Abstract
Introduction
Breaking bad news (BBN) is inevitable in medicine and is one of the most important and difficult professional tasks of physicians. The main aims of this study are to evaluate residents’ practice of BBN and identify perceived barriers to its implementation.
Methods
In this cross-sectional study in 2021, 240 residents from medical, surgical, and emergency medicine departments completed the demographic questionnaire, the Persian SPIKES questionnaire (P-SPIKES), and the researchers-made questionnaire of Barriers to Breaking Bad News (BBBN). In addition, they were asked about their previous experience, previous training, and their perceived level of competence in BBN.
Results
46.5% and 36.84% of residents rated their perceived competence in BBN and managing the patient’s emotions during BBN as good or very good, respectively. The most difficult aspects of BBN for residents were expressing upsetting information (78.1%) and not disappointing the patient while being honest (58.3%). The mean and standard deviation of the score of the P- SPIKES was 55.92 ± 6.84. The most common SPIKES item was not giving bad news by phone (98.9%). The SPIKES total score was only related to age (positive relationship). The most commonly reported barriers to BBN were concerns about controlling the patient’s emotions (61%) and the aggressiveness of the patient or companions (52.6%). A significant proportion of participants identified lack of training (28%) and insufficient skills (21.9%) as significant barriers to BBN.
Conclusions
The skill of residents in BBN is insufficient in some aspects and points to the need for BBN training courses during residency. BBN is difficult for residents in some aspects and residents may perceive barriers. To overcome the existing barriers and increase residents’ confidence in BBN, strategies such as incorporating BBN training into residency educational curricula and communication skills are recommended.
Similar content being viewed by others
Introduction
Bad news is defined as any information that has a negative and significant effect on an individual’s outlook on her or his future [1]. Bad news can include information related to a chronic disease, a life-altering illness, or an injury leading to significant change [2]. Patients dislike the way doctors indicate and label negative news as “unfortunate or bad” [3]. They prefer to view the news as something to process and deal with under the direction of their doctor [3]. Therefore, using “serious news” is recommended instead of bad news (4). Many patients seek out trustworthy information before making important decisions. However, those who find it too serious may exhibit behaviors like denial, shunning, or downplaying the significance of the knowledge, while still receiving treatment (5). It is unproven that getting serious medical information will invariably result in psychological harm (5). Therefore, even if doctors suspect it could harm the patient, they are not permitted to conceal medical information (6). Most patients prefer to know their diagnosis, but the amount of information they seek out varies depending on culture, level of education, age, and gender (2, 7,8,9). Younger patients, females, and those with high education levels prefer more comprehensive and detailed information (2). Cultural norms and ethnicity also have an impact on the amount of desired information. According to one study, Korean Americans and Mexican Americans prefer a family-centered medical decision model, whereas African Americans and European Americans prefer a model with greater individual patient autonomy (2). Given these notifications, physicians must notice and inquire about patients’ preferences before giving serious news [2].
There have been some recommendations for the giving bad news over the years that are primarily based on expert opinion rather than empirical evidence [10]. These universal models have been proposed and utilized effectively to guide and enhance the delivery of bad news among physicians. One of the most popular guidelines for breaking bad news (BBN), especially for cancer patients, is the SPIKES protocol [1].
The SPIKES protocol is an acronym that refers to six steps recommended for BBN: (S) setting up the interview; (P) assessing the patient’s perception; (I) obtaining the patient’s invitation; (K) giving knowledge to the patient; (E) addressing the patient’s emotions with empathic responses; and (S) strategy and summary (1). The first step “S”, or setting up, refers to the preparation of the environment, preferably in a private, reserved, and welcoming place. The second phase, “P,“ or perception, relates to determining whether the individual who received the news is aware of their own condition or disease by asking open-ended questions to assess the patient’s knowledge, expectations, and readiness to take the information. The third phase “I”, invitation, entails determining to whom and to what extent the patient wishes to disclose the news. The fourth stage “K” is knowledge, in which information is presented with a caring and honest demeanor, according to the patient’s needs and desires. Step “E”, Emotions, entails observing and listening to the patient, identifying the patient’s concerns, emotions, and reactions, and managing the patient’s emotions by employing identifying, acknowledging, and validating statements. The last step “S”, summary and strategy, is an important step for summarizing everything that has been delivered and checking whether the patient has understood it. It also provides an opportunity to develop a strategy in cooperation with the patient and identify the patient’s support resources [1, 5].
