Abstract
Background
The Hospital Readmissions Reduction Program (HRRP), established by the Centers for Medicare and Medicaid Services (CMS) in March 2010, introduced payment-reduction penalties on acute care hospitals with higher-than-expected readmission rates for acute myocardial infarction (AMI), heart failure, and pneumonia. There is concern that hospitals serving large numbers of low-income and uninsured patients (safety-net hospitals) are at greater risk of higher readmissions and penalties, often due to factors that are likely outside the hospital’s control. Using publicly reported data, we compared the readmissions performance and penalty experience among safety-net and non-safety-net hospitals.
Methods
We used nationwide hospital level data for 2009-2016 from the Centers for Medicare and Medicaid Services (CMS) Hospital Compare program, CMS Final Impact Rule, and the American Hospital Association Annual Survey. We identified as safety-net hospitals the top quartile of hospitals in terms of the proportion of patients receiving income-based public benefits. Using a quasi-experimental difference-in-differences approach based on the comparison of pre- vs. post-HRRP changes in (risk-adjusted) 30-day readmission rate in safety-net and non-safety-net hospitals, we estimated the change in readmissions rate associated with HRRP. We also compared the penalty frequency among safety-net and non-safety-net hospitals.
Results
Our study cohort included 1915 hospitals, of which 479 were safety-net hospitals. At baseline (2009), safety-net hospitals had a slightly higher readmission rate compared to non-safety net hospitals for all three conditions: AMI, 20.3% vs. 19.8% (p value< 0.001); heart failure, 25.2% vs. 24.2% (p-value< 0.001); pneumonia, 18.7% vs. 18.1% (p-value< 0.001). Beginning in 2012, readmission rates declined similarly in both hospital groups for all three cohorts. Based on difference-in-differences analysis, HRRP was associated with similar change in the readmissions rate in safety-net and non-safety-net hospitals for AMI and heart failure. For the pneumonia cohort, we found a larger reduction (0.23%; p < 0.001) in safety-net hospitals. The frequency of readmissions penalty was higher among safety-net hospitals. The proportion of hospitals penalized during all four post-HRRP years was 72% among safety-net and 59% among non-safety-net hospitals.
Conclusions
Our results lend support to the concerns of disproportionately higher risk of performance-based penalty on safety-net hospitals.
Similar content being viewed by others
The Hospital Readmissions Reduction Program (HRRP), enacted as part of the 2010 Affordable Care Act, aimed to reduce preventable hospital readmissions as a way to lower inpatient costs without compromising quality of care [1, 2]. Under HRRP, the Centers for Medicare and Medicaid Services (CMS), was mandated to review Medicare fee-for-service (FFS) hospitals paid under the Medicare Inpatient Prospective Payment System (IPPS) and impose financial penalties on the hospitals that exhibited higher-than-expected 30-day readmission rate for specified clinical conditions [3]. Financial penalties, which took the form of a percentage reduction in Medicare payments for a hospital’s inpatient care services, were levied on IPPS hospitals for excess readmissions starting October 1, 2012 (fiscal year (FY) 2013), with up to 1% of qualifying hospitals’ total Medicare reimbursements being withheld in the first year; the maximum penalty increased to 3% in FY 2015 and has been capped at this level [1].
Many observers have expressed concern about the program since it increases the risk of penalty for hospitals that serve higher proportions of uninsured, low income, and medically vulnerable patients – that is, safety-net hospitals – and therefore could adversely affect the financial viability of the hospitals and the services to the poor and vulnerable patients [4, 5]. Further, risk of penalty for such hospitals may be unduly higher since many factors that are associated with higher risk of readmission – inadequate social supports, low income, low levels of education, residential instability, risk health behaviors – are not included in the risk adjustment model for determining hospital performance [6,7,8,9,10,11,12].
There is a growing literature on assessing the impact of HRRP on the penalty experience and on readmissions. Early studies suggest that safety-net hospitals were penalized at a higher rate and incurred higher penalty under HRRP compared to non-safety-net hospitals [3, 13,14,15]. These studies documenting the penalty experience were limited by single state [14], single year [13] or single measure [15]. On the impact on readmissions performance, studies have varied on methodology and data used, thereby limiting comparability. One study assessed the differential impact on the readmissions rate in safety-net vs. non-safety-net hospitals [16]; however, as the analysis did not include pre-HRRP data, it did not adjust for baseline differences across hospitals. Another study used a hospital-wide readmission measure to compare safety-net vs. non-safety hospitals under HRRP [17]; however, this measure uses different patient cohorts and risk measures than that used by CMS in determining hospital performance [18]. To provide a more comprehensive and authentic assessment of the readmissions and penalty experience, what is needed is a nationally representative sample, with performance data from pre- and post-program periods for the same patient cohorts and using the same risk-adjustment method used by HRRP [1, 19].
