Abstract
Background
Telementoring seems to be a promising strategy to deliver training and counselling to physicians in remote areas. In Peru, early graduated physicians must work for the Rural and Urban-Edge Health Service Program where they face important training needs. The aim of this study was to describe the usage of a one-on-one telementoring program for rural physicians and evaluate the aspects related to the perceptions of acceptability and usability.
Methods
Mixed methods study on recently graduated physicians who work in rural areas and participate in the telementoring program. The program used a mobile application to connect these young doctors with specialized mentors to answer queries about real-life problems raised by working in a rural area. We summarize administrative data to assess participant characteristics and their participation in the program. Additionally, we conducted in-depth interviews to explore the perceived usability, ease of use, and reason for non-use of the telementoring program.
Results
Of 74 physicians (mean age 25, 51.4% women) enrolled, 12 (16.2%) actively used the program and performed a total of 27 queries, which received response in an average time of 5.4 ± 6.3 h. In the interviews, the main reasons for non-use were connectivity issues, feelings of shame, and self-efficacy. For those who used the telementoring program they referred it was easy to use and solve their inquiries timely.
Conclusions
The implementation of a telementoring program sought to provide guidance to recently graduated physicians working in rural areas. Low use rates show that administrative and process-related deficiencies in the program implementation need to be improved.
Similar content being viewed by others
Background
Educational interventions for health professionals have been continuously improved with the use of Information and Communication Technologies (ICT) since they facilitate the exchange of information and interaction between educators and their students [1]. However, the implementation of this interventions in rural and remote geographical areas continues to be a challenge, not only due to technical aspects such as connectivity, but also due to perception and usability problems by the health personnel who work there.
One type of these interventions in rural areas is called telementoring, which consists of continuously providing, using ICT, practical and theoretical content from more experienced professionals (mentors) to other professionals with little experience (mentees), focusing on topics of interest depending on the context where the participants are [2]. Although to date it has been shown that it could effectively improve the knowledge, skills and attitudes of health personnel [3, 4], most telementoring experiences follows the ECHO model, so they are usually focused on group sessions [5] and may not have the same applicability for all users. Especially for those groups whose individual needs are very different from each other, the acceptability and usability of the program could be different and a more personalized type of telementoring could be necessary. Therefore, one-on-one telementoring initiatives (the interaction between one mentor and one mentee) have been developed that have shown promising results in capacity building for health human resources, mostly related to medical procediments and surgery topics [6, 7].
In Peru, there is the Rural and Urban-Edge Health Service (SERUMS, in Spanish), where newly graduated physicians (SERUMS physicians) work for a year in primary health care facilities in different rural areas [8]. This service is mandatory since it is a requirement to opt for the second specialty or to work in public health centers. More importantly, it has been seen that these SERUMS physicians face great challenges due to various factors such as lack of experience, training background directed to hospital settings rather than primary-care, not interacting with colleagues, holding new administrative positions, among others [9,10,11].
The gap in knowledge and expertise that physicians present during the SERUMS is significant, likewise, the training needs would be different according to each case since they could differ, for example, according to their level of previous experience, the health needs of their community, the number of resources that have in their establishment, and the number of responsibilities that they will assume (administrative, clinical, legal, etc.). In this context, the National University of San Marcos (UNMSM, in Spanish) created a one-on-one telementoring program to provide SERUMS physicians with guidance and personalized educational advice during their year of work in remote areas. To carry out this program, a mobile application called JOIN© was used, which is a medical mobile application approved by the FDA to improve communication between health professionals, allowing the delivery of encrypted information, images, among other functionalities such as multi-device support, instant messaging, and video calling.
Since the introduction of new technologies to provide distance education implies a continuous interaction of users with new platforms and applications, these must be evaluated in practice from the perspective of the user (e.g. acceptability and usability) [12, 13]. Then, considering that this program is a first experience of one-on-one telementoring intervention in rural areas of Peru, our objective is to describe the use of the intervention and evaluate the aspects related to the perceptions of acceptability and its usability.
