Abstract
Background
A better understanding of medical students’ competencies about antimicrobial resistance and their use could facilitate a more effective education for them as future prescribers. The aim is to explore the educational impact of an elective course on medical students’ knowledge, perception, and attitude toward antibiotic resistance and use.
Methods
Between December 2021 and January 2022, when a 2-credit hours elective course was designed and implemented, this interventional study was conducted. The primary outcome measure was the change in medical students’ knowledge, perception, and attitude about antibiotic resistance and use. Using a pre-post course questionnaire, this outcome was assessed. The secondary measure included students’ perception of the course; assessed by a post-course online survey.
Results
Among the 50 enrolled students, the total knowledge score had significantly increased after the course with 95% CI After the course, with medium effect size ( Cohen’s d= -0.7 ) the participants’ mean ± SD total perception and attitude scores had significantly increased (52.38 ± 5.53 vs. 56.84 ± 5.86) respectively, (p = 0.000) with large effect size (( Cohen’s d= -0.8) There was a significant positive correlation between the total knowledge, attitude, and perception after the course (r = 0.542, p < 0.01). The mean ± SD of the overall course satisfaction was 4.20 ± 0.94. out of 5.
Conclusion
Medical students’ knowledge, perceptions, and attitudes towards antimicrobial prescription have been improved after the elective antibiotic prescribing etiquette course. Elective courses could offer a great opportunity to enable the students to understand the extent of the problem, stand on the facts, and take responsibility for the antibiotic resistance crisis.
Trial registration
NA
Similar content being viewed by others
Background
Currently, antibiotics are routinely misused and overused, hastening the development of bacterial resistance and resulting in problems such as extended hospital stays, increased medical expenses, and death [1]. We are in an urgent need to modify the way antibiotics are prescribed and used [2]. Students’ education could lead to well-informed adults appreciating the risk of increased antibiotic resistance and raising concerns about the over-prescription of antibiotics to limit such practices [3, 4]. The situation is of more concern when it comes to medical students. As citizens and potential prescribers, they have a dual role in this crisis prevention[5, 6].
In our institution, as is the case in many other medical schools in low-middle income countries, antibiotic use knowledge is developed during medical training, including lectures on the basics of antibiotic treatment and textbooks on infectious diseases. However, many physicians continue to prescribe antibiotics inappropriately [7]. This can be owed to the extent to which the problem is realized within the facility and its incorporation into the routine practice, and leadership support, [89].
From an educational perspective, the current teaching approaches and textbooks do not adequately prepare medical students for this task [9,10,11]. Many limitations do exist (i) the learning process is passive and students are not encouraged to develop an adequate level of critical thinking [12]; (ii) students memorize theoretical medical concepts, rather than learning to solve the practical problems that arise in medical practice; (iii) students focus on clinical situations encountered in hospitals, but not in primary care; (iv) students focus on a single patient, whereas, in real life, they often have to manage several patients simultaneously.
Many researchers. investigated the knowledge, attitude, and practice toward antibiotic use among medical students [9, 13,14,15]. Many teaching opportunities were designated juniors as problem-based learning, role-play games, round tables, musicals as well as e-learning [10].
In the current curriculum, the delivery of many competencies about the rational use of antibiotics is missed. It is taught in the form of separate topics in microbiology, pharmacology, public health, and clinical sciences. No separate theme for antimicrobial resistance exists in the current curricula. Comprehensive evaluations of antimicrobial stewardship teaching programs and overall effectiveness in undergraduate medical institutions are still few and sparse [16, 17]. As far as we know, not enough data are available about the impact of antibiotic use in educational courses in middle-income countries like Egypt. Given the good educational impact of elective courses on students’ learning [18], we designed an elective course titled “antibiotic prescribing etiquette” to help medical students better understand their role in combating the antimicrobial resistance crisis. We hypothesized that this course could improve the comprehension of medical students about their role in the proper antibiotic prescription process. In this study, we aimed to explore the educational impact of this course on medical students’ knowledge, perception, and attitude toward antibiotic resistance as well as proper antibiotic use and prescription. We anticipated the findings may help curriculum designers to consider adding this topic to the main curriculum.
Methods
This intervention prospective study was conducted in the Faculty of Medicine, Zagazig University; a leading medical school in Egypt from December 2021 to January 2022.
