Abstract
Background
Patients in spine surgery often have emotional disorders which is caused by multi-factors. Therefore, a multidisciplinary and multimodal intervention program is required to improve emotional disorders during the perioperative period. However, related studies were rare. This study aimed to confirm that the multidisciplinary-based psychological management leading by nurses was effective in treating emotional disorders and show the assignments of the members of the multidisciplinary team with the orientations of nurses.
Design
A retrospective, comparative study.
Method
This study was a retrospective cohort research and compared the results between the intervention group and control group using the Huaxi Emotional Distress Index (HEI) which was used to evaluate emotional disorders. The intervention group consisted of patients who underwent surgery between January 2018 and December 2020 after psychological management was implemented. The control group consisted of patients with regular care who underwent surgery between January 2015 and December 2017. To improve comparability between the two groups, baseline data from the recruited patients were analyzed using propensity-score-matching (PSM) based on age, sex, marital status, education, and disease region.
Results
A total of 539 (11.5%) people developed emotional disorders, of which 319 (6.8%), 151 (3.2%) and 69 (1.5%) had mild, moderate mood and severe emotional disorders, respectively. 2107 pairs of patients were matched after PSM. Scores of HEI in the intervention group were heightened compared with those in the control group (P<0.001) after matching. Moreover, the incidence of emotional disorders in patients decreased after implementing psychological management (P = 0.001). The severity of emotional disorders was alleviated with statistical significance as well (P = 0.010).
Conclusions
Nurses-led Multidisciplinary-Based psychological management was able to reduce the incidence of emotional disorders and improve the severity of these in spine surgery patients.
Similar content being viewed by others
Introduction
Spine degenerative diseases are highly prevalent worldwide and bring about a huge economic burden [1]. It estimated that direct costs were more than $80 billion for treatment of them [2, 3]. Spine surgery reduces patients’ suffering in degenerative spine conditions such as degenerative lumbar stenosis, disc herniation, and degenerative scoliosis [4,5,6]. However, surgery is a stressful experience for most people. A great deal of patients experienced emotional disorders, with 1 out of 3 experiencing depression or anxiety [7]. According to a cross-sectional study of 512 patients undergoing spine surgery, 55% had preoperative anxiety, and 54% had preoperative depression [8]. Emotional disorders such as anxiety might lead to exacerbated functional outcomes and clinical prognoses [9, 10]. Therefore, effective psychological management is beneficial to the prognosis of patients with spinal surgery.
Perioperative psychological management for spine surgery, such as pain management and timely psychological or information support, has been reported [7, 11]. However, these management schemes are unilateral, and emotional disorders are factorial [12]. It is well documented that patients with pain and multimorbidity are more prone to depression than the general population [13, 14]. Other studies have also found that the level of disability and knowledge of disease information affected the level of emotional disorders in patients with spine surgery [12]. Therefore, perioperative psychological management requires the cooperation of a multidisciplinary team. In 1997, Henrik Kehlet proposed a multimodal approach to perioperative management known as “Fast-Track Surgery” [15]. This approach was developed into the Enhanced Postoperative Recovery (ERAS) program aimed at improving recovery, which is an evidence-based approach to perioperative care and related to anesthesia, nutrition, sleep and other aspects [16]. Improving surgical outcomes, reducing complications, improving patient experience, and reducing hospital stays are the main goals of ERAS [17, 18]. Under the concept of ERAS, a multidisciplinary team is needed to boost a certain clinical outcome during the perioperative period [19]. Previously, numerous studies have confirmed the ERAS protocols in perioperative management effectively [20]. Nevertheless, multidisciplinary-based psychological management in spine surgery patients is still controversial.
Hence, this study sought to investigate the prevalence of emotional disorders and evaluate whether multidisciplinary-based psychological management was effective in improving emotional disorders in patients with spine surgery. This study discussed how multidisciplinary teams collaborate and the way nurses leading to.
Article types
Original research.
