Abstract
Background
Diabetes mellitus is one of the major global health disorders increasing at an alarming rate in both developed and developing countries. The objective of this study was to assess the effect of aqueous extract of Momordica charantia (AEMC) on fasting blood glucose (FBG), tissue glycogen, glycosylated haemoglobin, plasma concentrations of insulin and GLP-1 hormone (glucagon-like peptide 1) in healthy and diabetic wistar rats.
Methods
Male Wistar rats (both normal and diabetic) were treated with AEMC by gavaging (300 mg/kg body wt/day for 28 days).
Results
AEMC was found to increase tissue glycogen, serum insulin and GLP-1 non-significantly (P > 0.05) in normal, significantly (P < 0.01) in diabetic Wistar rats, whereas decrease in FBG and Glycosylated haemoglobin non-significantly (P > 0.05) in normal, significantly (P < 0.01) in diabetic Wistar rats. The elevation of GLP-1 level in normal and diabetic treated groups may be due to the L-cell regeneration and proliferation by binding with L-cell receptors and makes a conformational change, resulting in the activation of a series of signal transducers. The polar molecules of M. charantia also depolarize the L-cell through elevation of intracellular Ca2+ concentration and which in turn releases GLP-1. GLP-1 in turn elevates beta-cell proliferation and insulin secretion.
Conclusion
The findings tend to provide a possible explanation for the hypoglycemic action of M. charantia fruit extracts as alternative nutritional therapy in the management and treatment of diabetes.
Similar content being viewed by others
Background
Diabetes Mellitus (DM) is one of the most prevalent and serious metabolic disorders affecting about 200 million people worldwide [1]. Type 2 DM (T2DM) is the prevalent form of DM, which poses huge economic burden to all nations, especially the developing countries, which are accounting for more than 80% of reported cases of T2DM [2]. New generation antidiabetic drugs chiefly, α-glucosidase inhibitors, insulin sensitizers, GLP-1 agonists and DPP-4 inhibitors have been developed for effective control and management of T2DM [3].
Glucagon-like peptide (GLP-1) is physiologically important regulators of metabolic control and is an important hormone that stimulates the secretion of glucose-dependent insulin from pancreatic 훽-cells. This endocrine hormone of 30-amino acids is produced in the enteroendocrine L-cells [4]. Is has been reported that the continuous GLP-1 treatment in T2DM improve β-cell function, normalizes blood glucose and restore first-phase insulin secretion and “glucose competence” to β-cells; hence, GLP-1/GLP-1Rs are therapeutic targets for treating T2DM [5]. Recently GLP-1 analogs such as Exenatide, Liraglutide, Metformin etc. have been introduced for therapeutic intervention. However, there are many side effects of these drugs like fluid retention, weight gain, headache, upper respiratory tract infection and urinary tract infection.
The side effects and costly treatment associated with current day antidiabetic drugs, necessitated search for alternate remedy for the treatment of DM. Since ancient times, medicinal plants and their extracts have been effectively used as first line therapy to combat diabetes but are yet to be commercially formulated as modern medicines [6]. Traditional alternative medicine involves the use of herbs and their products as alternatives to chemical drugs.
Momordica charantia (MC) commonly known as bitter melon belongs to the family Cucurbitaceae is a tropical herbaceous vegatable used for management of DM throughout the world [7, 8]. The antidiabetic effects of MC have been extensively reviewed [9,10,11]. The possible mechanisms reported include protection of islet 훽-cells [12], increasing insulin secretion [13], inhibition of intestinal 훼-glucosidase [14], and glucose transport [15], activation of AMPK [16, 17], improving insulin resistance [18, 19] and increasing hepatic glucose disposal and decreasing gluconeogenesis [20, 21]. Charantin substance extracted from MC showed hypoglycaemic effect on normal and diabetic rabbits [22]. Bitter melon has been found to increase insulin sensitivity [23]. Decrease in blood glucose, cholesterol and triglycerides through a decrement in PKC-β activity was reported in diabetic rats induced by streptozotocin when MC juice was administered at 6 mL/kg [24]. At the dosage of 375 mg/kg, methanolic fruit extract of MC decreased the fasting blood glucose (FBG) after 12 h in alloxan-induced diabetic rats [25].
