long term in these populations. Determining the optimal timing and length of treatment is important in both progressive and non-progressive conditions as individuals have long-term needs related to improving or maintaining independence and slowing the rate of functional decline [35,36,37]. In the present study, the wide range of annual time spent in rehabilitation even within the same population, setting, and country, points to a lack of standardization and evidence-based practice in terms of the amount of rehabilitation received once discharged from the hospital. A goal of future research should be to determine the optimal amount of time needed to maximize the physical benefits of rehabilitation so that standards can be established. Notably, this determination of optimal usage of services can only be established through linking service use to functional outcomes. However, these findings provide the foundation for future development of clinical practice guidelines and can inform policies surrounding rehabilitation services in outpatient or community settings.
Limitations
This review is not without its limitations. Firstly, the calculation of time spent in rehabilitation was estimated based on the number of sessions when time in minutes or hours was not provided. Many factors may influence the length of therapy sessions, and these may vary over time. However, the purpose of these calculations was to provide a broad picture of the landscape of community rehabilitation for those with neurological impairments. In addition, due to the small number of studies and only three studies including subjects more than one year following injury [2, 22, 38], disease chronicity was not considered which likely impacts rehabilitation time. Furthermore, articles were limited to those published in English and therefore we may have missed some studies published in different languages from other countries that could have been useful in gathering a more global perspective of rehabilitation use. This review also did not include experimental research, which may limit understanding of physical rehabilitation service programs that are in development, however the aim was to describe utilization of current services. Several included articles used data collection tools such as surveys and interviews, which rely on self-reporting and may be subject to recall bias. In addition, there was a lack of details regarding the variables reported within the included studies such as: number of therapists, health care delivery model, funding type, and accessibility; these features would greatly strengthen our ability to discuss the physical rehabilitation context of the included studies. Lastly, while this review sought to explore time spent in rehabilitation in both progressive and non-progressive neurological disease, there was limited research available, particularly in progressive groups. The treatment and access to resources likely differs between these patient groups and warrants further research.
Conclusions
This scoping review found that the amount of physical rehabilitation received by individuals with neurological conditions living in the community varied greatly, with individuals who experienced a spinal cord injury or stroke receiving the greatest amount of care. In addition, more time is spent on average in physical therapy compared to occupational therapy in the community. These findings highlight the heterogeneity of physical rehabilitation received by individuals with a neurological condition and point to various avenues for future research including studying service use over time, the impact of community rehabilitation on functional outcomes and quality of life, and rehabilitation use in individuals with progressive neurological conditions.
Availability of data and materials
Not applicable.
References
Cott CA, Finch E, Gasner D, Yoshida K, Thomas SG, Verrier MC. The movement continuum theory of physical therapy. Physiother Can. 1995;47:87–95.
Green J, Forster A, Young J. A survey of community physiotherapy provision after 1 year post-stroke. Int J Ther Rehabil. 1999;6:216–21.
Gardiner P, Macgregor L, Carson A, Stone J. Occupational therapy for functional neurological disorders: A scoping review and agenda for research. CNS Spectr. 2018;23:205–12.
Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke. 2004;35:1005–9.
Whiteneck G, Gassaway J, Dijkers M, Backus D, Charlifue S, Chen D, et al. The SCIRehab project: treatment time spent in SCI rehabilitation. Inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med. 2011;34:133–48.
Latham NK, Jette DU, Slavin M, Richards LG, Procino A, Smout RJ, et al. Physical therapy during stroke rehabilitation for people with different walking abilities. Arch Phys Med Rehabil. 2005;86:41–50.
Turner-Stokes L, Sykes N, Silber E. Long-term neurological conditions: Management at the interface between neurology, rehabilitation and palliative care. Clin Med J R Coll Physicians London. 2008;8:186–91.
Sezer N, Akkuş S, Uğurlu FG. Chronic complications of spinal cord injury. World J Orthop. 2015;6:24–33.
Bustamante A, García-Berrocoso T, Rodriguez N, Llombart V, Ribó M, Molina C, et al. Ischemic stroke outcome: A review of the influence of post-stroke complications within the different scenarios of stroke care. Eur J Intern Med. 2016;29:9–21.
Di Fabio RP, Choi T, Soderberg J, Hansen CR. Health-related quality of life for patients with progressive multiple sclerosis: Influence of rehabilitation. Phys Ther. 1997;77:1704–16.
