Abstract
Background
My Dispense is a virtual pharmacy simulation developed for students to train and practice dispensing skills in a safe environment that causes no harm to patients. This study was aimed to investigate learners’ perspectives on the effectiveness of MyDispense and its suitability to integrate into the clinical pharmacy module in Viet Nam.
Methods
A mixed method approach was undertaken. Fourth- and fifth-year pharmacy students at University of Medicine and Pharmacy at Ho Chi Minh city and community pharmacists were invited to complete a survey questionnaire and to participate in semi-structured interviews.
Results
A total of 92/99 participants agreed to take part, of which 75% of participants were students and 65.2% were female. About three-quarters of the participants agreed or strongly agreed that MyDispense improved their dispensing skills, such as patient counselling (70.6%) and collecting patient infomation (85.9%). The majority of the participants (84.8%) considered that MyDispense was suitable to integrate into the clinical pharmacy module. Qualitative analysis from the interviews highlighted the advantages of MyDispense, comprising high interactivity with users, safe environment for practicing medication dispensing, and diversity of common marketed medications. In addition, certain barriers of this programme were also reported, including the complicated process, inconsistent quality of product images, and mixed English-Vietnamese languages.
Conclusions
From learner’s perspectives, MyDispense was an effective tool to enhance dispensing skills and was suitable to integrated into the clinical pharmacy module in Viet Nam.
Similar content being viewed by others
Background
A pharmacist is required to have strong foundation in pharmaceutical knowledge and skills in dispensing process [1]. This expected learning outcome, perhaps, is one of the biggest challenges to the pharmacy curriculum in Viet Nam. Conventionally, pharmacy students have been provided a series of lectures on medication use to obtain sufficient pharmaceutical knowledge [2]. However, whether skills for pharmacy practice are well trained is uncertain due to limited training hours in the curriculum across universities in Viet Nam [3, 4]. In addition, the internship at a pharmacy only takes place in the final year of the 5-year pharmacy programme and lasts for one week; accordingly, students could hardly conceptualize the pharmaceutical activities and operation procedures at community pharmacies within this short duration [2, 3]. Therefore, a self-learning tool that provides the visualization of pharmaceutical activities in a community pharmacy is necessary, especially when human resources are limited.
In 2011, MyDispense, a web-based pharmacy simulation programme, was first developed by Monash University in Australia [5]. This programme facilitated students with unique in-person experience of dispensing medications to a virtual patient. MyDispense encouraged student-patient communication by some embedded functions in the programme such as patient fact-finding and patient counselling. Notably, MyDispense provided a supportive environment for self-learning in which students could engage in the entire dispensing process, encounter simulated failure, and then receive specific case-by-case feedback from their instructors. By utilising MyDispense, the students were expected to familiarise with common scenarios at a community pharmacy prior entering their internship at a real-world pharmacy.
Since the introduction in 2011, MyDispense has been integrated into the undergraduate pharmacy programmes in Australia, United States of America, United Kingdom, Singapore, Turkey, and Ireland [6]. This integration has received several positive feedbacks. In previous studies, participants found that MyDispense was more interesting than paper-based cases and enhanced their confidence to communicate with patients after completing the provided exercises [7,8,9]. However, barriers to implementing MyDispense were noted such as some technical issues (e.g. unstable internet access), the cost of maintenance and training, and importantly, the additional workload for both students and lecturers [10, 11]. In Viet Nam, MyDispense was customised for pharmacy students with 30 exercises and 100 medications commonly dispensed in the context of Vietnamese healthcare system. The simulation programme was intended to be blended in the clinical pharmacy modules at University of Medicine and Pharmacy at Ho Chi Minh city (UMP) which were delivered to fourth-year pharmacy students. The customised scenarios were designated to facilitate students’ self-learning with the objectives of mastering pharmacy dispensing knowledge and skills.
This study was aimed to investigate learners’ perspectives on the effectiveness of MyDispense in learning of dispensing skills (patient information collection, prescription review, medication identification, recommendation of over-the-counter (OTC) medications, and patient counselling) and the suitability of this simulation programme to integrate into the clinical pharmacy curriculum in Viet Nam.