Methods
Study design and context
We conducted a mixed-methods study using a sequential explanatory design, which is a recommended approach that sequentially integrates quantitative and qualitative data for evaluating telehealth interventions [14]. First, we analyzed quantitative data from the administrative database of the 2018 cohort of the “UNMSM telementoring program” to describe users characteristics and mobile application usage. Then, from 2019 July to 2019 August, we performed interviews to gather qualitative information regarding usability and perceptions of the program from those physicians who were part of the 2018 cohort.
Population and sampling
In March 2018, two months prior to SERUMS beginning, 124 physicians were invited to participate in the one-on-one telementoring program by sending emails and telephone contact. Only 74 physicians agreed to participate, the reasons for declining from those who did not accept were not available in UNMSM records. For the quantitative phase of the study, we include data from all physicians who agreed to participate in the program. For the qualitative phase, 16 of those enrolled were interviewed, 8 of them used the program and 8 did not. Said sample size was obtained using the saturation technique, recruiting participants until their answers no longer contributed to the objectives of the interview.
About the telementoring program
Purpose
Because medical training in Peru is hospital-based and often physicians go through many challenges to carry out their professional activities during SERUMS in rural areas (clinical, community, administrative, legal, ethical activities, among others.), a telementoring Program using a mobile application was designed to communicate specialist physicians (mentors) with these newly graduated physicians in rural areas to provide them, in a short period of time, with information and personalized guidance on the problems they consulted.
Telementoring app
Within the processes of the telementoring program, a mobile application called JOIN© (Allm Inc., Japan) was used. This was a smartphone application approved in 2015 for FDA that allows healthcare professionals to share clinical data and multiple format files including DICOM medical images.
JOIN© was used as the platform of communication between SERUMS physicians and mentors or technical team. All the information shared via JOIN© follows the international standards HIPAA Compliance for securing confidentiality and anonymity [15]. Participants could share messages and ask questions in group chats, in personal chats and send images, videos, among others. Physicians interested in participating in the telementoring program were required to have a smartphone with an operating system of at least Android 5.0 or iOS 8.0 and able to access the Internet for at least one hour during the day.
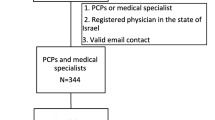
Users and structure of the telementoring program
The program was structured considering four types of users:
-
1.
Young physicians in rural service, who were the end-users of the program. When the telementoring program started, all enrolled physicians were registered in an instant messaging channel in JOIN©, where they could make inquiries by writing in the chat, sending documents, images, videos or in some cases by contacting the mentor with a video call.
-
2.
Mentors from Family medicine. This group was the first line of response to queries made by SERUMS physicians. It was made up of 15 family doctors from Lima (the capital city of Peru), who, based on a schedule, entered JOIN© and answered questions or problems of daily professional practice (clinical, community, administrative, legal, ethical activities, among others).
-
3.
Mentors from other specialties. This was the second line of response when the family doctors considered that the consultations required the opinion of another specialist doctor. The program had one specialist from each of the following medical areas: internal medicine, surgery, gynecology, obstetrics, pediatrics, neurology, and legal medicine
-
4.
Technical team. They provided technical support and ensured proper communication between SERUMS physicians and mentors when a query arose. It was made up of physicians, communications professionals, and IT professionals. The structure and workflow can be seen in Fig. 1.
Implementation
Recruitment: Graduates of 2018 from the UNMSM School of Medicine who would start SERUMS were invited to an informational meeting about the telementoring program. The invitation was made through the institutional social media and website. Everyone who attended the informational meeting was then asked to register for the program through an online form.
Training: Before starting the program, physicians and mentors received two weeks of training on the use of the application. This was done through asynchronous online training using a virtual classroom on the open platform Moodle. For this, multimedia materials (videos and documents) were used to teach about the use of the program including login, creation of user accounts, sending text, images, communication with mentors and video calls.
