Abstract
Background
Shock causes significant morbidity and mortality in children living in resource-limited settings. Simulation has been successfully used as an educational tool for medical professionals internationally. We sought to improve comfort and knowledge regarding shock recognition and fluid management by implementing a pediatric shock curriculum using simulation as an assessment for trainees in Manila, Philippines.
Methods
We assessed a shock curriculum focused on patients with malnutrition in a prospective cohort study, using a written test and a videotaped simulation-based objective standardized clinical examination. Implementation occurred in March 2020 with 24 Filipino pediatric residents at a single institution in Manila. Outcomes included time to initiation of fluid resuscitation, improvement in confidence, knowledge on a written assessment, and performance in simulation. Results were compared pre- and post-intervention using Wilcoxon signed-rank test.
Results
The time to initiation of fluids did not change between the baseline simulation (median [interquartile range] = 71.5 seconds [52–116.5]) and the final simulation (68 seconds [52.5–89]; P = 0.42). Confidence in identifying shock and malnutrition, managing hypovolemic shock, managing septic shock, and placing intraosseous access all increased (P < 0.01) post-intervention. Written test scores showed no improvement, but performance in simulation, measured using a checklist, improved from a total score of 10 [8.5–11] to 15 [13-16] (P < 0.01).
Conclusion
In our study of a simulation-based shock education program, we showed improvement in confidence and knowledge as measured by a resuscitation checklist. It is feasible to establish a successful simulation-based education program in a low-resource setting.
Similar content being viewed by others
Background
Children living in resource-limited settings (RLS) suffer disproportionate morbidity and mortality secondary to common childhood illnesses. In 2019, over 1 million children worldwide died from sepsis, diarrhea or pneumonia [1]. Despite barriers including limited training in pediatric-specific care and lack of funding, healthcare providers in RLS must treat children in shock. Simulation has been shown to effectively educate trainees on fluid resuscitation in shock. In studies of simulation-based shock education programs, participants have consistently shown improvements with respect to confidence [2] and knowledge [3, 4]. Knowledge acquisition may be measured via written assessment or by performance on a resuscitation checklist, several of which have been validated for various topics from intraosseous (IO) needle placement [5] to shock [6] and cardiopulmonary resuscitation [3, 7,8,9,10]. Greater confidence in skills and improvement in knowledge scores can translate into changes in clinical practice although the effect on outcomes is less well-known. In a study by Qian et al., providers who participated in a simulation program on first-hour care of sepsis were more likely to initiate fluids promptly in the clinical setting [11]. Rapid recognition, in addition to initiation of appropriate fluid resuscitation, has been documented to decrease the morbidity and mortality associated with most forms of shock [12, 13], as every hour of delay is associated with 50% increased odds of mortality [14]. Improvement in outcomes may be more likely with frequent re-education sessions to prevent skill decay [3, 6, 15]. Therefore, the World Health Organization (WHO) suggests a low-dose/high-frequency training paradigm for healthcare workers [16].
Teaching fluid resuscitation in RLS is not straightforward. In 2011, the Fluid Expansion as Supportive Therapy (FEAST) trial, which was conducted in three east African nations, was stopped prematurely because children with severe febrile illness who received rapid fluid resuscitation with either 0.9% sodium chloride or 5% albumin boluses had a higher mortality rate than those who received routine care [17]. Subsequently, the WHO and Surviving Sepsis Campaign updated their guidelines to recommend cautious fluid resuscitation in RLS, particularly when critical care is unavailable [16, 18]. One hypothesis for the increased mortality of patients who receive rapid fluid resuscitation in RLS is the higher rate of co-morbid malnutrition. Patients with severe acute malnutrition may have associated structural changes to the myocardium [19, 20] and are at high risk for sudden death, thought to be secondary to associated myocardial dysfunction [21,22,23,24]. Thereby, the WHO recommends reserving intravenous fluids in patients with malnutrition for those in decompensated shock [16]. While there have been a handful of studies evaluating the safety of various fluids given to patients with severe acute malnutrition and hypovolemic or septic shock, the data has not been conclusive, emphasizing the importance of repeated patient reevaluation to interventions [25,26,27,28,29,30]. Nevertheless, fluid administration is still essential. In fact, children in RLS with septic shock have increased mortality if they do not receive fluids within the first 30 minutes of presentation [31]. Hence, in settings with high rates of malnutrition, such as the Philippines, practitioners must learn not only to recognize shock, but also to evaluate nutritional status and perform frequent patient reassessments to guide fluid management. Although there are several published simulation-based curricula focused on hypovolemic shock in pediatric patients [2, 32, 33], there are few publications evaluating curricula focused on shock of any kind in pediatric patients with co-morbid malnutrition in RLS [34, 35].