Study population
We used a purposive sample in this study that included all the enrolled students in this elective course (50 students) with a 100% response rate. Informed written consent was collected from each student.
The enrolment of medical students: This elective course is delivered to third-year medical students. The course announcement and communication occurred via the official online platform; Microsoft teams.
At the time of course enrollment, our students have already studied microbiology, pharmacology, introduction to clinical practice, and infection control courses.
Study intervention “course description”
“Antibiotic prescribing etiquette” is a 2-credit hours elective course, that was delivered over 2-weeks duration. It was designed and prepared by experts in antimicrobial resistance, infection control, and medical education, this followed the methodology mentioned earlier for course design [10, 19,20,21]. First were revised earlier published reports about the selected topic [9, 13,14,15], revised the current curriculum, revised the national academic standards for medical students (NARS) 2017 [22], and the final course reports delivered from all related modules that were given in our faculty and are related to the antibiotic resistance topic. The course was designed with the aim to improve the awareness of medical students about antimicrobial resistance and identify how they could apply the proper prescription rules. The course specification was revised by the official MBBCh curriculum committee to revise the objectives’ alignment with the teaching methods to achieve the course goals, check the course quality and approve the suitability to teach the course as an elective course.
Learning outcomes and teaching methods: Course directors defined a list of learning outcomes (Los) that conveys what students would be able to do after completing the course, they were distributed upon the 3 learning domains: knowledge, attitude, and skills, Table 1.
We considered making the learning process attractive, exciting, and challenging using different teaching and learning methods [20]. This included 2 interactive sessions: an online and a face-to- face one, and 2 recorded lectures, and a reflective practice assignment. The latter is a health education message directed to one of the key players involved in the antibiotic prescription process. The students were requested to design and record a 2-minute multimedia file of their message.
Table 1 presents the course Los, the teaching activities, and the type of sessions in the three domains: knowledge, attitude, and skills. Course flow is illustrated in Fig. 1.
Learning environment
The course was developed for use in a class of 30–50 students, which was then divided into groups of three to five students for a small-group activity and the submission of the final assignment. We presented the session in a classroom equipped with a computer and projector, and students received handouts to guide them through the small-group work. The online session and the recorded lectures were conducted via the educational platform; Microsoft teams.
Criteria to pass the course included attendance, active participation, and the health education message. The latter was evaluated and scored according to a constructed checklist. The best 3 assignments were awarded for their creativity.
*Session type for knowledge and attitude domains were interactive sessions, lectures, and reflective performance assignment. For skills domain interactive sessions and the reflective performance assignment were used.
Outcome measures
The primary measure was the change in the medical students’ knowledge, perception, and attitude about antibiotic resistance and use. This was measured by a pre-post course questionnaire that was designed after reviewing literature [9, 19, 23, 24], revised, piloted, and validated.
The content validity of the questionnaire was assessed in terms of necessity and relevance, by 10 professional experts in the field. The necessity of questions was scored on a 3-point scale from (1–3) " not necessary, useful but not necessary, necessary” respectively. The relevance of the items was assessed on a scale of 1 to 4 ; [1: not relevant- 2: somewhat relevant and needs some revision, 3: quite relevant, 4: highly relevant]. Both the Content Validity Ratio (CVR) and the Scale Content Validity Index (S-CVI) for the questionnaire were calculated to be acceptable values of 0.83 and 0.87, respectively [25, 26].
It was divided into 4 sections: (1) demographics including age, gender, and motive to join the course. (2) prior experience in antibiotic use, as well as the source of information. (3) knowledge-related items. (4) perceptions and attitude. The post-course questionnaire included the same items mentioned in the pre-course survey in the knowledge section, as well as in the perception and attitude section.
The secondary measure included students’ perception of the elective course. At the end of the course, the students were requested to fill in an online survey form [10, 19]. This encompassed their interest in the course (3 items), as well as their satisfaction with the course design and implementation (7 items). Open-ended questions (3 items) were included: what they liked best, the most they disliked, and a suggestion for improvement.
Statistical analysis
Data were summarized and analyzed using SPSS 23 by calculating frequency, percentage, mean, and SD. Paired t-test and Wilcoxon Sign Ranks test were computed for the paired continuous data and McNemar’s test was for the paired nominal data to find the difference between the pretest and posttest results. Pearson’s correlation coefficient was calculated to determine the correlation between students’ satisfaction and the total knowledge,attitude, and perception scores. The significant level was determined as p < 0.05.
