Abstract
Background
Bedside teaching is an important modality for training medical students and postgraduate trainees in clinical settings. Despite its significance, the effective practice of Bedside teaching has been declining over the past few decades. The literature highlighted the need for structured training, assessment, and certification or in other words entrustment of bedside teachers. The current study aims to develop and validate the Entrustable Professional Activities (EPAs) for bedside clinical teachers.
Methods
A multi-method study with clinical teachers, medical educationists, and postgraduate medical students was conducted from July 2021-22. First, a nominal group using the jigsaw puzzle technique was conducted with 16 participants to identify EPAs. Then these EPAs were mapped and validated by the skills/competencies identified in the literature. Next, the EPAs were evaluated using the EQual rubric by 3 medical educationists. This was followed by two-rounds of modified Delphi to develop consensus among 90 participants in round-one and 69 in round-two. For qualitative data, a thematic analysis was conducted. For quantitative data, means and standard deviations were calculated.
Results
The study identified five EPAs for bedside clinical teachers: developing bedside teaching program, planning bedside teaching session, conducting bedside teaching, conducting bedside assessments and evaluating bedside teaching.
Conclusions
This study comprehensively developed and validated a full description of EPAs for bedside clinical teachers. The EPAs identified in the study can serve as a guiding framework for bedside clinical teachers’ training, assessment, and entrustment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Bedside teaching (BST) is one of the most important aspects of undergraduate and postgraduate medical education [1] It allows learners to develop effective history-taking, physical examinations, clinical reasoning, communication and problem-solving skills in real life clinical settings [2] BST also helps in learning professionalism and medical ethics. Despite its significance, the effective practice of BST has been declining over the past few decades [1]. Several reasons have been cited for its decline such as a lack of resources and incentives by hospitals, patients’ discomfort and their unavailability during rounds, increased advancements in technology, increased workload of clinicians, and most importantly their lack of training for BST [3]. Many clinical teachers learn to teach BST through observation and experimentation and remain ignorant of the educational theories, andragogical principles, and teaching methods [1, 3, 4].
Over the last few decades, there have been expectations from clinical teachers to develop certain educational competencies for effective clinical teaching. In this regard, various educational competency frameworks, guidelines, and training programs have been introduced globally. Literature described several competency frameworks for faculty members such as those proposed by Hesketh et al., [5] Tigelaar et al., [6] Molenaar et al., [7] Milner et al., [8] Hatem et al., [9] Srinivasan et al., [10] Ross et al., [11] Daouk-Oyry et al., [12] and Walsh et al. [13]. However, these frameworks do not guide the teachers on implementing them in their context. Several guidelines for providing effective clinical supervision such as Recognizing and approving trainers by General Medical Council (UK) [14]; the American Psychological Association’s Guidelines for Clinical Supervision of Health Service Psychologists [15]; the New Zealand Psychologists Board Guidelines on Supervision [16]; and the Psychology Board of Australia Guidelines for Supervisors and Supervision Training Providers [17] are also available. There is also a clinician educator milestone project for the assessment of the educational skills of teaching faculty, which is a joint effort of the Accreditation Council for Graduate Medical Education, the Accreditation Council for Continuing Medical Education, the Association of American Medical Colleges, and the American Association of Colleges of Osteopathic Medicine [18]. In Pakistan, the College of Physicians and Surgeons [19] conducts four training workshops which are mandatory to become a clinical supervisor. Unfortunately, these frameworks or trainings for clinical supervisors neither guarantee the transfer of training to the workplace nor ensure the maintenance of competence. Except for some developed countries such as USA, UK, and Canada [20], the educational competencies of clinical supervisors are not formally assessed in many countries.
Medical students and trainees have reported dissatisfaction with clinical teachers’ competence to understand the level of learners, observe patient-trainee encounters, provide a safe learning environment, demonstrate clinical tasks consistently, deliver constructive feedback, and encourage reflections [21,22,23] They reported experiencing opportunistic learning, which varies from one preceptor to another [24] This necessitates attention towards the selection, training, and preparation of clinical teachers for effective supervision of students [25, 26]. To develop, maintain, and bring continuous improvements in teaching competence, there is a need for structured training, assessments, and periodic certification of Bedside Clinical Teachers [25] or in other words Entrustment of Bedside Clinical Teachers.
