Abstract
Introduction
Empathy is considered the ability to understand or feel others emotions or experiences. As an important part of medical education, empathy can affect medical students in many ways. It is still lacking a comprehensive evaluation of the existing articles on empathy’s impact on medical students, despite the existence of many articles on the topic.
Objectives
To summarize the impact of empathy on medical students during medical education from four perspectives: mental health, academic performance, clinical competence, and specialty preference.
Methods
The search terms used for retrieval were “empathy”, “medical student”, “mental health”, “depression”, “anxiety”, “burnout”, “examinations”, “academic performance”, “clinical competence”, “specialty preference” on PubMed, EBSCO, and Web of Science before January 2024. The search was carried out by two reviewers. Titles and abstracts were screened independently and reviewed based on inclusion/exclusion criteria. A consensus was drawn on which articles were included.
Results
Our results indicated that high empathy was a positive factor for mental health, However, students with high affective empathy were more likely to suffer from depression, anxiety, and burnout. Empathy was found to be unrelated to academic performance, but positively correlated with clinical competence, particularly in terms of communication skills. Medical students with high levels of empathy tended to prefer people-oriented majors.
Conclusions
Medical students who score higher on the self-reported empathy scales often have better mental health, better communication skills, and tend to choose people-oriented specialties. But empathy is not related to academic performance. Additionally, the different dimensions of empathy have different impacts on medical students. It is necessary to design targeted courses and training for medical students to enhance their empathy.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
The definition of empathy encompasses a wide range of social, cognitive, and affective processes, primarily involving the capacity to understand or feel the emotions or experiences of others [1]. Specifically, empathy enables us to resonate with the positive or negative emotions of others, meaning that when we indirectly share the happiness or pain of others, we also feel happy or painful. And due to empathy, people still know that the reason for their resonant feelings are the feelings of others, and do not confuse themselves with the feeling of others [2]. Furthermore, empathy is regarded as a multidimensional construct [3], comprising two main components: affective and cognitive empathy [4, 5]. Among them, affective empathy is defined as the capacity to respond emotionally to the mental states of others, which can be divided into empathic concern and personal distress [6]. While, cognitive empathy is a kind of capacity to understand the views or mental states of others [7], and can be subdivided into perspective-taking and fantasy. In addition, both congenital and acquired factors can influence an individual’s level of empathy [8].
From a medical perspective, empathy refers to the ability to understand and empathize with patients’ situations, perspectives, and feelings, enabling healthcare professionals to communicate effectively and provide treatment with the patients’ consent and assistance [9]. Therefore, empathy is a highly desirable trait in physicians, serving as a crucial component of the physician-patient relationship. It significantly influences both the diagnostic process and the delivery of treatment [10]. Patients who feel treated with empathy are more likely to fully explain their symptoms, provide relevant details, and actively engage in the patient-physician relationship [3, 11]. And, the empathy of physicians has positive impacts on gaining the trust of patients [12], effective communication [13], patient’s insistence on treatment [11], adherence to medical recommendations [14, 15], patient satisfaction [16,17,18], alleviating patient pain [19], improving treatment outcome [20, 21], and reducing potential legal risks [22, 23]. Empathy, in addition to its beneficial effects on patients, also has a profound impact on doctors and medical students, as it is closely tied to the well-being of physicians [24]. Doctors with lower levels of empathy are more likely to exhibit symptoms of stress and fatigue compared to their colleagues with higher levels of empathy [25]. Doctors with lower levels of empathy also experience higher levels of burnout and are more likely to be involved in medical accidents [26]. In addition, empathy is also related to the professional satisfaction of doctors [27]. All in all, empathy is beneficial for both patients and physicians, as emphasized by the General Medical Council in the United Kingdom [28] and the Association of American Medical Colleges [29] who have both underscored its importance in medical education for medical students. Besides, in order to provide high-quality patient care, the cultivation of medical affective should focus on both training medical skills and cultivating affective skills. Compared to clinical knowledge and skills, professional spirit and empathy are relatively more difficult to cultivate [30]. Considering that medical student, who officially become doctor after graduating from medical school, will constantly face emotional challenges such as pain, fear, and despair, cultivating and strengthening empathy is an important goal of medical education, aiming to prevent them from losing the ability to act professionally and ethically [31]. And a systematic review has shown that educational interventions can effectively maintain and enhance medical students’ empathy [32].
To assess individual empathy, researchers have developed a variety of scale tools, with the Jefferson Scale of Physician Empathy (JSPE) being a common measurement tool [33]. JSPE was originally developed to measure the empathy of medical students in patient care scenarios. In some versions, it is also referred to as the JSE. When compared to JSPE, the Interpersonal Reactivity Index (IRI) exhibits numerous differences in terms of its applicable population, measurement standards, and the conceptual and structural understanding of empathy. Specifically, IRI was developed for the general public, whereas JSPE was based on empathy in clinical settings and was developed for students and healthcare professionals. In addition, while the authors of IRI conceptualized empathy as a combination of cognitive and affective attributes, the authors of JSPE defined empathy as a cognitive attribute. These differences were reflected in the content of the project [34, 35]. Additionally, Baron-Cohen et al. proposed the Empathy Quotient, a tool designed to measure and quantify differences in empathy among individuals [36]. There are other measuring tools, such as the Questionnaire of Cognitive and Affective Empathy (QCAE) [37] and the Toronto Empathy Questionnaire, which are mostly used to measure the empathy of the general population [38].