In this study, we improved upon prior work by using pre-HRRP data in addition to post-HRRP data and examined whether changes in readmission rates associated with HRRP were different for safety-net vs. non-safety-net hospitals for the three targeted conditions – AMI, heart failure, and pneumonia. Specifically, we compared changes in readmission rates in the post- vs. pre-HRRP period for safety-net hospitals with corresponding changes for non-safety-net hospitals using publicly reported hospital-level data from 2009 to 2016. In addition, we examined multiple penalty measures – share of hospitals penalized, average penalty, and distribution of repeated penalties – aimed at capturing the penalty experience of safety-net vs. non-safety-net hospitals from 2013 to 2016. Although changes are currently under way, whereby CMS will evaluate hospital performance relative to other hospitals with a similar share of dually eligible Medicare and Medicaid patients starting fiscal year (FY) 2019, understanding the impact of the initial years of HRRP on safety-net hospitals informs future interventions target hospital quality [20, 21].
Methods
Data and analysis
We obtained data on hospital readmissions performance (2009-2016) from CMS’ Hospital Compare Program [22] and data on safety-net hospital status (2009) and penalty (2013-2016) from CMS’ Final Impact Rule [23]. In addition, we used the American Hospital Association Annual Survey (2009) to obtain data on hospital characteristics [24]. Our sample universe included all IPPS hospitals over the period 2009-2016, with 2756 such hospitals in 2009 to 2607 in 2016. Non-IPPS hospitals were excluded from the analysis; these included all Maryland hospitals, critical access hospitals, pediatric hospitals, long-term care facilities, rehabilitation hospitals, psychiatric hospitals, and Veterans Affairs hospitals [25]. We also excluded hospitals that did not report 30-day-risk-adjusted readmissions or were not reimbursed through the IPPS during all the study years.
Readmission outcomes
Our analytic data were comprised of longitudinal (annual) observations for the included IPPS hospitals from 2009 to 2016. Our main outcomes were 30-day risk-adjusted readmission rates for the three conditions targeted by HRRP: AMI, heart failure, and pneumonia. For each hospital, the Hospital Compare Program reports 30-day risk-adjusted readmission rates for each cohort in each year, based on eligible admissions in the preceding 3 years and is adjusted for differences between hospitals in patient characteristics, including age, sex, comorbid health conditions, as well as other unobserved, systematic hospital effects [19, 26]. Therefore, the 30-day risk-adjusted readmission rate for 2009 corresponds to data collection period July, 2005-June, 2008 and similarly for the other years (Additional file 1: Table 1). We restricted the sample for the pneumonia cohort to 2009-2015, since CMS’ definition of pneumonia for this measure was modified in 2016 and resulted in a large increase in the number of eligible admissions [19].
Safety-net hospitals
We followed prior studies and used the disproportion share hospital (DSH) index to identify safety-net hospitals. The DSH index is defined as the sum of the proportion of elderly patients who receive Supplemental Security Income (SSI) and the proportion of non-elderly patients who receive Medicaid benefits [27, 28]. We defined the top quartile of hospitals in terms of the DSH index as safety-net hospitals. There is no single universally accepted method for identifying safety-net hospitals, and some of the alternatives that have been used include: Medicaid caseload, uncompensated care burden, and facility characteristics, with each having its own merits [14]. We prefer the DSH index to define safety-net hospitals since it is able to identify poor patients regardless of their age [14, 28]. Nonetheless, in sensitivity analysis we used the share of aggregate inpatient days attributable to Medicaid patients out of aggregate inpatients days for all patients as an alternative measure.
Hospital characteristics
We included several hospital characteristics in our analyses that were available from the American Hospital Association Annual Survey. These were bed size (less than 100, 100-199, and 200 or more); teaching hospital status based on membership in the Council of Teaching Hospitals; ownership (not-for-profit, government non-federal, and for-profit), region (Northeast, Midwest, South, and West), share of Medicare inpatient days out of total inpatient days, and share of Medicaid inpatient days out of total inpatient days.