The knowledge section, and the perception and attitude section each composed of 22 items. The total score ranged from 22 to 66. The score was calculated on a 3-point Likert scale: Agree, gets 3 points, neutral 2 points and disagree 1 point. Ten items were calculated by reverse coding. This was applied to 3 items in the knowledge section, and 7 items in the attitude and perception section.
The effect size of our educational intervention on total knowledge, perception and attitude was assessed using Cohen’s term d by taking the difference between the means in the pretest and posttest for the means and divided it by the standard deviation of the pretest for both domains.
Results
The course was delivered to 50 3rd year medical students: (26, 52%) males, and (24, 48%) females. Their mean age was 20.36 ± 0.63 years. When asked about their motive for joining the course, (35, 70%) were interested in the topic, (12, 24%) were attracted to the course title, and (3, 6%) joined because it was the only available course for them at the time of registration. Students’ personal experience in antibiotic use is summarized in Table 2.
The useful sources to get information about antibiotic use and resistance were arranged in descending order as follows: Formal lectures (84%), textbooks (78%), new technology such as the internet, smartphone applicants, etc. (72%), medical journals (58%) and social media (58%).
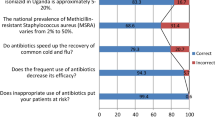
The total knowledge score of the participants has significantly increased after the course compared to the pre-course score; 48.06 ± 6.12 and 52.35 ± 5.91 respectively, p = 0.000. Table 3 shows the detailed knowledge items. The total perception and attitude scores of the participants significantly increased after the course (52.38 ± 5.53 & 56.84 ± 5.86) respectively, the mean difference was - 4.29 ± 5.04 with 95% CI (-5.75 to -2.82) (p = 0.000). Table 4 shows the detailed perception and attitude items.
The effect size of our educational intervention on total knowledge, perception and attitude equals - 0.7 for total knowledge which is considered as medium effect size and - 0.8 for total attitude and perception, that is a large effect size.
After the course, we reported a significant positive correlation between the total knowledge score and the attitude and perception score (r = 0.542, p < 0.01).
Perception of the students about their educational experience through the course
Out of the 50 students, 54% believed that it should be part of the main curriculum, most of them would go for an advanced course on the same topic (90%) and 94% would recommend the course to colleagues. The course met the expectations of 62% of the students. About 30% of the students recommended adding more details about antibiotic uses and types in cooperation with the pharmacology department. Following, more interactive face-to-face sessions were suggested by (14%), and be an obligatory module by (8%).
The overall satisfaction with the course was 4.20 ± 0.94. out of 5. A positive significant correlation was present between students’ satisfaction and total attitude and perception in post-test (r = 0.300, p < 0.05).
Discussion
Improving prescribers’ education has lately been advocated to ensure safer prescribing and optimum antibiotic use [27]. We aimed to study the impact of an elective educational course on prescription-related competencies among undergraduate medical students. The study disclosed the statistically significant increase in the medical students’ knowledge, attitude, and perception scores after attending the course. The majority of the students were interested and satisfied with the course.
First of all, we owe the appropriateness of this course mainly to the fact that students attended electively without being bothered by exams or any stressful evaluation; most of them (94%) joined either because they were attracted to or were interested in the topic. Medical students perceive electives as a valuable experience, allowing them to tailor learning skills and qualifying them to early differentiate during medical training [28].
The course improved the medical students’ knowledge with medium effect size of -0.7. It added information regarding some common terminology in antimicrobial resistance; extended spectrum B lactamases (ESBL), extended resistant (XDR) bacteria, and pan drug-resistant bacteria. Those 2 terms, in specific, were addressed in the interactive sessions ; storytelling, and case scenarios. As previously reported [29,30,31,32,33,34], the course enhanced their awareness that antimicrobial resistance is a national public health threat with a serious impact that exists in their local hospitals as well.
Deficiencies in the medical school curricula, including fundamental concepts of antimicrobial usage have been reported in studies conducted in different countries such as the USA, China, Colombia, Singapore, and Italy [9]. In the current report, the course succeeded to bring attention that many drivers can lead to antimicrobial resistance. Unlike how the antibiotic resistance topic is taught in the main curriculum, in this course it was delivered as a single theme that covered both medical and non-medical contributing factors. In addition, as previously recommended [10], we used many activities to address knowledge deficiency. We believe that this helped to some extent in filling the students’ knowledge gaps.
