Abstract
Background
Early career general practitioners are known to be at high risk of burnout. There is a need for widely applicable, cost-effective evidence-based interventions to develop trainees’ protective skills and strategies.
Results
Of 120 eligible trainees, 23 (19.2%) expressed interest in participating, 17 subsequently started the course, and 15 completed at least 5 out of its 6 sessions. All psychological measures were stable for the six-week period prior to commencing the course. Following the course, there were statistically significant (p < 0.05) improvements in wellbeing, resilience, mindfulness, emotional exhaustion, disengagement, and stress scores. Participants described numerous benefits, and most stated that they would recommend it to colleagues.
Conclusion
Including mindful practice within general practice vocational training is feasible, and in this study it benefited the psychological wellbeing of participants. Further research is needed to explore ways of increasing uptake and course completion, the sustainability of its effects, and the wider applicability of this approach.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
General practitioners (GPs) at all stages of their career are at high risk of suffering from emotional stress, depression and burnout [1, 2], and this is contributing to increasing levels of sickness absence, and difficulties in retaining the GP workforce [3]. This is an international issue, with risk of burnout reflecting numerous factors including personal attributes, workload pressures, and difficult encounters with patients and colleagues [3, 4].
General Practice vocational training in the United Kingdom last 3 years and represents an opportunity for proactively equipping future GPs with effective coping skills [5]. This includes building resilience, the ability to bounce back or recover from stress [6]. However, despite recent interest in techniques to improve physicians’ resilience and wellbeing the evidence to support such interventions is sparse [7].
Mindfulness is the capacity for enhanced, non-judgmental and sustained moment-to-moment awareness of one’s own mental and emotional state and being, in the context of one’s immediate environment. There is evidence that mindfulness can improve doctors’ resilience, wellbeing, self-awareness and interpersonal skills [8,9,10,11], as well as patient-centred care [11,12,13]. Adapted mindfulness based programmes are becoming more popular in medical training, but requiring further assessment [14].
In a recent study with 47 GP trainees in the West Midlands, we demonstrated both a need and desire for greater wellbeing and resilience support as part of their vocational training [15]. On validated psychological scales, the trainees showed high prevalence for signs of burnout, including emotional disengagement (36; 80%) and exhaustion (35, 77%), with 29 (64%) scoring above the cut-off value for both. Over a third reported practising some form of mindfulness already, and most described interest in engaging in mindfulness practice. Specific work-related factors such as a lack of knowledge and training to deal with complex patients, inability to detach from work, and the need to keep up appearances, were described as factors that contributed to emotional exhaustion.
In the current study, we worked with the same cohort of trainees to explore the potential for incorporating mindfulness into their vocational training programme. We used the results of the previous study to adapt the Mindful Practice Curriculum (MPC) [16] for delivery as part of the vocational training programme. The MPC is training programme from the USA that has been specifically designed for physicians, and is based on Mindfulness-Based Stress Reduction (MBSR) [17]. It focuses on improving clinical resilience, quality of care and caring, and personal wellbeing; it appeared well-suited to addressing the challenges described by GP trainees.
The primary aim of the study was to assess the feasibility and acceptability of delivering the MPC training within the busy timetable for vocational training. Additionally, the impact of the MPC on participants’ psychological outcomes was explored, including well-being, disengagement, emotional exhaustion, resilience, stress management and mindfulness, together with participants’ views about the programme.
Methods
Recruitment of participants
All 120 Specialty Training (ST) trainee GPs from second year (ST2) and third year (ST3) in Coventry and Warwickshire were invited to participate in the programme. A presentation about the project was made at their weekly half-day release teaching, outlining the project’s aims and objectives, timescales, and details of the MPC. Following this, an email was sent to trainees, summarising the material that had been presented and providing a participant information sheet. It was explained that only those who could commit to attending at least five of the six sessions involved in the MPC were eligible to participate. Eligible participants completed informed consent.
Intervention
The MPC aims to teach and reinforce patient-centered care through strengthening secular contemplative practices, narrative medicine, reflective questioning and appreciative inquiry. We adapted the programme to be delivered through weekly 1.5-h group sessions over a six-week period led by MK, a fully trained Mindful Practice tutor. Each session involved a didactic component in which information and research data relevant to the theme was presented, followed by a brief period of contemplative practice that included guided mindfulness practice and other exercises to practice at home and during clinical practice. Participants then engaged in a narrative exercise in which they were asked to recall a clinical experience related to the theme and were encouraged to write about their experience. These narrative exercises were used to share stories and practice using techniques of reflective questioning. The key themes covered in the course are described in Table 1. The sessions were delivered across lunchtime periods at a hospital teaching centre, which was felt to be the optimal time and location for enabling trainees’ participation.
