Abstract
Context
The challenging nature of the transition from medical student to doctor is highlighted by the associated negative consequences to new doctors’ mental health and wellbeing. Enhanced understanding of the lived experience of recent medical graduates as they move through the stages of transition over the first year of practice can inform interventions to ease the difficulties encountered.
Methods
Using interpretative phenomenological analysis (IPA), a novel approach to this topic, we explored the lived experience of transition from student to doctor over the first year of practice after graduation. Twelve new graduates were purposively recruited. We conducted semi-structured interviews at the end of their first year of practice with respect to their experience over the first year.
Results
The experience of transition was characterised by overlapping temporal stages. Participants’ initial adjustment period was characterised by shock, coping and stabilisation. A phase of development followed, with growth in confidence and a focus on self-care. Adversity was experienced in the form of interprofessional tensions, overwork, isolation and mistreatment. Finally, a period of reflection and rationalisation marked the end of the first year.
Discussion
Following initial anxiety regarding competence and performance, participants’ experience of transition was predominantly influenced by cultural, relational and contextual aspects of clinical practice. Solutions to ease this challenging time include stage-specific transitional interventions, curricular change at both undergraduate and postgraduate levels and a re-evaluation of the clinical learning environment to mitigate the difficulties endured.
Similar content being viewed by others
Introduction
Although the transition from medical student to doctor has been the focus of much research in medical education, it remains problematic, with persistent reports of a deterioration in doctors’ mental health and wellbeing during this time [1, 2]. The enduring nature of the challenges encountered by medical graduates, across countries and specialties, points to issues common to the transition experience [1, 3,4,5,6]. Commencing work has been described as a major change for new graduates, who can lack confidence and feel anxious in their role, with new responsibility and changing relationships with their workplace colleagues [7,8,9,10,11]. Issues relating to support, workload, workplace relationships and role ambiguity contribute to psychological distress in this group [12, 13]. Challenges to new doctors’ professional identity formation or personal growth during the first year of practice include adapting to the medical culture, and issues with confidence, work-life balance, self-care, and interactions with patients and colleagues [14,15,16].
The transition from medical student to doctor has been referred to, as a ‘rite of passage’, a process over time, involving different phases of, separation (withdrawal or detachment from a previous status or identity), transition (the in-between or ‘liminal stage’), and incorporation (assumption of new status or identity) [17,18,19]. This resonates with our understanding of the transition as an ongoing, dynamic process of professional discontinuity, with movement from ‘one context and set of interpersonal relationships to another’ [20], encompassing changes in ‘expectancies, tasks or responsibilities’ [21, 22]. The dynamic nature of this transition is mirrored in the variations in mood, empathy, stress and wellbeing reported in new doctors over the course of the first year [23,24,25,26], with their wellbeing shown to deteriorate during this time. Longitudinal studies, have described the experience over the first year in terms of a ‘preparedness journey’ with the development of competence and confidence over time [5, 11, 27, 28].
In summary, the current understanding of the first year of practice is of an intense formative experience involving different challenges and stressors with temporal variation in emotion and wellbeing. However the variety of cultural and contextual factors that influence the behaviour of new doctors [29] suggest that the actual experience of the transition as a dynamic transformative experience over time is more complex than is currently understood. We argue that deeper appreciation of this process is critical as a forerunner to intervention.
Research into other workplace transitions can inform our understanding of the process of transition to practice for medical graduates. Nicholson’s theory of work role transitions, describes a cycle in perpetual motion, each stage having different sets of tasks, expectancies, problems and solutions, and comprising of, prior preparation, followed by the initial encounter, a period of adjustment and a stabilisation phase [30]. Regarding transitions in healthcare, extensive work has been carried out on the transition of nursing graduates to professional practice [31, 32]. Kramer described an initial ‘honeymoon stage’ during orientation, characterised by idealism and excitement, followed by ‘reality shock’, where the disparity between expectations and the reality of practice provoked feelings of anxiety, doubt and confusion. After this stage comes ‘recovery’ with reduced anxiety and coping, and finally ‘resolution’ resulting in success or burnout [31]. Informed by Kramer, Duchscher expressed the transition of nursing graduates over the first year in terms of ‘a complex but relatively predictable array of emotional, intellectual, physical, sociocultural and developmental issues that in turn feed a progressive and sequential pattern of personal and professional evolution’ [32, 33].
The majority of qualitative research to date into the transition from medical student to doctor, described here, has been limited to thematic analysis, with other studies employing a grounded theory methodology. Enhanced understanding of the experience of new medical graduates is critical to wellbeing, and would inform interventions to ease the difficulties encountered. An exploration of the lived experience of recent medical graduates over the first year of practice using a phenomenological lens, specifically interpretative phenomenological analysis, has not been carried out. Therefore, we aim to advance the current understanding of the transition by exploring the lived experience of recent medical graduates as they move through the stages of transition over the first year of practice using the contemporary phenomenological approach of interpretative phenomenological analysis. This study is part of a larger project exploring the lived experience of recent graduates as they anticipate their transition to clinical practice and of their experience over the first year of work [34].
Methodology
This study was carried out within an interpretative paradigm using interpretative phenomenological analysis (IPA) as originally described by Jonathan Smith, of Birkbeck, University of London in 1996 [35]. The theoretical underpinnings of IPA include phenomenology, hermeneutics and idiography. Phenomenology focuses on how individuals make sense of the world and aims to provide insightful accounts of subjective experience [36, 37]. IPA is connected to the hermeneutic tradition, in it’s acknowledgement of the role of the researcher in making sense of the individual’s account of their experience [38]. Smith has described a hermeneutics of empathy in IPA’s attempt to achieve an insider’s perspective, and a hermeneutics of questioning with its interpretive undertaking to analyse and make sense of the experience [35]. IPA involves a ‘double hermeneutic’ in that, the participant provides an account of how they have made sense of their experience, and the researcher, interprets this account, potentially revealing insights beyond the direct assertions of the participant [35]. Finally, IPA involves an idiographic commitment with its focus on a detailed exploration of the particular. An in-depth exploration of each individual case is carried out before analysis of subsequent cases, after which, similarities and differences between cases can be explored [35]. Further detail on the methodology chosen, is provided in the first paper arising from this project, exploring the experience of anticipation of commencing work as a doctor, from the perspective of new medical graduates [34].
