Abstract
Background
Clinical reasoning (CR) is a crucial ability that can prevent errors in patient care. Despite its important role, CR is often not taught explicitly and, even when it is taught, typically not all aspects of this ability are addressed in health professions education. Recent research has shown the need for explicit teaching of CR for both students and teachers. To further develop the teaching and learning of CR we need to improve the understanding of students' and teachers' needs regarding content as well as teaching and assessment methods for a student and trainer CR curriculum.
Methods
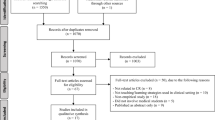
Parallel mixed-methods design that used web-surveys and semi-structured interviews to gather data from both students (nsurvey = 100; ninterviews = 13) and teachers (nsurvey = 112; ninterviews = 28). The interviews and surveys contained similar questions to allow for triangulation of the results. This study was conducted as part of the EU-funded project DID-ACT (https://did-act.eu).
Results
Both the surveys and interview data emphasized the need for content in a clinical reasoning (CR) curriculum such as “gathering, interpreting and synthesizing patient information”, “generating differential diagnoses”, “developing a diagnostic and a treatment plan” and “collaborative and interprofessional aspects of CR”. There was high agreement that case-based learning and simulations are most useful for teaching CR. Clinical and oral examinations were favored for the assessment of CR. The preferred format for a train-the-trainer (TTT)-course was blended learning. There was also some agreement between the survey and interview participants regarding contents of a TTT-course (e.g. teaching and assessment methods for CR). The interviewees placed special importance on interprofessional aspects also for the TTT-course.
Conclusions
We found some consensus on needed content, teaching and assessment methods for a student and TTT-course in CR. Future research could investigate the effects of CR curricula on desired outcomes, such as patient care.
Similar content being viewed by others
Introduction
Clinical reasoning (CR) is a universal ability that mobilizes integration of necessary fundamental knowledge while delivering high-quality patient care in a variety of contexts in a timely and effective way [1, 2]. Daniel et al. [3] define it as a “skill, process or outcome wherein clinicians observe, collect, and interpret data to diagnose and treat patients”. CR encompasses health professionals thinking and acting in patient assessment, diagnostic, and management processes in clinical situations, taking into account the patient ‘s specific circumstances and preferences [4]. How CR is defined can vary between health professions, but there are also similarities [5]. Poor CR is associated with low-quality patient care and increases the risk of medical errors [6]. Berner and Graber [7] suggested that the rate of diagnostic error is around 15%, underlining the threat that insufficient CR ability poses to patient safety as well as increasing healthcare costs [8]. Despite the importance of CR, it appears to be rarely taught or assessed explicitly, often only parts of the CR process are covered in existing curricula, and there seems to be a lack of progression throughout curricula (e.g. [9,10,11,12,13,14].). Moreover, teachers are often not trained to explicitly teach CR, including explaining their own reasoning to others [10,11,12] although this appears to be an important factor in the implementation of a CR curriculum [15]. Some teachers even question whether CR can be explicitly taught [16]. Considering these findings, efforts should be made to incorporate explicit teaching of CR into health care professions curricula and training for teachers should be established based on best evidence. However, to date, little is known about what a longitudinal CR curriculum should incorporate to meet the needs of teachers and students.
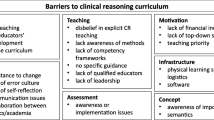
Insights regarding teaching CR were provided from a global survey by Kononowicz et al. [10], who reported a need for a longitudinal CR curriculum. However, the participants in their study were mainly health professions educators, leaving the needs of students for a CR curriculum largely unknown. As students are future participants of a CR curriculum, their needs should also be investigated. Kononowicz et al. [10] also identified a lack of qualified faculty to teach CR. A train-the-trainer course for CR could help reduce this barrier to teaching CR. To the best of our knowledge, in addition to the work by Kononowicz et al. [10], no research exists yet that addresses the needs of teachers for such a course, and Kononowicz et al. [10] did not investigate their needs beyond course content. Recently, Gupta et al. [12] and Gold et al. [13] conducted needs analyses regarding clinical reasoning instruction from the perspective of course directors at United States medical schools, yet a European perspective is missing. Thus, our research questions were the following:
-
1)
What aspects of clinical reasoning are currently taught and how important are they in a clinical reasoning curriculum according to teachers and students?
-
2)
What methods are currently used to teach and assess clinical reasoning and which methods would be ideal according to teachers and students?
