Abstract
Introduction
This study investigated medical students’ intended learning outcomes based on e-learning and in-person education.
Methods
In this cross-sectional comparative analytical study, a group of 126 undergraduate medical students’ intended learning outcomes under two different teaching methods, including e-learning and in-person, were repeatedly measured based on the census sampling method. Participants were in the preclinical curriculum phase (physiopathology) at Mashhad University of Medical Sciences (MUMS), Iran. Due to expert panel opinion, the same medical teachers and similar difficulty of lessons were considered in two investigated academic semesters. In addition, difficulty and discrimination indexes of formative and summative assessments were controlled for two study groups. The students’ learning outcome index was the knowledge test scores participants received in the relevant lessons of the General Medicine (GM) curriculum preclinical courses.
Results
The findings indicated that students learning outcomes were significantly higher during e-learning than in in-person education for all examined variables (P < 0.05). Moreover, the difference between students’ Grade Point Average (GPA) categories among the two groups was significant (P = 0.022). Students with a GPA of less than 14 experienced higher increments in their average scores after the e-learning compared to in-person education. Compared to face-to-face courses, improvements in pharmacology, theoretical semiology, and pathology scores after e-learning courses were statistically significant (P < 0.001). The differences in mean scores related to practical pathology and semiology in the two approaches were not statistically significant, P = 0.624 and P = 0.149, respectively. Furthermore, the overall students’ average scores increased significantly during e-learning versus in-person education (P < 0.001).
Conclusion
We concluded that e-learning could be appreciated as a successful method of medical education and can be used as an alternative educational method. However, considering the importance of practical or clinical courses in medical education, further research about the efficacy of the e-learning approach is highly recommended.
Similar content being viewed by others
Introduction
The pandemic of COVID-19 infection has interrupted the educational programs in different universities, especially in medical schools all over the world [1]. Most medical schools were suspended from their regular face-to-face courses to ensure the safety of their students and faculties. After that, e-learning was added as one of the core teaching methods throughout the COVID-19 pandemic [2, 3]. This technology refers to the web-based software for distributing, tracking, and managing curriculum-based internet programs between students and faculty [4]. E-learning might be included structures like whiteboards, chat rooms, polls, quizzes, discussion forums, and surveys to be allowed the lecturers and students to communicate online and share course content side by side [5]. E-learning provides facilities for many training aspirations, including independent learning, self-directed learning, special time-independent learning, collaborative training, and real-time feedback [6]. Therefore, students increasingly use e-learning as a complementary educational method. Different e-learning methods are available for medical education, such as online learning platforms, e-books (electronic versions of standard textbooks), e-journals, online question banks, medical websites, and mobile phone apps [7]. Students declared that substituting electronic books and online articles during teaching could increase the active attitude toward learning [8, 9]. However, the success of the e-learning teaching method is influenced by many variables, consisting of access to suitable practice, the course content, and demographic criteria for students. In addition, advantages having improved convenience, more accessible resources irrespective of the location and time, and reduced costs must be deliberated [10,11,12,13,14]. Although conventional learning methods such as the in-person approach have been approved for many years, e-learning courses have been recognized as efficient learning modalities in different educational and governmental studies [8, 15]. In low- and middle-income countries (LMICs), e-learning for medical education may alleviate the burden of severe health worker shortages and deliver affordable access to high-quality medical education [16]. Concurrent with stressing recent advancements in educational technology, researchers believe that the learning environment is one of the causes of satisfying the learners’ diverse requirements. So, the growing demand for the extension service for e-courses has created issues that need comprehensive consideration [17].
Consequently, investigating students’ learning in different teaching methods seems necessary. For many years, it was believed that face-to-face training has a more significant impact on students’ performance than e-learning and distance methods. Until the COVID-19 pandemic, the virtual learning environment was mainly used as a teaching aid. Therefore, pursuing this particular learning method’s effectiveness in the students’ learning outcomes was impossible. During the coronavirus pandemic, due to the complete mandatory shift from face-to-face education to e-learning, it was an opportunity to evaluate students’ performance in virtual learning environments. This study aims to compare the students’ learning outcomes between in-person and e-learning methods.