In this study, we probed the effects of oral administration of aqueous extract of Momordica charantia (AEMC) on fasting blood glucose (FBG), tissue glycogen, glycosylated haemoglobin, serum insulin and GLP-1 in diabetic Wistar rats.
Methods
Plant material and its extraction
The fruit of M. charantia was purchased from local market. The sample were taken to the Herbarium in Department of Botany, Bundelkhand University, Jhansi, where Dr. Rajdeep Kudesia, confirm its identification and a voucher specimen number (BU-MC- 00712) was placed in the Herbarium. The dried fruit was grinded into powder using grinder and extracted with double distilled water (1:3) by stirring whole night using homogenizer. The extract was filtered and then centrifuged (3000 x g, 10 min) for further purification. The supernatant was further lyophilized for complete dryness to obtain Aqueous Extract of M. charantia.
Chemicals
Streptozoticin (STZ) from Sigma Aldrich was used to induce diabetes. All chemicals and solvents used in this study were purchased from different companies like Merck, Himedia, Rankem, Qualikems, Loba, Sigma and other chemical companies of analytical grade.
Animals
Two to three months old adult male Wistar rats weighing about 200–250 g (average = 235.5 ± 4.27 g) were purchased from animal DRDE, Gawlior (India). Rats were individually housed in stainless steel wire cages in an animal room with a light: dark cycle (12:12) and temperature (22 ± 2 °C). The Animals were fed pellet diet and water ad-libitum. All procedures described in this study were performed in accordance to the guidelines of Institutional Animal Ethical Committee (BU/ Pharma/ IAEC/12/031).
Induction of diabetes
In overnight fasted animals, diabetes was induced at 7 am by a single intraperitoneal injection of a freshly prepared solution of streptozotocin (50 mg/kg b.w) in a 0.1 M citrate buffer (pH 4.5). On the third day of STZ-injection, the animals with signs of polyuria and polydipsia and with fasting glycemia (> 200 mg/dl) were considered to be diabetic and included in the study [26].
Treatment schedule
In the experiment, the rats were randomly divided into 4 groups (n = 6/group) as per treatment schedule given below.
Group I (n = 6) Normal Control
Group II (n = 6) Normal treated with AEMC @ 300mg/kg body weight
Group III (n = 6) Diabetic control
Group IV (n = 6) Diabetic treated with AEMC @ 300mg/kg body weight
The control group was given 0.9% normal saline, intramuscularly. Single dose of AEMC was given orally on daily basis for 28 days. Acute study of GLP-1 and serum insulin was done from blood serum in single dose administration of AEMC on first day of experiment. The blood samples were obtained from tail vein at the interval of 0, 20, 30, 40, 50, and 60 min, whereas the sub-chronic study was done following same procedure after 28 days’ administration of AEMC. The 0 min reading indicates taking blood for the estimation of GLP-1 and serum insulin without giving the treatment of AEMC. At the end of the experimental period (after 28 days of treatment), the rats were anaesthetized by chloroform inhalation followed by cervical dislocation and sacrificed as per the guidelines of Institutional Animal Ethics Committee (IAEC). A midline incision was performed at the thoracic region on 29th day of treatment. Trunk blood was collected in heparinized tubes and the plasma was obtained by centrifugation at 5000 rpm for 5 min for the determination of biochemical parameters. The liver and muscle tissues were collected from each group of rats and used for estimation of free and fixed Glycogen.
Fasting Blood Glucose (FBG)
The blood glucose level of animals was estimated on 0, 14th and 28th day by Glucose Oxidase–Peroxidase Enzymatic Method using a digital glucometer (ACCU-CHEK brand active).
Glycosilated Haemoglobin (HbA1C)
Glycosylated haemoglobin was estimated by Euro diagnostic system kit based on photometric test at 415 nm using ion exchange resin [27,28,29].
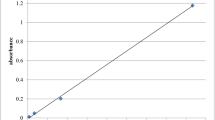
Tissue glycogen
This estimation indicates the distinction between free and fixed glycogen content in tissues by using the Anthrone reagent. Immediately after the excision of liver and muscle tissues, 1 g of the tissue were digested within 2 mL of 30% boiling potassium hydroxide (KOH) solution and cooled, and following this 3 mL of 95% ethanol was added and heated until the tissues gets dissolved. Mixtures were cooled and centrifuged at 1000 rpm for 5 min, the supernatant was discarded. The residual material was dissolved in 2 mL of distilled water, and then 10 mL of Anthrone reagent was added and immersed in ice bath to prevent excessive healing. The Tubes were incubated at 100 °C for 4 min for color development and immersed in an ice bath. The absorbance was measured at 620 nm using spectrophotometer.