Analysis
The hospital characteristics of safety-net vs. non-safety-net hospitals were compared in the baseline year 2009. We conducted t-tests for differences between the two groups for continuous variables and chi-square tests for categorical variables. We plotted trends in hospital readmission rates for each condition for safety-net vs. non-safety-net hospitals over the study period. Linear time series models were estimated to capture average annual change in readmission rates for the same conditions from 2009 to 2016 [29].
The association between the main outcome (risk-adjusted hospital 30-day readmission rate for each condition) and safety-net hospital status was estimated using a difference-in-differences approach, whereby pre- vs. post-period changes in the outcome were compared between safety-net hospitals and non-safety-net hospitals [30, 31]. Since HRRP was announced in March 2010, we considered hospital readmissions performance in and after 2010 as potentially influenced by HRRP (i.e., post-period), even though the first year of implementation was 2013. As noted, the Hospital Compare readmission rates reported were based on admission during the three preceding years. Accordingly, we categorized the readmission rates for 2009 and 2010 (for admissions during July 2005 to June 2009) as representing the pre-HRRP period, and the rates for 2014 to 2016 (for admissions during July 2010 to July 2015) as representing the post-HRRP period. The intervening years 2011-2013 (the “washout” period) were excluded from the difference-in-differences analysis since the readmission rates were based on both pre- and post-2010 time period.
For our core analysis to estimate the change in the main outcome (risk-adjusted 30-day readmission rate) associated with HRRP we used a linear hospital-level random effects regression model with a difference-in-differences specification and heteroscedasticity-robust standard errors [32, 33]. For the difference-in-differences specification, we included an indicator for the safety-net hospitals, a post-period time indicator, an interaction term between safety-net hospitals and post-period – the difference-in-differences estimator – and adjusted for hospital characteristics in the baseline year. The difference-in-differences estimate gives the excess pre to post change in readmission rate for safety-net hospitals compared to that for non-safety-net hospitals [30, 34, 35]. The difference-in-differences approach assumes similarity in pre-period trends for each outcome between safety-net and non-safety net hospitals (“parallel trends assumption”) [31]. We tested for parallel trends by estimating a placebo version of the proposed difference-in-difference models using only pre-period data (2009-2010) (Additional file 1: Table 2). Specifically, outcome in 2009 was compared with that in 2010 (“post 2010”). Absence of a significant coefficient of the interaction term (safety-net x post) is indicative of similar trends in safety-net and non-safety-net hospitals. We also examined sensitivity of the estimates to an alternative longitudinal data structure model that controls for time-invariant unobserved differences across hospitals (i.e., “hospital fixed effects”) [33, 36]. All models included year fixed effects to adjust for secular trends in readmission rates.
Using data on HRRP penalties from 2013 to 2016, we compared several indicators of the penalty experience of safety-net vs. non-safety-net hospitals: (i) share of hospitals penalized, (ii) average annual penalty, and (iii) distribution of repeated penalties. The comparisons were made using t-test.
Statistical analyses were conducted using Stata version 14.1 [37]. The Institutional Review Board of the Boston University School of Medicine considered this study exempt from human subjects review as no person-level data was involved.
Results
Our final analytic sample included 1915 hospitals in each year from 2009 to 2016. The characteristics of the safety-net and non-safety-net hospitals are shown in Table 1. The mean DSH index value was 0.54 for safety-net hospitals and 0.20 for non-safety-net hospitals. Safety-net hospitals were more likely to be teaching hospitals (25%) than non-safety-net hospitals (8%). Safety-net hospitals had a lower share of Medicare and higher share of Medicaid inpatient days relative to non-safety-net hospitals (Medicare share: 0.41 vs 0.52; Medicaid share: 0.29 vs. 0.15). The majority of the safety-net hospitals were concentrated in the South and West (72.02% overall) and non-safety-net hospitals in the Midwest and South (63.37% overall).
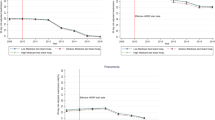
Figure 1 indicates the longitudinal 30-day risk adjusted readmission rates for safety-net vs. non-safety hospitals by admission condition. In 2009, the baseline year, safety-net hospitals had a slightly higher readmission rate compared to non-safety net hospitals for all three conditions: AMI, 20.3% vs. 19.8% (p value< 0.001); heart failure, 25.2% vs. 24.2% (p-value< 0.001); pneumonia, 18.7% vs. 18.1% (p-value< 0.001). Beginning in 2012, readmission rates declined for both hospital groups for all three conditions. The average (unadjusted) annual change in readmission rates for safety-net vs. non-safety-net hospitals over the study period was − 0.51% vs. -0.53% [p-value = 0.80] for AMI, − 0.45% vs. -0.48% [p-value = 0.74] for heart failure, and − 0.22% vs. -0.27% [p-value = 0.59] for pneumonia.