Recently, Costa et al. reported that medical students’ empathy remained relatively stable throughout their medical education [39]. However, most studies examining the variation of empathy among medical students have demonstrated a tendency for empathy to decline during their medical school training. These researches originated from different countries, each possessing unique cultural systems, rather than being limited to a handful of nation [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. And, in most studies, gender has been found to be a predictor medical students’ empathy levels, with females typically exhibiting higher levels of empathy than males [62, 63]. More importantly, empathy is believed to significantly impact various aspects of medical students’ educational experience. Researchers in this field have studied the importance of empathy in the educational process and discovered that different dimensions of empathy exert distinct influences on students’ mental health, academic performance, clinical competence, and specialty preferences.
Although evidence on the impact of empathy on medical students is increasing, it should be noted that most studies examining the role empathy played in the development of medical students have not been comprehensive. For example, the researches of Thomas et al., and Carrard et al., studied the impact of empathy on the mental health among medical students [64, 65]. The study of Javaeed et al., investigated the impact of empathy on the academic performance [66]. A study discussed the impact of empathy on the clinical competence [67], while another study from Iran involved the impact of empathy on the academic performance and specialty preference [68]. It should be noted that most studies examining the role empathy played in the development of medical students were not comprehensive. Each individual study only involved one or two aspects about the impact of empathy on medical students. At present, there is a lack of comprehensive evaluation of the overall impact of empathy on medical students. Furthermore, some researchers considered empathy as a single construct [33, 42, 47, 52, 62, 68,69,70,71,72,73,74,75], ignoring its multiple dimensions.
Therefore, the research question of this integrative review is as follows:
How does empathy impact medical students’ mental health, academic performance, clinical competence, and specialty preferences?
Methods
We chose integrative review as the methodology to identify and synthesize the impact of empathy on medical students from literature. Integrative review allows researchers to combine experimental and non-experimental studies to fully understand theoretical aspects of the phenomenon analyzed. It also combines data from theoretical and empirical literature, and has a wide range of purposes, such as definition of concepts, review of theories and evidence, and analysis of methodological problems of a particular topic [76, 77]. While systematic review is an exacting synthesis of all investigations related to one specific question, focusing primarily on quantitative experimental studies, such as randomized clinical trials. It aims at overcoming possible biases in each stage, following a strict method to search and select investigations, assessing relevance and validity of the studies found [78]. Therefore, in order to extensively collect relevant references on the impact of empathy on medical students, we chose integrative review instead of a systematic review. We conducted this integrative review, using the methodological framework proposed by Whittemore and Knafl [76]. It involves the following stages: Problem identification, Literature search, Data evaluation, Data analysis and Presentation. Applied to this integrative review, each of these stages involved the following:
Problem identification
The primary problem that guided this review was “How does empathy influence medical students’ mental health, academic performance, clinical competence, and specialty preferences?”
Literature search
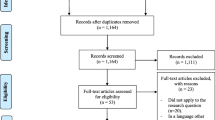
A search strategy was devised with input from the research team which was comprised of all authors. Two authors searched for articles on PubMed, EBSCO and Web of Science. The key search terms were “(empathy OR empathic OR empathetic) AND (medical student) AND (mental health OR depression OR anxiety OR burnout OR examination OR academic performance OR clinical competence OR specialty preference)”. A search process flowchart is shown in Fig. 1.
Data evaluation
We formulated the selection criteria for this review by combining the research question and the inclusion/exclusion criteria of the previous integrative reviews [79,80,81,82,83,84]. The language used in the article, the research object, the empathy scale involved in the research and the purpose of the research were taken as the main evaluation indicators. Regardless of the publication date and journal, above two authors independently screened articles through referring to the titles and abstracts based on the predefined inclusion criteria. If necessary, they would read the entire text to assess whether the candidate article met the inclusion criteria. Subsequently, they independently applied the exclusion criteria to finalize the included articles. In cases of disagreement, other authors would participate in the discussion until consensus was reached on whether to include a particular article. Finally, the research team reached a consensus on the final list of articles to be included in the review. The search was conducted until January 2024. For each of the included studies, two separate reviewers extracted the following information: author, year, country, title, aim, study type, sample, methods/scale, and brief summaries/findings.