Materials and methods
Study design
The study was designed as a nonrandomized controlled clinical trial. With the intent of comparing the incidence of emotional disorders and the differences in the composition of grades in emotional disorders of patients before and after the implementation of the management, we conducted a retrospective evaluation between January 2015 and December 2020 in a single-center orthopedic spine department. Baseline data of the enrolled patients were analyzed using propensity-score-matching (PSM) to enhance comparability between the two groups. Our study was conducted in accordance to the relevant guidelines and regulations or in accordance to the Declaration of Helsinki. The study protocol was reviewed and approved by the Research Ethics Committee of the Institutional Review Board (2017 (Review) No. 128). This study was conducted in accordance to the relevant guidelines and regulations.
Patient sample
The inclusion criteria for patients were as follows: (1) age greater than 16 years old, (2) surgery scheduled for the first time, and (3) had spine surgery. Exclusion criteria included trauma, infection, and cancer as indications for surgeries. Patients who were diagnosed with sleep disturbances were not considered. The intervention group consisted of patients who underwent surgery between January 2018 and December 2020 after psychological management was implemented. The controls were matched with those who underwent surgery prior to initiation of psychological management based on age, sex, marital status, education, and disease region in the same medical unit. Therefore, the control consisted of patients with regular care who underwent surgery between January 2015 and December 2017.
Outcome measures
Anxiety, depression, suicidal ideation, and other psychological problems, known as emotional disorders, were measured by the Huaxi Emotional-distress Index (HEI) [21]. The scale has a sensitivity of 88% and a specificity of 76.58%. The internal consistency was 0.898. The HEI self-evaluation scale was developed by West China Hospital of Sichuan University for the rapid screening of patients’ psychological status in nonpsychiatric clinical settings. The main scale consists of nine items that can be finished in less than 5 min. Using the 5-point Likert-scale scoring method, the total score is 36. Scores ranging from 0 to 8 indicate normal or no emotional disorder. Scores of 9 to 12 represent mild emotional disorder. Ranging from 13 to 16 hints at moderate emotional disorder, and over 17 represents severe emotional disorder. Items 10 and 11 were used as references and only appeared when items 1–9 scored more than 9 points and were not included in the final score. Patients who received a HEI score greater than 8 points were perceived as having emotional disorders. In this study, the postoperatively measured HEI score was used to represent the level of perioperative emotional disorders of patients.
Psychological management program
Under the guidance of a multidisciplinary team of experts, management based on ERAS was established in the spine surgery ward in 2017. This model focused on the improvement of patients’ psychology, sleep, rehabilitation and other aspects. A psychological management program for patients has been implemented since January 2018. During the implementation process, the content of the program was adjusted in time. Regular and complete psychological management was carried out finally.
Establishment of a multidisciplinary team (MDT) According to Best Evidence Summary, the core members’ departments were confirmed, including orthopedics, mental health centers, anesthesiology and pharmacy [22]. The medical team that closely cooperated with the orthopedic department was selected as a member of the cooperative management group from the included departments. Sunshine Angels, orthopedic nurses who have obtained the qualifications of psychological consultants and get the training from the Mental Health Center, took responsibility for psychological assessment and basic supports for patients directly. Additionally, she would feed back the general emotional situation of patients, interventions, effects of interventions and other information to all levels of management, who decided on further intervention programs. Under the leadership of the multidisciplinary experts from management group, the implementation of specific measures was progressive from the decision-making layer (medical team leader, head nurse) to the implementation layer (resident surgeons, advanced doctors, nursing team leaders, charge nurses) and then to the security layer (mental health experts, anesthesiology experts, pharmacy experts). Table 1 revealed the members’ tasks in detail.
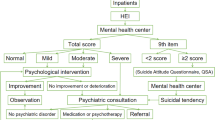
Regular pathway of psychological management Fig. 1 illustrated the flow diagram of the management pathway. All patients were evaluated for HEI within 2 h of admission by the nurses in charge. In the case of a patient with a severe emotional disorder, an additional assessment within 24 h was needed. Results of HEI were registered and fed back by the mental health center who reported patients with emotional disorders to the ward. The surgeon in charge would receive the results of the psychological assessment from the patient’s nurse in charge as soon as possible. Then, the orthopedic ward formulated corresponding psychological management according to the level of emotional disorders. Multidisciplinary-Based Psychological Management adopted a 4-level stepwise intervention for patients.