Entrustable Professional Activities (EPAs) are defined as a set of professional tasks that can be fully entrusted to a learner to perform independently once they have attained the required specific competencies [27]. EPAs were first introduced in 2005 for graduate medical students [27]. Later, the use of EPAs has been increasingly taken up by various health professions with the intent to improve patient safety in the workplace [28]. EPAs embrace the concept of Competency-Based Medical Education (CBME) which in turn emphasizes the attainment and demonstration of required competencies that are crucial for job performance [29]. EPAs ground competencies in daily clinical practice & make them assessable. EPAs lay more emphasis on outcome-based, learner-centered, and skills-oriented flexible education, while less on time-barred training, which distinguishes it from the traditional training approaches [30]. Development of EPAs for BST can help inform faculty training in this important modality for training medical students. These can also be used for training of residents to reduce the burden of clinical teachers [31] The use of EPAs will also enhance the confidence, insight, and motivation of clinical teachers, while reducing the discomfort of patients and medical students in the process [25, 26]. Dewey et al., [25] proposed the use of EPAs for teaching faculty as well. Iqbal et al., [32] also emphasized on expanding EPAs for faculty training on specific teaching domains such as bedside teaching, mentoring, small group discussions, etc. In the literature, we could only find one study that developed an EPA for BST [33]. They used a focus group discussion and open-ended questionnaires via e-mail to collect participants’ perspectives on BST definitions and its essential features to develop an EPA for BST. However, their participants did not involve medical educationists who are the stakeholders in designing, implementing, and evaluating BST. Also, they did not use an EPA evaluation tool such as EQual rubric [34] for quality or ensured a national consensus or validation [35] of the final set of EPAs. The current study aims to develop and validate Entrustable Professional Activities (EPAs) for bedside clinical teachers through a rigorous multimethod approach.
Methods
A multi-method study was conducted in Pakistan from July 2021 - July 2022 (Fig. 1). Ethical approval was obtained from the Ethical Review Board of Medical Teaching Institution Abbottabad (Approval Code/Ref.No.RC-2022/EA-01/143 dated 24.05.2021). As an EPA expert has not been precisely defined in the literature, therefore we invited clinical teachers, medical educationists, and postgraduate medical students involved with BST for the study. Participants were selected through purposive maximum variation sampling. The inclusion criteria were set as clinical teachers with a relevant qualification of Member of College of Physicians and Surgeons (MCPS)/ Fellow of College of Physicians and Surgeons (FCPS), a minimum of three years’ field experience, and a designation of Assistant Professor or above. For medical educationists, a relevant qualification of Master in Health Professions Education (MHPE)/ PhD in Health Professions Education, a minimum of three years of experience, and a designation of Assistant Professor or above. Postgraduate students of any age, gender, specialty, and having willingness to participate in the study, were included. The participants were invited through a seminar and email including an information sheet and consent form.
Phase 1
In phase 1, we identified EPAs for BST. We invited 16 participants at Ayub Medical and Teaching Institution Abbottabad, which is a 1460-bedded tertiary care teaching hospital in Pakistan, and currently caters to around 1482 medical students and 546 postgraduate residents in different disciplines of Medicine, Surgery, and Dentistry. Participants were given orientation on study objectives. As the EPA concept was relatively novel to most of them, a detailed presentation encompassing substantial information on EPAs was given by the authors to ensure a common understanding among the participants. The first set of EPAs was developed using the Nominal Group Technique (NGT). In NGT, the experts are involved in independent activities and group interactions for quality ideas (in this research EPAs) generation and consensus development [36]. As part of NGT, a jigsaw puzzle technique [37] was used to generate EPAs’ description i.e., title; specifications and limitations; potential risks in case of failure; required competencies; required knowledge, skills, attitudes, and experience; resources for assessment; level of supervision and expiry period [38]. Jigsaw puzzle technique helped to develop a comprehensive description of all the EPAs through collaborative ideas of all participants in one session. Participants were grouped into four jigsaw groups, where each member of the group was tasked to develop the assigned aspect of EPAs description for all the EPAs. Members (from each jigsaw group) with the same assigned task were then regrouped as expert groups to discuss and compare their ideas with others. Next participants were returned to their original jigsaw groups, where they revised their descriptions to develop a full set of descriptions for all EPAs. Lastly, each group presented their sets of descriptions to other groups for discussion and clarification resulting in the final set of EPAs with descriptions.