Inclusion criteria
Articles included in this review, regardless of publication date or journal, had to meet the following inclusion criteria: should be peer-reviewed English journal articles; the subjects in the studies must undergo at least one form of empathy measurement; the participants must be medical students; and the research must investigate at least one aspect of the impact of empathy on medical students’ mental health, academic performance, clinical competence, or specialty preference. Both experimental, non-experimental, and mixed-method studies were eligible for inclusion.
Exclusion criteria
The exclusion criteria were as follows: editorials, letters to the editor, viewpoints, case presentations, articles not written in English, and those for which we could not obtain the full text. Additionally, articles lacking research methods and references were also excluded.
Data analysis and presentation
Once the data extraction process was completed, the authors analyzed the study results. The focus of the analysis was to extract data that meted the aim of this integrative review. The first and second authors finished the analysis, which was then reviewed and refined with the assistance of the third author. Once the data evaluation and analysis processes were completed, the review findings were presented in the form of descriptions.
Results
A total of 2294 articles were returned from PubMed, EBSCO, and Web of Science using search strategies. 1688 articles were remained after deleting duplicates. After removing articles that did not meet the selection criterias and evaluating 3 results that required discussion, 38 results were included in this review. The types of studies included cross-sectional, longitudinal, and network analysis. All research subjects were medical students. Among the 38 articles included in this review, 21 articles used different versions of JSPE/JSE to assess the empathy of medical students [33, 42, 52, 62, 67,68,69,70,71,72,73,74,75, 85,86,87,88,89,90,91,92], 6 articles used IRI [64, 66, 93,94,95,96], 1 article used JSP and IRI [97], 3 article used Toronto Empathy Questionnaire [98,99,100], 1 article uses JSPE and Toronto Empathy Questionnaire at the same time to evaluate students’ empathy [101], 1 article uses JSPE, QCAE and IRI at the same time to evaluate students’ empathy [65], 1 article used the Basic empathy scale [102], 2 articles used JSPE, IRI and Empathy Quotient [103, 104], 1 article used the interpersonal and communication skills checklist to evaluate the empathy [105], and 1 article evaluated the empathy of medical students by examiners and simulated patient actor [106].
The included researches indicated that empathy might affect the following aspects of medical students:
Mental Health
A multicenter cross-sectional study used the Thai Mental Health Indicator and the Toronto Empathy Questionnaire to evaluate the mental health and empathy of medical students participating in the experiment, and analyzed the relationship between the two. The results showed that good mental health was related to higher empathy [98]. In order to explore whether the well-being of medical students was related to empathy, a multi-institutional cross-sectional survey used validated tools to measure students’ empathy, burnout and well-being. The results indicated that students’ empathy scores derived from IRI were negatively correlated with burnout and positively correlated with well-being [64]. Their conclusions were consistent with other researches [85, 93, 99, 102]. A study was conducted at medical schools in Spain, and analyzed medical students’ empathy, depression, anxiety and burnout. The researchers found that students who scored higher in the JSE had a lower risk of depression [69]. In order to research the impact of different dimensions of empathy on burnout, Harscher et al. requested medical students to complete the Maslach Burnout Inventory and IRI scale. After statistical analysis, they found that students with high levels of empathic concern had statistically lower scores of burnout over time while students with high levels of personal distress showed statistically higher scores of burnout during medical education [94], similar to another research [95]. And a network analysis measured medical students’ empathy dimensions and depression symptoms using IRI and PHQ-9. A positive correlation was found between depression and personal pain [96]. However, empathic concern and personal pain belong to the affective empathy, and this study did not further explore the impact of cognitive empathy on medical students’ burnout. In another study, researchers measured students’ empathy through JSPE-S and QCAE [65]. Then they chose depression, anxiety and burnout as the indicators of mental health. In this study, positive associations were found between affective empathy and more mental health issues such as depression, anxiety and burnout, while cognitive empathy was the opposite.
Academic performance
Academic performance reflects medical students’ basic science and clinical knowledge [68]. Austin et al. examined the empathy of medical students from different grades by using JSPE and investigated whether the students’ empathy scores were related to the end-of-year overall academic performance [42]. At any grade, there was no statistical evidence indicated that empathy scores were related to the academic performance of medical students. Moreover, in a cross-sectional study, students’ empathy data was collected using the IRI, and the Spearman Rank Correlation test was used to determine whether or not there was a correlation between students’ empathy and their academic performance. According to the results, academic performance and empathy were not significantly associated [66]. Two studies from Iran [68] and South Korea [86] evaluated the empathy of medical students participating in the studies using the JSE and JSE-S scales respectively, and investigated empathy score correlation with academic performance. Their results, similar to previous studies, showed that there was no significant relationship between empathy among medical students and academic performance.