-
3)
In what study year does the teaching of clinical reasoning currently begin and when should it ideally begin according to teachers and students?
-
4)
How should a train-the-trainer course for teachers of clinical reasoning be constructed regarding content and format?
Methods
Design
In this study, we used a convergent parallel mixed-methods design [17] within a pragmatic constructivist case study approach [18]. We simultaneously collected data from students and educators using online questionnaires and semi-structured interviews to gain deeper insight into their needs on one particular situation [19]– the development of a clinical reasoning curriculum—to address our research questions. To help ensure that the results of the survey and the interviews could be compared and integrated, we constructed the questions for the survey and the interviews similarly with the exception that in the interviews, the questions were first asked openly. The design was parallel both in that we collected data simultaneously and also constructed the survey and interviews to cover similar topics. We chose this approach to obtain comprehensive answers to the research questions and to facilitate later triangulation [17] of the results.
Context of this study
We conducted this study within the EU-funded (Erasmus + program) project DID-ACT (“Developing, implementing, and disseminating an adaptive clinical reasoning curriculum for healthcare students and educators”; https://did-act.eu). Institutions from six European countries (Augsburg University, Germany; Jagiellonian University in Kraków, Poland; Maribor University, Slovenia; Örebro University, Sweden; University of Bern, Switzerland; EDU, a higher medical education institution based in Malta, Instruct GmbH, Munich, Germany) with the support of associate partners (e.g., Prof. Steven Durning, Uniformed Services University of the Health Sciences, USA; Mälardalen University, Sweden.) were part of this project. For further information, see https://did-act.eu/team-overview/team/. In this project, we developed an interprofessional longitudinal clinical reasoning curriculum for students in healthcare education and a train-the-trainer course for health profession educators. The current curriculum (for a description of the curriculum, see Hege et al. [20]) was also informed by this study. This study was part of the Erasmus + Knowledge Alliance DID-ACT (612,454-EPP-1–2019-1-DE-EPPKA2-KA).
Target groups
We identified two relevant target groups for this study, teachers and students, which are potential future users and participants of a train—the—trainer (TTT-) course and a clinical reasoning curriculum, respectively. The teacher group also included individuals who were considered knowledgeable regarding the current status of clinical reasoning teaching and assessment at their institutions (e.g. curriculum managers). These specific participants were individually selected by the DID-ACT project team to help ensure that they had the desired level of expertise. The target groups included different health professions from a large number of countries (see Table 1), as we wanted to gather insights that are not restricted to one profession.
Development of data collection instruments
Development of questions
The questions in this study addressed the current status and needs regarding content, teaching, and assessment of clinical reasoning (CR). They were based on the questions used by Kononowicz et al. [10] and were expanded to obtain more detailed information. Specifically, regarding CR content, we added additional aspects (see Table 8 in the Appendix for details). The contents covered in this part of the study also align with the five domains of CR education (clinical reasoning concepts, history and physical examination, choosing and interpreting diagnostic tests, problem identification and management and shared decision-making) that were reported by Cooper et al. [14]. It has been shown that there are similarities between professions regarding the definition of CR (e.g. history taking or an emphasis on clinical skills), while nurses placed greater importance on a patient-centered approach [5]. We aimed to cover as many aspects of CR in the contents as possible to represent these findings. We expanded the questions on CR teaching formats to cover a broader range of formats. Furthermore, two additional assessment methods were added to the respective questions. Finally, one aspect was added to the content questions for a train-the-trainer course (see Table 8 in the Appendix). As a lack of qualified faculty to teach CR was identified in the study by Kononowicz et al. [10], we added additional questions on the specific needs for the design of a CR train-the-trainer course beyond content. Table 8 in the Appendix shows the adaptations that we made in detail.
We discussed the questions within the interprofessional DID-ACT project team and adapted them in several iterative cycles until the final versions of the survey questionnaire and the interview guide were obtained and agreed upon. We tested the pre-final versions with think-alouds [21] to ensure that the questions were understandable and interpreted as intended, which led to a few changes. The survey questionnaires and interview-guides can be found at https://did-act.eu/results/ and accessed via links in table sections D1.1a (survey questions) and D1.1b (interview guides), respectively. Of these questions, we included only those relevant to the research questions addressed in this study. The questions included in this study can be found in the Appendix in Table8.