Average hospital 30-day risk adjusted readmission rate (%) by safety-net status and admission condition, 2009-2016. Notes: Safety-net hospitals: hospitals that fall in the top quartile of the Disproportionate Share Hospital (DSH) index; non-safety-net hospitals: hospitals in the bottom three quartiles of the DSH index. Pre-period: FY 2009-2010; Washout period: FY 2011-2013; Post-period: FY 2014-2016. Data reporting year and data collection period (in parenthesis) reported from Hospital Compare website
To test the validity of the proposed difference-in-differences approach to obtain adjusted rates of post-program change in readmission rates, we compared pre-period readmission trends (using 2009-2010 data) between safety-net vs. non-safety-net hospitals (“parallel trends test”) and found that for all three admission cohorts pre-period trends were similar among both the hospital groups (Additional file 1: Table 2). Applying this approach to the analytic data spanning the pre and post HRRP periods we found that pre-to-post change in readmission rates were similar among safety-net and non-safety-net hospitals for AMI and heart failure (Table 2; Additional file 1: Table 3). For pneumonia admissions, we found a larger post-period reduction (of 0.23%) in safety-net hospitals relative to non-safety-net hospitals (Additional file 1: Table 3). In sensitivity analysis using an alternative approach to identify safety-net hospitals, based on Medicaid share of total hospital inpatient days of care, we found largely similar results of pre-to-post adjusted changes in readmission rates (Additional file 1: Table 4). Estimation using a hospital-level fixed effects specification also yielded similar results (Additional file 1: Table 5).
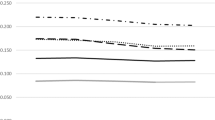
The proportion of hospitals penalized under HRRP was significantly higher among safety-net hospitals than non-safety-net hospitals in each year of the program (Fig. 2); in 2016, 90% of safety-net hospitals were penalized, compared to 85% of non-safety-net hospitals. The proportion of safety-net hospitals (72%) that were penalized all 4 years was higher compared to that for non-safety-net hospitals (59%) (Additional file 1: Fig. 3). In the first 2 years, the average penalty rate was also higher for safety-net hospitals (Table 3).
Share of hospitals penalized under HRRP by safety-net status, 2013-2016. Notes: 1) Safety-net hospitals: hospitals that fall in the top quartile of the Disproportionate Share Hospital (DSH) index; non-safety-net hospitals: hospitals in the bottom three quartiles of the DSH index. 95% confidence intervals indicated with vertical lines. 2) p-value for difference in mean share of hospitals penalized under HRRP between safety-net and non-safety-net hospitals reported for each year 2013-2016
Discussion
Our study highlights two contrasting findings on the experience of safety-net hospitals following HRRP. Readmission rates for all three admission conditions declined, and the extent of reduction in safety-net hospitals was no smaller than that in non-safety hospitals. Specifically, we found similarity in reduction for AMI and heart failure cohorts; although safety-net hospitals experienced a larger reduction for the pneumonia cohort compared to non-safety-net hospitals the margin of difference was small (0.23% larger reduction over a 18.8% baseline rate). However, the proportion of safety-net hospitals penalized under HRRP was higher than that among non-safety-net hospitals during each of the 4 years examined (2013-2016).
This study extends prior work on HRRP impact on safety-net hospitals by addressing methodological differences in previous studies that limit the comparability and interpretability of findings: we contrasted within hospital changes in post-program with pre-program readmission rates; we used readmission rates obtained from the Hospital Compare program instead of those derived from alternative admission cohorts or risk adjustment methods; we examined a longer post-program period. Our finding that readmission rates in safety-net hospitals decreased at least as much as in non-safety-net hospitals for all three admission conditions is largely in concordance with the findings of the previous studies. The study by Carey and Lin [16] was based on comparison of only the post-program experience of the hospitals. Specifically, comparing change in readmission rates between 2013 and 2016 in safety-net hospitals with that in (all or a matched subgroup of) non-safety-net hospitals, that study found similar changes in both settings or modestly higher reductions in safety-net hospitals across the different conditions [16]. Salerno et al. [17] compared readmission rates for (nearly) all hospitalized patients, and found that between 2008 and 2015, readmission rates in safety-net hospitals decreased more than in the non-safety-net hospitals, although the magnitude of the difference was small. Our study uses hospital readmission performance during 2010 to 2015 to evaluate the post-HRRP changes so as to accommodate potential changes at the hospital level in response to the announcement of HRRP penalties in 2010. We have specified hospital characteristics identified at baseline, and therefore interpret the estimated changes in readmission rates associated with HRRP as arising from direct and indirect (mediated) changes, including strategic hospital responses in making systematic changes in the profile of patients hospitalized.