Godwin KM, Wasserman J, Ostwald SK. Cost associated with stroke: Outpatient rehabilitative services and medication. Top Stroke Rehabil. 2011;18:676–84.
Fagerström C, Borglin G. Mobility, functional ability and health-related quality of life among people of 60 years or older Aging Clinical and Experimental Research. Aging Clin Exp Res. 2010;22:387–94.
Kim K, Kim YM, Kim EK. Correlation between the activities of daily living of stroke patients in a community setting and their quality of life. J Phys Ther Sci. 2014;26:417–9.
Werner R, Kessler S. Effectiveness of an intensive outpatient rehabilitation program for postacute stroke patients. Am J Phys Med Rehabil. 1996;75:114–20.
Teasell R, Mehta S, Pereira S, McIntyre A, Janzen S, Allen L, et al. Time to rethink long-term rehabilitation management of stroke patients. Top Stroke Rehabil. 2012;19:457–62.
Harkema SJ, Schmidt-Read M, Lorenz DJ, Edgerton VR, Behrman AL. Balance and ambulation improvements in individuals with chronic incomplete spinal cord injury using locomotor trainingbased rehabilitation. Arch Phys Med Rehabil. 2012;93:1508–17.
Foster M, Allen S, Fleming J. Unmet health and rehabilitation needs of people with long-term neurological conditions in Queensland. Australia Heal Soc Care Community. 2015;23:292–303.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73.
Jackson K, Hamilton S, Jones S, Barr S. Patient reported experiences of using community rehabilitation and/or support services whilst living with a long-term neurological condition: a qualitative systematic review and meta-aggregation. Disabil Rehabil Taylor & Francis. 2019;41:2731–49.
World Health Organization. Neurological Disorders: Public Health Challenges. 2006.
Kaur G, English C, Hillier S. How physically active are people with stroke in physiotherapy sessions aimed at improving motor function? A systematic review. Stroke Res Treat. 2012;2012.
Homaifar BY, Harwood JE, Wagner TH, Brenner LA. Description of outpatient utilization and costs in group of veterans with traumatic brain injury. J Rehabil Res Dev. 2009;46:1003–10.
Gladman JRF, Lomas S, Lincoln NB. Provision of physiotherapy and occupational therapy in outpatient departments and day hospitals for stroke patients in Nottingham. Disabil Rehabil. 1991;13:38–41.
Freburger JK, Li D, Johnson AM, Fraher EP. Physical and Occupational Therapy From the Acute to Community Setting After Stroke: Predictors of Use, Continuity of Care, and Timeliness of Care. Arch Phys Med Rehabil. 2018;99:1077-1089.e7.
Freburger JK, Li D, Fraher EP. Community Use of Physical and Occupational Therapy After Stroke and Risk of Hospital Readmission. Arch Phys Med Rehabil. 2018;99:26-34.e5.
Jackson D, McCrone P, Mosweu I, Siegert R, Turner-Stokes L. Service use and costs for people with long-term neurological conditions in the first year following discharge from in-patient neuro-rehabilitation: A longitudinal cohort study. PLoS One. 2014;9.
Canadian Institute for Health Information. Health Workforce Database [Internet]. 2020 [cited 2021 Sep 23]. p. 1–35. Available from: https://www.cihi.ca/en/health-workforce
Booth J, Hewison A. Role overlap between occupational therapy and physiotherapy during in-patient stroke rehabilitation: An exploratory study. J Interprof Care. 2002;16:31–40.
Steultjens EMJ, Dekker J, Bouter LM, Van de Nes JCM, Cup EHC, Van den Ende CHM. Occupational therapy for stroke patients: A systematic review. Stroke. 2003;34:676–86.
Nicholson C, Francis J, Nielsen G, Lorencatto F. Barriers and enablers to providing community-based occupational therapy to people with functional neurological disorder: An interview study with occupational therapists in the United Kingdom. Br J Occup Ther. 2021;8–11.
Doig E, Fleming J, Tooth L. Patterns of community integration 2–5 years post-discharge from brain injury rehabilitation. Brain Inj. 2001;15:747–62.
Pettersen R, Dahl T, Wyller TB. Prediction of long-term functional outcome after stroke rehabilitation. Clin Rehabil. 2002;16:149–59.