Clinical competence
Communication, knowledge, technical skills, and clinical reasoning are all components of clinical competence [107]. Significant relationship between empathy and clinical competence was reported [108]. The authors used JSPE to assess the empathy of medical students. Then they examined the relationship between empathy scores and the global rating of clinical competence assessed by clinical teachers. Their findings indicated a positive relationship between empathy and clinical competence, particularly in the areas of history taking and physical examinations [70]. These results were consistent with previous findings [105]. Ogle et al. assessed the clinical competence of students through the objective structured clinical examination (OSCE). And the empathy of medical students was self-evaluated by the JSPE, and also evaluated by observers. According to results of the t-test, they found that the clinical competence of medical students was positively correlated with the observed empathic behaviors, but not with the self-evaluation empathy score [71]. In another study using OSCE as an evaluation of medical students’ clinical competence, researchers proved that the self-test empathy score from JSPE could predict the communication score of OSCE but not the overall score [67]. In addition, other researchers collected empathy scores of medical students independently evaluated by examiners and simulated patient actors, and compared them with OSCE scores. After statistical analysis, the results showed that students’ empathy scores were positively correlated with the interaction-based part of OSCE, while the skill-based part was almost irrelevant [106]. Wimmers et al. also believed that the relationship between empathy and OSCE might be determined by the interaction with the patient [87].
Specialty Preference
Empathy has significant impact on medical students’ mental health, clinical competence, and specialty preference. Medical specialties were divided into people-oriented specialties that paid more attention to communication with patients and the technology-oriented specialties that relied more on medical technology [33]. Internal medicine, family practice, pediatrics, neurology, rehabilitation, psychiatry, emergency medicine, obstetrics and gynecology, ophthalmology, and dermatology are all people-focused medical subspecialties. Surgery, radiology, radiation oncology, pathology, and anesthesia are all examples of technology-focused medical subspecialties.
Using self-reported questionnaires, empathy and specialty preferences of medical students were evaluated by Santos et al. They found that compared with students who preferred technology-oriented majors, students with an inclination toward people-oriented specialties typically exhibit more empathy [97]. In another cross-sectional study, researchers collected students’ specialties preference and empathy scores through IRI, JSPE and Empathy Quotient [103]. According to the study, higher scores on empathy were found among students who favored people-focused majors. This conclusion was the same as previous studies [33, 62, 72, 73, 90, 91, 100, 104]. The relationship between empathy and specialty preference has several explanations. However, other researchers put forward different views on the relationship between empathy and medical students’ specialty preferences. In an Iranian study, researchers collected data on medical students’ empathy and specialty preferences through convenient sampling. Two-way ANOVA was computed to assess the difference of empathy and specialty preference, and there was no statistically significant relationship between them, as evidenced by the results [68]. Additionally, Magalhães et al. asked first-year and senior medical students to complete the JSPE to assess their empathy, and then analyzed the differences in JSPE scores between specialty preferences. They hypothesized that students who prefer people-oriented majors could get higher empathy scores. But the results indicated that there was no significant relationship between specialty preference and empathy of medical students [75]. Other studies also reached similar conclusions: empathy could not affect medical students’ specialty preferences [52, 74, 88, 89, 92, 101].
Author, year, country, title, aim, study type, sample, methods/scale and brief summaries/findings of the studies are provided in Table 1 below.
Discussion
Main findings
This integrative review aimed to synthesize the comprehensive impact of empathy on medical students. The results indicated that medical students who scored higher on self-reported empathy scales often have better mental health. However, low level of cognitive empathy and high level of affective empathy might lead to poor mental health among medical students, manifested as depression, anxiety, and burnout. Although there was no correlation between medical students’ empathy and their academic achievement, a positive correlation was observed between empathy and clinical competence, particularly in terms of communication skills. Additionally, most researches indicated that medical students with high empathy tended to choose people-oriented specialties, while students with lower empathy scores tended to choose technology-focused specialties.
Mental health, academic performance and clinical competence, and specialty preference
The poor mental health caused by high affective empathy and low cognitive empathy could be explained by the guilt and shame caused by both [109, 110]. The term “mental health” refers to a state of well-being that enables individuals to cope with life’s challenges. However, the risk of depression [111], anxiety [112] and burnout [113] was found to be especially high among medical students. Their mental health was worse than general population [112]. Too much or too little empathy may have a negative impact on the mental health of students in medical school. It is evident that this negative effect is driven by high levels of affective empathy and low levels of cognitive empathy. Medical students usually have higher academic workload than those without medical background; they also often have higher exposure to patient pain, fewer social connections, and get less sleep compared to others. As a result, there are some serious challenges that medical students face when it comes to their mental health. A reasonable explanation for the relationship between empathy and clinical competence is that empathy is less relevant to physical exam skills but strongly correlates with communication skills. The positive connection between empathy and clinical competence is mainly determined by the communication. However, there exists a dispute among researchers regarding whether empathy is associated with other aspects of clinical competence. Furthermore, medical students’ specialty preferences may be influenced by interpersonal skills, which are reflected in empathy. The nature of people-oriented specialties means that their graduates have more opportunities to practice empathy than those who choose to focus on technology [114], while technology-oriented majors typically involve a relatively low degree of interpersonal contact [115]. Other studies indicated that the difference in empathy scores between specialties was not statistically significant [88, 89]. This may be because, when choosing their specialties, medical students consider factors such as popularity, income, and night shifts rather than personal empathy.