-
Level 1 (charge nurses): The main task is to provide simple psychological support to the patient. The charge nurses used their interpersonal skills to ask patients whether they needed assistance. They tended to encourage patients who have not yet manifested emotional illnesses by listening to them and showing empathy.
-
Level 2 (sunshine-angel-led physical prevention): The Sunshine Angel had to step in again when patients developed emotional disorders. The first time the reasons of the patient’s emotional disorders were recognized was through a professional and quick psychological consultation. Sunshine Angels only offered psychological supports through physical means due to they are not permitted to prescribe in China. Music therapy, which may help patients learn to relax and treat emotional issues, was the physical technique employed in this study (Solanki et al., 2013).
-
Level 3 (Surgeon-led medication prevention): Physical therapies were ineffective when patients had mild emotional difficulties. In order to treat emotional problems, combination medications were therefore required. A mixture of analgesics (nonsteroidal anti-inflammatory medicines), anti-anxiety medications (paroxetine hydrochloride), and sleep aids (zolpidem tartrate, estazolam) was utilized as the foundation for the Level 2 intervention. The medication must be taken in accordance with a doctor’s prescription, and nurses were present to ensure that the patients took their medications on schedule.
-
Level 4 (MDT-led integrated intervention): MDT-led integrated therapies were necessary when patients had serious emotional problems. Early intervention by medical professionals from the mental health facility included professional behavior and cognitive therapy paired with medication, as well as extensive cognitive behavioral therapy and relaxation treatment. Patients were expected to take their medications as directed by their doctors, supervised by charge nurses. If required, the patient was sent to mental care after their specialized condition was stabilized.
Statistical analysis
Statistical description was performed using Python 3.9.5 software, and statistical analyses were performed using SPSS 22.0 software((SPSS, Chicago, IL, USA)with the PSM plug-in. The characteristics of patients and the incidence of emotional disorders were displayed using a heatmap. To control for bias, we used PSM by the Nearest Neighbor Matching method with a ratio of 1:1. Age, sex, marital status, education level, and disease region were conducted as covariance of matching by 3-step procedure: development of propensity score, matching, and assessment imbalance. Logistic regression was used to calculate propensity scores, that is, to predict the likelihood of entry into the group implementing psychological management based on ERAS. Matching was performed by a greedy algorithm, and the caliper distance was 0.02 with exact matching and fuzzy matching. For continuous variables, the standard mean deviation (SMD) was used to assess the balance after matching. SMD of the categorical variable was transformed by the formula and used for the balance test as well. SMD < 0.02 was considered a small effect size. The McNemar test was used for matched binary variables, and the chi-square test was used for unordered multi-categorical variables for analysis. Rank tests were used for ordinal multi-categorical variables and nonnormal continuous variables. The paired t test was used for normal continuous variables after PSM. The test level was P < 0.05.
Results
General information of patients
We exported 5813 patient data points from the hospital information system (HIS). 775 patients had sleep disturbances, and 109 had a diagnosis of chronic pain. In addition, 179 patients who underwent operations more than twice during 2015–2020 were excluded. Subsequently, 4571 patients meeting the inclusion and exclusion criteria were included. Flow charting was illustrated in Fig. 2. Their ages ranged from 18 to 95 years old, and the mean age was 52.25 ± 14.85 years. A total of 2436 males accounted for 52.2%. The education of 2506 (53.7%) was junior high school and below. There were 579 (12.4%) with a high school education and 871 (18.6%) with an associate degree. The remaining 715 (15.3%) were undergraduate or above. Regarding marital status, majority of married patients were 4,122 (88.2%). There were 365 (7.8%) unmarried and 184 (3.9%) divorced or widowed patients. The diseased region included cervical (1508, 32.3%), thoracic (170, 3.6%), lumbar (2813, 60.2%) and other parts (180, 3.9%). Others included multi-segment scoliosis and sacrococcygeal disease. The visualization of the patient’s general information was shown in Fig. 3.
Emotional disorder prevalence
In this study, a total of 539 (11.5%) people developed emotional disorders, of which 319 (6.8%), 151 (3.2%) and 69 (1.5%) had mild, moderate mood and severe emotional disorders, respectively. The details of the emotional disorders of the patients are shown in Fig. 3.