In our study, we used medium-fidelity mannequin-based simulation as part of an educational program designed to teach Filipino pediatric residents shock concepts, with an emphasis on fluid resuscitation, nutritional status assessment, and patient re-evaluation. We hypothesized that implementing a hands-on shock curriculum would decrease time to fluid administration on a simulated mannequin. In addition, we hypothesized that this curriculum would improve comfort and knowledge regarding shock recognition and fluid management based on varying nutritional status. Improving recognition of the shock state, combined with cautious initiation of fluids and improved patient assessment skills, could be lifesaving and prevent mortality of children suffering from various forms of shock.
Materials/methods
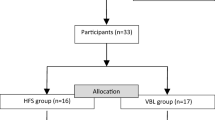
In this pre/post prospective cohort study, we evaluated a shock curriculum implemented over the course of a half-day workshop at Philippine Children’s Medical Center (PCMC) (Fig. 1), a tertiary care pediatric center in Manila. Ethics approval was obtained through Johns Hopkins University School of Medicine (JHUSOM) institutional review board, in addition to the PCMC office of research development. PCMC is one of the more resourced pediatric hospitals in the Philippines. The hospital has pediatric specialists, intensive care units with some limited ventilator capacity, a dialysis unit and access to some imaging studies such as simple CT scan and ultrasound. However, resource limitations still exist regarding laboratory frequency/availability, number of and access to mechanical ventilation, lack of supplies for central venous access, and the like, making the setting vastly different from a tertiary care pediatric facility in many other settings. In addition, the residents who train at PCMC will ultimately work in different settings across the country and may need to practice independently with minimal pediatric-specific resources. For this reason, we chose pediatric residents rotating at PCMC as participants for our pilot study. The intervention was implemented in March 2020 with 24 pediatric residents. Simulation cases were piloted and all materials, including cases, questionnaires, checklists, and didactics, were reviewed for content and fidelity by pediatric critical care fellows and attending physicians at both PCMC and JHUSOM. The residents were randomly divided between a morning and an afternoon session to ensure instructor to participant ratio of 4:1. We made no modifications to any materials between sessions to effectively compare the two cohorts.
Participants were given a written pre-test, which included questions about demographic information, an assessment of confidence with shock management on a 5-point Likert scale, and 10 knowledge-based multiple-choice questions on shock concepts. Six of these questions pertained to shock concepts typically taught as part of Pediatric Advanced Life Support (PALS) course content. Four additional questions were added on subjects of IO access, response to resuscitation, malnutrition, and management of shock secondary to dengue hemorrhagic fever. The questions underwent content review by a total of eight pediatric critical care fellows and attendings. We also administered the questions to non-curriculum participants at various levels of training as part of this process to assess discriminatory validity of the written questions. After the written exam, each resident participated individually in a simulation-based objective standardized clinical examination (OSCE) using a medium-fidelity mannequin that presented in hypovolemic shock with co-morbid malnourished status. Due to the inability to connect the mannequin to the simulation control box, we used the mannequin in a low-fidelity mode. Therefore, we were unable to change vital signs and physical exam findings in response to participant interventions. Mannequin capabilities included static palpable pulse, breath sounds, and ability to place IO. The simulation facilitator provided the participant with the clinical vignette background/history. In order to mimic a RLS, supplies required for the OSCE included intravenous/IO supplies, fluids, and the ability to check glucose. Sessions were videotaped and scored in real time by the primary investigator, who used a checklist to evaluate for the primary outcome, time in seconds to initiation of fluid resuscitation. This checklist was not formally validated. Content and construct of the checklist was modeled on previously validated checklists for pediatric resuscitation scenarios, identified by Medline literature review of simulation-based pediatric resuscitation programs [5, 8, 10]. These checklists were compiled and modified to reflect skills performed in the OSCE. Additionally, the checklist was reviewed by eight pediatric critical care specialists, four from each institution. Items on the checklist included oxygen delivery, appropriate choice and administration of fluid, assessment for malnutrition, capillary refill assessment, correct placement of IO access, identification and appropriate treatment of hypoglycemia, and reassessment of physical exam and vital signs between fluid boluses (Additional file 1: Appendix). Videotaping of each scenario allowed for later re-review by the primary investigator to confirm intra-rater reliability. Two additional reviewers blinded to pre/post assessment were trained and reviewed 20% of the videos to ensure inter-rater reliability.