Context
Internship in Ireland is a twelve-month period of pre-registration training following graduation from medical school. This study was carried out in the Southern Intern Training Network, one of six networks nationally with responsibility for this first postgraduate year of training. Interns spend a minimum of three months in General Surgery and three months in General Medicine. The remaining two, three-month, rotations are spent in other specialties such as Paediatrics, Psychiatry, Surgery, and General Practice. Each post involves the newly qualified doctor working within a particular specialty for the duration of that rotation.
Ethical approval for this study was granted by the Clinical Research Ethics Committee of the Cork Teaching Hospitals Ireland. NC, POL and DB are medical doctors with roles in the undergraduate medical programme linked to the Southern Intern Training Network. POL also has a role in the Intern Training Network. NC, who carried out recruitment and interviews, had no oversight of the participants as interns. The interviews were anonymised prior to analysis by the rest of the research team, and pseudonyms were used in the reporting of results. The wellbeing of participants was considered at all stages of the study, including the potential need for support or intervention, however no such need arose.
Recruitment
Participants were purposively recruited, with respect to gender and graduate entry to medical school or entry directly from high school. All were in their first year of postgraduate practice in the Southern Intern Training Network, working in affiliated hospitals and primary care settings. Contact emails were obtained from the Network administrator and thirtyfive recently qualified doctors were emailed and invited to participate.
Data collection
Individual semi-structured interviews were carried out with participants as they neared the end of their first year (Interview schedule- appendix 1), with respect to their experience of the first year of practice. Interviews were audio recorded, transcribed verbatim, and anonymised.
Data analysis
Data was analysed using interpretative phenomenological analysis [35, 39]. The research team, NC, POL and DB met regularly to discuss all aspects of data analysis. Analysis began with immersion and familiarisation with the data by listening to, reading and re reading each interview. Experiential themes were identified (recurrent experiential assertions), which were then grouped into clusters of themes addressing related issues called superordinate themes. Each transcript was analysed fully prior to moving on to the next one. When all data was analysed, integration of themes across the entire dataset was carried out and commonality and divergence were noted. NVivo software was used as a data management tool [40].
Reflexivity
We acknowledge our role as researchers in the co-construction of knowledge with participants. As faculty members of the medical school aligned with the Southern Intern Training Network, we were aware that as ‘insiders’ we would have preconceptions and beliefs about the research question. We critically reflected on how our prior experience and beliefs about the phenomenon may impact on the research process. While familiarity with the nature and language of the context could be beneficial, we were cognisant that our prior experience would not translate into knowledge of how others might experience the phenomenon. Throughout the research process, the research team continually reflected and discussed on how our attitudes might be informing the research. We supported each other’s reflexivity and kept reflexive diaries throughout the process.
Results
Twelve participants agreed to take part in these interviews, six males, (two who had prior degrees and four who commenced their medical degrees directly from high school) and six females (two who had prior degrees and four directly from high school).
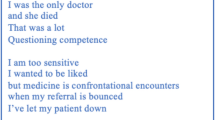
We identified superordinate themes of, adjustment, development, adversity, and rationalisation (Fig. 1). These themes reflected overlapping temporal phases in the transition experience.
Commencing work provoked an emotional response from participants, and prompted compensatory actions and dependence on others in the workplace. In time, participants became more comfortable in their roles, however, fulfilling the requirements of the job entailed endurance of challenging working conditions, lack of support and difficult workplace interactions. Finally, from their perspective at the end of the year, having prevailed over the challenges encountered, participants reflected on their role, and on their personal evolution.
Adjustment
This theme was comprised of subthemes of shock, coping and stabilisation. Many participants experienced negative emotions, including anxiety and self-doubt during the early phase of commencing practice. Support was appreciated, and some dysfunctional coping strategies were employed to fulfil workplace expectations. Participants’ critical gaze at this stage was predominantly inward-looking, focusing on themselves and their performance. As time progressed, their initial fear and anxiety abated as they became more comfortable in their new role.
Shock
Words such as terrifying, overwhelming and very stressful were used by participants to describe their early days as a doctor. New responsibility, role uncertainty and fear of making mistakes contributed to the fear and anxiety experienced by most, to varying degrees in the early days.
‘The first week was absolutely terrifying and everything was a challenge at that point, from taking blood to cannulas to prescribing to being called to a sick patient and having to assess them, everything was hard at the start’ Jane
Most struggled initially with prioritisation of workload and the unique pressure of the bleep system, especially when they were on call at night, which was stressful and sometimes overwhelming.
Responding to calls on your own and being overwhelmed by bleeps and not being able to triage things effectively is really and can be really quite overwhelming Gerard
Not all early work experiences were difficult. Andrew and Brian described a gentler transition which did not include these negative emotions, however both expressed frustration and disappointment that their first job did not require them to assume responsibility.
So, very little sort of using your brain, but it was an ok one to start off on for maybe the first 6 weeks until you realise this is actually not medicine Brian
Coping
Coping strategies in the early weeks included working longer hours, missing breaks to fulfil their obligations and depending on others in the workplace for support and guidance.
And again, coming in earlier and getting it done so you wouldn’t be delaying the surgeons Claire
I used to like not eat during the day on the day job because I would be like, I had so much to do. Mark
Their nursing colleagues were crucial sources of early support. Participants felt reliant and dependent on them, willingly accepting their direction without question.
I think at the beginning … they are your best allies and I think you lack confidence in yourself so you do whatever they say. If they say jump, you’re just, ok how high Faye
All, also acknowledged the benefit of integration, camaraderie and support that derived from a team structure and the solidarity of other interns was greatly valued.