Program engagement and monitoring: The use of the telementoring program was not mandatory. The participants could use the application if they consider that they need guidance with a situation in their professional work.
Legal aspects and confidentiality of information: All participants had to sign a document of the terms and conditions of participation, where it was mentioned that the program was designed to provide personalized educational advice, not to solve clinical cases and it should not be used for emergency situations. The program does not represent a remote medical work, for which it was prohibited to carry out consultations sharing personal information of patients. The terms and conditions of use of this telementoring program can be downloaded in link [16].
Program length: the program was offered from June 2018 to December 2018
Program funding: The program was financed by UNMSM. The license to use the JOIN© application was financed by the Ministry of Telecommunications of Japan and granted to the UNMSM for research projects during the year 2018–2019.
Measures and data analysis
First, we collected quantitative data from SERUMS physicians who enrolled in the telementoring Program in 2018 available in UNMSM registries of the telementoring program. Some variables were the level of resolution of the healthcare facility they work according to Peruvian normativity [17], dependency, quintile of poverty, and location. In addition, we collected data regarding mobile application usage, such as the total number of queries, attended cases, average response-time and medical specialties required from the JOIN© app records. Descriptive analyses were performed using Stata 16 (Stata Corp, College Station, TX, USA). Numerical variables were summarized means and standard deviations, and categorical variables were summarized as frequencies and percentages.
Then, we collected qualitative information through telephone interviews. We explored perceived ease of use, usefulness, and reasons for participating in the telementoring program. The interviews lasted an average of 15 min and were audio recorded. For the analysis, the ATLAS.ti v7.0 software was used, applying the thematic analysis methodology [18]. Content was first coded from text segments that were related to the research questions. Subsequently, these codes were linked to generate categories that outline the perceptions of SERUMS physicians.
Results
Usage
Of 74 SERUMS physicians who agreed to participate in the telementoring program and completed the initial training, 38 (51.4%) were women and more than 70% of the participants reported no previous experience with medical applications and that 79.5% reported that they worked in health facilities located in areas of poverty and extreme poverty that depended mainly on the Ministry of Health of Peru (See Table 1).
Only 12 (16.2%) of physicians enrolled used the program, that is, made inquiries or questions to the mentors. A total of 27 consultations were carried out, with a mean of 2.1 ± 1.3 consultations for each physician. All queries were answered. The majority (62.5%) were answered in less than six hours and were mainly related to the topics of dermatology (40.7%), legal medicine (14.8%) and cardiology (11.1%) (See Table 2).
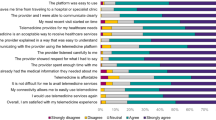
Regarding the interviews carried out, we explored the ease of use and usability of the system among physicians who used the telementoring program, and we explored the main reasons for not using the system among those who did not use the system during the study period (See Fig. 2).
Easy to use
SERUMS physicians who used the program reported that was easy to use because it was intuitive and similar to other instant messaging systems, they were more familiar with, such as WhatsApp groups. Also, due to the possibility of sharing a specific consultation in a structured way by attaching multimedia files, which were necessary for consultations with some specialties such as dermatology or pediatrics.
“I think it is a good tool to help us in our medical work. Especially for some clinical issues since in the group chat, we could share some clinical data in a structured way and images in good resolution.” (Participant 7).
However, it was also reported that some physicians found it difficult to use other features such as starting a personal chat, notification settings, etc. For this, the need for additional training was raised due to the little previous experience of some physicians in the use of medical applications.
“Almost all individual questions were done in the group chat. I didn’t really know how to use personal chat because it wasn’t very clear to me in the initial training and I’m not very familiar with apps. On certain occasions I would have liked to ask questions in private.” (Participant 1).
Usability
It was reported that the system was of great help in resolving cases since, due to the physicians’ lack of experience, they were not clear on how to act in certain situations. Also, because the queries of others could be seen in the chat, and served as learning material to develop skills to solve similar problem situations.
