Abstract
Background and objectives
The purpose of this study was to determine the outcomes of a two- week US-Sino Family Medicine Leadership Symposium for medical educators from China and how participants have integrated their learning into their teaching and practice of medicine.
Methods
Teaching topics emphasized principles of family medicine, teaching methods, assessment, and curriculum development. Each cohort received a wide range of practical, didactic and hands-on learning experiences. Online surveys were distributed anonymously to participants from the 2013–2019 cohorts to assess learner opinion and learner behavior change as a result of the leadership symposium. Quantitative measures assessed their level of integration of the topics into teaching and clinical practice and their satisfaction in the areas of teaching and leadership. They were also asked to provide qualitative feedback regarding incorporation of the content into their work.
Results
The survey response rate was 47.6% (39/82). Respondents stated that they incorporated topics such as basic interviewing skills and information on the patient-centered medical home into their teaching in China. The most applied clinical skills they were able to incorporate into their clinical environment in China included: Breaking Bad News, Simulations Sessions with practice, One-Minute Preceptor, and Interprofessional Education.
Conclusions
Results indicate that participants have demonstrated behavior changes that have led to the incorporation of the content into teaching and clinical practice. We demonstrated effectiveness of the curriculum in cultivating the teaching and practice of family medicine. The program appears to be a positive experience that has led to embracement of the roles as trainer and leader. 100% of the participants who completed the survey felt that the program improved patient confidence in their ability as a family doctor. Future assessment on barriers to their progress as teachers and leaders in family medicine would be helpful to explore.
Similar content being viewed by others
Background
Since 2006, China has been strengthening their primary care workforce by training family medicine doctors [1,2,3]. That year, a nationwide family medicine training base was organized and evaluated by China’s Ministry of Health and sought to improve care at the grassroots level by growing community health centers and the practitioners to work in them [1]. Up until then, Chinese medical colleges tended to exclude clinical practice training in family and community medicine [4, 5]. With its increasing population, burgeoning economic development, and demands for better health care, China recognized the need to adapt the “new medical model of biology-psychology-society and to meet tertiary health care needs.” [4] China continues to work toward their goal of establishing a robust primary care network, but there have been challenges in recognizing the roles and importance of family doctors as well as standardizing the content and quality of training [6, 7]. Patient satisfaction and trust have been areas of concern in China and the lack of doctor-patient communication and shared decision-making contribute to this [8, 9]. There has been a need to develop more community based primary care-oriented curricula [10, 11] and increase exposure to family medicine and family medicine role models to have a positive impact on the profession of family medicine and recruitment to the specialty [10]. In order for family medicine to have a sustainable future, trainers need practical education on how to: ensure safe and effective patient care through training, teach and facilitate learning, enhance learning through assessment, and support and monitor educational progress [12].
For the past 12 years, the University of Nebraska Medical Center (UNMC) Department of Family Medicine has partnered with universities in China to develop family medicine faculty. Medical foreign exchange programs exist [2, 5] between family medicine departments in China and the US, as well as collaborations between China and other countries, however we could not find any publications that have studied outcomes of these collaborations. Our two-week US-Sino Leadership Development Symposium was created for teaching physicians from China to travel to UNMC to build educational and leadership capacity in family medicine, foster the continued development of family medicine in China, and prepare them to address the health needs of their communities. Several exchanges have been done over the years with our faculty also traveling to China on many occasions.
Methods
Curriculum
After direct observation, review of the family medicine curriculum in China, and surveying the needs of the Chinese faculty, we chose to address topics that would help the Chinese faculty develop curricula to nurture principles of family medicine in their learners (comprehensive, compassionate, collaborative, coordinated, patient-centered care), particularly the humanistic aspects that are characteristic of family medicine. Initially, these concepts were new and unpracticed. Authors of a Lancet article on the quality of primary care in China appear to be in agreement and recommended that “training should prepare students to work in interprofessional teams, and emphasis should be placed on the importance of doctor–patient communication, which for example includes empathy and shared decision making to build trust between patients and primary care providers [13].” We also recognized contrasts in how content was delivered in the US vs China. Chinese medical colleges used strict lectures and laboratory classes to deliver content [4], though over the years it was observed that PBL instruction was introduced and now has become more widely used in teaching.