Aside from these steps, mental preparation is essential for those who are tasked with delivering serious news. They must review the patient’s condition, previous treatments, results, and scripts, anticipate the patient’s questions about the prognosis and treatment failure, and prepare to manage the patient’s emotions (11). It is also beneficial to note any previous discussions with other healthcare workers to gain an understanding of the patient’s prior knowledge and expectations [11]. As a result, the SPIKES was modified in 2005 to the PSPIKES. Users of this model reported more confidence in their ability to discuss unfavorable medical information with their patients [11].
Physicians must be able to deliver bad news [12]. BBN is one of the most important duties of physicians and medical staff, despite its importance, barriers to BBN have been identified. According to research, time constraints, language differences, personal fears, the illiteracy of the patients, crowded wards with no privacy, and a lack of training are all significant barriers to BBN [13].
Most undergraduate and graduate medical programs do not typically provide specialized training in BBN [14]. There is relatively little information on how residents deliver bad news in recent years. Previous studies had limitations such as small sample sizes, different study samples, and being limited to only a few specialties. Some of these limitations are addressed in this study.
The aims of the current study were to survey the skill of residents in medical, surgical, and emergency medicine departments regarding BBN based on the SPIKES protocol and to identify perceived obstacles to implementing it. We also looked at doctors’ demographic characteristics, their training in communication skills, and their experience with serious news, all of which can influence how physicians deliver bad news. Furthermore, we asked general questions about BBN, such as how often they deliver bad news and the extent of their need to receive additional academic training. The findings of the study can provide information about the current practice of residents in delivering bad news and increase their proficiency by assisting policymakers in developing the necessary strategies to overcome perceived obstacles.
Methods
This cross-sectional study was conducted in 2021 at two general medical hospitals affiliated with Iran University of Medical Science. Participants included residents from medical, surgical, and emergency medicine departments who agreed to fill out the questionnaires and participation was voluntary and anonymous. All residents who agreed to complete the questionnaires were included in this study, but the residents who did not have a strong clinical performance in their career (radiologists and pathologists) and those whose responses to questionnaires were incomplete were excluded. At first, demographic data and some questions related to residents’ opinions about delivering bad news, their previous experiences of receiving or delivering bad news, and their prior training in BBN were assessed. Then, the participants were asked to complete the SPIKES and the barriers to BBN questionnaire.
Material
The Persian questionnaire of SPIKES (P-SPIKES)
P-SPIKES showed good reliability and validity [15]. This questionnaire includes 16 questions and two psychological and environmental domains. The items are scored on a 5-point Likert scale (always, often, sometimes, rarely, and never) with minimum and maximum total scores of 16 and 80, respectively; higher scores show the proficiency of the physician. Each of the domains has 8 items with a minimum score of 8 and a maximum score of 40. In the majority of questions, always and often were considered the favored option; in a few questions, rarely and never were preferred [15, 16]. Also, some questions regarding the preparation step were added to the questionnaire.
Barriers to Breaking Bad News Questionnaire (BBBN)
We used the BBBN to identify the barriers to delivering bad news. To provide the BBBN, an initial set of items was prepared by reviewing the literature and consulting a multidisciplinary panel of experts affiliated with ***(comprising one cardiologist, one neurologist, one psychiatrist, one emergency medicine specialist, one oncologist, one internal medicine specialist, and four surgeons in different specialties). In the quantitative assessment of the content, the experts rated the items of the questionnaire on a 5-point ordinal scale to determine the potential significance of the various barriers using the formula “Impact Score = Frequency (%) ×Importance”, which frequency (%) represents how often they perceived the item as a barrier to BBN and importance shows a subjective measure of how the significance of the item is on a scale of 1 to 5 (importance = 5). Based on the minimum acceptable score of 1.5, 14 items were selected and included in the initial draft of the questionnaire [17].