Effect of multidisciplinary-based psychological management
This study compared the baseline data of patients before and after the implementation of multidisciplinary-based psychological management. The differences between the two groups were statistically significant. Therefore, PSM was used to match the baseline data of the two groups of patients to create a quasi-experimental design. 2107 pairs were matched after PSM. The baseline data and the incidence of emotional disorders in patients before and after PSM were shown in Tables 2 and 3, respectively. The results illustrated that the incidence of emotional disorders in patients dropped down after implementation of psychological management after PSM (P<0.001). In the control group, 283 people (13.5%) developed emotional disorders. Of these, 174 (8.3%) had mild emotional disorders, 75 (3.6%)) had moderate emotional disorders, and 34 (1.6) had severe emotional disorders. While 211 (10.0%) people had emotional disorders in the intervention group, of which the mild, moderate and severe emotional disorders were 118 (5.6%), 65 (3.1%) and 28 (1.3%), respectively. Meanwhile, scores of HEI in the intervention group were also heightened compared with those in the control group (P<0.001). The severity of emotional disorders was also alleviated with statistical significance (P = 0.010).
Discussions
Our findings demonstrated that 11.5% of patients had emotional disorders during spine surgery. This was close to the result of Bekeris et al., who reported that the incidences of anxiety and depression were 6% and 11.2% [23]. Prior study also found the incidence of emotional disorders in spine surgery were higher by using the Patient Reported Outcomes Measurement Information System (PROMIS) screening measures [8]. Although many studies focused on the occurrence of emotional disorders in patients during the perioperative period, the latest research verified that emotional disorders of a small number of patients were difficult to resolve and even developed a new depressive phenotype with the passage of postoperative time [24, 25]. Hence, it is particularly important to manage the emotions of perioperative patients scientifically and effectively. It is well known that an individual’s psychological state was affected by a variety of factors. A previous integrative review confirmed that pain, the need for information, disability, and workforce were factors associated with emotional disorders [12]. Factors influencing new-onset emotional disorders in patients undergoing spinal fusion surgery included long-term opioid using (OR: 1.31–2.93, P < 0.01), female sex (OR: 1.25–1.67, P < 0.01), longer hospital stay (OR: 1.05–1.08, P < 0.01) and readmission within 6 months after surgery (OR range 1.31 to 1.68, P < 0.01) [23]. The emotional disorder level increased as preoperative anesthetic uses increased as well [26]. Studies have shown that a single psychological intervention program was less effective than a multimodal psychological intervention program [27]. Hence, setting up various targeted interventions for the aforementioned factors may be able to control the occurrence of emotional disorders in spinal surgery patients.
Notably, patients’ emotional disorders were effectively alleviated by implementing a multidisciplinary-based psychological management. Similar research results were illustrated from the studies of Pennington et al. [22]. The aforementioned literature systematically reviewed the intervention programs and effects of multiple ERAS procedures in spine surgery and mentioned that multidisciplinary-based protocols had mostly followed patient education, blood glucose control, analgesia programs, fluid management, and nutritional management. Multidisciplinary-based management specifically for the psychology of perioperative patients were rare. Furthermore, surgeons might ignore the psychological problems of patients readily [28]. A survey of North American spine surgeons showed that they did not actively measure patients’ awareness of emotional disorders, and only 33.3% of them took the initiative to evaluate patients [28]. A total of 20.3% of spine surgeons preferred to deal with preoperative anxiety by cultivating the nurse–patient therapeutic relationship. Most spine surgeons did not realize their key role in the psychological management of patients. Meanwhile, they believed that this work should mainly allocate by anesthesiologists and patients themselves. In the circumstances, the unity of perception of these entities could support shared decision-making [29].
The interdisciplinary team’s defined roles in the cooperative psychological care of patients were highlighted in our psychological management. A sensible use of medical resources was targeted intervention by medical professionals from many disciplines for individuals with varying degrees of emotional disorders. The improvement of the intervention effect was also facilitated by consideration of elements at all levels during the intervention. In contrast to earlier research, ours placed a greater emphasis on the roles played by each member of the multidisciplinary team as well as the treatment of patients undergoing spine surgery who had varying degrees of emotional disturbances. In order to help with the design of psychological support during spine surgery, we want to offer some references. The team members’ total efforts improved as a result of the lead of Sunshine Angel, a special nurse who served as the key identity and organized the collaboration between several disciplines.