Participants of our US-Sino Leadership Program completed educational sessions ranging from basic interviewing skills and population health, to physician leadership. Other topics introduced contemporary methods of teaching, assessment, curriculum development, and collaborative care. The format included inter-departmental lectures in small groups, interactive case presentation and discussion of patients, role playing, simulation training, and demonstrations of procedures. Additionally, there were shadowing opportunities to observe US family medicine physicians on the inpatient teaching service and ambulatory clinics using the strategies and techniques being taught, attendance of teaching day (resident teaching day), and presentation of a final project in which the participants demonstrated the knowledge and skills they attained and described how they would incorporate it into their teaching and/or clinical environment in China. Table 1 illustrates a typical two-week agenda for the leadership symposium.
Participants
Participants in the Symposium were health care professionals and administrators in China who had an interest in becoming future leaders in educational and care delivery models. Many were in the mid-career phase. Some originally worked in other specialties but were being retrained as family doctors due to China’s efforts in growing their primary care workforce. Most were already practicing family physicians or GP’s working in community health centers, where they reported seeing an average of 60 patients per day and spent approximately one day per week (8 hours) teaching.
Measures
Our project assesses the outcomes of the two-week US-Sino Family Medicine Leadership Program. To date, seven cohorts (n = 82) participated from 2013 to 2019. The UNMC Institutional Review Board deemed this project exempt.
In September 2019, an online anonymous survey (translated to Mandarin) was administered to all past participants (n = 82) of the US-Sino Leadership Symposium regarding their experience. Using Kirkpatrick’s four level approach [14] as a model for evaluating our learner outcomes, we assessed 1) learner satisfaction, and 2) if and how they have applied their knowledge to their teaching and/or clinical environment. In addition, a question regarding improvement in interpersonal trust in the doctor-patient relationship was included.
Results
Thirty-nine of 82 participants responded to the survey (47.6%; Table 2). The majority of respondents (64.1%) were female, the average age was 38.7 years (SD = 5.1) and they have been in practice for an average of 14.5 years (SD = 6.6). On average, they spend 26 hours per week (SD = 13.0) seeing patients and 7.9 hours per week teaching students and/or residents. Table 2 includes a description of our sample.
Respondents incorporated most skills and concepts into their current teaching and/or practice. The most frequently applied teaching skills included Basic Interviewing Skills and information about Patient-Centered Medical Homes; the most applied clinical skills included Breaking Bad News, Simulations Sessions with practice, One-Minute Preceptor, and Interprofessional Education.
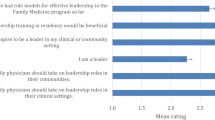
Table 3 illustrates skills that the participants were able to incorporate into teaching and clinical practice when they returned to China. Most attendees were Satisfied or Very Satisfied with their progress as a teacher and a leader of family medicine (see Fig. 1). All respondents (100.0%) felt that the program improved patient confidence in their ability as a family doctor(see Fig. 2).
Discussion
The US-Sino Leadership Symposium was well-received, and participants incorporated their learning into their teaching and/or clinical practice. It appears to be a positive experience that has led to participants’ embracement of their roles as trainer and leader and improved patient confidence in their ability.
Limitations
One obvious limitation we encountered was language. The Chinese health care providers attending this Symposium had limited working proficiency of the English language. The curriculum was delivered in English with synchronous translation into Mandarin. It is unclear how much our visitors were able to comprehend, but they were able to present their final projects in English without difficulty.
Additionally, due to participant feedback, minor changes in curriculum occurred with each cohort, so there was some inconsistency from year to year. Participants may not have been able to implement some concepts in their respective educational or clinical environments.
Our response rate was low at 47.6%. This may be due, in part, to difficulty locating participants; in some cases, surveys were sent up to 6 years following their participation in the Symposium. Additionally, there are biases that are inherent in all survey research. Participants who had satisfying experiences may also have been more likely to respond to the survey. Social desirability bias may lead to self-reported outcomes that are less reliable/more positive than objective observations. Furthermore, participating physicians’ perceptions of their patients’ confidence may include participants’ own confidence in their abilities. Because of these biases, results should be interpreted carefully.
Next steps
Continued follow-up with graduates will allow us to obtain updates on goal development and achievements including progress in community engagement, communication/interviewing skills, doctor-patient relationship, collaboration, and patient care outcomes.
Conclusion
We anticipate that China’s health care reforms to train family physicians will take place with greater urgency due to the COVID pandemic. In October 2020, we adapted our curriculum to a webinar format which was attended by over 1500 medical professionals in China. Future innovation in digital learning may advance family medicine physician training and support and help meet the needs of growing their primary care workforce.