I had a fellow intern so the two of us used to go around together so having him made everything so much easier … We had 4 *SHOs … they were great as well ... So it was good, it was a nice team, the structure kind of made it. Deirdre *senior house officers
Stabilisation
The initial negative feelings of shock abated with time. This marked the transition to the next phase of the experience for participants.
I was afraid of making mistakes, that I was going to hurt someone, but then that eases off … gradually you get a little more confident as you go along Jane
Development
This superordinate theme comprised of subthemes of growth in confidence and focus on self-care. After the initial adjustment period, participants continued to evolve, developing increasing confidence and competence. This resulted in a change in some of their earlier attitudes and perspectives.
Growth in confidence
As the year progressed, participants became more competent and confident, characterised by their assumption of increased responsibility, making clinical decisions and prioritising their workload.
I think for me that was the active point of transition where I went from just blindly following orders … to actually employing my own clinical judgement Gerard
Gradually, their requirement for support lessened and their attitudes towards requesting support also changed.
I would have looked at asking for help a bit differently early on .. felt a bit bad about having to ask .. now I realise I have brought this to where I can bring it .. and part of your job almost is to get further help Hannah
Focus on self-care
In contrast to the initial days of transition, participants recognised the importance of self-care, and of maintaining a work life balance.
On long days .. when you are run off your feet … it was about teaching myself that I needed to stop … to take a break even if it was only 20 minutes or something .. because I would work better after that Jane
Keeping up hobbies and things outside work … that has been really important to me.. seeing friends and talking with them … It is important to take your mind off things Gerard
Adversity
This superordinate theme comprised of subthemes of interprofessional tensions, overwork, isolation, and rude and aggressive communication. Following participants’ initial adjustment to the clinical environment, their relationships with their nursing colleagues began to change. During this stage, their main focus shifted from their own abilities or shortcomings, to exogenous workplace stressors. All described experiences of feeling overworked, unsupported, or subject to difficult workplace interactions with more senior doctors, for example when requesting consults or investigations, which they accepted and endured.
Interprofessional tensions
As their first year of practice progressed, rather than simply complying with all the demands placed on them, participants became more assertive. This sometimes resulted in tensions developing with their nursing colleagues.
The nurses are more of a challenge now .. at the beginning .. whatever they said, I did, because I didn’t know, whereas now you are questioning them more and it is a little bit more of a challenge. Deirdre
Faye addressed what she perceived as the strong division between interns and their nursing colleagues, relating this, in part, to their different working practices.
There is definitely quite a strong division between doctors and nurses .. they [nurses] have no consideration, they are on a ward and they look after their room and they know their patients well. They have no kind of notion … that you could have patients on every ward of the hospital and you are up and down …. they could bleep you and say I have such and such daughter here she wants to meet you and like I am ... [busy with a sick patient] .. and they won’t care and then they will document it 'wouldn’t speak to daughter'. Faye
Many participants were critical of how their nursing colleagues used the bleep system, including the constant nature of the calls, their tone which was often perceived as pressurising and demanding, and their numerous non-urgent requests, especially on call when participants were often very busy.
They have just decided ... they need a repeat* potassium at 2 in the morning .. there is no point arguing with them because they are just going to keep bleeping you. Irene*blood test
Some participants also struggled with what they perceived as a devolving of responsibility for a patient to them by the nurses, while others felt undermined when nurses would contact senior doctors if they did not respond quickly or appropriately enough.
They’re all about defending themselves and all about, ‘bleeped doctor up, never came’ you know, there will be no explanation from the doctor documented afterwards, just, ‘never came’ you know Faye
And I told the nurses, ‘she’s fine, you don’t need to give her fluids, she’s sleeping, and she’s fine’…. What annoyed me was she went over my head and rang the SHO. Irene
Gerard and Jane however, contended that nurses are generally more experienced and are therefore entitled to question interns, or seek higher authority, and, that jobs, perceived as trivial by many interns, could be valuable learning experiences and are also important to the patient.
That is just part of being an intern I think. You are the first port of call and you are the first person to decide is this trivial or is it not… it is only by seeing those as well that you learn what actually is trivial and what is not…. It is important to the patients as well ... if they are worried about something .. it is good to reassure them and things. Jane
Overwork
Most participants had experiences where they felt overwhelmed due to long working hours, intense workloads, and lack of breaks, especially on call. The resulting consequences to their health and wellbeing, included extreme fatigue, irritability, emotional lability and diminished empathy. Participants accepted and complied with the all workplace demands placed on them.
It was so busy. It was horrible, it was just constantly, my bleep ...…. But that was very overwhelming ... at the end of the shift I felt so emotionally drained I felt that I was going to cry, not from just being upset but from the emotional exhaustion of it you know? Irene
When you are tired sometimes it is difficult to muster empathy for patients and that’s meant to be the core of the job you know ... so you feel like that's been chipped away a little bit. Brian
Faye felt there were occasions when her performance was impaired, potentially compromising patient safety.
You're hypoglycaemic. You’re overloaded with work. You’re completely not performing to your best and you slow down and then your job ends up longer because you are doing it slower so it is horrendous like ... and you are not even thinking straight. I have been on call where I have put my own date of birth on blood bottles because I cannot even see or think Faye
Isolation
Although in general, participants felt supported, most admitted to occasions when they felt isolated and alone. Support could be variable depending on specialty, individual asked, or time of the day.
With surgery, you’re thrown in the deep end, because … all the team goes off the theatre for the day, and unless there is something like a massive, massive emergency, you don’t want to go up and interrupt a theatre. Noel
I think it is lonely, you are on your own, depending on what regs* you are on with, some of them are very helpful .. others a little slower... Deirdre (support seeking on call) *registrar or senior resident
Most participants recounted episodes where they had difficulty accessing support in spite of requesting it, which caused them great distress.