Clinicians are increasingly forced to negotiate an ever-changing healthcare landscape in which the focus of patient care must be delicately balanced between a value-based model that offers high-quality treatment while being accessible and feasible [30]. For this model to be successful, efforts must be aligned across multiple professionals to optimize outcomes and improve patient progress across the continuum of care [31]. The nurse-led management has demonstrated its superiority and cost-effective in several studies [32,33,34]. For example, a meta-analysis showed that nurse-led psychological interventions were effective in improving patients’ emotional disorders (mean difference: -5.51, 95% CI: -10.68, -0.34) [35]. Nurse-led clinical managements were initially used as a means of controlling rising healthcare costs, not only addressing health care shortages and needs, but also reducing the working hours of junior doctors [36]. Its development has been driven by health policies and the demand for health care, while being supported by the development of the nursing profession [37].
This study fully demonstrated that the leading role of nurses in psychological management could make management more executable. Nurse-led psychological interventions also availed the maintenance of the nurse–patient relationship.
The incidence of emotional disorders reported in this study could arouse clinical staff’s attention to the emotional problems of patients. In addition, this study also reported the effectiveness of Multidisciplinary-based management and the specific content of the program. By showing a more mature psychological management protocol, it was hoped that more clinical staffs could be enlightened in the psychological management of spinal surgery patients during the perioperative period. Finally, the disclosure of this protocol aimed to provide a reference for how multidisciplinary cooperation in improving one clinical outcome could be achieved. It also suggested what responsibilities each department could undertake in multidisciplinary and multimodal management.
Limitations: There were some limitations in our study. First, there were fewer variables that could be included in the PSM, and more confounding factors should be controlled to achieve a higher quality quasi-experimental study in the future. Because we can only get HEI scores after surgery and we only have access to restricted data from HIS. Secondly, more indicators should be added to verify the effect of the management implementation. Due to the single outcome measure, the strength of verifying that the implementation improved emotional disorders directly was limited. It was not clear whether the implementation would improve other indicators, such as pain, to improve emotional disorders. In the future, the relationship between these outcome measures and emotional disorders could be integrated by constructing a structural equation model. Moreover, patients who were diagnosed with different spine disease had various emotional disorder grade probably. Hence, we could conduct further research on the association of spine disease region and emotional disorders.
Conclusions
Our study used a retrospective PSM controlled study to confirm that multidisciplinary-based psychological management was able to reduce the incidence and improve the severity of perioperative emotional disorders in spine surgery patients. The prevalence of emotional disorders was 11.5% during the perioperative period. The perioperative psychological management of patients requires multidisciplinary cooperation. It was of vital importance that surgeons and nurses clearly understood their responsibilities. In this way, a good doctor-nurse-patient relationship would be maintained while managing the patient’s psychology.
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
References
Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, Dellavalle R, Danaei G, Ezzati M, Fahimi A, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.
Chotai S, Khan I, Nian H, Archer KR, Harrell FE, Weisenthal BM, Bydon M, Asher AL, Devin CJ. Utility of Anxiety/Depression domain of EQ-5D to define psychological distress in spine surgery. World Neurosurg. 2019;126:e1075–80.
Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, Horst C, Kaldjian A, Matyasz T, Scott KW et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020, 323(9):863–884.
Cushnie D, Thomas K, Jacobs WB, Cho RKH, Soroceanu A, Ahn H, Attabib N, Bailey CS, Fisher CG, Glennie RA, et al. Effect of preoperative symptom duration on outcome in lumbar spinal stenosis: a Canadian Spine Outcomes and Research Network registry study. Spine J. 2019;19(9):1470–7.
Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, Hwang SW, Mendel RC, Reitman CA. North American spine S: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013;13(7):734–43.
Demirel A, Yorubulut M, Ergun N. Regression of lumbar disc herniation by physiotherapy. Does non-surgical spinal decompression therapy make a difference? Double-blind randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30(5):1015–22.