Aside from studies comparing the readmissions experience of safety-net and non-safety net hospitals, several studies examining all hospitals together also found reductions in readmission rates following HRRP announcement in 2010. Studies by Zuckerman et al. [38], Figueroa et al. [39] and Chaiyachati et al. [40] found significantly large annual reductions in readmission rates. Several studies have indicated that upcoding of patient comorbidity status may account for a sizable proportion of the reduction in readmissions [41, 42]. As our study is based on Hospital Compared risk-adjusted readmission rates – that are based on diagnosis codes identified in both outpatient and inpatient claims data – our estimates are less susceptible to the over-estimation of reduction in readmissions.
The readmissions performance contrasts sharply with the penalty experience of safety-net hospitals relative to that of non-safety-net hospitals: during 2013-2016, safety-net hospitals were more likely to be penalized each year, more likely to be repeatedly penalized and have higher average penalty. Our findings on the penalty experience are consistent with those from prior studies, but present a more comprehensive overview of the penalty measures, spanning multiple years and national data. Using 2013 data alone, Joynt et al. [13] found that safety-net hospitals were more likely to be highly penalized compared to non-safety-net hospitals. Favini et al. [15] found larger mean penalty for safety-net hospitals in the initial years of HRRP (2013-2014) but similar penalty in the latter years (2015-2016). Using data from California, Gilman et al. [14] found safety-net hospitals to be more likely to be penalized compared to non-safety-net hospitals. In dollar terms, the Office of the Assistant Secretary for Planning and Evaluation also estimated the average penalty to be $191,000 for safety-net and $150,000 for non-safety-net hospitals (2011-2013) [43]. Although the difference in average amounts are relatively small, the adverse effect of the penalty may be greater among safety-net hospitals as they are likely to have a smaller “profit” (surplus) margin and rely more on Medicare revenues compared to non-profit hospitals [15].
This dichotomy in readmission rate performance and penalty experience validates and accentuates the concern of undue burden of HRRP penalties on safety-net hospitals. Cross-sectional differences in readmission rates across hospitals, which primarily underlie the penalty experience, may arise from systematic differences in patient profiles across hospitals. In the existing penalty determination algorithm, hospitals are penalized for unplanned readmissions that are unrelated to the index admission, despite the fact that such readmissions may not be associated with the care provided by the hospital [3]. Another concern is that the HRRP penalty formula does not adjust for factors that are outside the control of the hospital and increases the risk of readmissions. One study attributed roughly 60% of the variation in hospital readmission rates to community-level factors [44]. Joynt et al. estimated an enhanced risk adjustment model adding patient neighborhood deprivation indicator and found that readmissions performance of safety-net hospitals improved and that of other hospitals worsened [45]. Other studies have also highlighted the role of socioeconomic and environmental factors such as income, living status, social support, education, employment status, home stability, and risk behaviors in explaining a portion of the variation in readmission rates [6,7,8,9,10]. Another study found racial/ethnic differences in the likelihood of readmissions for targeted conditions [46]. It found that among Medicare enrollees, African-Americans having an index hospitalization for AMI, heart failure, or pneumonia had a higher likelihood of readmissions compared to whites. Overall, our results lend support to the concerns about the lack of fairness of the current HRRP penalty formula, particularly toward safety-net hospitals [3].