This study showed significant improvement in the perception and attitude scores with large effect size of -0.8. After the course, students thought they are sufficiently prepared to interpret antibiograms and get the treatment information needed from reliable sources. Published reports emphasize how crucial it is to educate physicians about antibiograms. Though important, this point is not addressed in the undergraduate medical curriculum in our institution.
Students showed a significant improvement in their perception of proper antibiotic prescription indications, dosage, and duration. Previous reports recommended the delivery of properly designed educational courses targeting antibiotic use specific items in the three learning domains [35]. Not a small percentage of students in our study believed that improvement of symptoms is an indication for stopping the antibiotic course, which was considerably alarming. Following the course, a statistically significant shift in their perception was noticed. In concordance with this, Okedo-Alex S et al., [36] reported that 22% of the respondents stopped the course of antibiotics when they felt better. Increasing knowledge and improving the perception and attitude from the pretest to post-test with medium and large effect size respectively can be considered as an indicator of thevaluable impact of our work. .
Thus this elective course could be recommended for wider scale application ; moreover, it could be adapted to the obligatory courses for undergraduate students keeping the positive points feedback and opportunities for improvement in mind for future implementation rounds.
The course helped students to recognize and promote the role of different health team members in proper antibiotic use, from that notion came the idea of the assignment. We thought that delivering messages to targeted groups would help students understand the concept of an interprofessional environment, in which doctors and others work within complex clinical groups promoting collaborative practice among various professionals. Teaching others gives information retention by 90% [37]. Using videos added more dynamism; it not only gave them the opportunity to integrate, but also ensured the active participation of each student.
Ortega-Paredes et al., 2022 reported, about 60% agreed with the development of novel antibiotics as a good solution for the problem [38]. After the course, the students showed more confidence that the development of new and effective drugs will not keep pace with the growing rate of antibiotic resistance and hence this increased their awareness of the preventive methods of the antibiotic resistance problem.
Earlier reports [24, 39] recommended medical schools should devote more effort to teaching proper antibiotic usage. More than half of the respondents thought that the course should be included within the main curriculum and almost all would recommend the course to colleagues. The majority of the students were satisfied with the course, their satisfaction positively correlated with their perception and attitude. This was evident in their interest to join an advanced course on the same topic (90%).
Limitation of the study
Many limitations existed that could affect the presented results. The course was of short length; a longer duration may give better results. Lacking a control group was a limiting factor. Although, this type of study design is accepted to be used in case of evaluation of a training program/course where the group is selected in a non-random way, and the randomization is impractical, however, it has many potential consequences, for instance, conveying the improved post-test results to other outside influencers. In the current study, the main outcomes were the knowledge and attitudes of students. To what extent medical students would translate these beliefs into effects in future clinical practice was not addressed. Further research is needed to tackle this domain.
Conclusion
Our findings suggest that medical students’ knowledge, perceptions, and attitudes towards antimicrobial prescription have been improved after the elective antibiotic prescribing etiquette course.
This study affirmed the potentials elective courses could offer in the medical school curriculum. The investigated course provided a great opportunity to enable the students to understand the extent of the problem, stand on the facts, and take responsibility towards the antibiotic resistance crisis. However, further improvements to the course content may be considered in future research to include how to deal with patient expectations, how to manage specific types of infections, etc.
Availability of data and materials
All data generated or analysed during this study are included in this published article (Supplementary file).
References
-Davey PG, Marwick C. Appropriate vs. inappropriate antimicrobial therapy. Clin Microbiol Infect. 2008 Apr;14:15–21.
Organization -WorldH, antibiotic resistance. 2018. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Accessed 2 Feb 2022.
Mayi BS, Mainville M, Altaf R, Lanspa M, Vaniawala S, Ollerhead TA, Raja A. A crucial role for Antimicrobial Stewardship in the midst of COVID-19. J Microbiol Biol Educ. 2021;22:22.
Rosenbaum L. No cure without care—soothing science skepticism. N Engl J Med. 2021;384:1462–5.
Leekha S, Terrell CL, Edson RS. General principles of antimicrobial therapy. InMayo Cin Proc. 2011;86(2):156–67.