“It has been an important and useful tool because in some specific issues we had inexperience. Especially since we are working at the first level of care, and we do not receive specific training for some situations here… It was also useful when you share and see the cases of your colleagues, it encourages you to think about similar problems, you learn from it.” (Participant 4) .
Additionally, it was mentioned that the response time of the questions played an important role. Although they initially expected responses to be immediate, given the nature of the program (not used for urgent/emergencies) and given the limited availability of specialists, most agreed that the time delay was adequate.
“When I joined the program, I was inexperienced, so I was encouraged to consult ... now I have more knowledge in these aspects, for example, how to act when faced with an autopsy request for a legal medical problem ... The program it is especially useful in the first months of SERUMS.” (Participant 10).
Reasons for not using the system
It was reported that although it would have been very helpful to have the opinion of a specialist physicians or a university professor, recent graduated physicians did not ask questions because they had a certain degree of embarrassment and fear of appearing foolish or inexperienced to other colleagues. It was reported that they would prefer no group chats, only direct communications, and that it would be good for some not to show their full name but an alias.
“It seemed that those who did write in the groups put really difficult cases… and it was embarrassing to write simple questions. I know of a friend who sometimes had questions but didn’t want to show that he didn’t know because they could later identify him with his full name. In the case of us (physicians)... even more so, we are too proud to admit it.” (Participant 2).
Another reason was because they started accessing the program late when they had already obtained enough experience to solve most of the frequent doubts on their own. The reason for this was that they had never participated in a similar telehealth program before and did not fully understand how it worked. Most agreed that the program should be prioritized in the first months of social service.
“In my case at this point I have no longer had any doubts about cases. That would be the main reason why I did not have the need to consult or present a clinical case. It would have been especially helpful at the beginning of SERUMS when we were adapting”. (Participant 4).
Other reasons referred by SERUMS physicians were related to technical aspects. Internet bandwidth was mentioned to be a main issue, being in most cases of poor quality or simply inaccessible for some settings. Also, some physicians mentioned they did not desire to install new mobile-phone apps, instead they preferred and use frequently commercial messaging apps, such as WhatsApp, to performed clinical queries to their peers.
“I do not use the application because of the internet problem… The truth is that the connection was bad almost all last year, only calls or text messages came in” (Participant 13).
Discussion
Principal results
Our results reflect that the participation rates in this first version of the telementoring program were low and that the physicians indicated the feelings of embarrassment to ask in groups, the lack of familiarity with new apps and low connectivity as the main reasons. However, users who did use the system reported that the program was easy to use and useful for resolving their queries in a timely manner.
Other one-on-one telementoring experiences showed to be equally effective on developing medical procediments compared to physical mentoring or virtual reality assisted training [6, 7, 19, 20]. Nonetheless, most one-on-one telementoring reports has the aim of developing particular prodecimental skills and were oriented to surgical settings, so its application on primary health and most diverse set of topics still uncertain. Also, this type of telementoring strategy only covers the lack of knowledge of health personnel in the context of predefined medical topics and not in complex real-life situations. In contrast, the telementoring program studied in this research was designed as an on-demand telementoring service to support the specific medical queries of each SERUMS physicians through responses from specialist physicians using a new medical mobile application.
In general, all mentoring programs have the advantage of being more student-centered than traditional teaching [21]. However, despite this, which theoretically also promotes student motivation and engagement [22], our findings in this experience revealed low usage rates that could be due to several reasons.
First, the design of the program did not include conducting an educational survey to assess the specific needs of graduate physicians and how they would like to be provided with such information. Consequently, despite previous evidence suggesting an important need for clinical guidance during SERUMS [23], the main needs of medical graduates could actually be different. Some of these needs could include aspects of health management, legal medicine, ethics, or public health, so it would be necessary to include experts in these topics within the mentoring. This is especially relevant since most of their training at the university is mainly oriented to clinical aspects and not to these other activities [24].