The goal of our Family Medicine Leadership Development Symposium was to provide scholars a knowledge base and skill set in teaching, curriculum, assessment, and leadership while highlighting the core strengths of family medicine - comprehensive, compassionate, collaborative, coordinated, patient-centered care. This will help define family medicine as an essential specialty in China and lead to improved access to care, quality of care, and reduced costs.
Feedback has been overwhelmingly positive and demonstrates how an immersive two-week experience can have positive impacts and lead to change in thinking, teaching, and patient care for Chinese family medicine physicians.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The datasets generated and/or analysed during the current study are available in the Harvard Dataverse repository: Outcomes of a US-Sino Family Medicine Leadership Program - Jenenne Geske Dataverse (harvard.edu).
References
State Commission Office of Public Sector Reform in China. Ministry of Health of the People's Republic of China. 2006. The distribution standards of human resource staffing and community health services organization settings. http://www.gov.cn/zwgk/2006-09/04/content_377067.htm [in Chinese]. The State Commission Office of Public Sector Reform in China, Beijing. Available at: Accessed 15 Oct 2010.
Chen TH, Du Y, Sohal A, Underwood M. Essay - family medicine education and training in China: past, present and future. Br J Gen Pract. 2007;57(541):674–6 PMCID: PMC2099684.
Zhang D, Unschuld PU. China’s barefoot doctor: past, present, and future. Lancet. 2008;372(9653):1865–7. https://doi.org/10.1016/S0140-6736(08)61355-0.
Baozhi S, Yuhong Z. Medical curricula in China and the USA: a comparative study. Med Teach. 2003;25(4):422–7. https://doi.org/10.1080/0142159031000136725.
Nieman LZ, Kvale J, Fu X, Gu Y, Strobel HW. Bringing a family practice model of health to the People's Republic of China. Fam Med. 2001;33(9):696–701 PMID: 11665909.
Wu D, Lam TP. Underuse of primary care in China: the scale, causes, and solutions. J Am Board Fam Med. 2016;29:240–7. https://doi.org/10.3122/jabfm.2016.02.150159.
Lian S, Chen Q, Yao M, Chi C, Fetters MD. Training pathways to working as a general practitioner in China. Fam Med. 2019;51(3):262–70. https://doi.org/10.22454/FamMed.2019.329090.
Pun JKH, Chan EA, Wang S, Slade D. Health professional-patient communication practices in East Asia: an integrative review of an emerging field of research and practice in Hong Kong, South Korea, Japan, Taiwan, and mainland China. Patient Educ Couns. 2018;101:1193–206. https://doi.org/10.1016/j.pec.2018.01.018.
Wu D, Lam TP, Lam KF, Zhou XD, Sun KS. Public views towards community health and hospital-based outpatient services and their utilisation in Zhejiang, China: a mixed methods study. BMJ Open. 2017;7(11):e017611. https://doi.org/10.1136/bmjopen-2017-017611.
Wu D, Lam TP. At a crossroads: family medicine education in China. Acad Med. 2017;92(2):185–91. https://doi.org/10.1097/ACM.0000000000001512.
Huang Y, Guo A. Development of undergraduate family medicine teaching in China. Br J Gen Pract. 2011;61(585):304–5. https://doi.org/10.3399/bjgp11X568134.
Li X, Krumholz H, Yip W, Cheng K, Massener J, Meng Q. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–12. https://doi.org/10.1016/S0140-6736(20)30122-7.
Frye AW, Hemmer PA. Program evaluation models and related theories: AMEE guide no. 67. Med Teach. 2012;34(5):e288–99. https://doi.org/10.3109/0142159X.2012.668637 PMID: 22515309.
Acknowledgements
Hannah Tong PhD from the Office of Global Engagement and former associate director of the Asia Pacific Rim Development Center at University of Nebraska Medical Center and Jialin Zheng MD PhD Dean of Tongji University School of Medicine in Shanghai, China.
Conflict disclosure
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
JL, JKS, JG, KJ, JH, and MS made substantial contributions to the conception and design of the work; JL, JKS, JG made substantial contributions to the acquisition, analysis, and interpretation of data and drafting and revising of the work. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was deemed exempt by the University of Nebraska Medical Center IRB. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, J., Koran- Scholl, J., Geske, J. et al. Outcomes of a US-Sino family medicine leadership program. BMC Med Educ 22, 788 (2022). https://doi.org/10.1186/s12909-022-03856-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03856-z