-Simpson SA, Wood F, Butler CC. General practitioners’ perceptions of antimicrobial resistance: a qualitative study. J Antimicrob Chemother. 2007;59:292–6.
Van den Broek d’Obrenan J, Verheij J, Numans TJ, Van der Velden AW. Antibiotic use in Dutch primary care: relationship between diagnosis, consultation and treatment. J Antimicrob Chemother. 2014;69(6):1701–7.
-. El-Sokkary RH, Negm EM, Othman HA, Tawfeek MM, Metwally WS. Stewardship actions for device associated infections: an intervention study in the emergency intensive care unit. J Infect Public Health. 2020 Dec;13(12):1927–31.
-Higuita-Gutiérrez LF, Roncancio Villamil GE, Jiménez Quiceno JN. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: a cross-sectional descriptive study. BMC Public Health. 2020;20(1):1861.
-Marvasi M, Casillas L, Vassallo A, Purchase D. Educational Activities for students and Citizens supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics. 2021;10(12):1519.
-Miles S, Kellett J, Leinster SJ. Medical graduates’ preparedness to practice: a comparison of undergraduate medical school training. BMC Med Educ. 2017 Dec;17(1):1–9.
Schmidt HG, Wagener SL, Smeets GA, Keemink LM, Van der Molen HT. On the use and misuse of lectures in higher education. Health Prof Educ. 2015;1(1):12–8.
Health Education England annual report. Tackling antimicrobial resistance: educational priorities. London, UK; 2018. https://www.hee.nhs.uk/sites/default/files/documents/Tackling%20antimicrobial%20resistance%20-%20educational%20priorities%20report.pdf. Accessed 2 Feb 2022.
-Eley CV, Young VL, Hayes CV, McNulty CAM. Evaluation of an e-Learning platform for educators to improve education around infection prevention and antibiotics. Technol Pedagog Educ. 2019;28:485–501.
Manoj K, Gupta C, Vohra P, Raghav P. Assessment of knowledge, attitudes, and practices about antibiotic resistance among medical students in India. J Family Med Primary Care. 2019;8(9):2864.
Courtenay M, Lim R, Castro-Sanchez E, Deslandes R, Hodson K, Morris G, Reeves S, Weiss M, Ashiru-Oredope D, Bain H, et al. Development of consensus-based national antimicrobial stewardship competencies for UK undergraduate healthcare professional education. J Hosp Infect. 2018;100:245–56.
-McMaster D, Courtenay M, Santucci C, Davies AP, Kirby A, Seddon O, Price DA, Barlow G, Lim FH, Davies BS, et al. Consensus-based antimicrobial resistance and stewardship competencies for UK undergraduate medical students. JAC-Antimicrob Resist. 2020;2:dlaa096.
-Stys D, Hopman W, Carpenter J. What is the value of global health electives during medical school? Med Teach. 2013;35(3):209–18.
Khalil MK, Elkhider IA. Applying learning theories and instructional design models for effective instruction. Adv Physiol Educ. 2016;40(2):147–56.
Gauthier TP, Sherman EM, Unger NR. An elective course on antimicrobial stewardship. Am J Pharma Educ. 2015;79(10):157.
-Agarwal A, Wong S, Sarfaty S, Devaiah A, Hirsch A. Elective courses for medical students during the preclinical curriculum: a systematic review and evaluation. Med Educ Online. 2015;20:26615.
National Authority for Quality Assurance and Accreditation of Education- Egypt, National Academic Reference Standards- NARS forMedicine. 2017. https://admin.naqaae.eg/api/v1/archive/download/4718. Accessed 2 Jan 2022.
McGee EU, Pius M, Mukherjee K. Assessment of structured classroom debate to teach an antimicrobial stewardship elective course. Curr Pharm Teach Learn. 2020;12(2):220–7.
-Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-Cochran R, Srinivasan A, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis. 2013 Sep;57(5):631–8.
-Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28:563–75.
Polit DF Beck CT. Nursing Research: Principles and Methods. 7th Ed. Philadelphia: Lippincott Williams & Wilkins; 2004.
-Gharbi M, Moore LS, Castro-Sánchez E, Spanoudaki E, Grady C, Holmes AH, et al. A needs assessment study for optimising prescribing practice in secondary care junior doctors: the antibiotic Prescribing Education among doctors (APED). BMC Infect Dis. 2016 Dec;16(1):1–0.