Phase 2
The EPAs developed in phase 1 were then validated with the literature review [39]. A search was made with keywords (EPAs, bedside teaching, and clinical teachers) and by using their synonyms and various combinations in Medline, Embase, Cochrane, ERIC, ScienceDirect, and Google Scholar (Additional file 1). Inclusion criteria were set as full text, original articles, and systematic and scoping reviews in the English language with a focus on Medicine specialty. Search also involved controlled vocabulary and free text terms combined using Boolean operators ‘AND’ and ‘OR’.
Phase 3
In this phase, the EQual rubric was used to evaluate the structure and content of EPAs because it reliably measures the alignment of the key domains of EPAs with literature defined standards. It consists of 14 questions which are classified under three sub-scales: EPAs as discrete units of work; EPAs as entrustable, essential, and important tasks of the profession; and EPAs’ curricular role [34]. An online survey was created using QuestionPro® (Survey Analytics LLC, Beaverton, Oregon, USA) based on 14 items of the EQual rubric along with three additional questions regarding EPAs improvement (Additional file 2). An orientation video on the EQual rubric was also inserted into the first page of the survey for participants’ guidance [40]. A modified Angoff approach was used for the determination of a cut-off score of 3.95 for EPAs adequacy. Three expert medical educationists with qualifications and experience in clinical teaching and medical education reviewed each EPA using the rubric.
Data was analyzed using means, standard deviations, and level of agreement for each EPA. Free text comments were summarized as standalone qualitative data [41]. Changes were made when suggested by at least two experts for items with mean scores below 3.95.
Phase 4
This phase used a modified Delphi technique to seek national consensus on EPAs identified in the earlier phases [42]. Participants of this phase included clinical teachers and postgraduate students from multiple specialties as well as medical educationists. By using purposive maximum variation sampling, participants across Pakistan with known contacts were sent invitations through emails for participation. To increase the sample size, we also employed snowball sampling which is a non-probability sampling method and involves asking initially willing participants to suggest other diverse and information-rich participants with similar characteristics from among their acquaintances. Participants’ number reached 90, which is considered appropriate in Delphi studies involving diverse groups [41].
A piloted and electronically developed questionnaire via QuestionPro was distributed to participants in two rounds. Participants were provided with AMEE Guide No.140 on recommended description of an EPA, to use as a reference guide [38]. Participants’ agreement was asked on a 5-point Likert scale from strongly agree to strongly disagree. Round-one survey’s first part was about participants’ demographics and the second part had two sections, A and B. Section A consisted of seven questions repeated for each EPA. The first six questions were about participants’ agreement on the provided title; specifications; limitations; potential risks in case of failure; competencies; and knowledge, skills, and attitude, while the seventh question asked for suggestions for improvements. Section B had four questions. The first two questions asked for participants’ agreement on the provided EPA level and required resources of entrustment. The last two questions asked for participants’ comments on the expiry period and suggestions on the overall EPAs’ description (Additional file 3). Round-two survey had ten questions for EPAs’ descriptions, which received below 80% agreement or had major revisions based on round-one (Additional file 4).
Data were analyzed using means, standard deviations, and level of agreements. The consensus was set as ≥ 80% agreement for a minimum score of 4 out of 5 on a 5-point Likert scale. Suggestions were incorporated when recommended by at least two participants and after thorough review and discussions amongst the authors.
Results
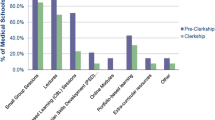
Initial 16 EPAs were refined through different phases into 5 EPAs. Demographic details of participants who were clinical teachers, medical educationists, and postgraduate medical students are given in Table 1. Participants belonged to a diverse range of specialties and from different cities grouped into four provinces of Pakistan.