Second, some SERUMS physicians referred to the presence of limited mobile internet connectivity in their healthcare facilities. This is a common problem in rural areas, where regardless of mobile phone signal coverage, connectivity could be affected considering various geographic and climatic conditions [25]. Despite this, since the program was not geared towards emergency/urgency cases and immediate responses were not necessary, we do not consider this to be a limiting factor for implementation. Due to this characteristic, if necessary, the use of voice calls or text messages could be included, which require less technical infrastructure for their application in rural areas [26].
Thirdly, despite having a telementoring system with family doctors and specialist doctors available, the SERUMS physicians preferred to consult with their own networks of contacts, generally made up of other recently graduated physicians, with whom they had more confidence. Some degree of embarrassment in asking questions and fear of appearing inexperienced to other colleagues was reported. This situation was also evidenced in other countries such as Colombia [27] and suggests that future telementoring interventions for recently graduated physicians should include the presence of previously known professionals, such as university professors of medicine and with experience who provide greater confidence. In addition to enabling ways to ask questions privately or anonymously. Another alternative would be to include a group telementoring approach, which has shown evidence of improving knowledge, perceived ability and patient outcomes in primary care [28, 29] and/or rural settings [27, 30, 31]; and which also has the advantage of reducing health professionals reluctance to participate, as they report feeling integrated into their learning teams [28].
Fourth, most of the physicians who participated in the study had no prior experience using medical apps. This would imply that, despite having a smartphone, it is possible that many of them do not trust or prefer not to use new applications or technological tools to support their professional training, as observed in medical students and recent graduates in our country [32, 33].
On the other hand, among the physicians who did actively use the Telementoring program, it was found that most of the consultations are related to dermatology and legal medicine, specialties not initially included in the program. Possibly due to little prior training in these specialties at the primary care level during university [34]. This leads us to think that it is important to include more specialists from different branches in a telementoring program for primary care, so it is important to explore the needs of users before implementing it [35].
In terms of ease of use, our findings were similar to a study conducted at Jikei University Hospital in Japan, in which interns reported that the use of the JOIN© was intuitive and similar to other apps. Messaging as LINE [36]. Still, the need for additional training was also raised. This could be explained by their lack of previous experience with the use of medical applications, which was reported by almost 70% of the physicians enrolled in the program. Although this is contradictory with other Peruvian studies, where they show that 97% of the interviewees reported that they used some medical application and 72% used applications to share medical images or videos [37]. Another explanation could be due to the fact that the training provided was carried out through an asynchronous and unsupervised online course, which, although it allowed progress at the student’s pace and to review the materials at any time, could not have been completed correctly. This is consistent with evaluations of a massive open online courses that showed a dropout rate of 84.5% of registered participants, regardless of geographic location [38].
Limitations and strengths
Although these are important findings, some limitations must be considered. First, the recruitment of participants was not random but was done through invitations by mail and telephone, which implies a possible selection bias, more specifically a voluntary bias. Second, the interviews were conducted at the end of the SERUMS year, so there might be some possibility of recall bias. Finally, we do not know if the sociodemographic or occupational characteristics of physicians from other universities are similar to those from UNMSM, so our findings may not be extrapolated to all contexts.
Despite these limitations, our study provides important insights into the potential of telementoring interventions using mobile technologies to close knowledge gaps in rural physicians in low- and middle-income countries. Although we were unable to measure the direct impact of the program, our results suggest that this impact exists and would merit evaluation in future cohorts. In addition, the Telementoring program presented several strengths that have previously been shown to generate positive results in medical education, such as the ease of use of the technology, the confidential transmission of information, and the adequate response time to queries about real problem situations of a recently graduated physicians working in a rural area [39].