There was one night that I think will always haunt me, … we had a really sick patient…and I rang the surgical reg .... [she said], I’ll be in A&E for another hour .. you end up pleading like, please,…. and like at 2 o’clock in the morning you’re like, can somebody else just come .. I remember thinking that night, god it’s just me... I remember feeling very unsupported, …. I kind of cried after that, …thinking, god, is this what it’s going to be like every night? Claire
Panic and stress initially and then quite frustrated because .. it is not fair on the patient, they shouldn’t be left in a situation where they are sick and I don’t know what to do, and the person who should know what to do isn’t going to come and see them. Frustrated for myself as well because you are told in medical school oh don’t worry you won’t ever be left in a situation where you'll had to deal with something Jane
Rude and aggressive communication
Participants were vulnerable to difficult interactions with senior doctors when they had to contact other teams to request consults or investigations. Participants accepted, rather than challenged, any negative or hostile reactions.
I remember ringing for consults,.. sometimes you feel afraid, because you wouldn’t know what form you’d find the other person on the phone. Claire
The interactions could be quite unpleasant, distressing and belittling.
‘I remember contacting an anaesthetist ... I was told to contact him and he was going ‘why is an intern contacting me? Your Reg needs to contact me’ and *bang’ Deirdre (* he hung up the phone)
One of the interns was brought to tears by a Radiologist and was furious with herself and didn’t do it until after she had left but it was just unnecessary really … and you know interns generally get the brunt of that kind of thing I suppose which is unfortunate. Mark
Participants described how they accepted mistreatment directed towards them, with Noel perceiving organisational tolerance towards it.
‘You just learn to live with it’ Jane
‘They do this sort of thing all the time, they get away with it, it’s never really challenged properly’ Noel
Rationalisation
This superordinate theme was comprised of subthemes of survived and transformed, and learning from adversity. This final phase is characterised by a retrospective positive evaluation of the transition, an acknowledgement of the learning opportunities in the challenging aspects of the year and a recognition of personal evolution over the course of the year.
Survived and transformed
From their perspective at the end of the year, the most commonly held overall impression was that it was an enjoyable experience, and that they had prevailed over the challenges encountered.
Yeah I enjoyed it, yeah I liked it and survived it Mark
Reflecting on the early transition period, initial sources of fear and apprehension seemed much less significant. Participants recognised how they changed over the course of the year.
The things that worried me back then, now seem a bit silly. Just literally I was so ridiculously stressed about putting in a line, which now I can do in my sleep, so that’s great. Irene
It has been a massive transition, I don’t think I would recognise myself if I saw myself approaching a patient back in July now Gerard
Learning through adversity
Many participants acknowledged the role played by the more challenging aspects of the job in their evolution as more resilient, competent practitioners. Intense workloads, acutely ill patients, and working out of hours, although often stressful and anxiety provoking at the time, were now evaluated as important and valued learning opportunities.
The pace was so much faster, it was a little bit overwhelming at times, .. but I actually think I prefer it like that, because you get more efficient with dealing with things, and learning to do things quickly Irene
So it was very much learning on your feet but as terrifying as it is at the time it is nearly the best way to learn. Jane
Discussion
Principal findings
Our analysis identified overlapping temporal stages, as students made the transition to doctor over the first year post graduation. The early transition period was characterised by a high degree of anxiety regarding competence and performance. Support eased the experience, and some dysfunctional strategies, such as skipping meals and breaks, were employed to fulfil the requirements of the role. While the necessary skills and competencies were significant in participants’ early transition experience, beyond this, cultural, relational and contextual aspects of clinical practice were more influential in participants’ experience of the transition. From their perspective at the end of the year, challenges were minimised and reframed as learning experiences.
Initial experience
Fear and apprehension were prominent early emotions in this study, resonating with existing research on medical graduates’ transition to practice [8, 9, 11]. Organisational socialisation theory describes the early experience of a newcomer to an organisation characterised by sense making and coping, and is often termed ‘reality shock’ or ‘transition shock’. Factors that contribute to this are, a disparity between job expectations and the reality encountered (surprise), and the degree of change (the objective difference between previous and new roles), and contrast (subjective difference as perceived by the individual) encountered [41]. The shock described in this study reflects the degree of surprise, change and contrast experienced by participants in their new roles compared with their previous roles as medical students [7, 42].
Participants’ expectations of their performance did not include any allowances for the early transition period. High personal expectations, and concerns regarding competency increase the stress of the transition [7, 22]. The dysfunctional coping strategies employed to compensate for perceived inefficiency, reflect the pressure on novice doctors to ‘keep on top of things’ [43], and perhaps the common assumption in medicine of doctors as ‘supernaturally resilient’ [44]. A more positive coping strategy was participants’ support-seeking from workplace relationships. Access to insiders can provide the context-specific experiences that newcomers lack, helping them to make sense of their new reality and facilitating enhanced understanding of their new environment [45]. Support and team integration [46, 47], positively impacts on feelings of preparedness for transition [48], improves work related wellbeing [23, 25], creates a positive working environment and reduces the stress around transition as seen in this study [8, 10, 23, 25, 27, 49].
Inter-professional collaboration
The early reliance on nursing colleagues by doctors commencing clinical work, is not a novel finding [23, 47]. Nurses play an important but often unacknowledged role in the socialisation of new doctors [50, 51]. Participants displayed an initial vulnerability and willingness to accept their direction without question, as they acclimatised to their new roles. This resonates with Burford et als’ ‘pragmatic hierarchy’ where the experience and expertise of nurses carries an authority to which participants were initially happy to defer [50].
