Abstract
Background
The Tibetan area is one of China’s minority regions with a shortage of general practice personnel, which requires further training and staffing. This research helps to understand the current condition and demand for general practitioner (GP) training in Tibetan areas and to provide a reference for promoting GP education and training.
Methods
We conducted a cross-sectional survey using stratified sampling targeting 854 GPs in seven cities within the Tibetan Autonomous Region, utilizing an online questionnaire. Achieving a high response rate of 95.1%, 812 GPs provided invaluable insights. Our meticulously developed self-designed questionnaire, available in both Chinese and Tibetan versions, aimed to capture a wide array of data encompassing basic demographics, clinical skills, and specific training needs of GPs in the Tibetan areas. Prior to deployment, the questionnaire underwent rigorous development and refinement processes, including expert consultation and pilot testing, to ensure its content validity and reliability. In our analysis, we employed descriptive statistics to present the characteristics and current training needs of GPs in the Tibetan areas. Additionally, chi-square tests were utilized to examine discrepancies in training needs across various demographic groups, such as age, job positions, and educational backgrounds of the participating GPs.
Results
The study was completed by 812 (812/854, 95.1%) GPs, of whom 62.4% (507/812) were female. The top three training needs were hypertension (81.4%, 661/812), pregnancy management (80.7%, 655/812), and treatment of related patient conditions and events (80.5%, 654/812). Further research shows that the training required by GPs of different ages in “puncturing, catheterization, and indwelling gastric tube use” (64.6% vs. 54.8%, p = 9.5 × 10− 6) varies statistically. GPs in various positions have different training needs in “community-based chronic disease prevention and management” (76.6% vs. 63.9%, p = 0.009). The training needs of GPs with different educational backgrounds in “debridement, suturing, and fracture fixation” (65.6% vs. 73.2%, p = 0.027) were also statistically significant.
Conclusions
This study suggests the need for targeted continuing medical education activities and for updating training topics and content. Course developers must consider the needs of GPs, as well as the age, job positions, and educational backgrounds of GPs practicing in the Tibetan Plateau region.
Trial registration
Not applicable.
Similar content being viewed by others
Background
General practitioners (GPs) play a vital role in providing a wide range of primary health care (PHC) services, including preventive care, treatment, and referrals for common diseases, chronic disease management, and health management [1, 2]. In the context of Tibet, a unique province in China with distinct characteristics such as a high-altitude, low-oxygen geographic environment, limited economic development, and specific cultural and historical traditions, the number and training of GPs are insufficient to meet the region’s future healthcare needs [3,4,5]. The quantity and quality of GPs in Tibet continue to be lower than the minimum requirements of the Chinese government, and this situation will be expected to worsen by 2030 [6]. Given the challenges faced by primary healthcare institutions and GPs in Tibet, it is crucial to identify and address the specific training needs of GPs to enhance the overall quality of PHC in the region.
The existing literature has highlighted constraints such as limited participation in training due to practical course attendance and time constraints in Chaya County, Tibet [7, 8]. Other researchers have evaluated the training needs of GPs in different regions of China, comparing the knowledge and skill requirements across the eastern, central, and western areas [9, 10]. Furthermore, a review of GP training needs in Ireland highlighted common CME needs such as updated protocols, geriatrics, chronic disease treatment, and dermatology [11]. Additionally, multiple studies have delved into the training needs of GPs in areas such as evidence-based medicine, tuberculosis control and management, and the care of vulnerable populations [12,13,14]. Despite there have been descriptions and evaluations of GP training needs, the published literature on GP training needs is very preliminary and not specific enough to support wider adoption, and research on GP training needs in the entire Tibet Autonomous Region is limited.
In Tibet, the training of physicians comprises basic medical education, clinical practice, and specialized training [7]. Medical students undergo 3–5 years of basic medical education at universities, focusing on mastering fundamental medical knowledge and skills. Subsequently, they engage in 1–3 years of standardized residency training and internship. Following this, doctors pursue further specialization through programs such as master’s or doctoral studies. To address the need for primary medical services, Tibet has introduced a GP training program, transforming rural doctors into GPs after a brief transfer training period or offering free training for medical students under the Rural Order Orientation Program, emphasizing general practice in primary health-care institutions. Additionally, Continuing Medical Education (CME) plays a vital role in Tibet, with GPs gaining further training at larger hospitals and participating in various educational opportunities such as study classes, academic conferences, and online education [15].In spite of this, the opportunities and number of GPs in Tibet who can receive CME are still very limited, making it far more difficult to meet the needs of local PHC.