To determine the face and content validity of the questionnaire, the same experts from various specialties were asked to provide corrective opinions on the 14 items. In the qualitative assessment, the experts were asked to offer their opinions about each item in terms of proper words, grammar, understandability of the items, and appropriate time for completion of the questionnaires to modify the items according to their feedback. The content validity index (CVI) was used to determine to the extent each item was in terms of clarity, simplicity, and relevancy on a 4-point ordinal scale (from 1 = the lowest to 4 = the highest). A CVI > 0.79 was considered acceptable [18]. The content validity rate (CVR) used to determine whether an item was necessary in the questionnaire on a 3-point ordinal scale. According to the Lawshe method given a panel size of ten experts, a CVR > 0.62 was considered acceptable [19].
Finally, 25 residents completed the questionnaire twice with an interval of 10–14 days to determine the temporal reliability of the BBBN using the test-retest method. The CVI, CVR, and temporal reliability of the questionnaire were calculated to be 0.94, 0.85, and 0.81, respectively. The final questionnaire consisted of 11 items focusing on 10 barriers and an open-ended item that inquired about additional items. Based on the acceptable results, this questionnaire was used to collect the information required for this research.
Sample size
The ratio estimation formula was used and an initial sample size of 216 people was calculated. Considering 10% of the non-response rate, 240 eligible residents participated in the study by convenience sampling method as the final sample size.
Ethics
The study protocol was approved by the Research Ethics Committee of ***.
Data analysis
The data were analyzed using SPSS version 22. First, descriptive statistics analyses including frequencies, percentages, means, and standard deviations, were used to measure characteristics of the participants and their experiences with bad news. The distribution of the normality of the P-Spikes total score was examined using the Kolmogorov–Smirnov test. The means of P-Spikes domains were compared using independent t-test. The association between the mean of P-Spikes total score and categorical variables determined using independent sample t-test and one-way ANOVA (respectively for two groups and more than two groups of the variable). Pearson’s correlation test was used for association of P-Spikes total score and age. P-value ≤ 0.05 was considered significant.
Results
After excluding the uncompleted questionnaires of the 240 participants, the data of 228 first- to fourth-year residents in medical, surgical, and emergency medicine departments were included in this study. Table 1 shows the participants’ demographic data and attitudes toward delivering bad news.
31.6% of residents reported delivering bad news to their patients more than five times in the previous month and reported an average of 10.93 ± 6.8 min for each patient. On a 5-point scale, 46.5% and 36.84% of residents rated their perceived competence in BBN and managing the patient’s emotions during BBN as good or very good, respectively. The most difficult aspects of giving bad news were expressing upsetting information (i.e., new serious medical information, relapse of disease, death, or permanent loss of an organ or organ function) (78.1%), and not disappointing the patient while being honest (58.3%).
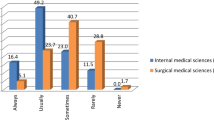
Figure 1 demonstrates the percentage of different skills used by residents for delivering bad news.
The cumulative percentage of always and often responses to each P-SPIKES item is shown.
According to the findings, among the SPIKES skills, not giving the bad news over the phone (98.9%) and wearing a medical gown while delivering the bad news (92.1%) were most common, while informing the patient of the approximate survival time if she/he is interested (23.7%), making physical contact with the patient (34.6%), and sitting next to the patient (35.1%) were the least frequent when delivering the bad news. Regarding resident characteristics, only gender showed an association with the items of P-SPIKES; male residents were more likely to arrange for privacy (p = 0.007) and to inform the patient of the approximate survival time (p = 0.012), whereas female residents were more likely to wear a medical gown (p = 0.001) and to break the bad news in person (p = 0.006). There was no significant difference between the residents from different departments (P > 0.05).
In response to the two questions from the preparation stage, which were not included in the SPIKES questionnaire, but we inquire of residents, the majority of participants (73%) stated that they review the medical history and mentally rehearse giving bad news. Also, 83% stated that they prepare themselves to face and address the patient’s emotions before BBN.