Methods
Study population
The study inclusion criteria were pharmacists who had been working in community pharmacies or hospital pharmacies for at least one year, and fourth- and fith-year pharmacy students at UMP, Viet Nam from 09/2021 to 07/2022. At the time of conducting this study, fourth- and fith-year pharmacy students had completed their clinical pharmacy modules related to dispensing skills at community pharmacies.
Sample size
A required sample size was calculated using the following formula where p was the estimated percentage of learners who were satisfied with learning experience using MyDispense:
\(({Z}_{1-\frac{\alpha}{2}}\)= 1.96 with α = 0.05, d = 0.1)
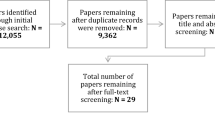
Based on a study by Johnson et al., p equal to 65.7% was used to calculate the sample size [12]. Thus, the minimum sample size was 87. In this study, invitation emails were sent to 99 participants.
Study design and data collection
Purposive sampling with the maximum variation approach was used to recruit participants. An invitation was sent to potential participants via email. Pharmacists and pharmacy students volunteering to take part in the study were asked to complete an informed written consent. Subsequently, participants were instructed to use MyDispense via a tutorial video, then required to complete at least one out of five standard dispensing excercises within two weeks prior to entering the study. An automatic reminder email was sent to all participants one week before the deadline. There were no time boundary for each exercise. Participants were allowed to redo five exercises as many times as they wished and also received explanatory notes and feedback immediately after submitting each exercise. All five exercises were developed by the Department of Clinical Pharmacy, UMP, to represent common situations in a community pharmacy in Viet Nam. The five exercises were validated by a committee consisting of 5 senior lecturers and clinical pharmacists.
The original language of command button labels used in MyDispense was translated into Vietnamese to facilitate understanding and the prescription form was modified to align with current regulations in Viet Nam. Images of 100 brand name products marketed in Viet Nam were also added.
Subsequently, a mixed quantitative and qualitative method was undertaken with two phases:
Phase I: An online questionnaire was sent to participants via email (Supplementary 1). All responses were encrypted anonymously. Demographic data including gender and year of study (if participants were pharmacy students) were collected. Participants’ perspectives toward conventional education (the realistic of the traditional paper-based scenarios, the interest of learners toward traditional class, the duration of on-class learning, and their self-confidence in the knowledge and skills gained) were collected using a five-point Likert scale (1 – strongly disagree; 2 – disagree; 3 – neutral; 4 – agree; 5 – strongly agree). The participants were also asked to rate statements about the effectiveness and suitability of MyDispense using the same Likert scale.
Phase II: Participants who completed the questionnaire in phase I were stratified into three groups of fourth year students, fifth year students, and pharmacists. We then selected a random participant from each group to send an invitation email for a face-to-face semi-structured interview. If the recipient refused to take part in the interview, the next random participant in the same group was recruited. The main content of the interview comprised the perspectives of learners regarding the advantages and disadvantages of MyDispense (Supplementary 2). Invitations were sent to participants until data saturation was reached (i.e. no more new perspectives or insights were found in the interview). Each interview was conducted by two authors: M. L-C. D. used a topic guide with predetermined open-ended questions and provided prompts to facilitate discussion while K. T-T. N. observed the interviewee’s reactions and recorded a summary of the interview details. Each interview lasted from 10 to 15 minutes and was audio-recorded.
Statistical analysis
Data from the online questionnaire were collected, stored, and processed using Microsoft Office Excel and Word 365, and the Statistical Package for Social Sciences (SPSS) version 20.0. Quantitative data such as the categorical variables and Likert scores were presented as frequencies or percentages.
All recordings from the interviews were transcribed verbatim. Data collection and analysis were conducted simultaneously to detect the data saturation point. Transcripts from the interviews along with noted summaries were read iteratively to familiarise context, followed by content analysis to identify themes relevant to MyDispense. Two investigators M. L-C. D. and K. T-T. N. independently analysed the recorded data. If any disagreements between the two investigators could not be addressed through discussion, the final judgment would be made by the third senior investigator (H. Q. N.). The phase II (qualitative approach) was reported according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines (Supplementary 3).