The intervention included a didactic curriculum taught by the primary investigator. Topics included shock definitions, presenting symptoms, fluid types, and management recommendations guided by the Surviving Sepsis Campaign, with a differentiation based on nutritional status and concern for sepsis or dengue hemorrhagic fever. The didactic session was followed by three hands-on skills stations covering (1) oxygen delivery, assisted ventilation, and patient reassessment; (2) emergency access and rapid fluid initiation/administration; and (3) dextrose administration for hypoglycemia, appropriate assessment/evaluation for malnutrition, and importance of timely antibiotic administration in some forms of shock. Each skills station was taught in small groups by a pediatric intensive care fellow or attending physician. After the intervention, participants repeated the same written test as they had completed at the beginning of the session. Each participant again attempted a videotaped OSCE as an individual. The post-intervention scenario utilized a different clinical vignette stem to minimize recall bias, but was similarly a malnourished patient presenting in hypovolemic shock who required an identical series of interventions to achieve successful resuscitation from shock. In addition to the primary outcome of time to initiation of fluids, secondary outcomes included participant self-reported improvement in confidence with shock concepts, participant improvement in knowledge of shock concepts measured on the written post-test, and total score on the OSCE checklist.
Statistical analysis
To achieve 80% power and an α level of 0.05 to detect an improvement of 1 minute in performance, we calculated that we would need 21 training participants for target enrollment. Analysis was carried out with Stata/IC 16.1 (StataCorp). Outcome measures were compared before and after curriculum implementation. Medians with interquartile ranges (IQR) were reported for nonparametric data. Each pairing of variables/outcome measures was compared by Wilcoxon Sign Rank test. Statistical significance was set at p < 0.05. Subgroup analysis by cohort was performed using χ [2] and by resident postgraduate year (1, 2, or 3) using Kruskal-Wallis. Sub-item performance on the checklist was evaluated by using McNemar’s paired proportion. Spearman correlation was used for intra-rater and inter-rater reliability with a goal of ρ > 0.8.
Results
As a result of the COVID-19 pandemic, enrollment in the research study was stopped prematurely when the Philippines shut its borders to non-citizens and PCMC forbade gatherings of more than 10 people per room. A total of 24 pediatric residents were enrolled prior to this shutdown (Table 1). Of these participants, 96% were female, 71% had participated in simulation 1–3 times, and all were certified in Basic Life Support (BLS) and PALS. Nine participants were post-graduate year (PGY) 1, seven were PGY-2 and eight were PGY-3.
Individuals reported a median of 4 out of 5 on a Likert scale in regard to their confidence in English in the medical setting (IQR 4–4). Despite median confidence with some shock concepts remaining the same post-intervention, on analysis, confidence in all domains improved significantly (p < 0.01; Table 2). Test scores showed no significant improvement post-intervention (Table 2). The time to initiation of fluids showed a non-significant decrease from 71.5 seconds to 68 seconds, but the total score on the checklist improved (p < 0.01; Table 2).
No differences were apparent by postgraduate year on sub-analysis for any outcome. Significant improvement on the checklist was seen in skills related to appropriate malnutrition assessment, initiation of oxygen therapy, choice of correct isotonic fluid for volume resuscitation, correct placement of the IO needle, correct reassessment of patient post-interventions, and identification and treatment of hypoglycemia (Table 3).
Intra-rater agreement was good for the total checklist score (ρ = 0.97; p < 0.001; mean difference = 0.06; 95% confidence interval [CI], − 0.18-0.31) and time to initiation of fluid (ρ = 0.98; p < 0.001; mean difference = 3.3; 95% CI, 1.8–4.9). Similarly, inter-rater reliability was good for the total checklist score (ρ = 0.81; p = 0.004; mean difference = 1.3; 95% CI, 0.4–2.2) and time to initiation of fluid (ρ = 0.98; p < 0.001; mean difference = 0.6; 95% CI, − 3.5-2.38).