Methods
In this analytical cross-sectional study, a group of 126 undergraduate medical students’ intended learning outcomes under two different teaching methods, including e-learning and in-person, were repeatedly measured based on the census sampling method. Participants were in the preclinical curriculum phase (physiopathology) of the GM (General Medicine) at MUMS (Mashhad University of Medical Sciences), Iran. The same set of students was considered for both teaching modalities. The students’ learning outcomes were assessed due to the knowledge test scores they received in the relevant lessons of the GM curriculum preclinical courses from September 2020 to August 2021. The background characteristics were mainly students’ gender, age, residency status (native and non-native), type of university admission (free tuition, paying tuition, and international students), and GPA. To ensure the similarity and difficulty of lessons, the same courses in two consecutive semesters were evaluated. These courses, including pharmacology, pathology, and semiology, were taught in two successive semesters due to the large volume of educational materials in the GM curriculum. Students attended regular face-to-face classes for mentioned courses which consisted of pharmacology I, theoretical and practical pathology I, and theoretical and practical semiology I from September 2020 to February 2021. In the in-person training, the educators taught lessons using lectures and interactive presentations; at this point, questioning was allowed. After that, the students who successfully passed these courses entered the new semester and were educated on the intended courses under the e-learning approach and attended pharmacology II, theoretical and practical pathology II, and theoretical and practical semiology II from February 2021 to August 2021. Participants who failed in face-to-face training courses were excluded from further analysis.
Methods of providing e-content for e-learning, modes of interaction, and many other factors in online learning are classified into synchronous and asynchronous. Synchronous e-learning is live, real-time, facilitating instruction and learning-oriented interaction [17]. Asynchronous online learning is a time-delayed interaction that the communication of both instruction and learning is not occurring simultaneously [18]. The e-learning content was delivered to students in several interactive multimedia formats (slide-based lectures, standalone training videos, embedded videos, webinar or live training playback, podcasts, dialogue simulations, animations, and interactive videos) with formative and summative assessment modules at the end of each Learning Object (LO). The LOs were designed and created in collaboration with instructional designers and electronic content developers under the supervision of an expert panel, including relevant faculty members. During the e-learning, students received the courses via the Learning Management System of MUMS (NAVID®, https://mumsnavid.vums.ac.ir) for asynchronous online learning and Adobe Connect and Skyroom for synchronous e-learning. All theoretical and practical courses assessed in this study were delivered to students similarly based on the curriculum.
All methods were carried out following relevant guidelines and regulations. The study protocol was aligned with the ethics committee (the approval date was 2020-08-18 with IR.MUMS.MEDICAL.REC.1399.298 reference code). All registered students voluntarily agreed to participate in the study. Informed consent was obtained from all subjects. Also, to maintain confidentiality, all data were analyzed anonymously and based on an identification code.
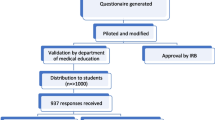
The data collection tools for students’ intended learning outcomes were knowledge tests in both groups. The test questions were designed and developed based on the content of the courses taught and consisted of 20 Multiple Choice Questions (MCQ) with one correct option out of four for each lesson. The maximum score of the tests was 20 points, and there were no partial or subtracted points. Due to the expert panel’s opinion, the same medical teachers and lessons that were similar in difficulty were considered in two investigated academic semesters. However, these courses were the prerequisite to each other and were related vertically during the educational curriculum. Nine medical faculty members approved the validity and reliability of the questions for both semesters, and Cronbach’s alpha was in the range of 0.79 to 0.86. Difficulty and discrimination indexes of formative and summative assessments were controlled for two study groups. In our university, the electronic examination system has the possibility of various reports, including the difficulty and discrimination indexes of questions. Therefore, the system report was used to check the questions extracted from the question bank (https://qsanjesh.mums.ac.ir), and the questions in both groups were homogeneous in terms of the mentioned criteria. The steps of the current study are demonstrated in Fig. 1.
In this study, the students of the in-person education participated in the onsite proctored exams. Yet, for individuals who attended the e-learning, due to the limits of COVID-19, we had to hold the formative and summative assessments online in the MUMS central examination system (https://esanjesh.mums.ac.ir). This evaluation method has some challenges, including the necessity of matching with technology, infrastructural barriers, especially in our country as a developing one, and the probability of cheating in online exams. To ensure the privacy of the online tests, we attempted to detect cheating during the exam by verifying the student’s identity through continuous authentication. For added security, the exam-taker was required to answer a short series of security questions based on background student information extracted from the MUMS educational system. In addition, we supervised remote exam-takers by watching live online videos to identify suspicious examinee behaviors or items in their immediate environments, such as repeatedly glancing away from the screen. Since the effect of cheating in online exams was an important confounder in this study, we applied other ways to reduce it, including randomizing examination questions and supplemental oral tests using online video calls.