Time and experience in the clinical environment diminished this initial collaborative practice. As participants began to critically appraise the requirements of their role, tensions became apparent. A number of cultural and organisational barriers to collaborative practice have been described [52,53,54]. Doctors and nurses appear to identify primarily with their own teams and only secondarily with the interprofessional team, illustrating the ‘tribal behaviours associated with the discrete cultures of the different professions’ [52, 55]. Their individual work practices differ substantially, while nurses are generally ward based as part of a team, with a set number of patients to care for, first year doctors work as ‘inter-professional isolates’, caring for a variable number of patients, on different wards, often with limited senior support and are only transiently present prior to moving to their next job [52]. Some participants felt undermined by their nursing colleagues at times. As the ‘emergent identity’ of new doctors can be affirmed or disaffirmed by others in the workplace, friction can result if other healthcare professionals either do not see them as experienced enough to claim the authority they desire, or if their expectations of the novice doctors are too high [56].
Mistreatment
This study further highlights the pervasive issue of mistreatment of residents [57,58,59,60,61]. Experiencing or witnessing this behaviour negatively impacts on health and wellbeing, with reports of psychological distress, post-traumatic stress disorder, professional demotivation, burnout, dissatisfaction with the job and with training, and thoughts of leaving [57, 59, 60, 62,63,64,65,66,67]. Patient care is also adversely affected, with an increase in errors, disruption to collegiality and communication and diminished teamwork and morale [57, 59, 60, 62,63,64,65,66,67,68,69]. Mistreatment often remains unreported by residents [59,60,61, 64, 70,71,72]. Senior doctors from other departments were cited as perpetrators of mistreatment towards participants in this study, which has been reported previously [62, 73]. This reluctance to challenge seniors may indicate fear, or vulnerability in the medical hierarchy, or residents’ socialisation into the culture of medicine as transmitted by the hidden curriculum, with the acceptance of mistreatment as a way of signifying their worthiness for the profession [43, 64, 74,75,76]. Community of practice theory describes learners actively engaging with, and acquiring the identity associated with the community, who exert ‘a compelling social influence on its members’ [77,78,79]. Residents may assimilate the negative behaviours they are exposed to via the hidden curriculum and themselves become perpetrators, continuing a legacy of abusive behaviours [64, 80]. It is noteworthy that participants in this study appraised their job positively in retrospect. Earlier difficulties were downplayed to some extent and they evaluated the more challenging aspects of the year as valuable learning experiences. This may imply that they have acquired important experiences in order to work as doctors in the future, however it may also indicate an element of denial of difficulties encountered [23, 47, 81]. It has been suggested that doctors tend to trivialise or normalise their experiences of stress as a form of impression management to demonstrate professionalism [82] This attitude has the potential to maintain negative workplace culture for future residents [83].
Implications for practice
This study reveals overlapping temporal stages of the transition experience for new doctors. The themes that have been identified will inform stage-appropriate interventions to ease the transition. To mitigate the shock experienced in the initial stage of the transition, an undergraduate practice-based pedagogy such as Experience Based Learning (ExBL) would facilitate supported participation in clinical practice, and empower students to acquire intellectual, practical and affective capabilities gradually over time [84]. Anxiety and self-doubt characterised the early phase and support eased participants’ experience. Acknowledgement of the early transition period should include organisational expectation of initial underperformance, with increased early support and supervision [11, 85]. Consideration could be given to a period of overlap between incoming and outgoing interns, and faculty development to enable senior colleagues to support new doctors. Participants identified their nursing colleagues as key sources of early support. The contribution of nurses to new doctor socialisation, should be formally recognised and interventions designed to facilitate nurses to provide appropriate support [51, 85].
To mitigate the interprofessional tensions evident in this study, undergraduate and postgraduate education should include interdisciplinary involvement to promote role understanding, mutual respect, trust and collaboration and any barriers to collaboration identified and addressed [52, 86,87,88,89].
Focused interventions to tackle mistreatment of residents should target organisational, team and individual levels commencing with a zero tolerance policy of unprofessional behaviour, transparently monitored and enforced [67]. Education aimed at all levels in the organisation should include shared mental models as to what qualifies as mistreatment, facilitating the recognition and reporting of any problematic behaviour [64]. Residents need to feel psychologically safe in the clinical environment, to speak up or ask for assistance without fear of a hostile reaction [90]. Healthcare organisations must address issues within their own cultures and ensure that positive and supportive workplace relationships are fostered [91], including the education of senior residents who are responsible for supervising more junior doctors [92].
A culture that promotes student and resident wellness and resilience in undergraduate and postgraduate curricula should be a priority, with positive leadership, targeted interventions and the provision of resources promoting resilience and self-care. Interventions could include resident wellness programs, coaching, mentorship, and mindfulness [93, 94]. However, interventions focusing on the individual are only one aspect of promoting wellness. The work environment of doctors in their first year of practice should be re-evaluated. Residents should not be overburdened by high workload or long working hours, both of which were identified as issues by participants. Duty hour restrictions have been introduced by many countries to regulate working hours, however concerns have been raised regarding a resultant increase in work intensity due to pressure to complete workload with less time [23, 95]. A potential solution may be the introduction of an optimal patient caseload per resident, depending on specialty or patient complexity [96, 97] or strategies designed to minimise interruptions or the geographical distances residents cover [97].
Strengths and limitations
The use of interpretative phenomenological analysis, which is acknowledged as being a particularly effective methodology to explore experiences of existential importance to individuals [35], has resulted in a nuanced, in-depth understanding of the experience of transition from student to doctor in this study.
There are some potential limitations to consider. All participants were recruited from one intern training network. This has potential consequences for wider applicability, however, it is our intention that the reader may evaluate the transferability of conclusions, drawn in the context of this study, to other settings. To facilitate this a rich detailed description has been provided of the context, methodology and all research processes, and findings are discussed with reference to the extant relevant literature [98]. NC carried out all interviews. As a member of the faculty of the medical school aligned to the intern training network, she was known to many of the participants. Although she had no involvement in the intern programme, it is possible that this may have resulted in participants not being fully open in their accounts. Furthermore, her position as an ‘insider’ with prior experience of the subject of the inquiry, may have resulted in her failure to probe elements of participants’ experience sufficiently. It is possible therefore that aspects of the experience remain underexplored.