Discussion
Despite universal evidence that early recognition of shock and goal-directed therapy with fluids is beneficial, rapid high-volume fluid resuscitation may not be the correct management in all populations [17]. The WHO and the Surviving Sepsis Campaign differentiate management based on critical care availability, and stress judicious fluid resuscitation and frequent reassessments with particular attention to signs of fluid overload [16, 18]. We were successful in designing, implementing, and studying a simulation-based educational program that focused on immediate recognition of shock, obtaining access, examining the patient and identifying signs of malnutrition, carefully choosing fluids, and frequently reassessing patients for response to therapy or signs of fluid overload.
Following our educational intervention, the participants showed no significant improvement in time to initiation of fluids. However, all residents started fluids within 5 minutes of case start both pre- and post-intervention, consistent with the gold standard for fluid initiation in shock. Scores on the written knowledge-based test did not improve, which may be due to the high median pre-test scores or to the limited number of questions. Both of these findings may also be due to the participants being previously trained in and knowledgeable about PALS algorithms. Similar to prior studies, participants showed consistent improvement in confidence with shock resuscitation skills [2, 3]. Additionally, total checklist scores increased post-intervention. Residents showed improvement in recognition of malnutrition, placement of the patient on oxygen, choice of correct fluid, administration of fluid at an appropriate rate, correct placement of an IO needle, reassessment of the patient for fluid overload, and evaluation and treatment of hypoglycemia. Interestingly, these represent the skills taught in the hands-on stations. The primary outcome of time to initiation of fluids is likely a poor single marker of good clinical care. The rapidity with which the residents started a fluid bolus often precluded a full assessment and reassessment of the patient. Therefore, the majority of participants were unable to identify a malnourished patient, recognize decompensation, and modify management on the pre-test OSCE. Although administration of fluids in a timely manner is essential, accurate choice of fluids, ability to place alternative emergency access, and patient reassessment skills are likely all equally important, skills represented by total score on the checklist.
Similar to checklist use in other simulation studies on shock [5,6,7,8, 10], the total score on the checklist may be a better representation of knowledge acquisition than the written test and a more clinically relevant outcome than simply time to initiation of fluids. Although the checklist is not formally validated, we did complete components of the validation process, including partial expert review and assessment for intra- and inter-rater reliability. Checklist content was reviewed by senior pediatric intensive care specialists from both the United States and the Philippines, and we showed good intra- and inter-rater agreement on analysis. While the resuscitation checklist still needs to undergo a formal validation study, it could potentially be applied to clinical scenarios as a marker of change in practice and management in the future.
Our study had several limitations. It was a small pilot study to evaluate feasibility of curriculum implementation in this setting, made smaller by international circumstances during a pandemic. Additionally, our power calculation overestimated resident time to initiation of fluids and the checklist we used to evaluate our outcomes is not yet a validated tool. PCMC is a large academic institution with residents who are BLS- and PALS-certified, generally experienced in simulation, and comfortable speaking English in medically complex situations. Although reflective of the typical make-up of pediatric trainees, participants were almost exclusively female. The power and generalizability of our study are therefore limited. It would be beneficial to continue implementation with more residents and to extend the curriculum to healthcare workers from various regions of the country. Although not the case in our study, lack of familiarity with simulation is a common limitation in RLS, emphasizing the importance of introducing the mannequin functionality and the concept of simulation and debriefing. Importantly, this curriculum is not fully applicable to some rural and low-resource areas, as the simulation minimally requires access to intravenous/IO supplies, fluids, and the ability to check glucose. In these lowest resource areas, the curriculum could be adapted to focus on physical exam skills and early recognition of shock to guide healthcare workers in patient triage and escalation to a higher level of care. Additionally, we used a medium-fidelity mannequin for the OSCE, which is an expensive tool. However, we experienced technical challenges with the mannequin, essentially rendering it a low-fidelity mannequin. The OSCE could easily be modified for implementation using a low-fidelity mannequin. Finally, although residents showed improvement in confidence and knowledge as measured by the checklist, it is unclear how our results will translate both long-term, and to the clinical setting. As a future direction of this study, it will be important to assess skill and long-term knowledge retention at various intervals following this curriculum. Participants would likely benefit from refresher training using a low-dose/high-frequency training paradigm that would help them to maintain their skills and facilitate translation of their knowledge into improved clinical practice [5, 16].