The P-SPIKES total score had a mean and standard deviation of 55.92 ± 6.84 (Table 2). No statistically significant distinction was observed between the two domains of delivering bad news (P = 0.072).
Table 3 shows the association between the variables and the SPIKES total score. The skill of residents to BBN was only related to age (p = 0.014). Older residents were significantly more likely to arrange for privacy (p = 0.041), ensure adequate time (p = 0.004), sit next to the patient (p = 0.027), assess the patient’s perception of her/his medical condition before BBN (p = 0.023), try to determine how much the patient wants to know (p = 0.036), and introduce the patient to a supportive team after BBN (p = 0.031).
Regarding the barriers to BBN that residents introduced, the results of BBBN showed that concerns about controlling the patient’s emotions (61%), the aggressiveness of the patient or the companions (52.6%), and the reluctance of the patient’s companions to give bad news to the patient (39.9%) were among the most prevalent barriers to giving bad news among medical residents (Table 4).
Discussion
The current research aimed to evaluate residents’ skills in BBN and to identify perceived barriers to BBN. In the present study, about one-third of respondents reported frequently breaking bad news (more than five times in the last month). The study found that residents don’t perform well in some steps of BBN, particularly empathy and nonverbal delivery (allocating time, sitting down, making physical contact), but they perform better in preparation step and verbal aspects of delivering bad news, such as correctly applying the steps of invitation and knowledge. The vast majority of residents (87.3%) agreed that bad news should be delivered to the patient and identified the physician as the best person to deliver bad news (95.2%). Despite this, more than half rated their perceived ability to deliver bad news as not good, and approximately two-thirds rated their ability to manage patients’ emotions as moderate or low. The principles of informed consent, patient autonomy, and case law have established clear ethical and legal obligations to provide patients with as much information about their illness and treatment as they desire [20].
The lack of formal training in BBN as a basic clinical task may be one of the factors contributing to low self-confidence and feeling difficulty to do BBN (21). It is worth noting that education will not facilitate communication in BBN unless it is combined with training. Training will allow clinicians to overcome the stress of BBN and develop confidence(22,23,24). In the current study, a significant proportion of residents reported having no theoretical or clinical training in either BBN (35.5%) or dealing with the patient’s emotions (57%). These findings are consistent with previous studies in our country, though it seems formal training for BBN has improved in recent years [25,26,27]. The findings were also in line with research from other countries. A cross-sectional survey that targeted all healthcare providers of the intensive care units of 40 countries revealed that only one-third had received formal training [28]. This survey found that younger healthcare workers and those with fewer years of work experience had been trained less [28]. The current study showed that the ability to BBN (as measured by the SPIKES score) was only associated with age and has not shown a significant relationship with years of professional experience and training specialty (medical, surgical, and emergency medicine). Differences in the SPIKES scores may be related to factors such as the age, gender, and cultural background of the residents [29]. Since awareness of the need for training in BBN has increased in health care over time, more residency programs have incorporated BBN training into their curriculum. However, the ratio of formally trained healthcare providers is not proportional to the anticipated need, highlighting the global need to develop BBN educational courses [28].
Another important finding of this study was that there was no significant difference in performance between residents with and without prior training, suggesting that the current training programs are ineffective and should be modified. Implementing a strategy in which residents adhere to a predetermined protocol is also critical. Lectures, small-group discussions, role-playing with peers and standardized patients (SPs), and learning in the context of patient care are all potential strategies for providing education in the delivery of bad news [21].
According to another finding of the study, the most difficult aspects of giving bad news were conveying upsetting information to the patient, not disappointing the patient while being honest, and addressing the patient’s emotions. These difficulties can be greatly facilitated by using communication skills and several strategies, such as exploring the patient’s knowledge, expectations, and hopes (5). BBN is a complex communication task, of which the verbal component is only one. So, it requires other skills, such as responding to patients’ emotional reactions, patient involvement in decision-making, coping with the stress arising from patient expectations, the participation of multiple family members, and the manner of how to give hope in an unfavorable conditions [5]. BBN can be facilitated by understanding the process, using a step-by-step approach, and applying well-established communication and counseling principles [30].