Therefore, this study aims to fill this knowledge gap by investigating the current situation of GPs and their CME needs, specifically, our research questions are as follows:
-
(1)
What is the structure of GPs in Tibet in terms of age, gender, job position, practicing categories, professional positions and degree?
-
(2)
Are there differences in CME needs among GPs of different age groups?
-
(3)
Are there differences in CME needs among GPs with different positions and education degrees?
In brief, this study delved into the training needs of GPs in the Tibet Autonomous Region, offering valuable insights for the future development of CME programs for GPs.
Methods
Survey sample and participants
A multicenter, cross-sectional, descriptive survey methodology was used for this study. From March to August 2022, the survey study was carried out. Based on the population density, economic conditions and distribution of PHC institutions in Tibet, a stratified sampling method was used to survey seven cities, including the Lhasa, Xigaze, Nyingchi, Qamdo, Shannan, Nagqu, and Ngari Prefectures. From March to August 2022, we submitted the questionnaire to GPs in the seven cities listed above. The inclusion criteria for participants in the study population were as follows: (1) those working at PHC facilities such as primary hospitals, community health service centers, and village clinics and (2) those able to read and understand the questions included in the questionnaire. The exclusion criteria were as follows: (1) non-GPs and (2) individuals who were unable to complete the web-based survey questionnaire.
Survey questionnaire development
The employed questionnaire is based on the classic six-step framework for curriculum development proposed by Kern et al. [16] (problem identification; needs assessment of the learners; educational goals and objectives; instructional strategies; implementation, and evaluation and feedback) with reference to the World Organization of Family Doctors (WONCA) core competence model for GPs [17]. For further guidance, we invited 18 experts, including 5 general practice professionals, 4 public health experts, 4 managers of PHC institutions, and 5 GPs in Tibetan areas, to review and revise the content of the questionnaire. This expert review process aimed to ascertain that each item in the questionnaire accurately reflects the intended dimensions, particularly focusing on the unique context of CME for GPs in Tibet. To further refine the questionnaire and enhance its applicability, a pilot study was conducted with a carefully chosen group of GPs. The feedback obtained from this study was instrumental in the iterative process of fine-tuning the questionnaire. Finally, the questionnaire is comprised of multiple dimensions, encompassing comprehensive data. This includes basic demographic and professional information of GPs, educational background, as well as specific needs for CME. It covers 8 aspects, consisting of a total of 15 questions, as shown below (Additional file 1):
-
A)
basic information about the GPs (8 questions),
-
B)
clinical skill training needs (8 options),
-
C)
community chronic disease management skill training needs (7 options),
-
D)
common chronic disease training needs (13 options),
-
E)
public health service skill training needs (6 options),
-
F)
special population health management training needs (8 options),
-
G)
training needs for infectious diseases and handling of public health emergencies (5 options),
-
H)
rehabilitation technology training needs (5 options).
In addition to obtaining basic information, each question allowed for more than one response. Taking into account the diversity of languages, we meticulously translated the questionnaire into Tibetan. During this process, we employed back-translation techniques to ensure the accuracy of the language and the appropriateness of the cultural context. Ultimately, we produced the survey questionnaire in both Chinese and Tibetan versions. The internal consistency of the questionnaire was thoroughly evaluated using Cronbach’s alpha, resulting in a high reliability coefficient of α = 0.87. This indicates a strong degree of consistency in the responses across various items of the questionnaire, reinforcing the reliability of our tool for assessing the educational needs of GPs. To further validate the reliability of our questionnaire, a test-retest method was employed. A subgroup of participants (n = 30) completed the questionnaire twice with a two-week interval. The high correlation coefficient (r = 0.82) observed between the two sets of responses confirms the stability and reliability of the questionnaire over time.
Data collection and quality control
In March 2022, the online version of the questionnaire was developed using the Sojump software, a popular and user-friendly online survey tool in China. This platform was chosen for its reliability, ease of use, and features that facilitate effective data collection and management. The questionnaires were sent to the leaders of primary health services in Tibet through online WeChat (Quick Response) QR codes and then distributed to the managers of PHC institutions and GPs in seven cities in Tibet. Participants completed the questionnaire at their convenience, with an average completion time of approximately five minutes. The recruitment strategy involved coordination by research group staff members, who facilitated the distribution and collection of completed questionnaires. Three research group staff members coordinated the survey, which was sent via an online platform with the necessary guidelines and instructions. Each survey was completed and submitted anonymously by GPs and managers of PHC institutions in Tibet, and the leader of the research group reviewed the quality of the collected questionnaires. Questionnaires were excluded from the database if they were incomplete or if there were any data quality issues identified during the review process.