Survey
Teachers were asked questions about all content areas, but only the expert subgroup was asked to answer questions on the current situation regarding the teaching and assessment of clinical reasoning at their institutions, as they were considered the best informed group on the matter. Furthermore, students were not asked questions on the train-the-trainer course. Using the abovementioned procedures, we also hoped to improve the response rate as longer surveys were found to be associated with lower response rates [22].
Interviews
We created two different versions of the interview guide, one for teachers and one for students. The student interview guide did not contain questions on the current status of clinical reasoning teaching and assessment or questions about the train-the-trainer course. The interview guides were prepared with detailed instructions to ensure that the interviews were conducted in a comparable manner at all locations. By using interviews, we intended to obtain a broad picture of existing needs. Individual interviews further allowed participants to speak their own languages and thus to express themselves naturally and as precisely as possible.
Reflexivity statement
Seven researchers representing different perspectives and professions form the study team. MS has been a PhD candidate representing the junior researcher perspective, while also experienced researchers with a broad background in clinical reasoning and qualitative as well as quantitative research are part of the team (SD, SH, AK, IH, ME, FW). ME represents the physiotherapist perspective, SD, SH, and MS represent the medical perspective. We discussed all steps of the study in the team and made joint decisions.
Data collection and analysis
Survey
The survey was created using LimeSurvey software (LimeSurvey GmbH). The survey links were distributed via e-mail (individual invitations, posts to institutional mailing lists, newsletters) by the DID-ACT project team and associate partners (the target groups received specific links to the online-survey). The e-mail contained information on the project and its goals. By individually contacting persons in the local language, we hoped to increase the likelihood of participation. The survey was anonymous. The data were collected from March to July 2020.
Interviews
Potential interview participants were contacted personally by the DID-ACT project team members in their respective countries. We used a convenience sampling approach by personally contacting potential interview partners in the local language to motivate as many participants as possible. With this approach we also hoped to increase the likelihood of participation. The interviews were conducted in the local languages also to avoid language barriers and were audio-recorded to help with the analysis and for documentation purposes. Most interviews were conducted using online meeting services (e.g. Skype or Zoom) because of restrictions due to the ongoing coronavirus pandemic that occurred with the start of data collection at the beginning of the DID-ACT project. The data were collected from March to July 2020. All interview partners provided informed consent.
Ethics approval and consent to participate
We asked the Bern Ethics Committee to approve this multi-institutional study. This type of study was regarded as exempt from formal ethical approval according to the regulations of the Bern Ethics Committee (‘Kantonale Ethikkommission Bern’, decision Req-2020–00074). All participants voluntarily participated and provided informed consent before taking part in this study.
Data analysis
Descriptive analyses were performed using SPSS statistics software (version 28, 2021). Independent samples t-tests were computed for comparisons between teachers and students. When the variances of the two groups were unequal, Welch’s test was used. Bonferroni correction of significance levels was used to counteract alpha error accumulation in repeated tests. The answers to the free text questions were screened for recurring themes. There were very few free-text comments, typically repeating aspects from the closed questions, hence, no meaningful analysis was possible. For this reason, the survey comments are mentioned only where they made a unique contribution to the results.
The interviews were translated into English by the partners. An overarching summarizing qualitative content analysis [23] of the data was conducted. A summarizing content analysis is particularly useful when the content level of the material is of interest. Its goal is to reduce the material to manageable short texts in a way that retains the essential meaning [23]. The analysis was conducted first by two of the authors of the study (FW, SH) and then discussed by the entire author team. The analysis was carried out as an iterative process until a complete consensus was reached within the author team.
The results from the surveys and interviews were compared and are presented together in the results section. The qualitative data are reported in accordance with the standards for reporting qualitative research (SRQR, O’Brien et al. [24]).
Results
Sample
Table 1 shows the professional background and country of the interviewees and survey samples. The survey was opened by 857 persons, 212 (25%) of whom answered the questions included in this study. The expert sub-group of teachers who answered the questions on the current status of clinical reasoning teaching and assessment encompassed 45 individuals.
Content of a clinical reasoning curriculum for students
The survey results show that “Gathering, interpreting, and synthesizing patient information”, is currently most extensively taught, while “Theories of clinical reasoning” are rarely taught (see Table 2). In accordance with these findings, “Gathering, interpreting, and synthesizing patient information” received the highest mean importance rating for a clinical reasoning curriculum while “Theories of clinical reasoning” received the lowest importance rating. Full results can be found in Table 9 in the Appendix.