Then the students’ knowledge test scores in the lessons of courses mentioned above (pharmacology, pathology, and semiology) were collected. The participants’ background information was extracted from the university educational system to compare their intended learning outcomes in e-learning and in-person learning environments. We analyzed data under the statistical package for the social sciences version by SPSS (SPSS Inc., version 20, Chicago, Illinois, USA). The variables with a continuous normal distribution were defined in the text by the Mean ± Standard Deviation. Also, the qualitative variables were determined by frequency and percentages in their related groups. The Shapiro-Wilk test was used to define the distribution of variables. The comparisons between two study groups with normal distribution have been performed under Student’s T-Test independent samples. Analysis of Variance by ANOVA Test was committed to comparing the difference between two groups’ quantitative categorical variables. Furthermore, paired T-Test was performed to analyze the difference between e-learning and in-person intended learning outcomes. A P-value less than 0.05 was considered statistically significant.
Results
In this cross-sectional study, 126 undergraduate medical students participated. The participants’ background characteristics showed that most students were male (52%) and were admitted for free tuition (83%). Related features showed that most participants had a GPA between 14 and 17 (65%). Furthermore, most of the students were non-native (53%) in our study and had less than 24 years old (78%) (Table 1).
The Comparison of e-learning and in-person methods in medical students’ learning outcomes based on background characteristics is presented in Table 2. The findings indicated that students learning outcomes were significantly higher during e-learning than in in-person education for all examined variables (P < 0.05). The relation between teaching method and students’ gender was insignificant (P = 0.205) as male and female students had approximately an equal increment of average scores during e-learning compared to in-person education. There wasn’t any statistically significant difference between students’ types of admission (P = 0.533) and their residency status (P = 0.085) with intended learning outcomes. The students with different age categories had similar average scores in both teaching methods (P = 0.546). Moreover, the difference between students’ GPA categories among the two groups was significant (P = 0.022). Students with a GPA of less than 14 experienced higher increments in their average scores after the e-learning compared to in-person education.
-
Tukey’s honestly significant difference (HSD) post hoc test showed statistically significant diffrences between every two groups based on grade point average.
The Comparison of e-learning and in-person methods in participants’ performance based on different lessons of preclinical medical education is presented in Table 3. Compared to face-to-face courses, improvements in pharmacology, theoretical semiology, and pathology scores after e-learning courses were statistically significant (P < 0.001). The differences in mean scores related to practical pathology and semiology in the two approaches were not statistically significant, P = 0.624 and P = 0.149, respectively. Furthermore, the overall students’ average scores increased significantly during e-learning versus in-person education (P < 0.001).
Discussion
In this study, we compared the intended learning outcomes of undergraduate medical students based on e-learning and in-person methods during the COVID-19 pandemic. It was revealed better learning outcomes based on students’ knowledge test scores attributed to e-learning versus face-to-face education. Besides, some significant differences were found in the two mentioned methods due to background characteristics, including students’ gender, age, residency status, type of admission, and GPA. Previous research showed that simple access to learning subjects and the ability to select the place and the study time is considered the main benefit of e-learning compared to in-person education [19], which was too important during the COVID-19 pandemic. The role of e-learning in reducing accommodation and transportation expenses is a significant factor [20, 21]. The studies emphasize that e-learning enables educational subjects to be delivered to students fast, effectively, updated, and standardized [19, 22]. However, it is too difficult for the students as well as the teachers to conduct/attend classes online, due to which a lot of problems are being faced by both students as well as teachers like student assessment, proper class attendance, internet connectivity issue, and vice versa [23].
In this study, increasing the average scores of medical students indicated that e-learning enables them to improve their knowledge more than in-person education. So, the present study demonstrated that e-learning is an appreciated teaching method for medical students. Schrader (2015) showed that e-learning is 6% more effective than in-person training in providing knowledge. However, students’ learning was reported to be identical both ways, and students were satisfied with both methods [24]. Pallavi et al. (2022) declared that more than 50% of the respondents feel online learning is as effective as conventional classroom learning [25]. In an e-learning environment that emphasizes learner-centered activity and system interactivity, remote learners can outperform traditional classroom students [26]. However, Jiang et al. (2023) obtained that the e-learning behavior of undergraduate students needs to be improved [27]. Previous research supported that enhancing students’ knowledge of e-learning might increase secondary outcomes such as their self-discipline degree [28].