In response to the widespread concerns raised early after the announcement of HRRP, the twenty-first Century Cures Act of 2016 introduced modifications to HRRP beginning in 2019, wherein all hospitals are stratified by the proportion of low socioeconomic status patients served – as quantified by the proportion of Medicare patients who were also eligible for Medicaid benefits – into five groups (quintile “peer groups”), and readmissions performance will be assessed based on intra-group differences [20]. This modification was informed by early findings from studies in response to the Improving Medicare Post-Acute Care Transformation (IMPACT) Act, 2014 [47,48,49]. While the impact of the peer-group based HRRP is awaited, Joynt et al. [45] obtained penalty estimates under the traditional and the peer-group based HRRP penalty algorithms and found that hospitals serving in disadvantaged neighborhoods experienced lower penalties under the peer-group based program. Alternative modifications to HRRP performance evaluation have also been proposed; in particular, the National Quality Forum has advocated for the inclusion of social risk factors in the risk-adjustment models for pay-for-performance programs [50]. Recommending against this inclusion, the Office of the Assistant Secretary for Planning and Evaluation (ASPE) raises the concern that “if social risk adjustment were to undercut incentives to address the systemic problems that affect vulnerable patients, it could move us further away from an equitable health system “ [51, 52]. Instead ASPE favors a broader agenda of directly tackling social risk factors through additional supports in ongoing health-related programs and social service programs.
We acknowledge several limitations of our study. First, as our study data is observational, the ability to obtain firm causal estimates is limited. However, the difference-in-differences design is aimed at adjusting for unobserved secular trends to better isolate the changes in readmission rates associated with the introduction of the HRRP program. The “parallel trends” test indicated that, prior to the announcement of HRRP in 2010, the pattern of changes in readmission rates were similar between safety-net and non-safety net hospitals [31]. We concede that this test was limited to only 2 years (2009, 2010) since Hospital Compare reporting of hospital readmission rates began in 2009. HRRP has been expanded to include other admission cohorts (e.g., COPD). However, we limited the study to the three selected conditions as these original conditions have been the focus of much of the literature on HRRP impact. Second, given the lack of a universal definition of safety-net hospitals, our findings may be sensitive to the measure we used. Our measure based on the DSH index has been commonly used in prior studies. We also performed sensitivity analysis using an alternative definition of safety net hospitals, based on the Medicaid caseload of hospital admissions, and found largely similar results. Third, a limitation of using Hospital Compare data is that they do not include information on the racial/ethnic composition of the patients at the hospital level, thereby limiting our ability to examine subgroups of hospitals based on minority share of patients. As Hospital Compare risk-adjusted readmission rates are based on all index admissions during rolling 3-year periods, we were unable to estimate changes during individual years. As we only included hospitals that continuously were reimbursed through IPPS and for which Hospital Compare readmissions data were reported, the study cohort may not be representative of all hospitals.
Based on data from the first 4 years of HRRP penalties and readmission performance, our study findings add to the growing evidence that the HRRP performance assessment and penalty formula place an unduly higher risk of penalty on safety-net hospitals. While several modifications to the program have been suggested – with the imminent modification of performance assessment based on peer subgroups in 2019 – a clearer understanding of the nature of the modifications, their likely impact and the relative merits is needed. In the interim, CMS should consider measures to limit the burdensome revenue loss from HRRP penalties on safety-net hospitals, and introduce initiatives to collaboratively guide and support such hospitals in improving care for socioeconomically disadvantaged patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. We used publicly available nationwide hospital level data for 2009-2016 from the Centers for Medicare and Medicaid Services (CMS) Hospital Compare program http://www.medicare.gov/hospitalcompare/search.html;2018, CMS Final Impact Rule https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Historical-Impact-Files-for-FY-1994-through-Present.html;2017 and the American Hospital Association Annual Survey (www.ahadata.com).
Abbreviations
- HRRP:
-
Medicare’s Hospital Readmissions Reduction Program
- CMS:
-
Centers for Medicare and Medicaid Services
- AMI:
-
Acute Myocardial Infarction
- HF:
-
Heart Failure
- IPPS:
-
Inpatient Prospective Payment System
- DSH:
-
Disproportionate Share Hospital
References
Centers for Medicare and Medicaid Services. Readmissions reduction program (HRRP). Baltimore: Centers for Medicare and Medicaid Services; 2017.
Patient Protection and Affordable Care Act. H.R. 3590. Public Law 111-48; 2010.
American Hospital Association. Rethinking the hospital readmissions reduction program. Chicago: American Hospital Association; 2015.
Fos E. The unintended consequences of The Centers for Medicare and Medicaid Services pay-for-performance structures on safety-net hospitals and the low-income, medically vulnerable population. Health Serv Manag Res. 2017;30(1):10–5.
Fouayzi H, Ash AS. High-frequency hospital users: the tail that wags the readmissions dog. Health Serv Res. 2021. https://doi.org/10.1111/1475-6773.13677.
Amarasingham R, Moore B, Tabak Y, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–8.
Bhalla R, Kalkut G. Could medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152(2):114–7.
Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–82.
Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart Lung. 2003;32(2):88–99.
Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803–12.
Psotka MA, Fonarow GC, Allen LA, et al. The hospital readmissions reduction program: Nationwide perspectives and recommendations: a JACC: heart failure position paper. JACC Heart Fail. 2020;8(1):1–11.
Joynt K, Jha A. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309(4):342–3.
Gilman M, Adams EK, Hockenberry JM, Wilson IB, Milstein AS, Becker ER. California safety-net hospitals likely to be penalized by ACA value, readmission, and meaningful-use programs. Health Aff (Millwood). 2014;33(8):1314–22.
Favini N, Hockenberry JM, Gilman M, Jain S, Ong MK, Adams EK, et al. Comparative trends in payment adjustments between safety-net and other hospitals since the introduction of the hospital readmission reduction program and value-based purchasing. JAMA. 2017;317(15):1578–80.
Carey K, Lin MY. Hospital readmissions reduction program: safety-net hospitals show improvement, modifications to penalty formula still needed. Health Aff (Millwood). 2016;35(10):1918–23.
Salerno AM, Horwitz LI, Kwon JY, et al. Trends in readmission rates for safety net hospitals and non-safety net hospitals in the era of the US Hospital Readmission Reduction Program: a retrospective time series analysis using Medicare administrative claims data from 2008 to 2015. BMJ Open. 2017;7(7):e016149.
National Quality Forum. Endorsement summary: all-cause readmissions. Washington, DC: National Quality Forum; 2012.
Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. 2016 condition-specific measures updates and specifications report hospital-level 30-day risk-standardized readmission measures. Report. 2016.
Centers for Medicare & Medicaid Services. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and policy changes and fiscal year 2019 rates; quality reporting requirements for specific providers; Medicare and Medicaid Electronic Health Record (EHR) Incentive Programs (Promoting Interoperability Programs) requirements for eligible hospitals, critical access hospitals, and eligible professionals; Medicare cost reporting requirements; and physician certification and recertification of claims. Final rule. Fed Regist. 2018;83(160):41144–784.
Fuller RL, Hughes JS, Goldfield NI, Averill RF. Will Hospital peer grouping by patient socioeconomic status fix the Medicare hospital readmission reduction program or create new problems? Jt Comm J Qual Patient Saf. 2018;44(4):177–85.
Department of Health and Human Services. Medicare hospital compare quality of care. Available from: www.hospitalcompare.hhs.gov/.
Centers for Medicare & Medicaid Services. FY 2016 IPPS Final Rule. www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2016-IPPS-Final-Rule-Home-Page.html. Accessed 25 Jan 2018.
American Hospital Association. FY2010 American Hospital Association annual survey. Chicago: American Hospital Association; 2009.
Lake Superior Quality Innovation Network. Understanding value-based purchasing. 2015. www.lsqin.org/wp-content/uploads/2017/12/VBP-Fact-Sheet.pdf. Accessed 22 Jan 2018.
Normand S-LT, Shahian DM. Statistical and clinical aspects of hospital outcomes profiling. Stat Sci. 2007;22(2):206–26.
Centers for Medicare & Medicaid Services. Disproportionate Share Hospital (DSH): the Medicare DSH adjustment (42 CFR 412.106). Baltimore: Centers for Medicare and Medicaid Services; 2009.
Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Arch Intern Med. 2012;172(16):1204–10.
Hanchate AD, McCormick D, Lasser KE, Feng C, Manze MG, Kressin NR. Impact of Massachusetts health reform on inpatient care use: was the safety-net experience different than in the non-safety-net? Health Serv Res. 2016;52(5):1647–66.
Dimick J, Ryan A. Methods for evaluating changes in health care policy: the difference-in-differences approach. J Am Med Assoc. 2014;312(22):2401–2.
Ryan AM, Burgess JF Jr, Dimick JB. Why we should not be indifferent to specification choices for difference-in-differences. Health Serv Res. 2015;50(4):1211–35.
Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates? Q J Econ. 2004;119(1):249–75.
Cameron A, Trivedi P. Microeconometrics: methods and applications. New York: Cambridge University Press; 2005.
Wooldridge JM. Econometric analysis of cross-section and panel data. Cambridge: The MIT Press; 2002.
Kolstad J, Kowalski A. The impact of health care reform on hospital and preventive care: evidence from Massachusetts. J Public Econ. 2012;96(11):909–29.
Baltagi B. Econometric analysis of panel data. Chichester: Wiley; 2008.