Cushnie D, Fisher C, Hall H, Johnson M, Christie S, Bailey C, Phan P, Abraham E, Glennie A, Jacobs B, et al. Mental health improvements after elective spine surgery: a Canadian Spine Outcome Research Network (CSORN) study. Spine J. 2021;21(8):1332–9.
Purvis TE, Neuman BJ, Riley LH, Skolasky RL. Comparison of PROMIS anxiety and depression, PHQ-8, and GAD-7 to screen for anxiety and depression among patients presenting for spine surgery. J Neurosurg Spine 2019:1–8.
Carreon LY, Jespersen AB, Stottrup CC, Hansen KH, Andersen MO. Is the hospital anxiety and Depression Scale Associated with outcomes after lumbar spine surgery? Global Spine J. 2020;10(3):266–71.
Nordstoga AL, Vasseljen O, Meisingset I, Nilsen TIL, Unsgaard-Tondel M. Improvement in work ability, Psychological Distress and Pain sites in Relation to Low Back Pain Prognosis: a longitudinal observational study in primary care. Spine (Phila Pa 1976). 2019;44(7):E423–9.
Strom J, Hoybye MT, Laursen M, Jorgensen LB, Nielsen CV. Lumbar Spine Fusion patients’ Use of an internet support group: mixed methods study. J Med Internet Res. 2019;21(7):e9805.
Strom J, Bjerrum MB, Nielsen CV, Thisted CN, Nielsen TL, Laursen M, Jorgensen LB. Anxiety and depression in spine surgery-a systematic integrative review. Spine J. 2018;18(7):1272–85.
Yang Y, Tang TT, Chen MR, Xiang MY, Li LL, Hou XL. Prevalence and association of anxiety and depression among orthopaedic trauma inpatients: a retrospective analysis of 1994 cases. J Orthop Surg Res. 2020;15(1):587.
Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. 2017;221:36–46.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anesth. 1997;78:608–17.
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24(3):466–77.
Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362(9399):1921–8.
Liu VX, Rosas E, Hwang J, Cain E, Foss-Durant A, Clopp M, Huang M, Lee DC, Mustille A, Kipnis P, et al. Enhanced recovery after surgery program implementation in 2 Surgical populations in an Integrated Health Care Delivery System. JAMA Surg. 2017;152(7):e171032.
Debono B, Wainwright TW, Wang MY, Sigmundsson FG, Yang MMH, Smid-Nanninga H, Bonnal A, Le Huec JC, Fawcett WJ, Ljungqvist O, et al. Consensus statement for perioperative care in lumbar spinal fusion: enhanced recovery after surgery (ERAS(R)) Society recommendations. Spine J. 2021;21(5):729–52.
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–41.
Wang J, Guo WJ, Zhang L, Deng W, Wang HY, Yu JY, Luo SX, Huang MJ, Dong ZQ, Li DJ, et al. The development and validation of Huaxi emotional-distress index (HEI): a Chinese questionnaire for screening depression and anxiety in non-psychiatric clinical settings. Compr Psychiatry. 2017;76:87–97.
Pennington Z, Cottrill E, Lubelski D, Ehresman J, Theodore N, Sciubba DM. Systematic review and meta-analysis of the clinical utility of enhanced recovery after surgery pathways in adult spine surgery. J Neurosurgery: Spine. 2021;34(2):325–47.
Bekeris J, Wilson LA, Fiasconaro M, Poeran J, Liu J, Girardi F, Memtsoudis SG. New onset depression and anxiety after spinal Fusion surgery: incidence and risk factors. Spine (Phila Pa 1976). 2020;45(16):1161–9.
Chen Z, Luo R, Yang Y, Xiang Z. The prevalence of depression in degenerative spine disease patients: a systematic review and meta-analysis. Eur Spine J. 2021;30(12):3417–27.
Boakye M, Sharma M, Adams S, Chandler T, Wang D, Ugiliweneza B, Drazin D. Patterns and Impact of Electronic Health records-defined Depression phenotypes in spine surgery. Neurosurgery. 2021;89(1):E19–E32.