Teachers and students differed significantly in their importance ratings of two content areas, “Gathering, interpreting, and synthesizing patient information” (t(148.32) = 4.294, p < 0.001, d = 0.609) and “Developing a problem formulation/hypothesis” (t(202) = 4.006, p < 0.001, d = 0.561), with teachers assigning greater importance to both of these content areas.
The results from the interviews are in line with those from the survey. Details can be found in Table 12 in the Appendix.
Clinical reasoning teaching methods
The survey participants reported that, most often, case-based learning is currently applied in the teaching of clinical reasoning (CR). This format was also rated as most important for teaching CR (see Table 3). Full results can be found in Table 10 in the Appendix.
Teachers and students differed significantly in their importance ratings of Team-based learning (t(202) = 3.079, p = 0.002, d = 0.431), with teachers assigning greater importance to this teaching format.
Overall, the interviewees provided very similar judgements to the survey participants. Next to the teaching formats shown in Table 3, some of them would employ blended learning, and clinical teaching formats such as bedside teaching and internships were also mentioned. Details can be found in the Appendix in Table 13. In addition to the importance of each individual teaching format, it was also argued that all of the formats can be useful because they all are meant to reach different objectives and that there is not one single best format for teaching CR.
Start of clinical reasoning teaching in curricula
Most teachers (52.5%) reported that currently, the teaching of clinical reasoning (CR) starts in the first year of study. Most often (46.4%) the participants also chose the first study year as the optimal year for starting the teaching CR. In accordance with the survey results, the interviewees also advocated for an early start of the teaching of CR. Some interview participants who advocated for a later start of CR teaching suggested that the students first need a solid knowledge base and that once the clinical/practical education starts, explicit teaching of CR should begin.
Assessment of clinical reasoning
The survey results suggest that currently written tests or clinical examinations are most often used, while Virtual Patients are used least often (see Table 4). Despite written tests being the most common current assessment format, they received the lowest importance rating for a future longitudinal CR curriculum. Full results can be found in Table 11 in the Appendix.
Teachers and students differed significantly in their importance ratings of clinical examinations (t(161.81) = 2.854, p = 0.005, d = 0.413) and workplace-based assessments (t(185) = 2.640, p = 0.009, d = 0.386) with teachers assigning greater importance to both of these assessment formats.
The interviewees also placed importance on all assessment methods but found it difficult to assess CR with written assessment methods. The students seemed to associate clinical examinations more with practical skills than with CR. Details can be found in the Appendix in Table 14. Two of the interview participants mentioned that CR is currently not assessed at their institutions, and one person mentioned that students are asked to self-reflect on their interactions with patients and on potential improvements.
Train-the-trainer course
The following sections highlight the results from the needs analysis regarding a train-the-trainer (TTT-) course. The questions presented here were posed only to the teachers.
Most survey participants reported that there is currently no TTT- course on clinical reasoning at their institution but that they think such a course is necessary (see Table 5). The same was also true for the interviewees (no TTT- course on clinical reasoning existing but need for one).
In the interviews, 22 participants (78.6%) answered that a TTT-course is necessary for healthcare educators, two participants answered that no such course was necessary, and two other participants were undecided about its necessity. At none of the institutions represented by the interviewees, a TTT-course for teaching clinical reasoning exists.
When asked what the best format for a clinical reasoning TTT- course would be (single answer question), the majority of the survey participants favored a blended learning / flipped classroom approach, a combination of e-learning and face-to-face meetings. (see Table 6).
In the survey comments it was noted that blended-learning encompasses the benefits of both self-directed learning and discussion/learning from others. It would further allow teachers to gather knowledge about CR first in an online learning phase where they can take the time they need before coming to a face-to-face meeting.
The interviewees also found a blended-learning approach particularly suitable for a TTT-course. An e-learning course only was seen as more critical because teachers may lack motivation to participate in an online-only setting, while a one-time face-to-face meeting would not provide enough time. In some interviews, it was emphasized that teachers should experience themselves what they are supposed to teach to the students and also that the trainers for the teachers need to have solid education and knowledge on clinical reasoning.
Table 7 shows the importance ratings of potential content of a TTT-course generated from the survey. To elaborate on this content, comments by the interviewees were added. On average, all content was seen as (somewhat) important with teaching methods on the ward and/or clinic receiving the highest ratings. Some interviewees also mentioned the importance of interprofessional aspects and interdisciplinary understanding of CR. In the survey comments, some participants further expressed their interest in such a course.