Data collection
Data were collected via a range of validated instruments (see Table 2). Participants were invited via email to complete online questionnaires (using Qualtrics platform), including measures 6 weeks prior to the course, immediately prior to the course (to act as baseline measures), and up to 3 weeks after completion of the course. Participants were given a unique identifiable number, which allowed pairing of the responses immediately prior and post completion of the course; however, the unique identifier was not included with the measures completed 6 weeks prior to the course and so these scores could not be matched with the subsequent scores. Multiple reminders were sent to participants to encourage completion of the questionnaires.
In addition, at the time of completion of the post-course questionnaire, participants answered questions related to acceptability and experience of the programme. This included barriers to attending the course, behavioural changes experienced, and overall views of the course.
In order to avoid potential concerns over confidentiality and to encourage openness, no personal data were collected.
Data analysis
SPSS version 25 was used for data analysis. The analyses were planned on the assumption that data were normally distributed. Independent t-tests were used to analyse unmatched data (i.e. from data collected 6 weeks prior and immediately prior to the course delivery), and paired student t tests were used to analyse matched data (immediately prior and post course data). Intention to treat analysis was used for comparing results immediately prior and post course attendance. P < 0.05 was considered as a statistically significant different.
Qualitative data from the post-course questionnaire were analysed thematically.
Ethical approval
Ethical approval was obtained from the University of Warwick’s Biomedical and Scientific Research Ethics Sub-Committee (REGO-2018-2292).
Results
Participants
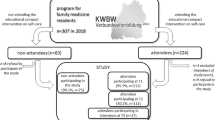
Twenty-three (19.2%) trainees stated that they could attend at least five of the six sessions and expressed interest in participating in the study, and 20 consented to take part. Of the latter, 17 subsequently started the course and 15 (88%) of them completed at least 5 out of its 6 sessions and were classed as “completers”. The other three consented individuals were unable to participate due to training schedule problems or changed personal circumstances. Consort diagram in Fig. 1 shows participant flow through the study.
Reasons for missing individual sessions mainly related to conflicting commitments and priorities within and outside work.
“Though I used to start my surgery early to attend, seeing patient on home visit caused delay to come to course on time”. R9
“Difficulty with anything outside of the curriculum (especially as course running at same time as sitting exams) that it can feel like another extra thing”.R2
“It is hard to concentrate on the present when we have many worries.” R.5
Effect of MPC on psychological outcomes
Matched scores for pre- and post-course outcome measures were available for 17 participants. Fourteen had also completed outcome measures 6 weeks prior to the course.
Outcome scores obtained 6 weeks prior and immediately prior to the start of the course (Table 3) were stable, suggesting that levels of wellbeing, burnout, stress, and resilience, were consistent during this control period.
Following the course, there was significant improvement in all outcome measures (Table 4). For example, while 13 (76%) trainees scored above the threshold for significant disengagement (2.10) in the pre-course survey, this dropped to 5 (29%) participants post-course. There were 16 trainees (94%) who scored above the threshold (2.25) for emotional exhaustion pre-course, but only 9 (53%) post-course.
Participant experience
Most participants reported a positive outcome in their post-course feedback, mentioning improvement in coping with stress and feeling better able to manage emotional exhaustion.
“I feel more able to recognize when I am tired and stressed” R4
“I feel I have tools to cope with stress and burnout better” R7
The mindfulness skills gained through the course were generally felt to have been of value.
“…being aware of your presence and surroundings, to observe rather than have a stress response” R9
“…. acknowledgment of feeling, body sensations and thoughts, including negative ones.” R13
Only one participant did not feel the course had had any personal impact.
“Unfortunately, not, there was no real new content for me and meditation was something I really don’t connect with” R14
Most stated that they would recommend the course being made available to all doctors, with 15 out of 16 (93.8%) stating that they would like to see mindfulness training included as part of vocational training.
“Absolutely, I think it could provide benefit to all trainees, a large part of our curriculum is on our fitness to practice with specific mention of our own health/ wellbeing and this course hugely supports this.”R4
“Absolutely. As a GP the public frustration about NHS seems to hit us hardest. It is a very demanding profession and without self-care it is extremely hard to be able to do this job until you retire.” R8
However, there was recognition that the MPC course would not suit all trainees.