Phase 1
The participants included 10 (62.5%) males and 6 (37.5%) females (Table 1). This phase resulted in a set of 16 EPAs and their descriptions (Table 2). However, a definitive consensus could not be obtained for the expiry period of EPAs, so it was included for comments in the round-one Delphi survey.
Phase 2
Five new EPAs i.e., EPAs 7, 12, 17, 20, and 21 were added via literature review through selected databases resulting in 21 EPAs (Table 2).
Phase 3
Of 21 EPAs, 11 made below the 3.95 cut-off score and were nested with other EPAs as suggested by the participants resulting in 10 EPAs (Table 2).
Phase 4 - Delphi
Round-one
Of 144 invitees, 90 agreed to participate in the study. The response rate to round-one was 85.5%(77/90 responses). Four EPAs scored ≥ 80% agreements, while titles of six EPAs scored < 80% agreements. Modifications were also made to those EPAs’ descriptions that had already scored ≥ 80% agreement if suggested by at least two participants or with consensus among researchers reviewing the comments. Guided by participants’ feedback, EPAs 2, 6, and 10 were nested under the recommended title as “developing BST program”; EPAs 1 and 5 as “planning BST”, EPAs 3, 4, and 9 as “conducting BST”; EPA 8 was retained as “conducting BST assessments” and EPA 7 as “evaluating BST” resulting into five EPAs (Table 2). Levels of entrustment for all EPAs had scored > 80% agreement, so, it was not repeated in round-two. Regarding required resources for entrustment, “minutes of meeting” failed to achieve ≥ 80% agreement and was eliminated from the list (Summary of results of round-one of a modified delphi study is available as Additional file 5).
Round-two
Round-two was completed by 69 participants. Eight participants could not fill in the survey because of other commitments. The response rate for round-two was 89.6% (69/77 responses). In this round, all five EPAs, and their descriptions scored ≥ 80% agreement (Summary of the results of round-two of a modified Delphi study is available as Additional file 5 and 6) (Insert Table 2 here provided as a separate file of Tables 1 and 2).
Discussion
Five EPAs were developed through four phases of a multimethod approach for bedside teachers of both undergraduate and postgraduate students (Additional file 6). The primary set of 16 EPAs was gradually refined through these phases under the guidance of the participants’ feedback to a final set of five EPAs. Some EPAs were nested with others as sub-activities which is consistent with the literature, advocating EPAs to be broader in design that provide less detailed guidance to the trainee on their expected work [43].
Resulting EPAs are developing BST program, planning BST session, conducting BST, conducting bedside assessments, and evaluating BST. Each of these EPAs encompasses a full set of descriptions and requires standalone entrustment because a bedside teacher can attain certification for developing BST sessions, but is not yet able to plan or conduct BST.
First EPA ensured an organized and well-defined set of tasks for bedside teachers. It was related to planning and developing a complete BST program that encompassed the development of BST curriculum, study guides, assessment policies, written ethical guidelines, feedback, and evaluation forms in collaboration with all stakeholders. It also included a suggestion from a participant of round-two Delphi to use an evidence-based approach while designing the BST curriculum as supported by literature studies [44,45,46,47,48] Second EPA was planning individual BST sessions for ensuring timely and smooth information delivery to students. It included lesson planning, pre-briefing the patients, and orienting the students before BST [33, 49, 50] Participants endorsed this EPA in avoiding untoward situations between doctors and patients or their attendants. Third EPA incorporated steps for BST conduction based on principles of evidence-based teaching and this was in line with previous studies [51,52,53] Fourth EPA is the ability of bedside teachers to design and conduct standardized assessments using multiple workplace-based assessment tools [54, 55]. This is important because carefully designed assessments lead to professional competence in medical students. The last EPA encompassed tasks related to the evaluation of BST sessions and program, vital for any ongoing dynamic process. This EPA will serve to bring improvements in the overall EPAs structure by identifying BST tasks not yet recognizable in this study. Nearly all study participants deemed these EPAs important, but they also pointed out that these tasks might not be practical in terms of bigger workload of clinical faculty.