Conclusions
Telementoring through a mobile application represents a useful alternative to provide educational support to young physicians who work in rural areas and who need help to face problems that arise in their professional work. However, its implementation may be limited by the physicians' lack of experience in using mobile applications, limited Internet access, lack of anonymization when asking questions, and the presence of medical specialist mentors with whom they did not trust to ask openly. This tells us that telementoring interventions designed for physicians working in rural areas should include the considerations discussed above such as conducting an initial formative study and a final evaluation of the impact of improving physicians' experience while serving in rural areas.
Availability of data and materials
The Faculty of Medicine of the UNMSM has possession of the raw quantitative information regarding the Telementoring program and reserves the right to share it publicly, but it can be requested for research purposes through a formal request to the faculty at telesalud.fm@unmsm.edu.pe. Interview respondents were assured raw qualitative data would remain confidential and would not be shared, hence, data are not available, but are available from the corresponding author upon request.
Abbreviations
- SERUMS:
-
Rural and Urban-Edge Health Service Program
- UNMSM:
-
National University of San Marcos
- FDA:
-
Food and Drug Administration
- ICT:
-
Information and Communication Technology
References
Mikre F. The Roles of Information communication technologies in education: review article with emphasis to the computer and Internet. Ethiop J Educ Sci. 2011;6(2):109–26.
Eisenman G, Thornton H. Telementoring: Helping New Teachers through the First Year. THE J. 1999;26(9):79–82.
Cheallaigh CN, O’Leary A, Keating S, Singleton A, Heffernan S, Keenan E, et al. Telementoring with project ECHO: a pilot study in Europe. BMJ Innov. 2017;3(3). Available from: https://innovations.bmj.com/content/3/3/144. [Cited 2022 Oct 30]
Carlin L, Zhao J, Dubin R, Taenzer P, Sidrak H, Furlan A. Project ECHO Telementoring Intervention for Managing Chronic Pain in Primary Care: Insights from a Qualitative Study. Pain Med Malden Mass. 2018;19(6):1140–6.
Arora S, Kalishman SG, Thornton KA, Komaromy MS, Katzman JG, Struminger BB, et al. Project ECHO: A Telementoring Network Model for Continuing Professional Development. J Contin Educ Health Prof. 2017;37(4):239–44.
Kirkpatrick AW, McKee JL, Tomlinson C, Donley N, Ball CG, Wachs J. A randomized controlled pilot trial of video-modelling versus telementoring for improved hemorrhage control wound packing. Am J Surg. 2022;224(2):769–74.
Antoniou SA, Antoniou GA, Franzen J, Bollmann S, Koch OO, Pointner R, et al. A comprehensive review of telementoring applications in laparoscopic general surgery. Surg Endosc. 2012;26(8):2111–6.
Ministerio de Salud del Perú. Reglamento de la Ley No 23330 Servicio Rural y Urbano Marginal de Salud-SERUMS. D.S. No 005–97-SA, 23330 Jun 22, 1997. Available from: https://www.amp.pe/normasjurDS_N_005_97_SA.htm
AnticonaHuaynate CF, PajueloTravezaño MJ, Correa M, MaytaMalpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. 2015;5(15):454.
Inga-Berrospi F, Taype-Rondán Á, Purizaca-Rosillo N. La problemática del médico serumista en el Perú: conclusiones de la Segunda Convención Nacional de Médicos Serumistas, 2013. An Fac Med. 2014;75(3):271–2.
Solari ER. «Allá es clínicamente así: saber llegar». De la formación a la práctica profesional médica. El Servicio Rural Urbano Marginal en Salud (SERUMS). Apunt Rev Cienc Soc. 2011;18:55–80.
Huff EW, Mack NA, Cummings R, Womack K, Gosha K, Gilbert JE. Evaluating the Usability of Pervasive Conversational User Interfaces for Virtual Mentoring. In: Zaphiris P, Ioannou A, editors. Learning and Collaboration Technologies Ubiquitous and Virtual Environments for Learning and Collaboration. Cham: Springer International Publishing; 2019. p. 80–98 (Lecture Notes in Computer Science).