StataCorp. Stata statistical software: release 14. College Station: StataCorp LP; 2015.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. New England J Med. 2016;374(16):1543–51.
Figueroa JF, Zheng J, Orav EJ, Epstein AM, Jha AK. Medicare Program Associated With Narrowing Hospital Readmission Disparities Between Black And White Patients. Health Affairs. 2018;37(4): 654-661.
Chaiyachati KH, Qi M, Werner RM. Changes to racial disparities in readmission rates after medicare’s hospital readmissions reduction program within safety-net and non–safety-net hospitals. JAMA Network Open. 2018;1(7):e184154.
Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of coded severity with readmission reduction after the hospital readmissions reduction program. JAMA Intern Med. 2018;178(2):290–2.
Ody C, Msall L, Dafny LS, Grabowski DC, Cutler DM. Decreases in readmissions credited to Medicare’s program to reduce hospital readmissions have been overstated. Health Aff. 2019;38(1):36–43.
Office of the Assistant Secretary for Planning and Evaluation. Report to congress: social risk factors and performance under Medicare’s value-based purchasing programs. 2016.
Herrin J, St Andre J, Kenward K, Joshi MS, Audet AM, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20–39.
Joynt Maddox KE, Reidhead M, Hu J, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;54(2):327–36.
McHugh MD, Carthon JM, Kang XL. Medicare readmissions policies and racial and ethnic health disparities: a cautionary tale. Policy Polit Nurs Pract. 2010;11(4):309–16.
Sheingold SH, Zuckerman R, Shartzer A. Understanding Medicare hospital readmission rates and differing penalties between safety-net and other hospitals. Health Aff (Millwood). 2016;35(1):124–31.
Centers for Medicare & Medicaid Services. IMPACT Act of 2014 & cross setting measures. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014-and-Cross-Setting-Measures.html2015.
Medicare Payment Advisory Commission. Report to the Congress: Medicare and the health care delivery system. Washington (DC): MedPAC; 2013. Available from: http://medpac.gov/docs/default-source/reports/jun13_entirereport.pdf?sfvrsn=0
National Quality Forum. Risk adjustment for socioeconomic status or other sociodemographic factors. Technical report. 2014; Available from: http://www.qualityforum.org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx.
Sheingold SH, Zuckerman R, DeLew N, Sommers BD. Health equity and value-based payment systems: moving beyond social risk adjustment. Health Affairs Blog. 2021; https://www.healthaffairs.org/do/10.1377/forefront.20210726.546811.
Office of the Assistant Deputy Under Secretary for Health for Policy and Planning. Developing health equity measures. https://aspe.hhs.gov/pdf-report/developing-health-equity-measures2021.
Acknowledgements
Not applicable.
Funding
This study was funded by the National Institutes of Health (Grant: R01MD010527; Principal Investigator: Amresh D. Hanchate).
Author information
Authors and Affiliations
Contributions
SB and ADH were responsible for the conception and design of the study, and analysis and interpretation of the data. SB and ADH drafted the manuscript. ADH and ML were responsible for obtaining and developing the analytic data. DM, MPO and ML contributed to interpretation of the findings, and were involved in the revising it for important intellectual content. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is approved by the Office of Research Institutional Review Board of Wake Forest University Health Sciences. The study reference number is IRB00059384. This research meets the criteria for a waiver of consent entirely according to 45 CFR 46(d), as well meeting the criteria for a waiver of HIPAA authorization according to 45 CFR 164.512. The study was carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Data collection and reporting dates for 30-day risk adjusted readmissions. Table 2. Validity of difference-in-differences model estimates of change in 30-day readmissions associated with HRRP: Parallel trends test. Table 3. Difference-in-differences model estimates of change in 30-day readmissions associated with HRRP: Main model estimates. Table 4. Sensitivity Analysis: Difference-in-difference model estimates of change in 30-day readmission rates using alternative definition of safety-net hospitals using Medicaid share inpatient days. Table 5. Sensitivity Analysis: Difference-in-difference model estimates of change in 30-day readmission rates using hospital fixed effects specification. Figure 3. Distribution of number of years of penalty under HRRP by safety-net status, 2013-2016.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Banerjee, S., Paasche-Orlow, M.K., McCormick, D. et al. Readmissions performance and penalty experience of safety-net hospitals under Medicare’s Hospital Readmissions Reduction Program. BMC Health Serv Res 22, 338 (2022). https://doi.org/10.1186/s12913-022-07741-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07741-9