Conclusions
This study adds to the existing knowledge on the transition to clinical practice by using a phenomenological lens to provide an in-depth exploration of the experience of transition from student to doctor over the first year of practice. Overlapping stages in the transition experience were revealed, informing stage appropriate interventions to ease the difficulties encountered. It also highlights a suboptimal clinical learning environment with issues with workload, supervision, mistreatment by senior doctors, and both the positive contribution of nurses to doctors’ early socialisation and the diminution of inter-professional collaboration with time.
Availability of data and materials
The data analysed in this study are available from the corresponding author on reasonable request, subject to ethical approval.
References
Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter J, et al. A prospective cohort study investigating factors associated with depression during medical internship. JAMA Psychiat. 2010;67(6):557–65.
Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–5.
Teunissen PW, Westerman M. Junior doctors caught in the clash: the transition from learning to working explored. Med Educ. 2011;45(10):968–70.
Irish Medical Council. Your training counts: results of the national trainee experience survey. 2014.
Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, et al. How prepared are medical graduates to begin practice? a comparison of three diverse UK medical schools. Final report to GMC April 2008. 2008.
Martin D, Nasmith L, Takahashi SG, Harvey BJ. Exploring the experience of residents during the first six months of family medicine residency training. Can Med Educ J. 2017;8(1):e22–36.
Lempp H, Cochrane M, Seabrook M, Rees J. Impact of educational preparation on medical students in transition from final year to PRHO year: a qualitative evaluation of final-year training following the introduction of a new Year 5 curriculum in a London medical school…Pre-registration House Officer. Med Teach. 2004;26(3):276–8.
Sturman N, Tan Z, Turner J. “A steep learning curve”: junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Med Educ. 2017;17:92.
Prince K, Van de Wiel M, Van der Vleuten C, Boshuizen H. Junior Doctors’ Opinions about the Transition from Medical School to Clinical Practice: A Change of Environment. Educ Health (Abingdon). 2004;17(3):323–31.
Ackerman A, Graham M, Schmidt H, Stern DT, Miller SZ. Critical events in the lives of interns. J Gen Intern Med. 2009;24(1):27–32.
Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, et al. The transition from medical student to junior doctor: today’s experiences of Tomorrow’s Doctors. Med Educ. 2010;44(5):449–58.
Tallentire VR, Smith SE, Facey AD, Rotstein L. Exploring newly qualified doctors’ workplace stressors: an interview study from Australia. BMJ Open. 2017;7(8):e015890.
Facey AD, Tallentire V, Selzer RM, Rotstein L. Understanding and reducing work-related psychological distress in interns: a systematic review. Intern Med J. 2015;45(10):995–1004.
Levine RB, Haidet P, Kern DE, Beasley BW, Bensinger L, Brady DW, et al. Personal growth during internship: a qualitative analysis of interns’ responses to key questions. J Gen Intern Med. 2006;21(6):564–9.
de Lasson L, Just E, Stegeager N, Malling B. Professional identity formation in the transition from medical school to working life: a qualitative study of group-coaching courses for junior doctors. BMC Med Educ. 2016;16:165.
Chang LY, Eliasz KL, Cacciatore DT, Winkel AF. The transition from medical student to resident: a qualitative study of new residents’ perspectives. Acad Med. 2020;95(9):1421–7.
Davis-Floyd RE. Obstetric training as a rite of passage. Med Anthropol Q. 1987;1(3):288–318.
Veazey Brooks J, Bosk CL. Remaking surgical socialization: Work hour restrictions, rites of passage, and occupational identity. Soc Sci Med. 2012;75(9):1625–32.
Van Gennep A, Vizedom MB, Caffee GL. The rites of passage, trans. Chicago: University of Chicago Press; 1960.
Gordon L, Jindal-Snape D, Morrison J, Muldoon J, Needham G, Siebert S, et al. Multiple and multidimensional transitions from trainee to trained doctor: a qualitative longitudinal study in the UK. BMJ Open. 2017;7(11):e018583.
Colbert-Getz JM, Baumann S, Shaffer K, Lamb S, Lindsley JE, Rainey R, et al. What’s in a Transition? An Integrative Perspective on Transitions in Medical Education. Teach Learn Med. 2016;28(4):347–52.
Teunissen PW, Westerman M. Opportunity or threat: the ambiguity of the consequences of transitions in medical education. Med Educ. 2011;45(1):51–9.
Goodyear HM. First year doctors experience of work related wellbeing and implications for educational provision. Int J Med Educ. 2014;5:103–9.
Satterfield JM, Becerra C. Developmental challenges, stressors, and coping in medical residents: a qualitative analysis of support groups. Med Educ. 2010;44(9):908–16.
Hurst C, Kahan D, Ruetalo M, Edwards S. A year in transition: a qualitative study examining the trajectory of first year residents’ well-being. BMC Med Educ. 2013;13:96.
Stratta EC, Riding DM, Baker P. Ethical erosion in newly qualified doctors: perceptions of empathy decline. Int J Med Educ. 2016;7:286–92.
Illing JC, Morrow GM, Rothwell nee Kergon CR, Burford BC, Baldauf BK, Davies CL, et al. Perceptions of UK medical graduates’ preparedness for practice: a multi-centre qualitative study reflecting the importance of learning on the job. BMC Med Educ. 2013;13:34.
Monrouxe L, Bullock A, Cole J, Gormley G, Kaufhold K, Kelly N, et al. How prepared are UK medical graduates for practice? Final report from a programme of research commissioned by the General Medical Council; 2014. 2015.
Tallentire VR, Smith SE, Skinner J, Cameron HS. Understanding the behaviour of newly qualified doctors in acute care contexts. Med Educ. 2011;45(10):995–1005.
Nicholson N. A theory of work role transitions. Adm Sci Q. 1984;29(2):172–91.
Kramer M. Reality shock; why nurses leave nursing: Mosby. 1974.