Serum insulin
The serum insulin concentrations were measured by an enzyme linked immunosorbent assay (ELISA) method using an ultrasensitive rat insulin ELISA kit (Mercodia, Uppsala, Sweden) in a multi plate ELISA reader (Biorad-680, BIORAD Ltd., Japan).
Glucagon-Like Peptide-1 (GLP-1)
GLP-1were determined by Ray Bio® Rat GLP-1 ELISA kit given by Toft-Neilsen [30] and Meier et al. [31].
Statistical analysis
All data were presented as the mean ± SEM. The groups were compared by one-way ANOVA analysis. Data were analyzed by using a statistical software package (SPSS for Windows, version 18) using Tukey’s-HSD multiple range post hoc test. Values were considered significantly different at p < 0.05.
Results
Effect of M. charantia on FBG level in normal and diabetic rats
Oral administration of AEMC 300 mg/kg/day b.w. in normal rats showed non-significant (P > 0.05) decrease in FBG on 14 day (5.2%) and 28 day (10.46%) as compared to 0 day in group II, whereas, no change was observed in group I and group III. However, FBG levels showed significant (P < 0.01) decrease in group IV on 14 day (41.42%) and 28 day (69.57%) as compared to 0 day readings. On comparing group I with group III, significant increase (P < 0.01) in FBG was observed in group III on 14 day (176.16%) and 28 day (286%). However non-significant (P > 0.05) decrease in FBG was found on 14 day (23.35%), followed by significant (P < 0.01) decrease at 28 day (70.23%) in group IV as compared to group I. At the end of treatment, significant reduction was observed on 14 and 28 day in relation to diabetic control (Group III) (Table 1).
Effect of M. charantia on liver glycogen, muscle glycogen and glycosylated haemoglobin in normal and diabetic rats
The effect of AEMC on the Liver Glycogen, Muscle Glycogen and Glycosylated Haemoglobin level of normal and diabetic rats is presented in Table 2. After administration of AEMC in normal rats, liver glycogen level was non-significantly (P < 0.05) increased (3.97%) in group II, whereas, significant (P < 0.01) decrease was observed (65.16%) in group III compared to group I. However, level of liver glycogen increased significantly (P < 0.01) in Group IV (171.42%) when compared to group III. Non-significant (P < 0.05) increase in muscle glycogen was found (6.37%) in group II. On contrary, significant (P < 0.01) decrease in muscle glycogen was reported in group III (58.48%) when compared to group I. However, muscle glycogen in AEMC treated groups increased significantly (P < 0.01) in group IV (110.36%) as compared to group III. The level of HbA1C decreased (9.48%) non-significantly (P > 0.05) in group II, whereas in diabetic control the HbA1C showed significant (P < 0.01) increase in group III (305.33%) as compared to group I. The diabetic rats when treated with AEMC, the HbA1C percentage significantly (P < 0.01) decreased in group IV (65.7%) when compared to group III.
Effect of single dose of AEMC on serum insulin level in normal and diabetic rats
Despite that the serum insulin levels were not significantly different (P > 0.05) at each time points (Table 3), except, 20 min where serum level was significantly higher in all groups, compared to that at 0 min. In group II, non-significant (P > 0.05) increase in serum insulin was observed on administration of AEMC at 20 min (6.41%), and tries to compensate towards normal at 60 min (1.41%). However, in group IV significant (P < 0.05) increase (85.36%) was observed at 20 min followed by non-significant increase (P > 0.05) at 30 min (75%), which again non-significantly falls towards normal at 60 mins (1.62%). Furthermore, significant (P < 0.05) change in serum insulin was observed at each time point (20 min 64.0%, 30 min 18.07%, 40 min 15.67%, 50 min 15.38%, and 60 min 0.0%) in group IV when compared to group III.