Finally, the interviewees were asked about the ideal length of a clinical reasoning TTT-course. The answers varied greatly from 2–3 hours to a two-year educational program, with a tendency toward 1–2 days. Several interviewees commented that the time teachers are able to spend on a TTT-course is limited. This should be considered in the planning of such a course to make participation feasible for teachers.
Discussion
In this study, we investigated the current status of and suggestions for teaching and assessment of clinical reasoning (CR) in a longitudinal curriculum as well as suggestions for a train-the-trainer (TTT-) course for CR. Teachers and students were invited to participate in online-surveys as well as semi-structured interviews to derive answers to our research questions. Regarding the contents of a CR curriculum for students, the results of the surveys and interviews were comparable and favoured content such as gathering, interpreting, and synthesizing patient information, generating differential diagnoses, and developing a diagnostic and a treatment plan. In the interviews, high importance was additionally placed on collaborative and interprofessional aspects of CR. Case-based learning and simulations were seen as the most useful methods for teaching CR, and clinical and oral examinations were favoured for the assessment of CR. The preferred format for a TTT-course was blended learning. In terms of course content, teaching and assessment methods for CR were emphasized. In addition to research from the North American region [11], this study provides results from predominantly European countries that support the existing findings.
Content of a clinical reasoning curriculum
Our results revealed that there are still aspects of clinical reasoning (CR), such as “Errors in the clinical reasoning process and strategies to avoid them” or “Interprofessional aspects of CR” that are rarely taught despite their high importance, corroborating the findings of Kononowicz et al. [10]. According to the interviewees, students should have basic knowledge of CR before they are taught about errors in the CR process and strategies to avoid them. The lack of teaching of errors in CR may also stem from a lack of institutional culture regarding how to manage failures in a constructive way (e.g. [16, 25]), making it difficult to explicitly address errors and strategies to avoid them. Although highly relevant in the everyday practice of healthcare professions and underpinned by CR theoretical frameworks (e.g., distributed cognition [26]), interprofessional and collaborative aspects of CR are currently rarely considered in the teaching of CR. The interviews suggested that hierarchical distance and cultural barriers may contribute to this finding. Sudacka et al. [16] also reported cultural barriers as one reason for a lack of CR teaching. Generally, the interviewees seemed to place greater importance on interprofessional and collaborative aspects than did the survey-participants This may have been due to differences in the professions represented in the two modalities (e.g., a greater percentage of nurses among the interview participants, who tend to define CR more broadly than physicians [5]).
“Self-reflection on clinical reasoning performance and strategies for future improvement”, “Developing a problem formulation/hypothesis” and “Aspects of patient-participation in CR” were rated as important but are currently rarely taught, a finding not previously reported. The aspect “Self-reflection on clinical reasoning performance and strategies for future improvement”, received high importance ratings, but only 25% of the survey-participants answered that it is currently taught to a great extent. The interviewees agreed that self-reflection is important and added that ideally, it should be guided by specific questions. Ogdie et al. [27] found that reflective writing exercises helped students identify errors in their reasoning and biases that contributed to these errors.
“Gathering, interpreting, and synthesizing patient information” and “Developing a problem formulation/hypothesis” were rated significantly more important by teachers than by students. It appears that students may be less aware yet of the importance of gathering, interpreting, and synthesizing patient information in the clinical reasoning process. There was some indication in the interviews that the students may not have had enough experience yet with “Developing a problem formulation/hypothesis” or associate this aspect with research, possibly contributing to the observed difference.
Overall, our results on the contents of a CR curriculum suggest that all content is important and should be included in a CR curriculum, starting with basic theoretical knowledge and data gathering to more advanced aspects such as errors in CR and collaboration. Two other recent surveys conducted in the United States among pre-clerkship clinical skills course directors [12] and members of clerkship organizations [13] came to similar conclusions regarding the inclusion of clinical reasoning content at various stages of medical curricula. How to fit the content into already dense study programs, however, can still be a challenge [16].