Only one study in the literature developed EPA for BST [33]. However that study did not involve diverse stakeholders including medical educationaists and only used focus group discussion and survey for developing BST definitions and features. On the other hand, the current study involved medical educationists involved in professional development, clinical teachers and postgraduate students and used a four-phased multimethod approach for EPAs development and validation [56]. Moreover, this study also focused on the development of a full set of descriptions of individual EPAs [38] to provide explicit details for bedside teachers training programs. Also, Participants chose competency domains required for each EPA from the teaching competency framework for the medical educators proposed by Srinivasan et al., [10] We have used this framework because it included six core competencies, based on the ACGME competencies framework: medical knowledge; learner-centeredness; interpersonal and communication skills; professionalism and role modeling; practice-based reflection; and systems-based practice and four specialized competencies: program design/implementation, evaluation/scholarship, leadership, and mentorship. These competencies were also cross-referenced with educator roles, from CanMEDS, to ascertain role-specific skills [10].
For summative entrustment, bedside teachers need to be evaluated by experts using multiple assessment methods at various stages of their training and professional development. Assessment methods which are also supported by other studies include direct observation [57] 360◦ feedback [58] reflective portfolio [59] Objective Structured Teaching Examinations [60] etc. This study used three instead of the original five entrustment levels as proposed for small group facilitators [61]. Levels of indirect supervision and entrusted to supervise others had not been used as indirect supervision may not be instantly available to teachers during an ongoing session, and without additional courses, a teacher is not competent enough to train other teachers [61]. It is our opinion that an EPA may expire if bedside teachers do not undergo appraisals for three consecutive years. This is because, unlike clinical skills, teaching skills may not immediately decay over time but would need re-entrustment after the expiry.
Implications
These EPAs can empower bedside teachers for capacity building by recognizing gaps in their BST practice and accordingly improving them. This would also benefit students, patients, program developers, and medical institutions. As recommended for EPA-based programs [38] this study also entailed that experienced teachers should train, and assess beginner levels and give appraisals to them for their performance. Teachers can then be awarded certification for independent BST after attaining the required entrustment level. As suggested, a ‘statement of awarded responsibility’ (STAR) can be given to a teacher achieving adequate expertise in an EPA [25] to signify that a certain task has now been entrusted to the awarded teacher to be performed proficiently. Entrusted teachers can be given reasonable points for the attained STARs to be used for recruitment and promotion [62] These EPAs can also be adopted as structured faculty development or continuing professional development programs to operationalize BST training at the workplace [63].
The strength of this study was that to our knowledge, it is the first study that used a multimethod approach to develop and validate a full set of descriptions of EPAs for bedside teachers in collaboration with clinical teachers, medical educationists, and postgraduate students to maximally accommodate their requirements and perspectives. This study design can serve as a guide for other researchers to develop EPAs in other fields.
This study also had some limitations. The study was confined to the context of Pakistan where EPAs’ concept is relatively novel and the majority of the participants had minimal prior experience of EPAs development. However, we tried to cope with this limitation, by providing substantial information on EPAs to the participants before each phase and throughout the study whenever required. Participants were mainly selected for their experience with BST. However, there is still a possibility of lacking one or more items in EPAs description relevant to work of bedside teachers, necessitating these EPAs to be field tested, revisited, and modified if required. Regarding the limitation section in EPAs description, the majority of participants of round-one Delphi misunderstood it as barriers of BST, therefore, their comments were not included. Although this was clarified to them again in round-two, however, some participants commented that limitations can be better identified once EPAs are executed. This study only focused on BST, therefore, its findings would be difficult to generalize to other teaching settings.