Results
Participants characteristics
Of 99 potential participants approached, 92 (93%) were agreed to take part in the study. Among 92 eligible participants, 65.2% were female. Students accounted for 75% (n = 69) of participants. In phase II, data saturation was reached after 13 participants were interviewed (3 pharmacists and 10 students). Details of participants’ characteristics are presented in Table 1.
Effectiveness of MyDispense simulation
A total of 56/92 (60.9%) participants supposed that their confidence on handling a dispensing task was improved after using MyDispense compared to 19/92 (21.7%) who also admitted the same effect with the conventional education (Fig. 1; Table 2). The majority of participants (both pharmacists and students) agreed or strongly agreed that MyDispense improved learners’ knowledge and dispensing skills (Table 2). Between pharmacists and students, we found a slightly higher percentage of pharmacists who agreed that MyDispense improved learners dispensing skills including collecting patient medical information, reviewing prescriptions, and recommending OTC medications (Table 3).
Suitability of MyDispense in the clinical pharmacy module
A total of 78/92 participants (84.8%) agreed/strongly agreed that it was necessary to integrate MyDispense into the pharmacy curriculum. Pharmacists and students shared the same perspectives toward the suitability of MyDispense (Table 3). Majority of the participants (71.8%) believed that the scenarios in MyDispense were realistic, interesting (68.5%), interactive (65.2%) and strongly connected to the intended learning objectives (77.2%). However, 17.4% of participants disagreed that MyDispense was a user-friendly programme (Table 2).
Learner’s perspectives on MyDispense simulation
After 13 interviews, three main themes regarding the advantages of MyDispense were identified (Table 4). Firstly, eight participants agreed that this simulation was advanced with an interactive platform. In particular, the design of the virtual pharmacy was elegant and perfectly replicated a real modern pharmacy. Virtual patients were designed to mimic the characteristic of real patients including their emotions such as anxiety, anger, or impatience. One participant also reported that learners could gather sufficient patient medical information by the “fact-finding” function. One participant enjoyed the accessibility of MyDispense on different mobile devices including smartphones.
Secondly, almost half of the participants remarked that MyDispense offered a safe practicing environment for learners with no prior experience. Some participants also appreciated that they could redo each exercise as many times as they wished, which was helpful to reduce potential mistakes regarding patient safety.
Finally, more than half of the participants indicated that MyDispense possessed a diversity of commonly marketed medications. Three participants revealed that they could easily familiarise themselves with some common brand name products through the provided scenarios before entering the pharmaceutical market (Table 4).
Nevertheless, some of the barriers were also mentioned by most of the participants, including complicated learning process (time consuming to get used to the programme), inconsistent quality of product images (unreadable medication labels), and mixed languages (Vietnamese and English).
Discussion
To our knowledge, this study is the first one that examined the perception of Vietnamese learners toward a virtual pharmacy simulation programme. Similarly to previous findings from other countries [7,8,9], the majority of participants, including pharmacy students and pharmacists, agreed that MyDispense was an effective tool to train dispensing skills and should be integrated into the pharmacy curriculum in Viet Nam.
MyDispense enhanced learners’ dispensing skills and supported self-learning. After using this simulation programme, the proportion of participants who were confident to handle a dispensing task increased from 21.7 to 60.9%. These findings were consistent with previous studies in which 71-75.4% of users agreed/strongly agreed that MyDispense improved their knowledge and dispensing skills [12,13,14]. Simulation activities have been reported to promote better knowledge retention and performance of clinical skills [15, 16]. Moreover, it should also be noted that the pharmacists participating in our study favoured how MyDispense improved learner’s ability to collect patient medical information, review prescriptions, and recommend OTC medications, while the pharmacy students preferred how the simulated scenarios enhanced their counselling skills (Table 3).
Majority of participants believed MyDispense should be integrated into the pharmacy curriculum. These findings were consistent with previous studies conducted in the United States [13, 14]. Nevertheless, a study by Shin et al. reported only 20.7% of users agreed to integrate MyDispense into their curriculum [8]. This discrepancy may be explained by the lack of sufficient training prior to the use of MyDispense as presented in the study. It should be mentioned that pharmacists were also recruited in our study. We found that the proportion of students who agreed/strongly agreed to integrate this simulation to their course was lower than that of pharmacists (82.6% vs. 91.3%). This is possibly because the pharmacists expected what they should have been trained for their current positions at their pharmacies, and the students might be concerned about the pressure of additional homework and classwork tasks.