Clinical reasoning teaching methods
In addition to case-based learning and clinical teaching, human simulated patients and Team-based learning also received high importance ratings for teaching clinical reasoning (CR), a finding not previously reported. Lectures, on the other hand, are seen as the least important to teach CR (see also Kononowicz et al. [10]), as they mainly deliver factual knowledge according to the interviewees. High-fidelity simulations (mannequins) and Virtual Patients (VPs) are rarely used to teach CR at the moment and are rated less important compared to other teaching formats. Some interviewees see high-fidelity simulations as more useful for teaching practical skills. The lower importance rating of VPs was surprising given that this format is case-based, provides a safe environment for learning, and is described in the literature as a well-suited tool for teaching CR [28, 29]. Considering that VPs seemed to be used less often at the institutions involved in this study, the lack of experience with this format may have led to this result.
Teachers rated Team-based learning as significantly more important for teaching clinical reasoning than students. In the interviews, many students seemed not to be familiar with Team-based learning, possibly explaining the lower ratings the students gave this format in the survey.
Taken together, our results suggest that there is not one best format for teaching all aspects of clinical reasoning but rather that the use of all teaching formats is justified depending on the specific content to be taught and goals to be achieved. However, there was agreement that a safe learning environment where no patients can be harmed is preferred for teaching clinical reasoning, and that discussions should be possible.
There was wide agreement that clinical reasoning (CR) teaching should start in the first year of study in the curriculum. However, a few participants of this study argued that students first need to develop some general knowledge before CR is taught. Rencic et al. [11] reported that according to internal medicine clerkship directors, CR should be taught throughout all years of medical school, with a particular focus during the clinical teaching years. A similar remark was made by participants in a survey among pre-clerkship clinical skills course directors by Gupta et al. [12] where the current structure of some curricula (e.g. late introduction of the pathophysiology) was regarded as a barrier to introducing CR from the first year of study on [12].
Assessment of clinical reasoning
Our results show that the most important format for assessing clinical reasoning (CR) that is also currently used to the greatest extent are clinical examinations (e.g. OSCE), consistent with Kononowicz et al. [10]. The interviewees emphasized that CR should ideally be assessed in a conversation or discussion where the learners can explain their reasoning. Given this argument, all assessment formats enabling a conversation are suitable for assessing CR. This is reflected in our survey results, where assessment formats that allow for a discussion with the learner received the most favourable importance ratings, including oral examinations. In agreement with Kononowicz et al. [10], we also found that written tests are currently used most often to assess CR but are rated as least important and suitable only for the assessment of some aspects of CR. Daniel et al. [3] argued that written exams such as MCQs, where correct answers have to be selected from a list of choices, are not the best representation of real practical CR ability. Thus, there still seems to be potential for improvement in the way CR is assessed.
Teachers rated clinical examinations and workplace-based assessments significantly higher than students. Based on the interviews, the students seemed to associate clinical examinations such as OSCEs more with a focus on practical skills than CR, potentially explaining their lower ratings of this format.
What a clinical reasoning train-the-trainer course should look like
Our results show a clear need for a clinical reasoning (CR) train-the-trainer course (see also Singh et al. [15]), which currently does not exist at most institutions represented in this study, corroborating findings by Kononowicz et al. [10]. A lack of adequately trained teachers is a common barrier to the introduction of CR content into curricula [12, 16]. According to our results such a course should follow a blended learning/flipped classroom approach or consist of a series of face-to-face meetings. A blended-learning course would combine the benefits of both self-directed learning and the possibility for trainers to discuss with and learn from their peers, which could also increase their motivation to participate in such a course. An e-learning only course or a one-time face-to-face meeting were considered insufficient. The contents “Clinical reasoning strategies” and “Common errors in the clinical reasoning process” were given greater importance for the trainer-curriculum than for the students-curriculum, possibly reflecting higher expectations of trainers as “CR experts” compared with students. There was some agreement in the interviews that ideally, the course should not be too time-consuming, with participants tending towards an overall duration of 1–2 days, considering that most teachers usually have many duties and may not be able or willing to attend the course if it were too long. Lack of time was also identified as a barrier to attending teacher training [12, 13, 16].
Strengths and limitations
The strengths of this study include its international and interprofessional participants. Furthermore, we explicitly included teachers and students as target groups in the same study, which enables a comparison of different perspectives. Members of the target groups not only participated in a survey but were also interviewed to gain in-depth knowledge. A distinct strength of this study is its mixed-methods design. The two data collection methods employed in parallel provided convergent results, with responses from the web survey indicating global needs and semi-structured interviews contributing to a deeper understanding of the stakeholder groups’ nuanced expectations and perspectives on CR education.