Conclusions
This study comprehensively developed and validated a full description of EPAs for bedside clinical teachers. The EPAs identified in the study can serve as a guiding framework for the training, assessment, and entrustment of bedside clinical teachers. Future research should explore the long-term impact of implementing EPAs on bedside clinical teachers’ performance, student outcomes, and overall patient safety.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- AMEE:
-
The International Association for Medical Education
- BST:
-
Bedside Teaching
- CBME:
-
Competency Based Medical Education
- EPA:
-
Entrustable Professional Activities
- ERIC:
-
Education Resources Information Center
- FCPS:
-
Fellow Of College of Physicians and Surgeons
- JPT:
-
Jigsaw Puzzle Technique
- MCPS:
-
Member Of College of Physicians and Surgeons
- MHPE:
-
Masters In Health Professions Education
- NGT:
-
Nominal Group Technique
- PhD:
-
Doctor Of Philosophy
- STAR:
-
Statement of Awarded Responsibility
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Peters M, ten Cate O. Bedside teaching in medical education: a literature review. Perspect Med Educ. 2014;3(2):76–88.
Carlos WG, Kritek PA, Clay AS, Luks AM, Thomson CC. Teaching at the bedside maximal impact in minimal time. Ann Am Thorac Soc. 2016;13(4):545–8.
Rousseau M, Könings KD, Touchie C. Overcoming the barriers of teaching physical examination at the bedside: more than just curriculum design. BMC Med Educ. 2018;18(1):1–11.
Harden RM, Crosby J. AMEE guide 20: the good teacher is more than a lecturer - the twelve roles of the teacher. Med Teach. 2000;22(4):334–47.
Hesketh EA, Bagnall G, Buckley EG, Friedman M, Goodall E, Harden RM, et al. A framework for developing excellence as a clinical educator. Med Educ. 2001;35(6):555–64.
Tigelaar D, Dolmans D, Wolfhagen I, Van der Vleuten C. The development and validation of a framework for teaching competencies in higher education. High Educ (Dordr). 2004;48:253–68.
Molenaar WM, Zanting A, Van Beukelen P, De Grave W, Baane JA, Bustraan JA, et al. A framework of teaching competencies across the medical education continuum. Med Teach. 2009;31(5):390–6.
Milner RJ, Gusic ME, Thorndyke LE, Perspective. Toward a competency framework for faculty. Academic Medicine. Volume 86. Lippincott Williams and Wilkins; 2011. pp. 1204–10.
Hatem CJ, Searle NS, Gunderman R, Krane NK, Perkowski L, Schutze GE, et al. The educational attributes and responsibilities of effective medical educators. Acad Med. 2011;86(4):474–80.
Srinivasan M, Li STT, Meyers FJ, Pratt DD, Collins JB, Braddock C, et al. Teaching as a competency: competencies for medical educators. Acad Med. 2011;86(10):1211–20.
Ross MT, Macrae C, Scott J, Renwick L, Moffat M, Needham G, et al. Core competencies in teaching and training for doctors in Scotland: a review of the literature and stakeholder survey. Med Teach. 2014;36(6):527–38.
Daouk-Öyry L, Zaatari G, Sahakian T, Rahal Alameh B, Mansour N. Developing a competency framework for academic physicians. Med Teach. 2017;39(3):269–77.
Walsh A, Koppula S, Antao V, Bethune C, Cameron S, Cavett T, et al. Preparing teachers for competency-based medical education: fundamental teaching activities. Med Teach. 2018;40(1):80–5.
The General Medical Council. Recognising and approving trainers: the implementation plan. Gen Med Council. 2012;(August).
Doll B, Ellis M, Goodyear RK, Mccutcheon S, Miville M, Directorate E. Guidelines for clinical supervision in health service psychology. Am Psychol. 2015;70(1):33–46.
New Zealand Psychologists Board. Guidelines Superv. 2021;1–40.
Psychology Board of Australia. Guidelines for supervisors and supervisión training providers. 2018;(August).
Clinician Educator Milestones. Accreditation Council for Graduate Medical Education.
College of Physicians and Surgeons Pakistan [Internet]. Karachi: Training guidelines; [updated 2022; cited 2022 Feb 5].
Falender CA. Ethics of clinical supervision: an international lens. Psychol Russia: State Art. 2020;13(1):42–53.
Orakzai GS, Sethi A, Victor G, Aamir HS. Clinical supervision: what do the supervisors and residents think? Prof Med J. 2020;27(11):2529–36.