BBN has been shown to be necessary and vital in reducing the traumatic effects of bad news on patients’ illness perceptions, disease coping, and life expectancy, and could encourage the patient to engage actively in difficult decisions.(31,32,33) However, the personal and institutional barriers make it difficult for residents to apply guidelines. Barriers, such as the aggressiveness of the patient or companions and the reluctance of the patient’s companions to BBN to their patient, were defined as more common in the current study than in other studies [34]. Bad news delivery can be influenced by culture-bound attitudes, religious values, and medical traditions [35]. In comparison to the United States [36], research in Brazil [37], Sudan [38], Saudi Arabia [39], and Korea [40] revealed a higher rate of bad news transmission to the family rather than directly to the patients, and families are heavily involved in the patient’s decisions. In this study, the most common barrier to giving bad news was concern about controlling the patient’s emotions. Furthermore, a significant proportion of participants identified a lack of training or insufficient skills as barriers to BBN. Empathy is one of the best methods to help patients feel less alone and validate their thoughts and feelings [5]. Communication skills training and the development of a therapeutic relationship positively impact patients and their relatives [30]. Although patients value knowledge and professional guidance, focusing solely on facts and ignoring the patient’s emotional requirements results in less positive responses than prioritizing the patient’s emotional needs [41]. Of importance, medical education, particularly during internship and residency, has the potential to suppress empathy and replace communication with techniques and procedures [42]. The problem is partly due to the tendency of medical students to prioritize technical proficiency over the significance of communication skills [26]. As a result, communication proficiency among medical students tends to decline as they progress through their academic programs [42]. This decline contrasts with the current model of patient-centered communication, as patients desire better communication with their physicians [42]. Patients prefer to receive serious news in person and with the physician’s undivided attention, but they also want to have faith in the physician’s competence [2, 43]. A good physician-patient relationship has the potential to help with emotional adjustment and increase patient satisfaction and compliance [42]. In recent years, universities and other institutions have made significant efforts in the form of courses, forums, and available printed materials to help physicians improve their abilities and knowledge in this challenging area [44].
There are some limitations to this study. First, the data were obtained through a self-reporting cross-sectional study, which may not have accurately represented the residents’ clinical performance. Second, the study was limited to residents practicing in two general hospitals. However, residents from different disciplines participated in this study. Finally, this study did not assess whether the specific guidelines affected patients’ satisfaction or outcomes. Despite these limitations, this study had numerous strengths; residents of different disciplines in three general groups of medical, surgical, and emergency medicine participated in this study, so this study can provide a better and broader description of the conditions of BBN in different departments of the hospital. Also, the results indicated that along with theoretical and practical training, it is better to review the current training programs and monitor the implementation of protocols and guidelines more carefully. In addition, this study reported barriers to BBN that were under-reported in previous research that should be addressed. Additional research is needed in the areas of objective assessments by patients or doctors of how physicians deliver bad news, whether published guidelines on delivering bad news accurately reflect patients’ expressed needs and preferences, and whether delivering bad news in accordance with current guidelines affects patient satisfaction and clinical outcomes.
Conclusions
Despite the importance of BBN in medicine, the obtained results revealed that about one-third of residents treating patients have never received any training on BBN and the skill of residents in BBN is not enough in some aspects, even among trained residents. Residents perceived the difficulty of BBN in some aspects and their incompetence in this field. They identified barriers to BBN that may be alleviated using several strategies such as the incorporation of BBN training and communication skill training courses in the educational curricula of residency. Also, physical modification of hospital departments to provide a suitable environment for BBN is important.
Data Availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Buckman R. How to break bad news: a guide for health care professionals. University of Toronto Press; 1992.
Berkey FJ, Wiedemer JP, Vithalani ND. Delivering bad or life-altering news. Am Family Phys. 2018;98(2):99–104.