“I don't think that all will get on board with this, therefore I don't think it would be worthwhile for all trainees. However, it has improved my resilience and I can see how it can reduce burnout etc.”R18
Discussion
Summary
This study demonstrated the feasibility of delivering the six-week Mindful Practice Curriculum [16] as part of vocational training for general practice. The MPC was modified to fit within the constraints of general practice training in the UK and to introduce participants to a variety of topics that work synergistically to benefit wellbeing, resilience and burnout. Finding a convenient time and setting for the course delivery in the context of trainees’ busy schedules proved difficult. As participation in the programme was limited to trainees who could commit to attending at least five of the six sessions, those with conflicting clinical or training commitments, planned annual leave or other unavoidable personal issues were prevented from participating. However, almost all of those who did participate, completed it successfully and experienced positive personal gains. Compared to pre-course levels, there was statistically significant improvement in outcome measure scores in specific areas of resilience, mindfulness, stress and burnout. Almost all participants stated that they would like to see mindfulness training being incorporated into future vocational training and hence becoming accessible to all trainees.
Strengths and limitations
The intervention drew on an evidence-based mindfulness training programme that has been specifically designed for doctors, and adapted it to increase its applicability and fit with the pressures of vocational training in the UK. Another strength was the use of validated psychological outcome measures. In the absence of a control group, the comparison of data at baseline and 6 weeks prior allowed us to demonstrate the persistent state of psychological health for the participants prior to participating in the course while the matching of pre- and post-course outcome measures enabled demonstration of the effect associated with course participation. Qualitative data collection provided greater depth to the findings, and understanding of how benefits were experienced; however, we lacked the resource to undertake a more in-depth qualitative exploration of participants’ experience, or of their intentions regarding future use of the skills that they have developed, limiting predictive sustainability of the programme.
The number of participants was sufficient to test the feasibility of intervention delivery as part of GP vocational training, but too small to draw definitive conclusions about its effectiveness. Despite the cohort of trainees who were eligible to participate in the course having high levels of stress and burnout and expressing a desire to engage in mindfulness training, as reported previously, relatively few volunteered to actually taking part. Finding a convenient and accessible time for delivering the course sessions was challenging, and individuals who were based in general practices that were distant from the hospital teaching centre found it more difficult to attend. Also, the need for participants to commit at the outset to attending at least 5 of the 6 sessions may have been off-putting for individuals who had annual leave or other conflicting commitments. For some individuals, the requirement to make an up-front commitment to attending the course may have been perceived as an addition stressor in the context of unavoidable everyday workload pressures. The novelty of this programme may have acted as an additional barrier for some individuals, and some may not have wanted to participate in research.
Given the small numbers involved and the lack of longer-term follow-up data, the effects observed on the measured psychological variables need to be interpreted with some caution. It was beyond the scope of the study to explore participants’ experience in-depth and how this affected outcomes; for example, participants may have varied in their interest in the weekly course topics (stress, burnout, recovery, concentration, well-being etc) and this may have affected the training effectiveness. In addition, longer term follow up is needed to demonstrate the sustainability of the skills gained beyond the period of the course itself.
Comparison with existing literature
A recent systematic review summarised the evidence base for the positive impacts of Mindfulness-based interventions (MBIs) on doctors’ well-being and performance [22]. Several studies were reported as having methodological limitations due to self-selection of participants and lack of active control conditions. However, MBIs, similar to MPC, that included multiple essential mindfulness elements (development of greater attentional, emotional and behavioural self-regulation, as well as positive qualities such as compassion, wisdom, equanimity) in their content, or that employed a group-based training format, mostly showed positive effects [23,24,25].
While ours is the first study to focus on GP trainees using MPC and addressing specific needs and dynamics of physician’s activity, other MBIs have been shown to improve levels of mindfulness and reduce burnout in primary care professionals in Brazil [26], psychiatry trainees in Australia [27] and foundation trainee doctors and medical students in the UK [28, 29]. The latter study was an adaptation of the Mindfulness Based Cognitive Therapy (MBCT) programme for the workplace. A study from the USA with primary care staff (doctors, nurses, allied medical staff) indicated that the Mindfulness-based Wellness and Resilience (MBWR), another approach to mindfulness training, may be feasible and acceptable [30]. Recent study in France describes a protocol aiming to assess in a randomized control trial the long-term effectiveness and acceptability of a mindfulness-based intervention (MBI) compared with relaxation training (RT) [31].