Limitations
There are limitations within this review which need to be acknowledged. Firstly, since this review focuses solely on published researches, it may overlook studies implemented by medical educators but not yet published in the literature. Despite rigorous search methodologies, there is a possibility that studies were missed due to the nature of the search strings used, particularly if keywords were not present in the title or abstract. Secondly, empathy is typically measured through self-report questionnaires, which may introduce bias in the results. Volunteers’ self-reported empathy may not accurately reflect their actual levels of empathy. Furthermore, differences in questionnaire usage for the same experiment may yield completely different results, an issue that is not addressed in this review. Additionally, articles written in languages other than English were excluded, potentially excluding relevant studies. This review did not use educational theories, models, and/or frameworks related to the research topic, which resulted in a lack of benefits from theory being a major limitation of the study.
Recommendations & future research directions
Considering the severe mental health challenges faced by medical students, any method that may help them maintain good mental health state is worth applying. In light of previous research findings, medical educators should develop feasible training programs or courses, such as patient narrative and creative arts, to help medical students reduce affective empathy and improve cognitive empathy within an appropriate range. Ultimately, medical students can maintain good mental health state to cope with challenges in their work and life. Medical educators should attach importance to the positive correlation between empathy and communication skills in clinical competence among students. Teachers should help medical students enhance their communication skills by improving their empathy, ultimately achieving improvement in clinical competence. Due to the lack of specific research on the impact of different dimensions of empathy on clinical competence, this is a meaningful research direction for researchers in this field. In the future, medical educators may effectively help medical students by using the conclusions drawn from research on the relationships between empathy and specialty preferences. For instance, freshmen in medical schools can be assessed their empathy levels to predict their specialty preferences, enabling educators to tailor targeted courses to enhance their competence in their preferred specialties. Furthermore, these conclusions can assist medical educators in identifying students with relatively low empathy scores who prefer technology-oriented specialties, allowing them to provide additional courses aimed at enhancing and maintaining empathy. Given the current scarcity of research on the impact of affective empathy and cognitive empathy on medical students’ specialty preference, further studies in this area are needed. Finally, it is important to note that scores on empathy scales may not accurately reflect medical students’ actual empathy. Future research can evaluate empathy by observing actual empathy behaviors.
Conclusions
Medical students who score higher on self-reported empathy scales often have better mental health. However, interestingly, positive associations were discovered between affective empathy and mental health issues such as depression, anxiety, and burnout, whereas cognitive empathy presented an opposite trend. There is no correlation between the empathy of medical students and their academic achievements, but it is positively correlated with their clinical competence, especially their communication skills. Moreover, medical students with high empathy tend to choose specialties that are dedicated to people. Because empathy consists of both cognitive and affective components, it has a complex impact on medical students. The findings from the studies reviewed can assist medical educators in their curriculum development efforts. Consequently, it is imperative to develop targeted courses and training for medical students to foster their empathy and reap its benefits.
Data availability
The datasets used and analyzed during the current study available from the corresponding author on reasonable request.
References
Bellet PS, Maloney MJ. The importance of empathy as an interviewing skill in medicine. JAMA. 1991;266(13):1831–2.
Singer T, Klimecki OM. Empathy and compassion. Curr Biol. 2014;24(18):R875–8.
Stepien KA, Baernstein A. Educating for empathy. A review. J Gen Intern Med. 2006;21(5):524–30.
Yan Z, et al. A meta-analysis of the relationship between empathy and executive function. Psych J. 2020;9(1):34–43.
Rogers K, et al. Who cares? Revisiting empathy in Asperger syndrome. J Autism Dev Disord. 2007;37(4):709–15.
Lamm C, Batson CD, Decety J. The neural substrate of human empathy: effects of perspective-taking and cognitive appraisal. J Cogn Neurosci. 2007;19(1):42–58.
Gerace A, et al. An exploratory investigation of the process of perspective taking in interpersonal situations. J Relationships Res. 2013;4:e6.
Roth-Hanania R, Davidov M, Zahn-Waxler C. Empathy development from 8 to 16 months: early signs of concern for others. Infant Behav Dev. 2011;34(3):447–58.
Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract, 2002. 52 Suppl(Suppl): p. S9–12.
von Fragstein M, et al. UK consensus statement on the content of communication curricula in undergraduate medical education. Med Educ. 2008;42(11):1100–7.
Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–51.
Johnson JA. Empathy as a Personality Disposition. 2005.
Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–33.
Vermeire E, et al. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–42.
Roter DL, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36(8):1138–61.
Bendapudi NM, et al. Patients’ perspectives on ideal physician behaviors. Mayo Clin Proc. 2006;81(3):338–44.