Statistical analysis
All calculations were conducted using the Statistical Package for Social Sciences (SPSS) for Mac (Version 26.0, SPSS, Inc., Chicago, IL, USA). Descriptive statistics (frequencies and percentages) were used to describe the characteristics of training needs. In this research, we clarified our research hypotheses before conducting multiple comparisons. Our study focused on several key indicators, mainly age, job position, and degree. For each indicator, we formulated the corresponding research hypotheses namely: (1) There are differences in CME training needs among GPs of different ages in Tibet, (2) There are differences in CME training needs among GPs of different job positions in Tibet, (3) There is a difference in the demand for CME training among GPs with different degrees in Tibet. For the first test hypothesis, we used the 2*3 chi-square test to test whether there is a difference between the entries of different ages of GPs in Tibet in terms of the need for CME and training, and for the entries where there is a difference, we continued to use the Bonferroni correction method to make a two-by-two comparison of whether there is a difference between the different age groups. In this way, we can reduce the risk of type I errors while maintaining statistical significance. For the 2nd and 3rd test hypotheses, whether there are differences in each entry of continuing education and training needs among GPs of different positions and education levels in Tibet, we analyzed them using a 2*2 chi-square test. The tests were two-sided, and a value of p < 0.05 was considered statistically significant.
Results
Demographic characteristics
A total of 854 GPs from 7 cities in the Tibet Autonomous Region participated in the questionnaire. We excluded 42 questionnaires due to incomplete items or repeated duplicate completion, and 812 valid questionnaires were finally collected, resulting in a response rate of 95.1% (812/845). We share the specific distribution of the number of valid questionnaires in eTable 1 in the supplementary material.
Table 1 shows the social demographics and characteristics of the participants. In total, 62.4% (507/812) of the participants were female, while 37.6% (305/812) were male. Overall, 62.9% (511/812) of the GPs were under the age of 30, and only 10.3% (84/812) were over 40. We found that 13.7% (111/812) of the GPs were administrative managers, while 38.8% (315/812) were neither practicing physicians nor assistant practicing physicians. Only 8.1% (66/812) of the participants had middle-level or higher titles, while the majority of participants had a bachelor’s degree or higher (68.5%, 556/812).
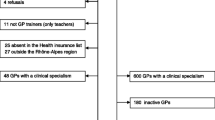
Training needs of GP participants in Tibet
Table 2 describes the identified training needs of all participants. The seven main training needs of GPs relate to “debridement and suturing and fracture fixation” (70.8%, 575/812), “GP clinical diagnosis and treatment analysis” (67.9%, 551/812), “hypertension” (81.4%, 661/812), “prevention and control of infectious diseases” (74.1%, 602/812), “pregnancy management” (80.7%, 655/812), “treatment of related patients and events” (80.5%, 654/812), and “rehabilitation assessment and treatment of common and frequently occurring diseases in the community” (79.1%, 642/812). We can see the differences in the training needs of GPs by age and job position group in Fig. 1A and B.
Training needs for GPs of different categories. Fig. 1A Training needs for GPs of different ages. “Various laboratory tests and imaging assignments” ranked first in terms of clinical skills training needs for the group over 40 years of age, but among the other categories, the main training needs of GPs were the same across different age groups. Fig. Fig. 1B Training needs for GPs of different job positions. “Community prevention and management of chronic diseases” ranked first in terms of training needs for community-based chronic disease management skills for the manager group, but for the other categories, the main training needs of GPs were the same among the two job position groups. Capital letters in Fig. 1A and Fig. 1B are defined as follows: (1) Clinical skills training needs. (2) Community-based chronic disease management skill training needs. (3) Common chronic disease training needs. (4) Public health service skills training needs. (5) Special population health management training needs. (6) Training needs in reporting and handling infectious diseases and public health emergencies. (7) Rehabilitation technique training needs
Comparison of differences in training needs of GPs from different age groups
Table 3 shows the variation and types of training needs of GPs in different age groups. Compared to the 30–40 age group, GPs under 30 years of age noted more significant training needs in “puncturing, catheterization, and indwelling gastric tube use” (64.6% vs. 54.8%, p = 9.5 × 10− 6), “sputum suction and enema treatment” (51.3% vs. 44.7%, p = 0.026), “medical history collection” (46.6% vs. 39.2%, p = 0.007), “osteoporosis and bone and joint disease ” (40.5% vs. 35.0%, p = 0.045), “late-stage cancer” (30.7% vs. 22.6%, p = 0.023), and “indications, contraindications, and precautions of common rehabilitation methods” (78.5% vs. 71.9%, p = 0.005). GPs over 40 years of age prioritized diabetes training needs (57.1% vs. 54.8%, p = 0.022) more than GPs in the 30-40-year age group.