Integrating MyDispense into the clinical pharmacy curriculum will probably tackle current challenge of the traditional teaching method by optimising students learning experience. In our current pharmacy curriculum, we did not provide any specific tool for students to conceptualize their professional activities or for self learning at home [2]. Most of our participants agreed/strongly agreed that the feedback function of MyDispense encouraged their self-learning compared to the traditional teaching method. A previous study indicated that MyDispense supported students to learn from their own experience [16]. Additionally, the participants reported that MyDispense provided more realistic experience than the conventional education with paper scenarios, which was also highlighted in previous studies [16, 17].
In the semi-structured interviews, the participants described three main advantages of MyDispense: high interactivity with users, provision of safe environment for dispensing practice, and the diversity of common marketed medications. This could be due to the fact that MyDispense was the first simulation programme adapted for Vietnamese users. To date, the current education approach in Viet Nam has not provided enough individual self-training before the pharmacy internship period. Moreover, pharmacy students were more familiar with names of active ingredients through class lectures than brand names of medications; therefore, three-dimension images of medication packaging embedded in MyDispense could enhance students’ ability to recognise common brand-name products which they may encounter during their pharmacy internship or after graduation.
Nevertheless, the participants also outlined certain barriers when using MyDispense, comprising complicated learning process, inconsistent quality of medication images, and mixed languages. A previous study also reported that students in Philippines encountered connectivity issues and gadget incompatibility when using MyDispense [18]. This discrepancy may be due to different adoptation process in our study. The participants were only instructed to use MyDispense with a short video instead of in-person lecturing which was undertaken in previous studies [16, 17]. By the time of the study conducted, the version of MyDispense was originally set English as default language instead of Vietnamese [6]. However, these problems could be addressed in the future with further improvement and adaptation of MyDispense.
While the results are in favor of integrating MyDispense into the pharmacy curriculum, they should be carefully interpreted. Firstly, the findings are vulnerable to bias resulted from a considerable proportion of participants (41.3%) completed less than 3 out 5 excercises. Secondly, in this present study, the effectiveness of MyDispense was evaluated according to learners’ opinions which could be subjective. Moreover, the endowment effect may have occurred as participants were allowed to redo the exercises as many times as they wished. Nevertheless, we accepted this practice as the participants probably took time to familiarise themselves with MyDispense which had first been developed in the non-Vietnamese context despite our adaption. Further studies are warranted to re-assess the effectiveness of MyDispense by objective measures such as exam scores before and after using this novel virtual programme.
Conclusions
From learners’ perspectives, MyDispense effectively improved their dispensing skills and was suitable for the integration to the Vietnamese pharmacy curriculum. Further investigation is warranted to assess feasibility and acceptability after MyDispense is integrated into the pharmacy education curriculum in Viet Nam.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tran VT. Innovation of pharmacy program in UMP to adapt oneself to the AUN QA and CIDPHARMEF. Paper presented at: Innovation to transform pharmacy higher education program; 2022 Mar 30–31; Hanoi, Vietnam.
Vo TH, Bedouch P, Nguyen TH, Nguyen TL, Hoang TK, Calop J, Allenet B. Pharmacy education in Vietnam. Am J Pharm Educ. 2013;77(6):114.
Baecker D, Mai Dung DT, Pham-The H, Hai-Nam N. Comparison of the University Pharmacy Education Programs in Germany and Vietnam. Pharmacy. 2022;10(6):146.
Nguyen VH, Nguyen TQM, Chau DT, Pham TA, Chan TN, Nguyen TTP. Pharmacy and patient care: evolution of its practice and education in Vietnam since 2012. R Clin Pharm. 2023;1:49–56.
Ambroziak K, Ibrahim N, Marshall VD, Kelling SE. Virtual simulation to personalize student learning in a required pharmacy course. Currents in Pharmacy Teaching and Learning. 2018;10(6):750–6.