Verheul W, Sanders A, Bensing J. The effects of physicians’ affect-oriented communication style and raising expectations on analogue patients’ anxiety, affect and expectancies. Patient Educ Couns. 2010;80(3):300–6.
Zachariae R, et al. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer. 2003;88(5):658–65.
Howick J, et al. Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis. J R Soc Med. 2018;111(7):240–52.
Hojat M, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–64.
Rakel D, et al. Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85(3):390–7.
Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–50.
Levinson W, et al. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553–9.
Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of Burnout in Physicians: New Neuro-Phenomenological hypotheses regarding Empathy and Sympathy in Care Relationship. Front Psychol. 2016;7:763.
Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS ONE. 2013;8(4):e61526.
Wang Q, et al. Empathy, burnout, life satisfaction, correlations and associated socio-demographic factors among Chinese undergraduate medical students: an exploratory cross-sectional study. BMC Med Educ. 2019;19(1):341.
Suchman AL, et al. Physician satisfaction with primary care office visits. Collaborative Study Group of the American Academy on Physician and Patient. Med Care. 1993;31(12):1083–92.
General Medical Council. Our strategy: 2021–25. In. Edited by Council GM. Manchester: General Medical Council. https://www.gmc-uk.org/-/media/gmc-site/about/how-we-work/corporate-strategy/corporate_strategy_document_final_en_04122020.pdf.
Association of American Medical Colleges Medical School Objectives Project. [cited 2005; http//www.aamc.org/meded/msop/msop1.pdf.
Samarasekera DD, et al. Development of student empathy during medical education: changes and the influence of context and training. Korean J Med Educ. 2022;34(1):17–26.
Seeberger A, et al. Can empathy be preserved in medical education? Int J Med Educ. 2020;11:83–9.
Batt-Rawden SA, et al. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171–7.
Chen D, et al. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–8.
Hojat M, Gonnella JS. What matters more about the interpersonal reactivity index and the Jefferson Scale of Empathy? Their underlying constructs or their relationships with Pertinent measures of clinical competence and patient outcomes? Acad Med. 2017;92(6):743–5.
Costa P, et al. Measuring Medical Students’ Empathy: exploring the underlying constructs of and associations between two widely used Self-Report instruments in five countries. Acad Med. 2017;92(6):860–7.
Baron-Cohen S, Wheelwright S. The empathy quotient: an investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. J Autism Dev Disord. 2004;34(2):163–75.
Reniers RL, et al. The QCAE: a Questionnaire of Cognitive and Affective Empathy. J Pers Assess. 2011;93(1):84–95.
Yeo S, Kim KJ. A validation study of the Korean version of the Toronto empathy questionnaire for the measurement of medical students’ empathy. BMC Med Educ. 2021;21(1):119.
Costa P, Magalhães E, Costa MJ. A latent growth model suggests that empathy of medical students does not decline over time. Adv Health Sci Educ Theory Pract. 2013;18(3):509–22.
Park KH, et al. Empathy in Korean medical students: findings from a nationwide survey. Med Teach. 2015;37(10):943–8.
Youssef FF, et al. An exploration of changes in cognitive and emotional empathy among medical students in the Caribbean. Int J Med Educ. 2014;5:185–92.
Austin EJ, et al. A preliminary study of empathy, emotional intelligence and examination performance in MBChB students. Med Educ. 2007;41(7):684–9.
Newton BW, et al. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244–9.
Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: evidence for positive changes. Med Educ. 2017;51(11):1146–59.
Kliszcz J, Hebanowski M, Rembowski J. Emotional and cognitive empathy in medical schools. Acad Med. 1998;73(5):541.
Neumann M, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009.
Khademalhosseini M, Khademalhosseini Z, Mahmoodian F. Comparison of empathy score among medical students in both basic and clinical levels. J Adv Med Educ Prof. 2014;2(2):88–91.
Rezayat AA, et al. Empathy score among medical students in Mashhad, Iran: study of the Jefferson Scale of Physician Empathy. Electron Physician. 2018;10(7):7101–6.
Tariq N, Rasheed T, Tavakol M. A quantitative study of Empathy in Pakistani Medical students: a Multicentered Approach. J Prim Care Community Health. 2017;8(4):294–9.
Li D, et al. Empathy in Chinese eight-year medical program students: differences by school year, educational stage, and future career preference. BMC Med Educ. 2018;18(1):241.
Iqbal MZ, et al. Measuring empathy in medical students: a cross-sectional study. J Pak Med Assoc. 2022;72(6):1101–5.
Shashikumar R, et al. Cross sectional assessment of empathy among undergraduates from a medical college. Med J Armed Forces India. 2014;70(2):179–85.
Chatterjee A, et al. Clinical empathy in medical students in India measured using the Jefferson Scale of Empathy-Student Version. J Educ Eval Health Prof. 2017;14:33.
Williams B, Sadasivan S, Kadirvelu A. Malaysian Medical Students’ self-reported Empathy: a cross-sectional comparative study. Med J Malaysia. 2015;70(2):76–80.