Wolfe AD, Frierdich SA, Wish J, Kilgore-Carlin J, Plotkin JA, Hoover-Regan M. Sharing life-altering information: development of pediatric hospital guidelines and team training. J Palliat Med. 2014;17(9):1011–8.
Back AL, Trinidad SB, Hopley EK, Arnold RM, Baile WF, Edwards KA. What patients value when oncologists give news of cancer recurrence: commentary on specific moments in audio-recorded conversations. Oncologist. 2011;16(3):342–50.
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oxford University Press; 2000. pp. 302–11.
Lind SE, DelVecchio Good M, Seidel S, Csordas T, Good BJ. Telling the diagnosis of cancer. J Clin Oncol. 1989;7(5):583–9.
Fujimori M, Uchitomi Y. Preferences of cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol. 2009;39(4):201–16.
Parker PA, Baile WF, de Moor C, Lenzi R, Kudelka AP, Cohen L. Breaking bad news about cancer: patients’ preferences for communication. J Clin Oncol. 2001;19(7):2049–56.
Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. Ethnicity and attitudes toward patient autonomy. JAMA. 1995;274(10):820–5.
Seifart C, Hofmann M, Bär T, Knorrenschild JR, Seifart U, Rief W. Breaking bad news–what patients want and what they get: evaluating the SPIKES protocol in Germany. Ann Oncol. 2014;25(3):707–11.
Ahmady AE, Sabounchi SS, Mirmohammadsadeghi H, Rezaei A. A suitable model for breaking bad news: review of recommendations. JMED Res. 2014;2014:1–15.
Hafidz MA, Zainudin LD. Breaking Bad News: an essential skill for doctors. Med J Malaysia. 2016;71(1):26–7.
Supe A. Interns’ perspectives about communicating bad news to patients: a qualitative study. Educ Health. 2011;24(3):541.
Tulsky JA, Fischer GS, Rose MR, Arnold RM. Opening the black box: how do physicians communicate about advance directives? Ann Intern Med. 1998;129(6):441–9.
Farokhyar N, Shirazi M, Bahador H, Jahanshir A. Assessing the validity and reliability of spikes questionnaires regard in of medical residents awareness breaking bad news in TUMS 2012. Razi J Med Sci. 2014;21(122):29–36.
Mostafavian Z, Shaye ZA. Evaluation of physicians’ skills in breaking bad news to cancer patients. J Family Med Prim care. 2018;7(3):601.
Lacasse Y, Godbout C, Series F. Health-related quality of life in obstructive sleep apnoea. Eur Respir J. 2002;19(3):499–503.
Rodrigues IB, Adachi JD, Beattie KA, MacDermid JC. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskelet Disord. 2017;18(1):1–9.
Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–75.
Annas GJ. Informed consent, cancer, and truth in prognosis. N Engl J Med. 1994;330(3):223–5.
Rosenbaum ME, Ferguson KJ, Lobas JG. Teaching medical students and residents skills for delivering bad news: a review of strategies. Acad Med. 2004;79(2):107–17.
Fuerst NM, Watson JS, Langelier NA, Atkinson RE, Ying G-S, Pan W, et al. Breaking bad: an Assessment of Ophthalmologists’ interpersonal skills and training on delivering Bad News. J Acad Ophthalmol. 2018;10(01):e83–e91.
Brouwers MH, Bor H, Laan R, van Weel C, van Weel-Baumgarten E. Students’ experiences with a longitudinal skills training program on breaking bad news: a follow-up study. Patient Educ Couns. 2018;101(9):1639–44.
Brouwers M, van Weel C, Laan R, van Weel-Baumgarten E. Training undergraduates skills in breaking bad news: how students value educators’ feedback. J Cancer Educ. 2019;34:1103–6.
Arbabi M, Roozdar A, Taher M, Shirzad S, Arjmand M, Mohammadi MR, et al. How to break bad news: physicians’ and nurses’ attitudes. Iran J Psychiatry. 2010;5(4):128.
Biazar G, Delpasand K, Farzi F, Sedighinejad A, Mirmansouri A, Atrkarroushan Z. Breaking bad news: a valid concern among clinicians. Iran J Psychiatry. 2019;14(3):198.