Stephan A, Cheung G. Clinical teaching and supervision in postgraduate psychiatry training: the trainee perspective. Australasian Psychiatry. 2017;25(2):191–7.
Boerboom TBB, Mainhard T, Dolmans DHJM, Scherpbier AJJA, Van Beukelen P, Jaarsma ADC. Evaluating clinical teachers with the Maastricht clinical teaching questionnaire: how much teacher is in student ratings? Med Teach. 2012;34(4):320–6.
Rousseau M, Könings KD, Touchie C. Overcoming the barriers of teaching physical examination at the bedside: more than just curriculum design. BMC Med Educ. 2018;18(1):1–10.
Dewey CM, Jonker G, ten Cate O, Turner TL. Entrustable professional activities (EPAs) for teachers in medical education: has the time come? Med Teach. 2017;39(8):894–6.
Iqbal MZ, Al-Eraky M. Using entrustable professional activities (EPAs) to assess teaching competence and transfer of training: a personal view. Med Teach. 2019;41(1):107–8.
Ten Cate O. Entrustability of professional activities and competency-based training. Med Educ. 2005;39(12):1176–7.
Ten Cate O, Taylor DR. The recommended description of an entrustable professional activity: AMEE Guide No. 140. Med Teach [Internet]. 2021;43(10):1106–14. https://doi.org/10.1080/0142159X.2020.1838465
Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR. A call to action: the controversy of and rationale for competency-based medical education. Med Teach. 2017;39(6):574–81.
Frank JR, Snell LS, Cate O, Ten, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–45.
Rana J, Sullivan A, Brett M, Weinstein AR, Atkins KM. Defining curricular priorities for student-as-teacher programs: a National Delphi Study. Med Teach. 2018;40(3):259–66.
Iqbal MZ, Könings KD, Al-Eraky M, AlSheikh MH, van Merrienboer JJG. Development of an entrustable professional activities (EPAs) framework for small group facilitators through a participatory design approach. Med Educ Online. 2020;25(1).
van Dam M, Ramani S, ten Cate O. An EPA for better Bedside Teaching. Clin Teacher. 2021;18(4):398–403.
Taylor DR, Park YS, Egan R, Chan MK, Karpinski J, Touchie C, et al. EQual, a Novel Rubric to Evaluate Entrustable Professional activities for Quality and structure. Acad Med. 2017;92(null):S110–7.
Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz LA, Mascioli K, et al. The Use of the Delphi and Other Consensus Group Methods in Medical Education Research: a review. Acad Med. 2017;92(10):1491–8.
O’Neil MJ, Jackson L. Nominal group technique: a process for initiating curriculum development in higher education. Stud High Educ. 1983;8(2):129–38.
Jeppu AK, Kumar KA, Sethi A. We work together as a group’: implications of jigsaw cooperative learning. BMC Med Educ. 2023;23(1):734.
Ten Cate O, Taylor DR. The recommended description of an entrustable professional activity: AMEE Guide 140. Med Teach. 2020;43(10):1106–14.
Haig A, Dozier M. BEME Guide 3: systematic searching for evidence in medical education - part 2: constructing searches. Med Teach. 2003;25:463–84.
Queen’s DOM Medical Education. EQual rubric training video for EPA evaluation. 2017.
LaDonna KA, Taylor T, Lingard L. Why open-ended survey questions are unlikely to support rigorous qualitative insights. Acad Med. 2018;93(3):347–9.
Humphrey-Murto S, Varpio L, Gonsalves C, Wood TJ. Using consensus group methods such as Delphi and Nominal Group in medical education research. Med Teach. 2017;39(1):14–9.
Taylor D, Park YS, Smith C, ten Cate O, Tekian A. Constructing approaches to Entrustable Professional Activity Development that deliver valid descriptions of Professional Practice. Teach Learn Med. 2020;1–9.
Dorsch JL, Aiyer MK, Meyer LE. Impact of an evidence-based medicine curriculum on medical students’ attitudes and skills. J Med Libr Association. 2004;92(4):397–406.
Glasziou P, Burls A, Gilbert R. Evidence based medicine and the medical curriculum. BMJ. 2008;337(7672):704–5.