Marques L, Matsubara P, de Souza Filho JC, Gomes G, Gadelha B, Conte T. Challenges and Learning from Remote Teaching of Usability and UX: An Experience Report. In: 19th Brazilian Symposium on Software Quality. New York, NY, USA: Association for Computing Machinery; 2021. p. 1–9. (SBQS’20). https://doi.org/10.1145/3439961.3440003. [Cited 2022 Oct 30]
Caffery LJ, Martin-Khan M, Wade V. Mixed methods for telehealth research. J Telemed Telecare. 2017;23(9):764–9.
USDHHS. OCR privacy brief: Summary of the HIPAA privacy rule. Summary of HIPAA Privacy Rule. 2003.
Unidad de Telesalud. UNMSM. Terminos y Condiciones de participación del programa de Telementoría para médicos serumistas en zonas rurales. Google Docs. 2019. Available from: https://docs.google.com/document/d/1z9HRbjs39piCon2UcqZsrzK0B64NJ-9u/edit?usp=sharing&ouid=111961705114195765163&rtpof=true&sd=true&usp=embed_facebook. [Cited 2022 Jun 19]
Ministerio de Salud del Perú. Norma Técnica de Salud en Telesalud. Perú; 2009 p. 1–25.
Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. United States: SAGE Publications, Inc.; 2012. p. 321. Available from: https://methods.sagepub.com/book/applied-thematic-analysis. [Cited 2022 Oct 30]
Williams TP, Klimberg V, Perez A. Tele-education assisted mentorship in surgery (TEAMS). J Surg Oncol. 2021;124(2):250–4.
Shabir D, Abdurahiman N, Padhan J, Anbatawi M, Trinh M, Balakrishnan S, et al. Preliminary design and evaluation of a remote tele-mentoring system for minimally invasive surgery. Surg Endosc. 2022;36(5):3663–74.
Walsh K. Online mentoring in medical education. South Afr Fam Pract. 2016;58(sup1):S7-8.
Kaput K. Evidence for Student-Centered Learning Education Evolving; 2018. Available from: https://files.eric.ed.gov/fulltext/ED581111.pdf
AnticonaHuaynate CF, PajueloTravezaño MJ, Correa M, MaytaMalpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. 2015;5(15):454.
Reyes Solari E. «Allá es clínicamente así: saber llegar». De la formación a la práctica profesional médica. El Servicio Rural Urbano Marginal en Salud (SERUMS). Apunt Rev Cienc Soc. 2011;38(69):55–80.
Telefónica presenta “Internet para todos”, un proyecto colaborativo para conectar a los no conectados en Latinoamérica | Detalle | Noticias | Sala de Prensa | Telefónica. Available from: https://www.telefonica.com/es/web/sala-de-prensa/-/telefonica-presenta-internet-para-todos-un-proyecto-colaborativo-para-conectar-a-los-no-conectados-en-latinoamerica. [Cited 2019 Oct 29]
Simba F, Mwinyiwiwa BM, Mjema EM, Trojer L, Mvungi NH. Broadband access technologies for rural connectivity in developing countries. Int J Res Rev Comput Sci IJRRCS. 2011;2(2):312–9.
Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199–207.
Teixeira PA, Bresnahan MP, Laraque F, Litwin AH, Shukla SJ, Schwartz JM, et al. Telementoring of primary care providers delivering hepatitis C treatment in New York City: Results from Project INSPIRE. Learn Health Syst. 2018;2(3):e10056.
Eaton LH, Godfrey DS, Langford DJ, Rue T, Tauben DJ, Doorenbos AZ. Telementoring for improving primary care provider knowledge and competence in managing chronic pain: A randomised controlled trial. J Telemed Telecare. 2018;27:1357633X18802978.