Implications for research and practice
There is an urgent need to promote wellbeing and resilience strategies within vocational training in order to prepare doctors for a career in general practice and lower the risk of emotional exhaustion and burnout in trainee and early career GPs [32]. This is important to retaining a healthy GP workforce, particularly given that relatively large numbers of trainees are currently intending to take career breaks, part-time work or leave the profession altogether [1, 2].
This study has demonstrated the feasibility within a real world context of delivering a six-week mindfulness course to trainee GPs. It found a high level of participant acceptability and identified associated benefits in participants’ mental wellbeing. While this needs to be interpreted in the context of this being a study conducted within one setting, with barriers such as competing vocational course priorities cited as a reason for a lack of engagement, the findings are sufficient to suggest that this offers a promising approach which may have widespread application. Further consideration is required of the resources that are needed to support the scaling up of this intervention, including protected time for undertaking wellbeing activities as part of vocational training, in order to support more widespread Integration into training programmes.
Availability of data and materials
Requests to access the data should be made to the corresponding author.
References
Cohidon C, Wild P, Senn N. Job stress among GPs: associations with practice organisation in 11 high-income countries. Br J Gen Pract. 2020;70(698):e657–67. https://doi.org/10.3399/bjgp20X710909.
Ratanawongsa N, Roter D, Beach MC, Laird SL, Larson SM, Carson KA, et al. Physician burnout and patient-physician communication during primary care encounters. J Gen Intern Med. 2008;23(10):1581–8. https://doi.org/10.1007/s11606-008-0702-1.
Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. 2016;11(7):e0159015. https://doi.org/10.1371/journal.pone.0159015.
Delbrouck M. The burnout of the caregiver. Sens-Dessous. 2017;1:5–18.
Dale J, Russell R, Scott E, Owen K. Factors influencing career intentions on completion of general practice vocational training in England: a cross-sectional study. BMJ Open. 2017;7(8):e017143. https://doi.org/10.1136/bmjopen-2017-017143.
Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. https://doi.org/10.1080/10705500802222972.
Murray M, Murray L, Donnelly M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Fam Pract. 2016;17(1):36.
Haimerl CJ, Valentine ER. The effect of contemplative practice on intrapersonal, interpersonal, and transpersonal dimensions of the self-concept. J Transpers Psychol. 2001;33(1):37–52.
Eberth J, Sedlmeier P. The effects of mindfulness meditation: a meta-analysis. Mindfulness. 2012;3(3):174–89. https://doi.org/10.1007/s12671-012-0101-x.
Singh NN, Singh SD, Sabaawi M, Myers RE, Wahler RG. Enhancing treatment team process through mindfulness-based mentoring in an inpatient psychiatric hospital. Behav Modif. 2006;30(4):423–41. https://doi.org/10.1177/0145445504272971.
Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med. 2013;11(5):412–20. https://doi.org/10.1370/afm.1511.
Beckman HB, Wendland M, Mooney C, et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87(6):815–9. https://doi.org/10.1097/ACM.0b013e318253d3b2.
Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA Netw Open. 2009;302(12):1284–93.
Epstein RM. Mindfulness in medical education: coming of age. Perspect Med Educ. 2020;9(4):197–8.
Hanson P, Clarke A, Villarreal M, Khan M, Dale J. Burnout, resilience, and perception of mindfulness programmes among GP trainees: a mixed-methods study. BJGP Open. 2020;4(3):bjgpopen20X101058.
Epstein R, Quill T, Krasner M, et al. A curriculum in mindful practice for students and residents faculty manual. University of Rochester: School of Medicine and Dentistry; 2007.
Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–90. https://doi.org/10.1007/BF00845519.
Demerouti E. The convergent validity of two burnout instruments: A multitrait-multimethod analysis. European Journal of Psychological Assessment. 2003. https://doi.org/https://psycnet.apa.org/doi/10.1027/1015-5759.19.1.12.
Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and Emotion Regulation: The Development and Initial Validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J Psychopathol Behav Assess. 2007;29(3):177–90.
Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav. 1983;24(4):385.
Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S,Parkinson J, Secker J, Stewart-Brown S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5(1):63.