Lim BT, et al. How well do medical students rate and communicate clinical empathy? Med Teach. 2013;35(2):e946–51.
Díaz Narváez VP, et al. Empathic orientation among medical students from three universities in Barranquilla, Colombia and one university in the Dominican Republic. Arch Argent Pediatr. 2014;112(1):41–9.
Triffaux JM, Tisseron S, Nasello JA. Decline of empathy among medical students: dehumanization or useful coping process? Encephale. 2019;45(1):3–8.
Hojat M, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934–41.
Stratton TD, Saunders JA, Elam CL. Changes in medical students’ emotional intelligence: an exploratory study. Teach Learn Med. 2008;20(3):279–84.
Shariat SV, Habibi M. Empathy in Iranian medical students: measurement model of the Jefferson scale of empathy. Med Teach. 2013;35(1):e913–8.
Hojat M, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91.
Tavakol S, Dennick R, Tavakol M. Empathy in UK medical students: differences by gender, medical year and specialty interest. Educ Prim Care. 2011;22(5):297–303.
Shin HS, Park H, Lee YM. The relationship between medical students’ empathy and burnout levels by gender and study years. Patient Educ Couns. 2022;105(2):432–9.
Thomas MR, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. 2007;22(2):177–83.
Carrard V, et al. The relationship between medical students’ empathy, mental health, and burnout: a cross-sectional study. Med Teach. 2022;44(12):1392–9.
Javaeed A, et al. Empathy scores amongst undergraduate medical students and its correlation to their academic performance. J Adv Med Educ Prof. 2022;10(2):99–104.
Casas RS, et al. Associations of medical student empathy with clinical competence. Patient Educ Couns. 2017;100(4):742–7.
Benabbas R. Empathy in Iranian medical students: a comparison by age, gender, academic performance and specialty preferences. Med J Islam Repub Iran. 2016;30:439.
Capdevila-Gaudens P, et al. Depression, anxiety, burnout and empathy among Spanish medical students. PLoS ONE. 2021;16(12):e0260359.
Hojat M, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36(6):522–7.
Ogle J, Bushnell JA, Caputi P. Empathy is related to clinical competence in medical care. Med Educ. 2013;47(8):824–31.
Assing Hvidt E, et al. A cross-sectional study of student empathy across four medical schools in Denmark-associations between empathy level and age, sex, specialty preferences and motivation. BMC Med Educ. 2022;22(1):489.
Chen DC, et al. Characterizing changes in student empathy throughout medical school. Med Teach. 2012;34(4):305–11.
Mostafa A, et al. Empathy in undergraduate medical students of Bangladesh: psychometric analysis and differences by gender, academic year, and specialty preferences. ISRN Psychiatry. 2014;2014:375439.
Magalhães E, et al. Empathy in senior year and first year medical students: a cross-sectional study. BMC Med Educ. 2011;11:52.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Whittemore R, et al. Methods for knowledge synthesis: an overview. Heart Lung. 2014;43(5):453–61.
Galvão CM, Sawada NO, Trevizan MA. [Systematic review: a resource that allows for the incorporation of evidence into nursing practice]. Rev Lat Am Enfermagem. 2004;12(3):549–56.
Liu M et al. Association of Personality Traits with life and work of medical students: an integrative review. Int J Environ Res Public Health, 2022. 19(19).
Lawn S, Zhi X, Morello A. An integrative review of e-learning in the delivery of self-management support training for health professionals. BMC Med Educ. 2017;17(1):183.
Han ER, et al. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: an integrative review. BMC Med Educ. 2019;19(1):460.
De Leeuw RA, et al. Quality specifications in postgraduate medical e-learning: an integrative literature review leading to a postgraduate medical e-learning model. BMC Med Educ. 2016;16:168.
Opoku EN, Khuabi LJ, Van Niekerk L. Exploring the factors that affect the transition from student to health professional: an integrative review. BMC Med Educ. 2021;21(1):558.
O’Doherty D, et al. Barriers and solutions to online learning in medical education - an integrative review. BMC Med Educ. 2018;18(1):130.
Brazeau CM, et al. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10 Suppl):S33–6.
Jung MK, Yeo S, Lee WK. Correlation between medical student empathy and a Korean nationwide comprehensive clinical assessment score at a medical school in Korea. Med (Baltim). 2022;101(30):e29497.
Wimmers PF, Stuber ML. Assessing medical students’ empathy and attitudes towards patient-centered care with an existing clinical performance exam (OSCE). Procedia - Social Behav Sci. 2010;2(2):1911–3.
O’Tuathaigh CMP, et al. Medical students’ empathy and attitudes towards professionalism: relationship with personality, specialty preference and medical programme. PLoS ONE. 2019;14(5):e0215675.
Hasan S, et al. Level of empathy among medical students in Kuwait University. Kuwait Med Princ Pract. 2013;22(4):385–9.