This educational program included a simulation portion, a didactic and multiple hands-on stations. Particularly in a setting where time, materials and personnel are limited, it would be helpful to know if all components of this program are essential for knowledge acquisition. Future iterations of the study could compare outcomes between individuals who participated in the entire curriculum, individuals who participated solely in the didactic and those who did not participate in any intervention. This could help delineate if one intervention is more effective than another, as it is possible that the OSCE on its own serves as the most substantial contributor to participant learning.
Global health research poses many unique challenges. We had a previously established relationship with individuals practicing pediatric critical care at PCMC [36], which enabled us to implement this curriculum more efficiently than may be typical. Despite this strong relationship with individuals at PCMC, the formal approval process for the project took several months, necessitating in-person meetings with hospital administrators and the establishment of an in-country proxy to attend additional meetings, obtain signatures and deliver paperwork. Remote communication and collaboration on educational materials was especially difficult. This improved significantly following our initial site visit, where we were able to better understand which channels of communication (e.g. phone messenger applications) were most utilized by our colleagues. Even with these positive interactions, we were unable to obtain approval to enroll non-physicians, and were limited in the dates for the experience due to difficulties finding protected time for the residents. However, in part due to excellent communication and preparation (materials, logistics, staffing), the day of implementation was very successful. Students expressed gratitude for the experience, requested to stay after their sessions were complete to ask questions and practice skills, and indicated that they would be very interested in future hands-on simulation experiences.
Conclusions
This study of a simulation-based education program on shock for pediatric residents in Manila was designed to establish a sustainable model of simulation education using accessible, low-cost materials in an RLS. All materials that we used, with the exception of the medium fidelity mannequin, were donated to PCMC in order to promote sustainability of the curriculum and refresher training sessions. We showed improvement with respect to confidence in skills needed for resuscitation of children in shock, in addition to knowledge as measured by a resuscitation OSCE checklist after our intervention. Based on the results of this study and the success of the curriculum, PCMC plans to use local faculty to continue teaching this curriculum to its pediatric residents, a practice that will enhance project sustainability.
We were able to successfully collaborate with local physicians who participated in the creation and implementation of the curriculum. We have laid the groundwork for continued simulation education at PCMC that could be elaborated upon to encompass other topics and scenarios beyond shock in a contextualized manner. If successful in creating a larger and more long-term educational network, over time we plan to evaluate for changes in clinical practice, and eventual changes in patient outcomes, with the intent to improve recognition and management of shock and decrease the associated mortality. Our results are promising, but transitioning from improvement in confidence and knowledge to changes in clinical outcome will require widespread and long-term use of an educational program that comes from local stakeholder commitment and institutional buy-in.
Availability of data and materials
Data and materials for implementing curriculum have been uploaded and are available for public access in Harvard Dataverse, V2. https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/OQEMLH
Abbreviations
- RLS:
-
Resource-limited settings
- IO:
-
Intraosseous
- WHO:
-
World Health Organization
- FEAST:
-
Fluid Expansion as Supportive Therapy
- PCMC:
-
Philippine Children’s Medical Center
- JHH:
-
Johns Hopkins Hospital
- PALS:
-
Pediatric Advanced Life Support
- OSCE:
-
Objective standardized clinical examination
- BLS:
-
Basic Life Support
- PGY:
-
Post-graduate year
References
World Health Organization: the Global Health Observatory: child mortality and causes of death. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/child-mortality-and-causes-of-death (2021). Accessed: 20 Dec 2021.
Rideout M, Raszka W. Hypovolemic shock in a child: a pediatric simulation case. MedEdPORTAL. 2018;14:10694.
Wright SW, Steenhoff AP, Elci O, Wolfe HA, Ralston M, Kgosiesele T, et al. Impact of contextualized pediatric resuscitation training on pediatric healthcare providers in Botswana. Resuscitation. 2015;88:57–62.
Cory MJ, Colman N, McCracken CE, Hebbar KB. Rapid cycle deliberate practice versus reflective debriefing for pediatric septic shock training. Pediatr Crit Care Med. 2019;20(5):481–9.