Duchscher JEB. Transition shock: the initial stage of role adaptation for newly graduated Registered Nurses. J Adv Nurs. 2009;65(5):1103–13.
Duchscher JB. A process of becoming: The stages of new nursing graduate professional role transition. J Contin Educ Nurs. 2008;39(10):441–50.
Coakley N, O’Leary P, Bennett D. ‘Waiting in the wings’; Lived experience at the threshold of clinical practice. Med Educ. 2019;53:698–709.
Smith JA, Flowers P, Larkin M. Interpretative Phenomenological Analysis. Theory, Method and Research: Sage; 2009. p. 225.
Kuper A, Reeves S, Levinson W. An introduction to reading and appraising qualitative research. BMJ. 2008;337:a288.
Moustakas C. Phenomenological research methods. Thousand Oaks, London, New Delhi: Sage Publications; 1994.
Smith JA. Evaluating the contribution of interpretative phenomenological analysis. Health Psychol Rev. 2011;5(1):9–27.
King N, Horrocks C. Interviews in Qualitative Research. Los Angeles, London, New Delhi, Singapore, Washington DC: Sage Publications; 2010. p. 232.
10 QIPLV. NVivo qualitative data analysis Software. 2014.
Louis MR. Surprise and sense making: what newcomers experience in entering unfamiliar organizational settings. Adm Sci Q. 1980;25(2):226–51.
Van Hamel C, Jenner LE. Prepared for practice? A national survey of UK foundation doctors and their supervisors. Med Teach. 2015;37(2):181–8.
Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. BMJ. 2004;329(7469):770–3.
Baker K, Sen S. Healing medicine’s future: prioritizing physician trainee mental health. AMA J Ethics. 2016;18(6):604–13.
van Maanen J, Schein EH. “Toward a theory of organizational socialization ”. Research in Organizational Behavior. 1979. p. 209–64.
Paice E, Rutter H, Wetherell M, Winder B, McManus IC. A well supervised working environment may offset reduction in hours or a high work intensity. Med Educ. 2002;36:56–65.
Brown J, Chapman T, Graham D. Becoming a new doctor: a learning or survival exercise? Med Educ. 2007;41(7):653–60.
Cave J, Woolf K, Jones A, Dacre J. Easing the transition from student to doctor: How can medical schools help prepare their graduates for starting work? Med Teach. 2009;31(5):403–8.
Lempp H, Cochrane M, Rees J. A qualitative study of the perceptions and experiences of Pre-Registration House Officers on teamwork and support. BMC Med Educ. 2005;5(1):10.
Burford B, Morrow G, Morrison J, Baldauf B, Spencer J, Johnson N, et al. Newly qualified doctors’ perceptions of informal learning from nurses: implications for interprofessional education and practice. J Interprof Care. 2013;27(5):394–400.
Varpio L, Bidlake E, Casimiro L, Hall P, Kuziemsky C, Brajtman S, et al. Resident experiences of informal education: how often, from whom, about what and how. Med Educ. 2014;48(12):1220–34.
Milne J, Greenfield D, Braithwaite J. An ethnographic investigation of junior doctors’ capacities to practice interprofessionally in three teaching hospitals. J Interprof Care. 2015;29(4):347–53.
O’Connor P, O’Dea A, Lydon S, Offiah G, Scott J, Flannery A, et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016;28(3):339–45.
Weinberg DB, Miner DC, Rivlin L. Original research: “It depends”: medical residents’ perspectives on working with nurses. Am J Nurs. 2009;109(7):34–43.
Weller JM, Barrow M, Gasquoine S. Interprofessional collaboration among junior doctors and nurses in the hospital setting. Med Educ. 2011;45(5):478–87.
Sheehan D, Wilkinson TJ, Bowie E. Becoming a practitioner: workplace learning during the junior doctor’s first year. Med Teach. 2012;34(11):936–45.
Crutcher RA, Szafran O, Woloschuk W, Chatur F, Hansen C. Family medicine graduates’ perceptions of intimidation, harassment, and discrimination during residency training. BMC Med Educ. 2011;11(1):88.
Quine L. Workplace bullying, psychological distress, and job satisfaction in junior doctors. Camb Q Healthc Ethics. 2003;12(1):91–101.
Scott J, Blanshard C, Child S. Workplace bullying of junior doctors: cross-sectional questionnaire survey. N Z Med J. 2008;121(1282):10–4.
GMC, Council. GM. National training survey 2014—bullying and undermining. London: General Medical Council; 2014.
Cheng MY, Neves SL, Rainwater J, Wang JZ, Davari P, Maverakis E, et al. Exploration of Mistreatment and Burnout Among Resident Physicians: a Cross-Specialty Observational Study. Medical Science Educator. 2020.
Bradley V, Liddle S, Shaw R, Savage E, Rabbitts R, Trim C, et al. Sticks and stones: investigating rude, dismissive and aggressive communication between doctors. Clin Med. 2015;15(6):541–5.
Paice E, Aitken M, Houghton A, Firth-Cozens J. Bullying among doctors in training: cross sectional questionnaire survey. BMJ. 2004;329(7467):658–9.
Leisy HB, Ahmad M. Altering workplace attitudes for resident education (A.W.A.R.E.): discovering solutions for medical resident bullying through literature review. BMC Med Educ. 2016;16:127.
Rafaeli A, Erez A, Ravid S, Derfler-Rozin R, Treister DE, Scheyer R. When customers exhibit verbal aggression, employees pay cognitive costs. J Appl Psychol. 2012;97(5):931.
Porath CL, Erez A. Does rudeness really matter? The effects of rudeness on task performance and helpfulness. Acad Manag J. 2007;50(5):1181–97.
Illing J, Carter M, Thompson NJ, Crampton PES, Morrow GM, Howse JH, et al. Evidence synthesis on the occurrence, causes, consequences, prevention and management of bullying and harassing behaviours to inform decision-making in the NHS. 2013.