Armaghani SJ, Lee DS, Bible JE, Archer KR, Shau DN, Kay H, Zhang C, McGirt MJ, Devin CJ. Preoperative narcotic use and its relation to depression and anxiety in patients undergoing spine surgery. Spine (Phila Pa 1976). 2013;38(25):2196–200.
Debono B, Sabatier P, Boniface G, Bousquet P, Lescure JP, Garnaud V, Hamel O, Lonjon G. Implementation of enhanced recovery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: a propensity score-matched analysis. Eur Spine J. 2021;30(2):560–7.
Musa A, Wang JC, Acosta FL, Movahedi R, Melkonian A, Shahbazi A, Safani D, Gucev G. Attitudes of spine surgeons regarding management of preoperative anxiety: a cross-sectional study. Clin Spine Surg. 2019;32(1):E1–E6.
Boss EF, Mehta N, Nagarajan N, Links A, Benke JR, Berger Z, Espinel A, Meier J, Lipstein EA. Shared decision making and choice for Elective Surgical Care: a systematic review. Otolaryngol Head Neck Surg. 2016;154(3):405–20.
Kumar A, Gabbard E, Smith H et al. ICU Liberation: Optimizing Quality and Efficiency of Critical Care Delivery. Becker’s Healthcare 2017. Available at: https://www.beckershospitalreview.com/quality/icu-liberation-optimizing-quality-and-efficiency-of-critical-care-delivery.html. Accessed April 5, 2020.
Gabbard ER, Klein D, Vollman K, Chamblee TB, Soltis LM, Zellinger M. Clinical nurse specialist: a critical member of the ICU team. Crit Care Med. 2021;49(6):e634–41.
Calabresi P, Nigro P, Schwarz HB. A nurse-led model increases quality of care in Parkinson disease. Neurology. 2019;92(16):739–40.
Lamas D. Nurse-led communication in the Intensive Care Unit. N Engl J Med. 2018;378(25):2431–2.
Gonçalves MIR, Mendes DA, Caldeira S, Jesus E, Nunes E. Nurse-led care management models for patients with multimorbidity in hospital settings: a scoping review. J Nurs Manag. 2022;30(6):1960–73.
Ruiz Hernandez C, Gomez-Urquiza JL, Pradas-Hernandez L, Vargas Roman K, Suleiman-Martos N, Albendin-Garcia L. Canadas-De La Fuente GA: effectiveness of nursing interventions for preoperative anxiety in adults: a systematic review with meta-analysis. J Adv Nurs. 2021;77(8):3274–85.
Carney M. International perspectives on Advanced nurse and Midwife Practice, regarding advanced practice, criteria for posts and persons and requirements for regulation of Advanced Nurse/Midwife practice. Undertaken for nursing and Midwives Board of Ireland (NMBI). Dublin: Nursing and Midwifery Board of Ireland; 2014.
Connolly C, Cotter P. Effectiveness of nurse-led clinics on healthcare delivery: an umbrella review. J Clin Nurs. 2023;32(9–10):1760–7.
Acknowledgements
We thank Pro. Roger Watson from Southwest Medical University for his excellent assistance in English language review.
Funding
The study was funded by 1.3.5 project for disciplines of excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (2019HXFH006).
Author information
Authors and Affiliations
Contributions
YL and JLC designed and conducted information retrieval, statistical analysis and writing the manuscript. WTK and PFL assisted in collecting the data and extracted and reviewed the data. JBH and WBY took charge of preparation and presentation of the published work, specifically visualization presentation. NN and HC supervised the design, reviewed the results, and revised the manuscript. All authors listed meet the author eligibility criteria according to the latest guidelines of the International Committee of Medical Journal Editors (ICMJE). All authors agreed with the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Research Ethics Committee of the Institutional Review Board (2017 (Review) No. 128). We did not require informed consent according to the study design. Hence informed consent was waived by the Research Ethics Committee of the Institutional Review Board (2017 (Review) No. 128). This study was conducted in accordance to the relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Chen, J., Wu, T. et al. Effects of nurses-led multidisciplinary-based psychological management in spinal surgery: a retrospective, propensity-score-matching comparative study. BMC Nurs 23, 217 (2024). https://doi.org/10.1186/s12912-024-01842-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-01842-y