Comparison of differences in training needs of GPs of different job positions and education backgrounds
Table 4 shows that when compared to nonmanager GPs, manager GPs have more training needs in “debridement and suturing and fracture fixation” (79.3% vs. 69.5%, p = 0.035), “laboratory testing and imaging reading” (79.3% vs. 66.6%, p = 0.008), “community prevention and management of chronic diseases” (76.6% vs. 63.9%, p = 0.009), “Chinese (Tibetan) Medicine and Chinese (Tibetan) Medicine Technology” (63.1% vs. 52.5%, p = 0.038), “coronary heart disease (CHD) ” (72.1% vs. 60.6%, p = 0.021), “resident health records management” (73.0% vs. 59.1%, p = 0.005), “assistance in the management of health supervision agencies” (69.4% vs. 47.8%, p = 2.4 × 10− 6), “pregnancy management” (88.3% vs. 79.5%, p = 0.029), “elderly patient management” (82.0% vs. 70.6%, p = 0.013), “treatment of patients with severe mental disorders” (78.4% vs. 55.8%, p = 7.0 × 10− 6), and “the management of related patients and events” (79.3% vs. 67.0%, p = 0.010) and fewer training needs in “diabetes ” (52.3% vs. 61.3%, p = 0.030).
Furthermore, GPs with a bachelor’s degree or higher have more training needs than those with less than a bachelor’s degree in “debridement and suturing and fracture fixation” (73.2% vs. 65.6%, p = 0.027), “various laboratory tests and imaging readings” (73.0% vs. 58.2%, p = 2.5 × 10− 6), “puncturing, catheterization, and indwelling gastric tube use” (63.7% vs. 50.8%, p = 0.001), “sputum suction and enema treatment” (51.4% vs. 40.6%, p = 0.004), “the rational use of drugs” (57.7% vs. 49.2%, p = 0.023), “Chinese (Tibetan) Medicine and Chinese (Tibetan) Medicine Technology” (58.1% vs. 44.9%, p = 4.7 × 10− 6), “common diseases of the digestive system” (73.4% vs. 65.6%, p = 0.024), “chronic obstructive pulmonary disease and emphysema” (65.8% vs. 57.0%, p = 0.016), “CHD” (64.9% vs. 56.3%, p = 0.018), “hyperuricaemia and gout” (56.5% vs. 43.8%, p = 0.001), “chronic kidney disease” (51.4% vs. 40.2%, p = 0.003), “stroke” (51.1% vs. 40.2%, p = 0.001), “osteoporosis and bone and joint diseases” (40.5% vs. 31.6%, p = 0.016), “elderly patient management” (74.8% vs. 66.4%, p = 0.013), and “management of related patients and events” (71.6% vs. 62.5%, p = 0.009).
Discussion
The main findings
Our study investigated the training needs of GPs in the Tibetan region, a unique plateau area characterized by slower development of general practice and lower medical skill levels among GPs compared to mainland China. Our findings revealed a significant demand for professional development training among Tibetan GPs, particularly in the areas of hypertension, pregnancy management, related patient events, trauma and fracture management, emergency medical care, maternity care, and traditional Chinese medicine (TCM) techniques. The disparity in training needs was noted across different age groups, job positions, and educational backgrounds, which is indicative of the varied professional development requirements in this region.
Comparing our findings with existing literature, we found consistency in the demand for training in hypertension and pregnancy management, highlighting the significance of addressing these specific needs [7, 18]. The high prevalence of hypertension in Tibet, potentially linked to environmental factors such as low oxygen levels and dietary habits, underscores the critical need for tailored training in this area [19]. Additionally, the scarcity of obstetricians and gynecologists in Tibet, coupled with suboptimal obstetric and gynecological care, contributes to a higher maternal morbidity rate, aligning with our identification of pregnancy management as a key training need [20]. The elevated prevalence of chronic diseases in Tibet, influenced by its unique geographic environment and dietary patterns, emphasizes the necessity of targeted medical training in these specific domains [21, 22]. Consequently, our study emphasizes the urgent need for tailored training programs to address the specific healthcare challenges in the Tibetan region.