GHAFARI NA, Salari P. MIRZAZADEH A. Study on breaking bad news to patients among physicians of kerman university of medical sciences. 2006.
Alshami A, Douedi S, Avila-Ariyoshi A, Alazzawi M, Patel S, Einav S, et al. editors. Breaking bad news, a pertinent yet still an overlooked skill: an international survey study. Healthcare: MDPI; 2020.
Locatelli C, Piselli P, Cicerchia M, Repetto L. Physicians’ age and sex influence breaking bad news to elderly cancer patients. Beliefs and practices of 50 italian oncologists: the GIO Ger study. Psycho-oncology. 2013;22(5):1112–9.
Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff. 2010;29(7):1310–8.
Schmitz FM, Schnabel KP, Bauer D, Woermann U, Guttormsen S. Learning how to break bad news from worked examples: does the presentation format matter when hints are embedded? Results from randomised and blinded field trials. Patient Educ Couns. 2020;103(9):1850–5.
Pieters HC, Green E, Sleven M. It just hit me like a Ton of Bricks: improving the patient experience of receiving a breast Cancer diagnosis at an older age. Res Gerontol Nurs. 2021;14(2):79–89.
Brouwer MA, Maeckelberghe EL, van der Heide A, Hein IM, Verhagen EA. Breaking bad news: what parents would like you to know. Arch Dis Child. 2021;106(3):276–81.
Dosanjh S, Barnes J, Bhandari M. Barriers to breaking bad news among medical and surgical residents. Med Educ. 2001;35(3):197–205.
Costantini A, Baile WF, Lenzi R, Costantini M, Ziparo V, Marchetti P, et al. Overcoming cultural barriers to giving bad news: feasibility of training to promote truth-telling to cancer patients. J Cancer Educ. 2009;24(3):180.
Aljubran AH. The attitude towards disclosure of bad news to cancer patients in Saudi Arabia. Ann Saudi Med. 2010;30(2):141–4.
Ferreira da Silveira FJ, Botelho CC, Valadão CC. Breaking bad news: doctors’ skills in communicating with patients. Sao Paulo Med J. 2017;135:323–31.
Dafallah MA, Ragab EA, Salih MH, Osman WN, Mohammed RO, Osman M, et al. Breaking bad news: awareness and practice among sudanese doctors. AIMS Public Health. 2020;7(4):758.
Alnefaie S, Filfilan NN, Altalhi EA, Al Juaid RS, Aljuaid ND, Abdulrahman R. Evaluation of surgeons’ skills in breaking bad news to cancer patients based on the SPIKES protocol in multiple medical centers at Taif city, Saudi Arabia: a cross-sectional study. Int J Med Developing Ctries. 2021;5(1):51–49.
Lee HR, Yi SY. Delivering bad news to a patient: a survey of residents and fellows on attitude and awareness. Korean J Med Educ. 2013;25(4):317.
Pun J. A study of chinese medical students’ communication pattern in delivering bad news: an ethnographic discourse analysis approach. BMC Med Educ. 2021;21(1):286.
Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38–43.
Chiu L-Q, Lee W-SD, Gao F, Parker PA, Ng G-Y, Toh C-K. Cancer patients’ preferences for communication of unfavourable news: an asian perspective. Support Care Cancer. 2006;14:818–24.
Konstantis A, Exiara T. Breaking bad news in cancer patients. Indian J Palliat Care. 2015;21(1):35.
Acknowledgements
We appreciate the assistants of residents of Iran University of Medical Sciences who participated in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
R.S and M.Z and A.G contributed to the conception and design of the study. M.M, M.Z and A.M performed data collection. Analysis was performed by A.M. R.S, M.M and M.Z drafted the manuscript and all authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study protocol was approved by the Research Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.FMD.REC.1400.419). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mansoursamaei, M., Ghanbari Jolfaei, A., Zandi, M. et al. Self-assessment of residents in breaking bad news; skills and barriers. BMC Med Educ 23, 740 (2023). https://doi.org/10.1186/s12909-023-04720-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04720-4