Scheepers RA, Emke H, Ronald M. Epstein ea. The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Educ. 2020;54(2):138–49.
Amutio A, Martinez-Taboada C, Delgado LC, et al. Acceptability and effectiveness of a long-term educational intervention to reduce Physicians’ stress-related conditions. J Contin Educ Heal Prof. 2015;35(4):255–60. https://doi.org/10.1097/CEH.0000000000000002.
Verweij H, Waumans RC, Smeijers D, Lucassen PLBJ, Donders ART, van der Horst HE, et al. Mindfulness-based stress reduction for GPs: results of a controlled mixed methods pilot study in Dutch primary care. Br J Gen Pract. 2016;66(643):e99–105. https://doi.org/10.3399/bjgp16X683497.
Amutio A, Martinez-Taboada C, Hermosilla D, et al. Enhancing relaxation states and positive emotions in physicians through a mindfulness training program: a one-year study. Psychol Health Med. 2015;20(6):720–31. https://doi.org/10.1080/13548506.2014.986143.
Ribeiro Santiago PH, Rodrigues Valle Serra L, Flemming Colussi C. Feasibility evaluation of a mindfulness-based stress reduction program for primary care professionals in Brazilian national health system. Complement Ther Clin Pract. 2019;35:8–17.
Kang M, Selzer R, Gibbs H, et al. Mindfulness-based intervention to reduce burnout and psychological distress, and improve wellbeing in psychiatry trainees: a pilot study. Australas Psychiatry. 2019;27:219.
Bu CNN, Cotzias E, Panagioti M. Mindfulness intervention for foundation year doctors: a feasibility study. Pilot Feasibility Stud. 2019;5(1):61. https://doi.org/10.1186/s40814-019-0449-y.
Rich A, Aly A, Cecchinato ME, et al. Evaluation of a novel intervention to reduce burnout in doctors-in-training using self-care and digital wellbeing strategies: a mixed-methods pilot. BMC Med Educ. 2020;20(1):294.
Colgan DD, Christopher M, Bowen S, Brems C, Hunsinger M, Tucker B, et al. Mindfulness-based wellness and resilience intervention among interdisciplinary primary care teams: a mixed-methods feasibility and acceptability trial. Prim Health Care Res Dev. 2019;20:e91. https://doi.org/10.1017/S1463423619000173.
Baeza-Velasco C, Genty C, Jaussent I, et al. Study protocol of a multicenter randomized controlled trial of mindfulness-based intervention versus relaxation to reduce emotional exhaustion in medical students in France: the “Must prevent” study. BMC Psychiatry. 2020;20(1):115.
Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–31. https://doi.org/10.1001/jamainternmed.2018.3713.
Acknowledgements
We thank course organisers of the Coventry and Warwickshire GP Vocational Training Scheme who accommodated the delivery of the MPC within the vocational training scheme programme, these include all the trainees who participated and completed outcome measures.
We specially thank Professor Ronald Epstein from the University of Rochester Medical School for working with us to adapt the MPC to be applicable to a UK GP training context.
MV acknowledges the Centre of Mindfulness of University of Albert Einstein broadened his understanding of patient centered care based on mindfulness, so informing the design of the current study.
Author information
Authors and Affiliations
Contributions
Professor Jeremy Dale design of study, data collection and analysis, drafting and approving the paper. Dr. Petra Hanson design of study, data collection and analysis, drafting and approving the paper. Dr. Amy Clarke, design of study, data analysis, drafting and approving the paper. Dr. Majid Khan, data collection, adaptation and delivery of the MP, analysis, drafting and approving the paper. Dr. M Villarreal design of study, adaptation and delivery of the MPC, data collection and analysis, drafting and approving the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the University of Warwick’s Biomedical and Scientific Research Ethics Sub-Committee (REGO-2018-2292).
All methods were performed in accordance with the relevant guidelines and regulations.
All participants completed inform consent.
Consent for publication
Not applicable.
Competing interests
Dr. Majid Khan delivered the adapted Mindful Practice Curriculum.
Dr. M Villarreal assisted Dr. Kahn in delivering Mindful Practice Curriculum.
Funding: Health Education England West Midlands.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Villarreal, M., Hanson, P., Clarke, A. et al. Feasibility, acceptability and effect of the Mindful Practice curriculum in postgraduate training of general practitioners. BMC Med Educ 21, 327 (2021). https://doi.org/10.1186/s12909-021-02747-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-021-02747-z