GP training in trauma and fracture management, emergency medical care, and maternity care is essential
It is worth noting that the CME content needs of the participating GPs varied, and the precision of CME material should be enhanced to improve its applicability [23]. Simple fracture and trauma management is a basic community first aid skill. According to the findings of this study, the leading training needs in terms of GPs’ clinical skills in Tibet relate to debridement, suturing, and fracture fixation. However, in a prior study of GP training needs by West China Hospital of Sichuan University, this skill placed 5th out of 23 items (5/23) [7]. Because Tibet is located on a plateau, transportation is challenging, there are many herdsmen, and traffic accidents and accidental injuries occur more frequently in the local population [24]. According to a study conducted in the United States, there are very few emergency doctors in rural areas, and GPs must perform the majority of emergency treatment procedures, thus necessitating the extension of GP training in rural areas [25]. This is consistent with the findings of the current study, which found strong demand for training in emergency and first aid capabilities among GPs in rural Tibetan areas. This may be due to a lack of emergency physicians and an inadequate level of emergency care and treatment techniques and capabilities among PHC GPs.
Notably, one retrospective analysis of maternal mortality in 34 Chinese provinces and cities from 1990 to 2017 revealed that while Tibet still had the highest maternal mortality rate nationally in the period (82.7 per 100,000 live births), it had fallen by 74.4% since 1990 [26]. Although the maternal mortality rate in Tibet has dropped in recent years as a result of rapid economic development and the widespread implementation of health care policy, there is still a substantial disparity relative to other Chinese provinces [27]. This could be the main cause of the strong demand for maternal special population training among GPs in Tibetan areas, as revealed by our findings. Therefore, it is imperative to improve the maternal management capacity and capabilities of local PHC GPs in Tibet.
The training needs of different categories of GPs have different focuses
Our findings show that junior GPs (< 40 years of age) had more need for training in “debridement and suturing and fracture fixation”, “puncturing, catheterization, and indwelling gastric tube use”, “sputum suction and enema treatment”, “medical history collection” and rehabilitation-related knowledge” than senior GPs (≥ 40 years of age). There may be several reasons for this result. First, many junior GPs have only recently started working and have only undergone short-term training. They often lack relevant theoretical knowledge, clinical experience, and skills. Second, the majority of junior GPs have more motivation to learn [28, 29]. Of course, senior GPs do not have extra time to attend training due to their work and family responsibilities, which may be a major reason for their fewer training needs.
Most PHC institution managers have transferred from other specialties, lacking systematic study and training in general practice and essential management expertise, particularly in Tibet [30]. Our findings reveal that managers of PHC institutions emphasize “community prevention and management of chronic diseases”, “resident health records administration”, and “assistance in the management of health supervision agencies” more than nonmanagers, while nonmanagers prioritize diabetes training. Although the Tibetan region has numerous medical specialists from China’s developed regions for long-term support, when experts leave Tibet’s local medical level and capacity frequently fail to meet local needs [31]. This could be why local PHC managers have greater training needs in the above areas. Management of special populations (mothers, the elderly, patients with severe mental problems or chronic conditions, etc.) is a significant responsibility of GPs and an important indicator of the quality of medical services offered by medical institutions [32]. According to our findings, there is a greater need for training for PHC institution managers in the management of special populations. As a result, more management training for Tibetan PHC institution managers, as well as comprehensive clinical training for nonmanager GPs, are advocated as a significant means to address out-of-date and missing skills among local primary medical-level staff.
TCM plays a unique role in prevention, health care, wellness, and rehabilitation, and it is widely used in Chinese PHC institutions. Tibetan medicine has facilitated the social development of numerous ethnic groups on the Tibetan Plateau and in the Himalayan region [33]. Our study found that those with a bachelor’s degree or higher had more training demands in TCM (Tibetan) medicine techniques than those with a lower degree. This disparity could be attributed to differences in learning aptitudes and interests among GPs of various educational backgrounds and to the significance of their understanding of regional ethnic medicine practice. Tibetan medicine is very popular among Tibetan residents [34]. Therefore, we should strengthen Tibetan medicine knowledge training and learning for local GPs and guide the continuity of practice among local GPs in their treatment work through the establishment of corresponding treatment protocols and guidelines.