Oriot D, Darrieux E, Boureau-Voultoury A, Ragot S, Scépi M. Validation of a performance assessment scale for simulated intraosseous access. Simul Healthc. 2012;7(3):171–5.
Dugan MC, McCracken CE, Hebbar KB. Does simulation improve recognition and management of pediatric septic shock, and if one simulation is good, is more simulation better? Pediatr Crit Care Med. 2016;17(7):605–14.
Donoghue AJ, Durbin DR, Nadel FM, Stryjewski GR, Kost SI, Nadkarni VM. Effect of high-fidelity simulation on pediatric advanced life support training in pediatric house staff: a randomized trial. Pediatr Emerg Care. 2009;25(3):139–44.
Donoghue AJ, Nishisaki A, Sutton R, Hales R, Boulet J. Reliability and validity of a scoring instrument for clinical performance during pediatric advanced life support simulation scenarios. Resuscitation. 2010;81(3):331–6.
Hunt EA, Duval-Arnould JM, Nelson-McMillan KL, Bradshaw JH, Diener-West M, Perretta JS, et al. Pediatric resident resuscitation skills improve after "rapid cycle deliberate practice" training. Resuscitation. 2014;85(7):945–51.
Levy A, Donoghue A, Bailey B, Thompson N, Jamoulle O, Gagnon R, et al. External validation of scoring instruments for evaluating pediatric resuscitation. Simul Healthc. 2014;9(6):360–9.
Qian J, Wang Y, Zhang Y, Zhu X, Rong Q, Wei H. A survey of the first-hour basic care tasks of severe sepsis and septic shock in pediatric patients and an evaluation of medical simulation on improving the compliance of the tasks. J Emerg Med. 2016;50(2):239–45.
Carcillo JA, Davis AL, Zaritsky A. Role of early fluid resuscitation in pediatric septic shock. JAMA. 1991;266(9):1242–5.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112(4):793–9.
Morris SM, Fratt EM, Rodriguez J, Ruman A, Wibecan L, Nelson BD. Implementation of the helping babies breathe training program: a systematic review. Pediatrics. 2020;146(3):e20193938.
World Health Organization. Updated guideline: Paediatric emergency triage, assessment and treatment. Care of Critically ill Children. https://apps.who.int/iris/handle/10665/204463 (2016). Accessed 20 Dec 2021.
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364(26):2483–95.
Weiss SL, Peters MJ, Alhazzani W, Agust MSD, Flori HR, Inwald DP, et al. Surviving Sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr Crit Care Med. 2020;21(2):e52–e106.
Bergman JW, Human DG, De Moor MM, Schulz JM. Effect of kwashiorkor on the cardiovascular system. Arch Dis Child. 1988;63:1359–62.
Kothari SS, Patel TM, Shetalwad AN, Patel TK. Left ventricular mass and function in children with severe protein energy malnutrition. Int J Cardiol. 1992;35:19–25.
Maitland K, George EC, Evans JA, Kiguli S, Olupot-Olupot P, Akech SO, et al. For the FEAST trial group. Exploring mechanisms of excess mortality with early fluid resuscitation: insights from the FEAST trial. BMC Med. 2013;11:68.
Dramaix M, Brasseur D, Donnen P, Bahwere P, Porignon D, Tonglet R, et al. Prognostic indices for mortality of hospitalized children in Central Africa. Am J Epidemiol. 1996;143:1235–43.
Wharton BA, Howells GR, McCance RA. Cardiac failure in kwashiorkor. Lancet. 1967;2:384–7.
Smythe PM, Swanepoel A, Campbell JA. The heart in kwashiorkor. BMJ. 1962;1:67–73.
Obonyo N, Maitland K. Fluid management of shock in severe malnutrition: what is the evidence for current guidelines and what lessons have been learned from clinical studies and trials in other pediatric populations? Food Nutr Bull. 2014;35(2 suppl):S71–8.
Brewster DR. Critical appraisal of the management of severe malnutrition: 3. Complications J Paediatr Child Health. 2006;42:583–93.
Akech SO, Karisa J, Nakamya P, Boga M, Maitland K. Phase II trial of isotonic fluid resuscitation in Kenyan children with severe malnutrition and hypovolaemia. BMC Pediatr. 2010;10:71.