Ilic D, Forbes K. Undergraduate medical student perceptions and use of evidence based Medicine: a qualitative study. BMC Med Educ. 2010;10(1).
Pammi M, Lingappan K, Carbajal MM, Suresh GK. Focused evidence-based Medicine Curriculum for trainees in Neonatal-Perinatal Medicine. MedEdPORTAL. 2017;13:10664.
Natesan S, Bailitz J, King A, Krzyzaniak SM, Kennedy SK, Kim AJ, et al. Clinical teaching: an evidence-based guide to best practices from the council of emergency medicine residency directors. Western J Emerg Med. 2020;21(4):985–98.
Ramani S. Twelve tips to improve bedside teaching. Med Teach. 2003;25(2):112–5.
Ramani S, Leinster S. AMEE guide 34: teaching in the clinical environment. Med Teach. 2008;30(4):347–64.
Groccia J, Buskist W. Need for evidence-based teaching. New Dir Teach Learn. (128):5–11.
Davies P. Approaches to evidence based Medicine. Med Teach. 2000;22(1):14–21.
Emplit P, Zhang T. Evidence-based approaches to learning and teaching Thematic Peer Group Report. Belgium; 2020.
Kurniawan C, Nainggolan MM, Sebayang K, Ginting M, Sebayang P. Assessment methods in medical education. Int J Health Sci (Qassim). 2(2):3–7.
Rege N. Principles of assessment in medical education: a review of revised second edition. Int J Appl Basic Med Res. 2022;12(1):67–9.
Ten Cate O, Chen HC, Hoff RG, Peters H, Bok H, Van Der Schaaf M. Curriculum development for the workplace using Entrustable Professional activities (EPAs): AMEE Guide 99. Med Teach. 2015;37(11):983–1002.
Finkelstein S, Sharma U, Furlonger B. The inclusive practices of classroom teachers: a scoping review and thematic analysis. Int J Incl Educ. 2021;25(6):735–62.
Berk RA. Using the 360° multisource feedback model to evaluate teaching and professionalism. Med Teach. 2009;31(12):1073–80.
Hong DZ, Lim AJS, Tan R, Ong YT, Pisupati A, Chong EJX, et al. A systematic scoping review on portfolios of medical educators. J Med Educ Curric Dev. 2021;8:238212052110003.
Fakhouri S, Nunes M. Objective structured teaching examination (OSTE): an underused tool developed to assess clinical teaching skills. A narrative review of the literature. Sao Paulo Med J. 2019;137(2):193–200.
Iqbal MZ, Könings KD, Al-Eraky M, AlSheikh MH, van Merrienboer JJG. Entrustable Professional Activities for Small-Group Facilitation: A Validation Study Using Modified Delphi Technique. Teach Learn Med [Internet]. 2021;In press(0):1–10. https://doi.org/10.1080/10401334.2021.1877714
Bing-You RG, Holmboe E, Varaklis K, Linder J. Is it time for Entrustable Professional activities for Residency Program directors? Acad Med. 2017;92(6):739–42.
Shorey S, Lau TC, Lau ST, Ang E. Entrustable professional activities in health care education: a scoping review. Med Educ. 2019;53(8):766–77.
Acknowledgements
The authors would like to thank all the participants for their active contribution to this research project. We would also like to thank Dr. Najia Sajjad Khan and Dr. Anam Rafiq for their valuable feedback and support throughout the project. The study was conducted as part of First author’s MHPE dissertation under the supervision of Dr Ahsan Sethi.
Funding
None.
Author information
Authors and Affiliations
Contributions
AS conceptualized and designed the study. Both authors have made substantial contributions to the acquisition, analysis, and interpretation of data; as well as in writing, proofreading, and approving the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from Ethical Review Board of Medical Teaching Institution Abbottabad (Approval Code/Ref.No.RC-2022/EA-01/143 dated 24.05.2021) and informed written consent was taken from the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rafiq, A., Sethi, A. Entrustable professional activities for bedside clinical teachers. BMC Med Educ 24, 887 (2024). https://doi.org/10.1186/s12909-024-05876-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05876-3