Lopez MS, Baker ES, Milbourne AM, Gowen RM, Rodriguez AM, Lorenzoni C, et al. Project ECHO: A Telementoring Program for Cervical Cancer Prevention and Treatment in Low-Resource Settings. J Glob Oncol. 2017;3(5):658–65.
Mehrotra K, Chand P, Bandawar M, Rao Sagi M, Kaur S, Aurobind G, et al. Effectiveness of NIMHANS ECHO blended tele-mentoring model on Integrated Mental Health and Addiction for counsellors in rural and underserved districts of Chhattisgarh India. Asian J Psychiatry. 2018;36:123–7.
Mejía CR, Valladares-Garrido MJ, Luyo-Rivas A, Valladares-Garrido D, Talledo-Ulfe L, Vilela-Estrada MA, et al. Factores asociados al uso regular de fuentes de información en estudiantes de medicina de cuatro ciudades del Perú. Rev Peru Med Exp Salud Publica. 2015;32(2):230–6.
Mejía CR, Caceres OJ, Vera CA, Nizama-Vía A, Curioso WH, Mayta-Tristán P. Uso de fuentes de información en médicos recién graduados de Lima. Rev Peru Med Exp Salud Publica. 2014;31(4):716–20.
Mejía Álvarez CR, Inga Berrospi F, Contreras P, Requena T, Ruiz D. Serums: Recomendaciones basadas en la experiencia. Universidad Continental. Universidad Continental; 2018. Available from: https://repositorio.continental.edu.pe/handle/20.500.12394/4624. [Cited 2022 Jun 19]
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res. 2011;38(2):65–76.
Riquelme Godoy Á. Evaluación de interfaces de usuario en aplicación mHealth. [Santiago de Chile]: Universidad de Chile.; 2019. Available from: https://repositorio.uchile.cl/handle/2250/175235
Mejia CR, Herrera CZ, Enríquez WF, Vargas M, Cárdenas MM, Oliva GJ, et al. Uso de teléfonos inteligentes y aplicaciones para la autocapacitación y la telemedicina en médicos peruanos. Rev Cuba Inf En Cienc Salud. 2016;27(3):286–97.
Quispe-Gamarra J, Escobar-Agreda S, Moscoso MG, Vargas J. Nivel de deserción en un curso virtual en salud en Perú. Rev Peru Med Exp Salud Pública. 2021;38(4):666–7.
Moran AM, Coyle J, Pope R, Boxall D, Nancarrow SA, Young J. Supervision, support and mentoring interventions for health practitioners in rural and remote contexts: an integrative review and thematic synthesis of the literature to identify mechanisms for successful outcomes. Hum Resour Health. 2014;12(1):10.
Acknowledgements
We would like to thank the SERUMS physicians who participated in this study and the Information technologies and innovation in healthcare Research Group from the UNMSM.
Funding
None.
Author information
Authors and Affiliations
Contributions
LR, HE and GR was involved in study conception. MM and MC collected data for quantitative analysis. MR, SE and JQ conducted interviews, prepared the results, and analyze and interpreted the data. MR and JS write article draft. All authors contributed to the design of study protocol and approve final version of the article to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Tropical Medicine Institute IRB of the UNMSM (CIEI-2019–003). Verbal consent to participate in the interviews was requested, and procedure of obtaining verbal consent was approved by the Tropical Medicine Institute IRB of the UNMSM (Study-code: CIEI-2019–003). The JOIN© mobile application is certified by the US-FDA (Food and Drug Administration). The UNMSM provided data confidentiality guidelines to the participating physicians, focusing on protecting the personal data from the patients involved. Finally, this study was carried out in accordance with the guidelines of the Declaration of Helsinki and the Finnish National Advisory Board on Research Ethics.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rojas-Mezarina, L., Escobar-Agreda, S., Chahuara-Rojas, M. et al. Usability and perceptions of a one-on-one telementoring program for young physicians in rural settings of Peru: a mixed method study. BMC Med Educ 23, 175 (2023). https://doi.org/10.1186/s12909-023-04142-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04142-2