Limitations
Our study has several limitations. Firstly, face-to-face interviews were difficult due to the Tibetan Plateau’s hypoxic natural environment, the remoteness of its rural areas, inconvenient local transportation, and language difficulties among Tibetans. Secondly, we conducted an online survey and were unable to identify some subtle differences that can be gained from the field, which may affect the answers obtained and the understanding of certain research questions. Thirdly, we did not compare the training needs of GPs in rural and urban areas of Tibet. In addition, the participants in this study could not fully represent all local GPs in Tibet. This is because we could not fully control the age and gender ratio of the participants during the actual research process. Due to a variety of factors, such as willingness to participate and availability, we could only strive to make the characteristics of the participants as close as possible to the overall characteristics of GPs in Tibet. Besides, another limitation of our study is the lack of detailed quantitative analysis of the needs across different dimensions, which may limit a comprehensive understanding of the degree of needs among general practitioners. In future research, we plan to introduce a more refined scoring system to supplement and deepen our understanding in this area. Finally, our questionnaire was primarily a subjective self-report survey, and our lack of objective survey evaluation may have affected the study outcomes. More residents will participate as researchers in the survey to provide guidance and incorporate more objective scales to improve the comprehensiveness of research to address the aforementioned limitations and issues in future research.
Conclusion
In conclusion, our study emphasizes the urgent need for tailored training programs to address the specific healthcare challenges in the Tibetan region. By focusing on hypertension, pregnancy management, and trauma care, we can better equip GPs to provide comprehensive care. These findings underscore the importance of personalized training initiatives that consider the unique sociodemographic characteristics and healthcare landscape of Tibet. Meanwhile, we call for graded, stratified, and targeted GP training to meet the needs of GPs in Tibetan areas, the cultivation of specialized and versatile GPs, and addressing insufficient professional knowledge among GPs and underdeveloped PHC in many Tibetan areas. Ultimately, addressing these training needs has the potential to significantly improve the quality of primary healthcare services in the region.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GP:
-
General Practitioner
- CME:
-
Continuing Medical Education
- PHC:
-
Primary Health Care
- WONCA:
-
World Organization of Family Doctors
- QR:
-
Quick Response
- SPSS:
-
Statistical Package for Social Sciences
- CHD:
-
Coronary Heart Disease
- TCM:
-
Traditional Chinese Medicine
References
Perkins P. General practitioners and their role today. J R Soc Med. 2019;112(4):132. https://doi.org/10.1177/0141076818820394.
Phillips WR, Dai M, Frey JJ 3rd, Peterson LE. General practitioners in US Medical Practice compared with Family Physicians. Ann Fam Med. 2020;18(2):127–30. https://doi.org/10.1370/afm.2503.
Wang H, Tang C, Dang Z, Yong A, Liu L, Wang S, et al. Clinicopathological characteristics of high-altitude polycythemia-related kidney disease in tibetan inhabitants. Kidney Int. 2022;102(1):196–206. https://doi.org/10.1016/j.kint.2022.03.027.
Stokstad E. Mountains and monsoons created tibetan biodiversity. Science. 2020;369(6503):493. https://doi.org/10.1126/science.369.6503.493.
Liu Q, Liu H, Shi L, Gan M, Zhao X, Lyu LD, et al. Local adaptation of Mycobacterium tuberculosis on the Tibetan Plateau. Proc Natl Acad Sci U S A. 2021;118(17):e2017831118. https://doi.org/10.1073/pnas.2017831118.
Han X, Li X, Cheng L, Wu Z, Zhu J. Performance of China’s new medical licensing examination for rural general practice. BMC Med Educ. 2020;20(1):314. https://doi.org/10.1186/s12909-020-02234-x. Published 2020 Sep 17.
An K, Zhang L, Qiao R, Li C, Zhong Q, Ma Y, et al. Training needs and curriculum of continuing medical education among general practitioners in Tibet, China: a cross-sectional survey. Front Public Health. 2022;10:914847. https://doi.org/10.3389/fpubh.2022.914847. Published 2022 Oct 11.
Chen L, Liu J, Zheng Z, Yeshi S. Needs and difficulties of tibetan rural health care workers participating in professional training. Aust J Rural Health. 2021;29(4):578–85. https://doi.org/10.1111/ajr.12767.
Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–12. https://doi.org/10.1016/S0140-6736(20)30122-7.
Tam YH, Leung JYY, Ni MY, Ip DKM, Leung GM. Training sufficient and adequate general practitioners for universal health coverage in China. BMJ. 2018. https://doi.org/10.1136/bmj.k3128. Published 2018 Jul 26. 362: k3128.
Dowling S, Last J, Finnegan H, O’Connor K, Cullen W. What are the current ‘top five’ perceived educational needs of Irish general practitioners? Ir J Med Sci. 2020;189(1):381–8. https://doi.org/10.1007/s11845-019-02047-y.