-Ramalho AR, Vieira-Marques PM, Magalhães-Alves C, et al. Electives in the medical curriculum – an opportunity to achieve students’ satisfaction? BMC Med Educ. 2020;20:449.
-Nogueira-Uzal N, Zapata-Cachafeiro M, Vázquez-Cancela O, López-Durán A, Herdeiro MT, Figueiras A. Does the problem begin at the beginning? Medical students’ knowledge and beliefs regarding antibiotics and resistance: a systematic review. Antimicrob Resist Infect Control. 2020 Dec;9(1):1–6.
Dyar OJ, Hills H, Seitz LT, Perry A, Ashiru-Oredope D. Assessing the knowledge, attitudes and behaviors of human and animal health students towards antibiotic use and resistance: a pilot cross-sectional study in the UK. Antibiotics. 2018;7(1):10.
-Saleem Z, Azmi Hassali M, Hashmi F, Azhar F, Mubarak R, Afzaal A, et al. Medical and pharmacy students’ knowledge, attitude and perception concerning antimicrobial use and resistance in Pakistan. Pharm Edu. 2019;19:199–205.
-Thriemer K, Katuala Y, Batoko B, Alworonga JP, Devlieger H, Van Geet C, et al. Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS ONE. 2013;18(2):e55495.
García C, Llamocca LP, García K, Jiménez A, Samalvides F, Gotuzzo E, et al. Knowledge, attitudes and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in Lima Peru. BMC Clin Pharmacol. 2011;11(1):1–8.
-Meher BR, Srinivasan A, Vighnesh CS, Padhy BM, Mohanty RR. Factors most influencing antibiotic stewardship program and comparison of prefinal-and final-year undergraduate medical students. Perspect Clin Res. 2020;11(1):18.
-El-Sokkary R, Kishk R, Mohy El-Din S, Nemr N, Mahrous N, Alfishawy M, Morsi S, Abdalla W, Ahmed M, Tash R. Antibiotic use and resistance among prescribers: current status of knowledge, attitude, and practice in Egypt. Infect Drug Resist. 2021;25:1209–18.
-Okedo-Alex I, Madubueze UC, Umeokonkwo CD, Oka OU, Adeke AS, Okeke KC. Knowledge of antibiotic use and resistance among students of a medical school in Nigeria. Malawi Med J. 2019 Jun;31(2):133–7.
-The learning pyramid. Does it point teachers in the right direction?. Lalley JP, Miller RH. Education 2007;128:64e79.
Ortega-Paredes D, Larrea-Álvarez CM, Torres-Elizalde L, de Janon S, Vinueza-Burgos C, Hidalgo-Arellano L, Šefcová MA, Molina-Cuasapaz G, Fernandez-Moreira E, Larrea-Álvarez M. Antibiotic resistance awareness among undergraduate students in Quito, Ecuador. Antibiotics (Basel). 2022;11(2):197. https://doi.org/10.3390/antibiotics11020197.
-Heaton A, Webb DJ, Maxwell SR. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66:128–34.
Acknowledgements
We acknowledge the technical support offered by the curriculum committee at Zagazig University, mainly Prof. Amira Waly. This helped the professional delivery of the elective course “Antibiotic prescribing etiquette”.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors didn’t receive any fund.
Author information
Authors and Affiliations
Contributions
RE, RT SB, YEdesigned the study. RE, RT designed the elective course. RE, RT, SB delivered the elective course. RE, RT, SB designed data collection tools. SB collected the data. OE validated the data collection tool and analyzed the collected data. RE, RT, YE, and OE interpreted the collected data. All authors participated in writing the manuscripts, preparing, and approving the final form.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board (IRB) Committee of Zagazig Faculty of Medicine no ZU-IRB # 9253/25-1-2022 approved the current work. Informed consent was obtained from all the participants for participation in the study. All methods were carried out in accordance with relevant guidelines and regulations and Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Data collected from the participants before the course
Additional file 2.
Data collected from the participants after the course
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
El-sokkary, R.H., Badran, S.G., El Seifi, O.S. et al. “Antibiotic prescribing etiquette” an elective course for medical students: could we recruit potential physicians to fight resistance?. BMC Med Educ 23, 8 (2023). https://doi.org/10.1186/s12909-022-03949-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03949-9