Further, the authors found the differences in mean scores related to practical pathology and semiology in the two approaches were not statistically significant. We considered it more challenging to understand practical courses than theoretical ones in the e-learning method versus in-person education. Since e-learning was less effective in increasing medical students’ achievement for practical semiology and pathology, concentrating on improving the average scores of practical courses besides theoretical lessons is critical. Garland (2010) explored e-learning versus classroom instruction in a Dental Hygiene Program. Findings demonstrated little difference between the two methods [29]. Several studies might support this finding, revealing that indirect e-learning could delay conventional direct learning in many aspects [30]. In this regard, this was similar to recently published investigations that assessed students’ understanding of online classes during the pandemic of COVID-19 [31,32,33]. This point might be due to the lack of interaction between lecturers and students in e-learning compared to face-to-face education, specifically for practical courses. A previous study considered this point as one of the disadvantages of e-learning compared to a face-to-face learning environment [19]. However, E-learning activities can turn rather dull online experiences into entertaining, interactive, meaningful, and valuable learning experiences for students [34]. Interactive learning environments respond dynamically to learners’ actions and are associated with active, learner-engaged processing of learning materials. Such settings are expected to promote deep cognitive processes and actively construct new knowledge [35]. Previous investigations declared that weak interaction between students and organizers and the lack of transparency regarding the learning goal could prevent the e-learning method’s education process compared to the face-to-face way [36, 37]. Bock et al. (2021) performed a randomized study to compare the effectiveness of face-to-face, blended, and e-learning teaching in local anaesthesia by assessing students’ knowledge gain and performance of practical skills. Their study indicated that blended learning improves the learning outcome for theoretical knowledge in teaching local anaesthesia more than either face-to-face learning or e-learning alone. For acquiring practical skills, their study showed that blended learning was as effective as other teaching methods [38]. Barteit et al. (2020) systematically reviewed e-learning interventions for medical education in low- and middle-income countries (LMICs). According to their findings, most studies self-concluded that they had an effective e-learning intervention, thus indicating the potential benefits of e-learning for LMICs [16]. Further, studies have shown that e-learning modalities are used widely by students outside of their formal curricula and by health professionals for continuing professional education, indicating that students and professionals appreciate and take advantage of e-learning [38]. Individual learners take advantage of self-paced learning environments in which they control their learning pace, information flow, selection of learning activities, and time management [17]. Finally, Frehywot et al. (2013) said, “E-learning in medical education is a means to an end, rather than the end in itself.“ It seems utilizing e-learning can result in more significant educational opportunities for students while enhancing faculty effectiveness and efficiency. [39].
Limitations of the study
The study has some limitations. Student assessment is one of the most challenging aspects of virtual education since academic integrity could be contravened due to various cheating behaviors in online examinations [40]. Although we tried cheating detection before and during the exams, this was one of the critical limitations of our study because cheating methodologies, types, and facilitators are widespread. Another limitation is that only short-term retention was assessed in our study. The assessment of students’ retention would be essential to determine future studies. Furthermore, studies on the existing literature, evidence, and a variety of e-learning examples could move beyond the determination of an appropriate blend of different instructional strategies, including e-learning, face-to-face/in-person instruction, and performance-based skill practices.
Conclusion
The present study’s findings could declare that e-learning alone might not have the necessary efficiency in practical and clinical medical education and should be applied alongside the in-person method as a complementary learning opportunity. Consequently, although e-learning may represent an optimal solution to maintain learning processes in exceptional emergencies such as the COVID-19 pandemic, in-person education is more effective for acquiring practical skills than other virtual learning environments.
Data Availability
All tables and the study results were provided based on the study’s raw data, which is available from the corresponding author. She will send the SPSS file upon your request.
References
Howlett D, Vincent T, Gainsborough N, Fairclough J, Taylor N, Cohen J et al. Integration of a case-based online module into an undergraduate curriculum: what is involved and is it effective? E-learning and digital media. 2009;6(4):372–84.
Blissitt AM. Blended learning versus traditional lecture in introductory nursing pathophysiology courses. J Nurs Educ. 2016;55(4):227–30.