Travers J, Romero-Ortuno R, Langan J, MacNamara F, McCormack D, McDermott C, et al. Building resilience and reversing frailty: a randomised controlled trial of a primary care intervention for older adults. Age Ageing. 2023;52(2):afad012. https://doi.org/10.1093/ageing/afad012.
Nguyen M, Chaudhry SI, Desai MM, Hajduk AM, McDade WA, Fancher TL, et al. Rates of Medical Student Placement into Graduate Medical Education by Sex, race and ethnicity, and Socioeconomic Status, 2018–2021. JAMA Netw Open. 2022;5(8):e2229243. https://doi.org/10.1001/jamanetworkopen.2022.29243. Published 2022 Aug 1.
Brickley B, Williams LT, Morgan M, Ross A, Trigger K, Ball L. Patient-centred care delivered by general practitioners: a qualitative investigation of the experiences and perceptions of patients and providers. BMJ Qual Saf. 2022;31(3):191–8. https://doi.org/10.1136/bmjqs-2020-011236.
Li X, Labaciren, Zhang YL, Shen L, Huang YG. Remote video lecture education improves anesthesiology residency training in Tibet of China. Chin Med J (Engl). 2020;133(2):245–6. https://doi.org/10.1097/CM9.0000000000000605.
Kern DE, Thomas PA, Howard DM et al. Curriculum Development for Medical Education: a six-step Approach. Baltim MD: Johns Hopkins Univ 1998;4–7.
WONCA Europe. The European definition of general practice/Family Medicine[EB/OL].2011. http://www.woncaeurope.Org/Definition%20GPFM. Accessed 3 June 2020.
Song C, Chongsuvivatwong V, Wangdui S, Mima D, Zhuoma C, Ji D, et al. Coverage and effectiveness of hypertension screening in different altitudes of Tibet autonomous region. BMC Public Health. 2021;21(1):33. https://doi.org/10.1186/s12889-020-09858-0. Published 2021 Jan 6.
Peng W, Li K, Yan AF et al. Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. Int J Environ Res Public Health. 2022;19(14):8787. Published 2022 Jul 19. https://doi.org/10.3390/ijerph19148787.
Li Q, Li X, Zhang Q, Zhang Y, Liu L, Cheng X, et al. A cross-sectional nationwide study on accessibility and availability of neonatal Care resources in hospitals of China: current Situation, Mortality and Regional differences: neonatal Care resources and Newborn Mortality in China. Lancet Reg Health West Pac. 2021;14:100212. https://doi.org/10.1016/j.lanwpc.2021.100212. Published 2021 Jul 21.
Su B, Li D, Xie J, Wang Y, Wu X, Li J, et al. Chronic disease in China: Geographic and socioeconomic determinants among persons aged 60 and older. J Am Med Dir Assoc. 2023;24(2):206–212e5. https://doi.org/10.1016/j.jamda.2022.10.002.
Niu M, Singh S, Mi M, Bian P, Deji Z, Mima D, et al. Safety and Efficacy of Therapeutic Erythrocytapheresis Treatment in Chronic Mountain sickness patients in Shigatse, Tibet, China. Med Sci Monit. 2020;26. https://doi.org/10.12659/MSM.927853. e927853. Published 2020 Dec 23.
O’Brien Pott M, Blanshan AS, Huneke KM, Baasch Thomas BL, Cook DA. What Influences Choice of Continuing Medical Education Modalities and providers? A National Survey of U.S. Physicians, Nurse practitioners, and Physician assistants. Acad Med. 2021;96(1):93–100. https://doi.org/10.1097/ACM.0000000000003758.
Deng R, Labasangzhu, Zhaxideji, Wang G, Hong P, Li J, et al. Illness prevalence rate in Tibet, China: data from the 2018 National Health Service Survey. BMC Public Health. 2020;20(1):955. https://doi.org/10.1186/s12889-020-08960-7. Published 2020 Jun 18.
Barreto T, Jetty A, Eden AR, Petterson S, Bazemore A, Peterson LE. Distribution of Physician Specialties by Rurality. J Rural Health. 2021;37(4):714–22. https://doi.org/10.1111/jrh.12548.
Li CL, Jiang M, Huang KC, Li J, Xu LG. The trends of maternal mortality ratios and cause pattern in 34 Chinese provinces, 1990–2017. BMC Public Health. 2022;22(1):1369. https://doi.org/10.1186/s12889-022-13770-0. Published 2022 Jul 16.