Chen AWL, Koh YT on., Leong SWM, Ng LWY, Lee PSY, Koh GCH. Post community hospital discharge rehabilitation attendance: Self-perceived barriers and participation over time. Ann Acad Med Singapore. 2014;43:136–44.
Cook C, Stickley L, Ramey K, Knotts VJ. A variables associated with occupational and physical therapy stroke rehabilitation utilization and outcomes. J Allied Health. 2005;34:3–10.
Cheng YY, Hsieh WL, Kao CL, Chan RC. Principles of rehabilitation for common chronic neurologic diseases in the elderly. J Clin Gerontol Geriatr. 2012;3:5–13.
Nas K, Yazmalar L, Şah V, Aydin A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6:8–16.
Brewer L, Horgan F, Hickey A, Williams D. Stroke rehabilitation: Recent advances and future therapies. QJM. 2013;106:11–25.
Hodgkinson A, Veerabangsa A, Drane D, McCluskey A. Service utilization following traumatic brain injury. J Head Trauma Rehabil. 2000;15:1208–26.
Backus D, Gassaway J, Smout RJ, Hsieh CH, Heinemann AW, Dejong G, et al. Relation between inpatient and postdischarge services and outcomes 1 year postinjury in people with traumatic spinal cord injury. Arch Phys Med Rehabil Elsevier Ltd. 2013;94:S165–74.
Geddes JML, Chamberlain MA. Home-based rehabilitation for people with stroke: A comparative study of six community services providing co-ordinated, multidisciplinary treatment. Clin Rehabil. 2001;15:589–99.
Grimley RS, Rosbergen ICM, Gustafsson L, Horton E, Green T, Cadigan G, et al. Dose and setting of rehabilitation received after stroke in Queensland, Australia: a prospective cohort study. Clin Rehabil. 2020;34:812–23.
Huang HC, Chung KC, Lai DC, Sung SF. The Impact of Timing and Dose of Rehabilitation Delivery on Functional Recovery of Stroke Patients. J Chinese Med Assoc Elsevier. 2009;72:257–64.
Jalayondeja C, Kaewkungwal J, Sullivan PE, Nidhinandana S, Pichaiyongwongdee S, Jareinpituk S. Factors related to community participation by stroke victims six month post-stroke. Southeast Asian J Trop Med Public Health. 2011;42:1005–13.
Minet LR, Peterson E, von Koch L, Ytterberg C. Healthcare Utilization After Stroke: A 1-Year Prospective Study. J Am Med Dir Assoc. 2020;21:1684–8.
Ngo L, Latham NK, Jette AM, Soukup J, Iezzoni LI. Use of physical and occupational therapy by medicare beneficiaries within five conditions 1994–2001. Am J Phys Med Rehabil. 2009;88:308–21.
Pucciarelli G, Ausili D, Rebora P, Arisido MW, Simeone S, Alvaro R, et al. Formal and informal care after stroke: A longitudinal analysis of survivors’ post rehabilitation hospital discharge. J Adv Nurs. 2019;75:2495–505.
Rhoda A, Mpofu R, DeWeerdt W. The rehabilitation of stroke patients at community health centres in the Western Cape. South African J Physiother. 2009;65:1–6.
Thompson S, Ranta A, Porter K, Bondi N. How much rehabilitation are our patients with stroke receiving? N Z Med J. 2019;132:49–55.
Whiteneck GG, Gassaway J, Dijkers MP, Lammertse DP, Hammond F, Heinemann AW, et al. Inpatient and postdischarge rehabilitation services provided in the first year after spinal cord injury: Findings from the SCIRehab study. Arch Phys Med Rehabil. 2011;92:361–8.
Acknowledgements
The authors would like to thank Maren Goodman for assistance with developing the search strategy.
Funding
This study was unfunded.
Author information
Authors and Affiliations
Contributions
TMS, SG, YX, and JU made substantial contributions to the conception of the work. JU ran the searches, all authors were involved in screening articles. TMS analyzed data. TMS and JU drafted the manuscript and SG and YX made substantial revisions. All authors have approved the submitted version (and any substantially modified version that involves the author's contribution to the study) and have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Medline (OVID) Search Strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saumur, T.M., Gregor, S., Xiong, Y. et al. Quantifying the amount of physical rehabilitation received by individuals living with neurological conditions in the community: a scoping review. BMC Health Serv Res 22, 349 (2022). https://doi.org/10.1186/s12913-022-07754-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07754-4