MyDispense. About-mydispense. Available from: https://info.mydispense.monash.edu/wp-content/uploads/2019/07/About-mydispense.pdf.
Nicolazzo JA, Chuang S, Mak V. Incorporation of MyDispense, a virtual Pharmacy Simulation, into Extemporaneous Formulation Laboratories. Healthcare: MDPI; 2022.
Shin J, Tabatabai D, Boscardin C, Ferrone M, Brock T. Integration of a community pharmacy simulation program into a therapeutics course. Am J Pharm Educ. 2018;82(1).
Dameh M. A report of second year pharmacy students’ experience after using a virtual dispensing program. J Pharma Care Health Sys. 2015;2:003.
Singh HK, Mak V, Sewell K, Malone DT. Barriers and facilitators to implementing simulation into pharmacy programs globally. J Pharm Policy Pract. 2023;16(1):1–3.
Mak V, Fitzgerald J, Holle L, Vordenberg SE, Kebodeaux C. Meeting pharmacy educational outcomes through effective use of the virtual simulation MyDispense. Currents in Pharmacy Teaching and Learning. 2021;13(7):739–42.
Johnson AE, Barrack J, Fitzgerald JM, Sobieraj DM, Holle LM. Integration of a virtual dispensing simulator MyDispense in an experiential education program to prepare students for community introductory pharmacy practice experience. Pharmacy. 2021;9(1):48.
Kebodeaux C, Sewell K. Implementation of community pharmacy dispensing software (MyDispense) in an advanced pharmacy practice course. 2016.
Rude TA, Eukel HN, Ahmed-Sarwar N, Burke ES, Anderson AN, Riskin J, et al. An introductory over-the-counter simulation for first-year pharmacy students using a virtual pharmacy. American Journal of Pharmaceutical Education; 2022.
Akhu-Zaheya L, Gharaibeh M, Alostaz Z. Effectiveness of Simulation on Knowledge Acquisition, Knowledge Retention, and self-efficacy of nursing students in Jordan. Clin Simul Nurs. 2013;9:e335–e42.
McDowell J, Styles K, Sewell K, Trinder P, Marriott J, Maher S, et al. A simulated learning environment for Teaching Medicine dispensing skills. Am J Pharm Educ. 2016;80(1):11.
Ferrone M, Kebodeaux C, Fitzgerald J, Holle L. Implementation of a virtual dispensing simulator to support US pharmacy education. Currents in Pharmacy Teaching and Learning. 2017;9(4):511–20.
Amatong A, Asentista H, Diasnes C, Erispe K, Malintad K, Paderog H, et al. Learners’ perceptions on my dispense virtual Simulation in the Philippines. Int J Innovative Res Sci Eng Technol. 2022;7:1627–36.
Acknowledgements
The authors would like to acknowledge Keith Sewell, Keenan Beaumont, and their team from Monash University, for their technical assistance with customising MyDispense to Vietnamese. The authors would like to acknowledge and thank the University of Medicine and Pharmacy at Ho Chi Minh City for their financial support. Finally, the authors would also like to thank all lecturers of the Department of Clinical Pharmacy for their valuable expertise and contributions in developing and validating dispensing scenarios embedded in this simulation programme.
Funding
This study was financially supported by the University of Medicine and Pharmacy at Ho Chi Minh city, Viet Nam.
Author information
Authors and Affiliations
Contributions
Kim TT Nguyen, Khoi N Nguyen, Ho N Nguyen, Hoang TM Nguyen, Hoa Q Nguyen conceived and designed the study. Kim TT Nguyen and My LC Dao performed the statistical analysis and drafted the manuscript. All authors examined and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the UMP Research Ethics Committee (REC number: 599/HDDD-DHYD). The methods were performed in accordance with the Declaration of Helsinki. Informed written consent was obtained from all participants before their participation in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nguyen, K.T., Dao, M.L., Nguyen, K.N. et al. Perception of learners on the effectiveness and suitability of MyDispense: a virtual pharmacy simulation and its integration in the clinical pharmacy module in Viet Nam. BMC Med Educ 23, 790 (2023). https://doi.org/10.1186/s12909-023-04773-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04773-5