Liang J, Li X, Kang C, Wang Y, Kulikoff XR, Coates MM, et al. Maternal mortality ratios in 2852 Chinese counties, 1996–2015, and achievement of Millennium Development goal 5 in China: a subnational analysis of the global burden of Disease Study 2016. Lancet. 2019;393(10168):241–52. https://doi.org/10.1016/S0140-6736(18)31712-4.
Bodendieck E, Jung FU, Conrad I, Riedel-Heller SG, Hussenoeder FS. The work-life balance of general practitioners as a predictor of burnout and motivation to stay in the profession. BMC Prim Care. 2022;23(1):218. https://doi.org/10.1186/s12875-022-01831-7. Published 2022 Aug 30.
Galanter W, Eguale T, Gellad W, Lambert B, Mirica M, Cashy J et al. Personal Formularies of Primary Care Physicians Across 4 Health Care Systems [published correction appears in JAMA Netw Open. 2021;4(8): e2127092]. JAMA Netw Open. 2021;4(7): e2117038. Published 2021 Jul 1. https://doi.org/10.1001/jamanetworkopen.2021.17038.
Li Z, Gao GF. Strengthening public health at the community-level in China. Lancet Public Health. 2020;5(12):e629–30. https://doi.org/10.1016/S2468-2667(20)30266-8.
Cui N, Pan W. Medical talents group aid Tibet to strengthen the construction of critical care medical personnel in Tibet Autonomous Region. Zhong Hua Wei Zhong Bing Ji Jiu Yi Xue. 2021;33(8):897–9. https://doi.org/10.3760/cma.j.cn121430-20210702-00997.
Damarell RA, Morgan DD, Tieman JJ, Healey D. Healthc (Basel). 2020;8(4):553. https://doi.org/10.3390/healthcare8040553. Published 2020 Dec 11. Bolstering General Practitioner Palliative Care: A Critical Review of Support Provided by Australian Guidelines for Life-Limiting Chronic Conditions.
Yan LS, Cheng BC, Zhang SF, Luo G, Zhang C, Wang QG, et al. Tibetan Medicine for Diabetes Mellitus: overview of pharmacological perspectives. Front Pharmacol. 2021. https://doi.org/10.3389/fphar.2021.748500. 12:748500. Published 2021 Oct 21.
Fu K, Xu M, Zhou Y, Li X, Wang Z, Liu X, et al. The Status quo and way forwards on the development of tibetan medicine and the pharmacological research of tibetan Materia Medica. Pharmacol Res. 2020;155:104688. https://doi.org/10.1016/j.phrs.2020.104688.
Acknowledgements
We thank Jia Can and Luo Sang Ren Zeng (Lazi County Health Service Center, Xigatse, Tibet, PR China) for their assistance in conducting research and collecting questionnaires for this study.
Funding
National Natural Science Foundation of China (72104183), Scientific Research Project of Shanghai Municipal Health Commission (20234Y0057), Projects of the Committee of Shanghai Science and Technology (20Y11913700), Shanghai Municipal Medical and Health Outstanding Academic Leader Program (GWVI-11.2-XD40), Guangdong Association of Clinical Trials (GACT)/Chinese Thoracic Oncology Group (CTONG) and Guangdong Provincial Key Lab of Translational Medicine in Lung Cancer (2017B030314120), and Beijing CSCO (Sisco) Clinical Oncology Research Grant (Y-HS202101-0205).
Author information
Authors and Affiliations
Contributions
In this analysis, Sen Yang and Dehua Yu contributed to the conception and design of the study; Sen Yang, Huaxin Zhao, and Junpeng Wang performed the statistical analyses; Hanzhi Zhang, Hua Jin, Le Ma and Zhen Pu acquired the data; Huaxin Zhao and Xuhua Ge supervised the data analysis and interpretation; Sen Yang and Xiaomin Niu drafted the manuscript; Kyle Stirling, Dehua Yu, and Xiaomin Niu critically reviewed and revised the manuscript; Sen Yang, Dehua Yu and Xiaomin Niu had the primary responsibility for the final content. Dehua Yu and Xiaomin Niu contributed equally to this work. All authors critically reviewed the manuscript and approved the final draft.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Yangpu Hospital affiliated with Tongji University’s Institutional Review Board (No. of ethics approval: LL-2022-LW-007). All study participants provided informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, S., Zhao, H., Zhang, H. et al. Current status and continuing medical education need for general practitioners in Tibet, China: a cross-sectional study. BMC Med Educ 24, 265 (2024). https://doi.org/10.1186/s12909-024-05143-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05143-5