Kötter T, et al. The development of Empathy and Associated Factors during Medical Education: a longitudinal study. J Med Educ Curric Dev. 2021;8:23821205211030176.
Hojat M, et al. Empathy in medical students as related to specialty interest, personality, and perceptions of mother and father. Pers Indiv Differ. 2005;39(7):1205–15.
Shah A et al. empathy-among-students-of-a-publicsector-medical-university-a-crosssectional-study. 2022.
Paro HB, et al. Empathy among medical students: is there a relation with quality of life and burnout? PLoS ONE. 2014;9(4):e94133.
von Harscher H, et al. The impact of empathy on burnout in medical students: new findings. Psychol Health Med. 2018;23(3):295–303.
Sulaiman R, et al. Experiences of burnout, anxiety, and empathy among health profession students in Qatar University during the COVID-19 pandemic: a cross-sectional study. BMC Psychol. 2023;11(1):111.
Li J, et al. The relationship between dimensions of empathy and symptoms of depression among university students during the COVID-19 pandemic: a network analysis. Front Public Health. 2022;10:1034119.
Santos MA, et al. Empathy differences by gender and specialty preference in medical students: a study in Brazil. Int J Med Educ. 2016;7:149–53.
Pitanupong J, et al. Relationship of mental health and burnout with empathy among medical students in Thailand: a multicenter cross-sectional study. PLoS ONE. 2023;18(1):e0279564.
Sathaporn K, Pitanupong J. The relationship between Mental Health with the level of Empathy among Medical students in Southern Thailand: A University-Based Cross- Sectional Study. Siriraj Med J. 2021;73:832–40.
Pantovic M, et al. Empathy predicting career choice in future physicians. Engrami. 2015;37:37–48.
Akgün Ö, et al. Medical students’ Empathy Level differences by Medical Year, gender, and Specialty Interest in Akdeniz University. J Med Educ Curric Dev. 2020;7:2382120520940658.
Wu W, et al. Empathy alleviates the learning burnout of medical college students through enhancing resilience. BMC Med Educ. 2022;22(1):481.
Guilera T, et al. Empathy and big five personality model in medical students and its relationship to gender and specialty preference: a cross-sectional study. BMC Med Educ. 2019;19(1):57.
Guilera T, Batalla I, Soler-González J. Empathy and specialty preference in medical students. Follow-up study and feedback. Educación Médica; 2017.
Colliver JA, et al. Assessment of Empathy in a standardized-patient examination. Teach Learn Med. 1998;10(1):8–11.
Wright B, et al. Examiner and simulated patient ratings of empathy in medical student final year clinical examination: are they useful? BMC Med Educ. 2014;14:199.
Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226–35.
Hojat M, Empathy as Related to Personal Qualities, Career Choice, Acquisition of Knowledge, and Clinical Competence, in Empathy in Health Professions Education and Patient Care, Hojat M. Editor. 2016, Springer International Publishing: Cham. pp. 151–167.
Gambin M, Sharp C. Relations between empathy and anxiety dimensions in inpatient adolescents. Anxiety Stress Coping. 2018;31(4):447–58.
O’Connor LE, et al. Guilt, fear, submission, and empathy in depression. J Affect Disord. 2002;71(1–3):19–27.
Rotenstein LS, et al. Prevalence of Depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and Meta-analysis. JAMA. 2016;316(21):2214–36.
Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73.
Frajerman A, et al. Burnout in medical students before residency: a systematic review and meta-analysis. Eur Psychiatry. 2019;55:36–42.
Chaitoff A, et al. Associations between Physician Empathy, physician characteristics, and standardized measures of patient experience. Acad Med. 2017;92(10):1464–71.
Hojat M, et al. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563–9.
Funding
This work was supported by Basic and Applied Basic Research Foundation of Guangdong Province (2023A1515010902), Heilongjiang Provincial Key Project of The Educational Science 14th Five-Year Plan (GJB1422780, GJB1423224), the Directive Project of Medical Scientific Research Foundation in Guangdong (A2022379), Key Laboratory of Philosophy and Social Sciences of Colleges and Universities in Guangdong Province (2023WSYS005, 2023WSYS007), Chinese Medical Association Medical Education Research Project (2023B089), Harbin Medical University Ideological & Political Educational Research Project (YJSSZKT2023-16HYD), and Harbin Medical University Educational Science Research Project (XY202201).
Author information
Authors and Affiliations
Contributions
HC contributed to conceptualization, writing – original draft, visualization, data curation. ML contributed to writing – original draft, conceptualization, data curation, funding acquisition. HX contributed to investigation, validation. JC and LS contributed to conceptualization, writing – review & editing, funding acquisition, supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, H., Xuan, H., Cai, J. et al. The impact of empathy on medical students: an integrative review. BMC Med Educ 24, 455 (2024). https://doi.org/10.1186/s12909-024-05448-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05448-5