Ahmed T, Ali M, Ullah MM, Choudhury IA, Haque ME, Salam MA, et al. Mortality in severely malnourished children with diarrhoea and use of a standardised management protocol. Lancet. 1999;353:1919–22.
Alam NH, Islam S, Sattar S, Monira S, Desjeux JF. Safety of rapid intravenous rehydration and comparative efficacy of 3 oral rehydration solutions in the treatment of severely malnourished children with dehydrating cholera. J Pediatr Gastroenterol Nutr. 2009;48:318–27.
Bachou H, Tumwine JK, Mwadime RKN, Ahmed T, Tylleskar T. Reduction of unnecessary transfusion and intravenous fluids in severely malnourished children is not enough to reduce mortality. Ann Trop Paediatr. 2008;28:23–33.
Oliveira CF, Nogueira de Sá FR, Oliveira DS, Gottschald AF, Moura JD, Shibata AR, et al. Time- and fluid-sensitive resuscitation for hemodynamic support of children in septic shock: barriers to the implementation of the American College of Critical Care Medicine/pediatric advanced life support guidelines in a pediatric intensive care unit in a developing world. Pediatr Emerg Care. 2008;24(12):810–5.
Huber J, Schimelpfenig M, Berner J, Hsu B. Simulation of cardiovascular and respiratory distress for the pediatric clerkship. MedEdPORTAL. Published online 2014.
Reid J, Stone K. Pediatric emergency medicine simulation curriculum: hypovolemic shock. MedEdPORTAL. Published online 2013.
Fallah PN, Ovsak GG, Kasper J, Riviello R, Nezerwa Y, Wispelwey B, et al. A longitudinal case-based global health curriculum for the medical student clerkship year. MedEdPORTAL. 2020;16:11038.
Maloney CE, Burns R, Hartford E, von Saint Andre-von Arnim A, Foohey S, Kailemia M, et al. “International pediatric emergency medicine and critical care fellow education: utilizing virtual resuscitation simulation in settings with differing resources. Cureus 2022;14(2):e21991.
Gardner Yelton SE, McCaw JM, Reuland CJ, Steppan DA, Evangelista PPG, Shilkofski NA. Evolution of a bidirectional pediatric critical care educational partnership in a resource-limited setting. Front Pediatr. 2021;9:738975.
Acknowledgements
We would like to acknowledge Claire Levine, MS, ELS (Scientific Editor, Department of Anesthesiology and Critical Care Medicine, Johns Hopkins University) for her assistance in editing this manuscript, the Johns Hopkins Simulation center for donating materials and simulation mannequins, and Kevin Psoter, PhD, MPA (Director of Science and Lead Methodologist Biostatistics, Epidemiology and Data Management Core, The Center for Child and Community Health Research, Johns Hopkins University) for his statistical support.
Funding
The primary investigator (SGY) is a recipient of the Lietman Travel Award from the Johns Hopkins Center for Global Health, which funded travel and selected educational materials. This funding source provided support for conduct of the research but did not play a role in the study design, data collection, analysis, or decision to submit the paper for publication. The senior author (NAS) has received research funding from the U.S. Department of Education Fulbright-Hays Group Projects Abroad Program and from the Laerdal Foundation to support work that is un-related to the research outlined in the manuscript. These funding sources did not provide any support for the conduct of the research described herein.
Author information
Authors and Affiliations
Contributions
SGY and NAS are responsible for the conception and design of the research study. SGY and NAS participated in acquisition of data, analysis, interpretation of data and drafting of primary manuscript and additional revisions. LCR and PPGE contributed to the design of the work, acquisition of data and revisions of the manuscript. CJR contributed to the analysis of the work and revisions of the manuscript. All authors have read and approve the submitted version and attest to the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research study was approved by the Johns Hopkins IRB 00216019 and the Philippine Children’s Hospital Institutional research – Ethics Committee PCMC IR-EC 2019–088. All methods were carried out in accordance with relevant guidelines and regulations. All participants were provided with informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gardner Yelton, S.E., Ramos, L.C., Reuland, C.J. et al. Implementation and evaluation of a shock curriculum using simulation in Manila, Philippines: a prospective cohort study. BMC Med Educ 22, 606 (2022). https://doi.org/10.1186/s12909-022-03669-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03669-0