Porath CL, Erez A. Overlooked but not untouched: How rudeness reduces onlookers’ performance on routine and creative tasks. Organ Behav Hum Decis Process. 2009;109(1):29–44.
Billings ME, Lazarus ME, Wenrich M, Curtis JR, Engelberg RA. The effect of the hidden curriculum on resident burnout and cynicism. J Grad Med Educ. 2011;3(4):503–10.
Grover A, Appelbaum N, Santen SA, Lee N, Hemphill RR, Goldberg S. Physician mistreatment in the clinical learning environment. Am J Surg. 2020;220:276–81.
IMC. Your Training Counts An investigation of Trainee wellbeing and their experiences of clinical learning environments in Ireland 2017. Dublin: Irish Medical Council; 2019.
Paice E, Smith D. Bullying of trainee doctors is a patient safety issue. Clin Teach. 2009;6(1):13–7.
Koh NJ, Wagner R, Newton RC, Casey BR, Sun H, Weiss KB. Detailed Findings From the CLER National Report of Findings 2018. J Grad Med Educ. 2018;10(4s):49–68.
Vaidyanathan B. Professional socialization in medicine. Virtual Mentor. 2015;17(2):164.
Timm A. ‘It would not be tolerated in any other profession except medicine’: survey reporting on undergraduates’ exposure to bullying and harassment in their first placement year. BMJ Open. 2014; 4(7):e005140. Available from: http://europepmc.org/abstract/MED/25009133,http://europepmc.org/articles/PMC4091461?pdf=render,http://europepmc.org/articles/PMC4091461, http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=EBI&pubmedid=25009133,http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=EBI&pubmedid=25009133&action=stream&blobtype=pdf, https://doi.org/10.1136/bmjopen-2014-005140.
Crowe S, Clarke N, Brugha R. ‘You do not cross them’: Hierarchy and emotion in doctors’ narratives of power relations in specialist training. Soc Sci Med. 2017;186:70–7.
Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718–25.
Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185–90.
Kenny NP, Mann KV, MacLeod H. Role modeling in physicians’ professional formation: reconsidering an essential but untapped educational strategy. Acad Med. 2003;78(12):1203–10.
Kassebaum DG, Cutler ER. On the culture of student abuse in medical school. Acad Med. 1998;73(11):1149–58.
Bearman M, Lawson M, Jones A. Participation and progression: new medical graduates entering professional practice. Adv Health Sci Educ. 2011;16(5):627–42.
Thompson N, Corbett S, Welfare M. A qualitative study of how doctors use impression management when they talk about stress in the UK. Int J Med Educ. 2013;4:236–46.
Bernabeo EC, Holtman MC, Ginsburg S, Rosenbaum JR, Holmboe ES. Lost in transition: The experience and impact of frequent changes in the inpatient learning environment. Acad Med. 2011;86(5):591–8.
Dornan T, Conn R, Monaghan H, Kearney G, Gillespie H, Bennett D. Experience based learning (ExBL): clinical teaching for the twenty-first century. Med Teach. 2019;41:1–8.
Kilminster S, Zukas M, Quinton N, Roberts T. Preparedness is not enough: understanding transitions as critically intensive learning periods. Med Educ. 2011;45(10):1006–15.
Jain A, Luo E, Yang J, Purkiss J, White C. Implementing a nurse-shadowing program for first-year medical students to improve interprofessional collaborations on health care teams. Acad Med. 2012;87(9):1292–5.
Shafran DM, Richardson L, Bonta M. A novel interprofessional shadowing initiative for senior medical students. Med Teach. 2015;37(1):86–9.
Barrow M, McKimm J, Gasquoine S. The policy and the practice: early-career doctors and nurses as leaders and followers in the delivery of health care. Adv Health Sci Educ. 2011;16(1):17–29.
Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90(1061):149.
Caverzagie KJ, Goldenberg MG, Hall JM. Psychology and learning: the role of the clinical learning environment. Med Teach. 2019;41(4):375–9.
Wiese A, Kilty C, Bennett D. Supervised workplace learning in postgraduate training: a realist synthesis. Med Educ. 2018;52(9):951–69.
Kilminster S, Cottrell D, Grant J, Jolly B. AMEE Guide No. 27: Effective educational and clinical supervision. Med Teach. 2007;29(1):2–19.
Shanafelt TD, Noseworthy JH, editors. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. In Mayo Clinic Proceedings, vol. 92, no. 1. Elsevier; 2017. p. 129–46.
Sharp M, Burkart KM. Trainee wellness: why it matters, and how to promote it. Ann Am Thorac Soc. 2017;14(4):505–12.
Pan TY, Fan HS, Owen CA. The work environment of junior doctors: their perspectives and coping strategies. Postgrad Med J. 2016;93:414–9.
Johns MME, Wolman DM, Ulmer C. Resident duty hours: enhancing sleep, supervision, and safety. Washington DC: National Academies Press; 2009.
Thanarajasingam U, McDonald FS, Halvorsen AJ, Naessens JM, Cabanela RL, Johnson MG, et al. Service census caps and unit-based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–7.
Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handb Qual Res. 1994;2(163–194):105.
Acknowledgements
None.
Funding
The study was funded by the South Intern Training Network, Cork.
Author information
Authors and Affiliations
Contributions
NC collected the data, analysed the data, wrote the first draft and edited it following feedback from DB and POL. POL analysed the data, and provided critical review and editing of manuscript DB conceived the study, analysed the data, and provided critical review and editing of manuscript. All have approved the final draft of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the guidelines and regulations contained in the Declaration of Helsinki. This study was approved by the Social Research Ethics Committee, University College Cork. All participants gave their informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Coakley, N., O’Leary, P. & Bennett, D. Endured and prevailed: a phenomenological study of doctors’ first year of clinical practice. BMC Med Educ 23, 109 (2023). https://doi.org/10.1186/s12909-023-04059-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04059-w