This study is limited in that most answers came from physicians, making the results potentially less generalizable to other professions. Furthermore, there were participants from a great variety of countries, with some countries overrepresented. Because of the way the survey-invitations were distributed, the exact number of recipients is unknown, making it impossible to compute an exact response rate. Also, the response rate of the survey was rather low for individuals who opened the survey. Because the survey was anonymous, it cannot completely be ruled out that some individuals participated in both interviews and survey. Finally, there could have been some language issues in the interview analysis, as the data were translated to English at the local partner institutions before they were submitted for further analysis.
Conclusion
Our study provides evidence of an existing need for explicit clinical reasoning (CR) longitudinal teaching and dedicated CR teacher training. More specifically, there are aspects of CR that are rarely taught that our participants believe should be given priority, such as self-reflection on clinical reasoning performance and strategies for future improvement and aspects of patient participation in CR that have not been previously reported. Case-based learning and clinical teaching methods were again identified as the most important formats for teaching CR, while lectures were considered relevant only for certain aspects of CR. To assess CR, students should have to explain their reasoning, and assessment formats should be chosen accordingly. There was also still a clear need for a CR train-the-trainer course. In addition to existing research, our results show that such a course should ideally have a blended-learning format and should not be too time-consuming. The most important contents of the train-the-trainer course were confirmed to be teaching methods, CR strategies, and strategies to avoid errors in the CR process. Examples exist for what a longitudinal CR curriculum for students and a corresponding train-the-trainer course could look like and how these components could be integrated into existing curricula (e.g. DID-ACT curriculum [20], https://did-act.eu/integration-guide/ or the described curriculum of Singh et al. [15]). Further research should focus on whether and to what extent the intended outcomes of such a curriculum are actually reached, including the potential impact on patient care.
Availability of data and materials
All materials described in this manuscript generated during the current study are available from the corresponding author on reasonable request without breaching participant confidentiality.
References
Connor DM, Durning SJ, Rencic JJ. Clinical reasoning as a core competency. Acad Med. 2020;95:1166–71.
Young M, Szulewski A, Anderson R, Gomez-Garibello C, Thoma B, Monteiro S. Clinical reasoning in CanMEDS 2025. Can Med Educ J. 2023;14:58–62.
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, Gruppen LD. Clinical reasoning assessment methods: a scoping review and practical guidance. Acad Med. 2019;94:902–12.
Scott IA. Errors in clinical reasoning: causes and remedial strategies. BMJ. 2009. https://doi.org/10.1136/bmj.b1860.
Huesmann L, Sudacka M, Durning SJ, Georg C, Huwendiek S, Kononowicz AA, Schlegel C, Hege I. Clinical reasoning: what do nurses, physicians, and students reason about. J Interprof Care. 2023;37:990–8.
Norman GR, Eva KW. Diagnostic error and clinical reasoning. Med Educ. 2010;44:94–100.
Berner E, Graber M. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121:2–23.
Cooper N, Da Silva AL, Powell S. Teaching clinical reasoning. In: Cooper N, Frain J, editors. ABC of clinical reasoning. 1st ed. Hoboken, NJ: John Wiley & Sons Ltd; 2016. p. 44–50.
Elvén M, Welin E, Wiegleb Edström D, Petreski T, Szopa M, Durning SJ, Edelbring S. Clinical reasoning curricula in health professions education: a scoping review. J Med Educ Curric Dev. 2023. https://doi.org/10.1177/23821205231209093.
Kononowicz AA, Hege I, Edelbring S, Sobocan M, Huwendiek S, Durning SJ. The need for longitudinal clinical reasoning teaching and assessment: results of an international survey. Med Teach. 2020;42:457–62.
Rencic J, Trowbridge RL, Fagan M, Szauter K, Durning SJ. Clinical reasoning education at US medical schools: results from a national survey of internal medicine clerkship directors. J Gen Intern Med. 2017;32:1242–6.
Gupta S, Jackson JM, Appel JL, Ovitsh RK, Oza SK, Pinto-Powell R, Chow CJ, Roussel D. Perspectives on the current state of pre-clerkship clinical reasoning instruction in United States medical schools: a survey of clinical skills course directors. Diagnosis. 2021;9:59–68.
Gold JG, Knight CL, Christner JG, Mooney CE, Manthey DE, Lang VJ. Clinical reasoning education in the clerkship years: a cross-disciplinary national needs assessment. PLoS One. 2022;17:e0273250.