Sadeghi R, Sedaghat MM, Ahmadi FS. Comparison of the effect of lecture and blended teaching methods on students’ learning and satisfaction. J Adv Med Educ professionalism. 2014;2(4):146.
Keis O, Grab C, Schneider A, Öchsner W. Online or face-to-face instruction? A qualitative study on the electrocardiogram course at the University of Ulm to examine why students choose a particular format. BMC Med Educ. 2017;17(1):1–8.
Thanji M, Vasantha S. ICT factors influencing consumer adoption of ecommerce offerings for education. Indian J Sci Tech. 2016;9(32):1–6.
Farokhi MR, Zarifsanaiey N, Haghighi FS, Mehrabi M, editors., editors. E-LEARNING OR IN-PERSON APPROACHES IN CONTINUOUS MEDICAL EDUCATION: A COMPARATIVE STUDY2016.
Samarasekar K. e-Learning in Medical Education in Sri Lanka: Survey of Medical Undergraduates and New Graduates. JMIR Med Educ. 2022;8(1):e22096.
Letterie GS. Medical education as a science: the quality of evidence for computer-assisted instruction. Am J Obstet Gynecol. 2003;188(3):849–53.
Aikawa L, Zornoff DCM, Matsubara BB. Guide of internet sites for the study of cardiology. Arquivos brasileiros de cardiologia. 2004;83:396–9.
Cook DA, Triola MM. What is the role of e-learning? Looking past the hype. Med Educ. 2014;48(9):930–7.
Salem AH. Randomized controlled trial of simulation-based teaching versus traditional clinical instructions in nursing: a pilot study among critical care nursing students. Int J Nurs Educ. 2015;7(1):277.
Attardi SM, Rogers KA. Design and implementation of an online systemic human anatomy course with laboratory. Anat Sci Educ. 2015;8(1):53–62.
Niebuhr V, Niebuhr B, Trumble J, Urbani MJ. Online faculty development for creating E-learning materials. Educ health. 2014;27(3):255.
Bediang G, Stoll B, Geissbuhler A, Klohn AM, Stuckelberger A, Nko’o S, et al. Computer literacy and E-learning perception in Cameroon: the case of Yaounde Faculty of Medicine and Biomedical Sciences. BMC Med Educ. 2013;13(1):1–8.
Rotimi O, Orah N, Shaaban A, Daramola AO, Abdulkareem FB. Remote teaching of histopathology using scanned slides via Skype between the United Kingdom and Nigeria. Arch Pathol Lab Med. 2017;141(2):298–300.
Barteit S, Guzek D, Jahn A, Bärnighausen T, Jorge MM, Neuhann F. Evaluation of e-learning for medical education in low- and middle-income countries: a systematic review. Comput Educ. 2020;145:103726.
Shahabadi MM, Uplane M. Synchronous and asynchronous e-learning Styles and academic performance of e-learners. Procedia - Social and Behavioral Sciences. 2015;176:129–38.
Zhang R, Bi NC, Mercado T. Do zoom meetings really help? A comparative analysis of synchronous and asynchronous online learning during Covid-19 pandemic.Journal of computer assisted learning. 2022.
Bączek M, Zagańczyk-Bączek M, Szpringer M, Jaroszyński A, Wożakowska-Kapłon B. Students’ perception of online learning during the COVID-19 pandemic: a survey study of Polish medical students.Medicine. 2021;100(7).
Stain SC, Mitchell M, Belue R, Mosley V, Wherry S, Adams CZ et al. Objective assessment of videoconferenced lectures in a surgical clerkship. The American Journal of Surgery. 2005;189(1):81 – 4.
Amesse LS, Callendar E, Pfaff-Amesse T, Duke J, Herbert WN. Evaluation of computer-aided strategies for teaching medical students prenatal ultrasound diagnostic skills. Med Educ Online. 2008;13(1):4482.
Zehry K, Halder N, Theodosiou L. E-Learning in medical education in the United Kingdom. Procedia-Social and Behavioral Sciences. 2011;15:3163–7.
Raju RS, Roy M, editors, editors. An Overview of the Framework for Development of E-Classroom Toward E-Learning. Advanced Computational Paradigms and Hybrid Intelligent Computing; 2022 2022//; Singapore:Springer Singapore.
Schrader TC. In: Chattanooga (Tenn.), editor. Is the classroom better? An introspective look at e-learning and classroom from a GED standpoint [Masters theses]. University of Tennessee at Chattanooga; 2015.