Cooper N, Bartlett M, Gay S, Hammond A, Lillicrap M, Matthan J, Singh M. UK Clinical Reasoning in Medical Education (CReME) consensus statement group. Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Med Teach. 2021;43:152–9.
Singh M, Collins L, Farrington R, Jones M, Thampy H, Watson P, Grundy J. From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. Diagnosis. 2021;9:184–94.
Sudacka M, Adler M, Durning SJ, Edelbring S, Frankowska A, Hartmann D, Hege I, Huwendiek S, Sobočan M, Thiessen N, Wagner FL, Kononowicz AA. Why is it so difficult to implement a longitudinal clinical reasoning curriculum? A multicenter interview study on the barriers perceived by European health professions educators. BMC Med Educ. 2021. https://doi.org/10.1186/s12909-021-02960-w.
Hingley A, Kavaliova A, Montgomery J, O’Barr G. Mixed methods designs. In: Creswell JW, editor. Educational research: planning, conducting, and evaluating quantitative and qualitative research. 4th ed. Boston: Pearson; 2012. p. 534–75.
Merriam SB. Qualitative research and case study applications in education. In: from" case study research in education.". Sansome St. Revised and Expanded. San Francisco, CA: Jossey-Bass Publishers; 1998.
Cleland J, MacLeod A, Ellaway RH. The curious case of case study research. Med Educ. 2021;55:1131–41.
Hege I, Adler M, Donath D, Durning SJ, Edelbring S, Elvén M, Wiegleb Edström D. Developing a European longitudinal and interprofessional curriculum for clinical reasoning. Diagnosis. 2023;10:218–24.
Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12:229–38.
Liu M, Wronski L. Examining completion rates in web surveys via over 25,000 real-world surveys. Soc Sci Comput Rev. 2018;36:116–24.
Mayring P, Fenzl T. Qualitative inhaltsanalyse. In: Baur N, Blasius J, editors. Handbuch methoden der empirischen Sozialforschung. Wiesbaden: Springer VS; 2019. p. 633–48.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89:1245–51.
Edmondson AC. Learning from failure in health care: frequent opportunities, pervasive barriers. BMJ Qual Saf. 2004;13 Suppl 2:ii3-ii9.
Merkebu J, Battistone M, McMains K, McOwen K, Witkop C, Konopasky A, Durning SJ. Situativity: a family of social cognitive theories for understanding clinical reasoning and diagnostic error. Diagnosis. 2020;7:169–76.
Ogdie AR, Reilly JB, Pang WG, Keddem S, Barg FK, Von Feldt JM, Myers JS. Seen through their eyes: residents’ reflections on the cognitive and contextual components of diagnostic errors in medicine. Acad Med. 2012;87:1361–7.
Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of medical education. Acad Med. 2016;91:1217–22.
Plackett R, Kassianos AP, Mylan S, Kambouri M, Raine R, Sheringham J. The effectiveness of using virtual patient educational tools to improve medical students’ clinical reasoning skills: a systematic review. BMC Med Educ. 2022. https://doi.org/10.1186/s12909-022-03410-x.
Acknowledgements
We want to thank all participants of the interviews and survey who took their time to contribute to this study despite the ongoing pandemic in 2020. Furthermore, we thank the members of the DID-ACT project team who supported collection and analysis of survey and interview data.
Disclaimer
The views expressed herein are those of the authors and not necessarily those of the Department of Defense, the Uniformed Services University or other Federal Agencies.
Funding
This study was partially supported by the Erasmus + Knowledge Alliance DID-ACT (612454-EPP-1–2019-1-DE-EPPKA2-KA).
Author information
Authors and Affiliations
Contributions
FW and SH wrote the first draft of the manuscript. All authors critically revised the manu-script in several rounds and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This type of study was regarded as exempt from formal ethical approval according to the regulations of the Bern Ethics Committee (‘Kantonale Ethikkommission Bern’, decision Req-2020–00074). All participants voluntarily participated and provided informed consent before taking part in this study.
Consent for publication
All authors consent to publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wagner, F., Sudacka, M., Kononowicz, A. et al. Current status and ongoing needs for the teaching and assessment of clinical reasoning – an international mixed-methods study from the students` and teachers` perspective. BMC Med Educ 24, 622 (2024). https://doi.org/10.1186/s12909-024-05518-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05518-8