Pallavi D, Ramachandran M, Chinnasamy S. An empirical study on effectiveness of E-Learning over Conventional Class Room Learning–A Case Study with respect to Online Degree Programmes in Higher Education. Recent trends in Management and Commerce. 2022;3(1):25–33.
Zhang D, Zhao JL, Zhou L, Nunamaker JF Jr. Can e-learning replace classroom learning? Commun ACM. 2004;47(5):75–9.
Jiang X, Zhang H, Wang T, Zhang C. The association of self-control, self-efficacy, and demographic characteristics with home-based E-learning behavior in nursing and midwifery undergraduates: a cross-sectional study under the COVID-19 epidemic. Nurse Educ Today. 2023;120:105628.
Stacey E, Gerbic P. Success factors for blended learning. Hello; 2008. p. 964-8.
Garland KV. E-learning vs. classroom instruction in infection control in a dental hygiene program. J Dent Educ. 2010;74(6):637–43.
Peine A, Kabino K, Spreckelsen C. Self-directed learning can outperform direct instruction in the course of a modern german medical curriculum-results of a mixed methods trial. BMC Med Educ. 2016;16(1):1–11.
Thomas A, Shenoy MT, Shenoy KT, Kumar SS, Sidheeque A, Khovidh C, et al. Survey among medical students during COVID-19 lockdown: the online class dilemma. Int J Med Students. 2020;8(2):102–6.
Minh DNT, Huy TP, Hoang DN, Thieu MQ. COVID-19: experience from Vietnam Medical Students. Int J Med Students. 2020;8(1):62–3.
Qarajeh R, Tahboub F, Rafie N, Pirani N, Jackson MA, Cochran CD. The effect of COVID-19 pandemic on US medical students in their clinical years. Int J Med Students. 2020;8(2):172–4.
Watkins BR. Developing interactive e-learning activities. Perform Improv. 2005;44(5):5–7.
Kalyuga S. Enhancing instructional efficiency of interactive e-learning environments: a cognitive load perspective. Educational Psychol Rev. 2007;19(3):387–99.
Docherty A, Sandhu H. Student-perceived barriers and facilitators to e-learning in continuing professional development in primary care. Educ Prim Care. 2006;17(4):343–53.
Gagnon M-P, L_gar_ F, Labrecque M, Fr_mont P, Cauchon M, Desmartis M. Perceived barriers to completing an e-learning program on evidence-based medicine. J Innov Health Inf. 2007;15(2):83–91.
Bock A, Kniha K, Goloborodko E, Lemos M, Rittich AB, Möhlhenrich SC, et al. Effectiveness of face-to-face, blended and e-learning in teaching the application of local anaesthesia: a randomised study. BMC Med Educ. 2021;21(1):137.
Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, et al. E-learning in medical education in resource constrained low- and middle-income countries. Hum Resour Health. 2013;11(1):4.
Noorbehbahani F, Mohammadi A, Aminazadeh M. A systematic review of research on cheating in online exams from 2010 to 2021. Educ Inform Technol. 2022;27(6):8413–60.
Acknowledgements
The authors appreciate Mashhad University of Medical Sciences, Mashhad, Iran, for their financial support of this study (Grant Number 990571). We also thank the IT management personnel of our university for providing related facilities during the research. Last but not least, the authors would like to thank the reviewers for their valuable comments and suggestions on an earlier version of this Article.
Funding
Mashhad University of Medical Sciences supported and funded this project.
Author information
Authors and Affiliations
Contributions
HM participated in the conception and design of the study, coordinated the study, collected data, participated in the data analysis and interpretation of data, and wrote the manuscript. AE participated in data collection, conducted the data analysis, assisted with interpreting the data, and commented on the manuscript. SN was responsible for data analysis, interpretation of data, and manuscript drafting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out following relevant guidelines and regulations. The study protocol was aligned with the ethics committee (the approval date was 2020-08-18 with IR.MUMS.MEDICAL.REC.1399.298 reference code). Informed consent was obtained from all subjects or their legal guardians.
Consent for publication
Not applicable.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mastour, H., Emadzadeh, A., Hamidi Haji Abadi, O. et al. Are students performing the same in E-learning and In-person education? An introspective look at learning environments from an Iranian medical school standpoint. BMC Med Educ 23, 209 (2023). https://doi.org/10.1186/s12909-023-04159-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04159-7