Effect of sub-chronic administration of M. charantiaon serum insulin level in normal and diabetic rats
On sub-chronic administration of AEMC in normal rats, non-significant (P > 0.05) increase in serum insulin was also observed on administration of AEMC at 20 min (23.3 and 85.1%) and falls towards normal at 60 min (0.40 and 8.15%) in comparison to 0 min in group II and group IV respectively. Significant (P < 0.01) increase in serum insulin level was observed (20 min 275.5%, 30 min 229.4%, 40 min 202.2%, 50 min 158.4% and 60 min 144%) in group IV as compared to group III (Table 4).
Effect of single dose of M. charantia on GLP-1 level in normal and diabetic rats
In the present investigation during short term administration of AEMC, GLP-1 level increased significantly (P < 0.01) at 20 min (64.6 and 111.46%) and non-significantly (P > 0.05) at 60 min (6.61 and 15.77%) in group II and group IV, respectively, when compared to 0 min readings (Table 5). The GLP-1 level showed significant (P < 0.01) decrease at 20 min (35.13%), 30 min (39.8%), 40 min (47.79%), 50 min (48.79%) and 60 min (51.4%) in group III as compared with group I. however, significant (P < 0.05) increase in GLP-1 was observed (20 min 19.67%, 30 min 19.52%, 40 min 19.41%, 50 min 18.26% and 60 min 14%) in group IV on comparison with group III.
Effect of long term exposure of M. charantia on GLP-1 level in normal and diabetic rats
Significant (P < 0.01) increase in GLP-1 in sub-chronic experiment was observed at 20 min (51.82%) and tends to be normalize at 60 min (6.61%) in comparison to 0 min in group II. However significant increase in GLP-1 level was depicted at 20 min (306.9%) and then falls towards normal at 60 min (16.5%) in comparison with 0 min in group IV. Long term administration of AEMC in diabetic rats results significant (P < 0.05) increase in GLP-1 level from (20mins 306.18%, 30mins 238.18%, 40mins 144.97%, 50mins 62.89%, and 60mins 16.50%) in group V, on comparison with group IV Table 6.
Discussion
Our hypothesis that AEMC might exert an incretin effect was supported by data obtained in this study. Fasting blood glucose levels in the normal control group remained unchanged throughout the experimental work. Administration of AEMC to normal rats showed reduction in blood sugar levels from day 1 to day 28. But in case of diabetic treated groups the blood sugar level reached near to normal control within 28 days of experiment. The antidiabetic effect of AEMC may be due to increased utilization of glucose, decreased absorption of glucose from GI tract, control on the insulin secretion or inhibition of the α-glucosidase activity.
AEMC has been reported to inhibit absorption of glucose by inhibiting α-glucosidase and suppressing the activity of disaccharidases in the intestine [32]. Whereas Lal et al. [33] experiment on diabetic rats, reported the hypoglycemic activity of AEMC. Results of other scientists [22, 34, 35] on AEMC treatment are also in conformity with the present work.
The Glycosylated hemoglobin (HbA1c) assay has become the most commonly used measure of chronic glycaemia in epidemiological studies, clinical trials and the management of diabetes. In the present study, the diabetic rats have shown significant increase in HbA1c level as compared to normal control which indicates that diabetic rats have poor glycemic control. The long term administration of aqueous extracts AEMC in diabetic rats results a significant decrease in the HbA1c levels in the diabetic rats, but no significant difference in HbA1c percentage found in normal treated groups. HbA1c levels which were noted in consistent with other reports may be due to low plasma level of insulin or high glucose utilization in the peripheral tissues as reported in the present work. The various experimental reports obtained from recent papers on AEMC [22] and in Elaeodendron glaucum [36] concords with our results.
It is well known that in diabetes mellitus there will be marked depletion in glycogen storage in hepatic cells and muscle cells in diabetic rats. Liver glycogen and muscle glycogen is drastically reduced in diabetic group and on administration of AEMC for 28 days in the normal and diabetic rats corrects the glycogen level, but not equivalent to normal control group. The decrease in tissue glycogen may be due to enhanced catabolic process such as glycogenolysis, lipolysis and proteolysis, which are the outcomes of lack of insulin or oxidative stress by diabetes may inactive the oxygen synthase or decrease in GLUT4 transporter protein of muscles and cellular glucose in liver cells. Previous studies have validated that a number of plant materials induced an antidiabetic activity partly through stimulation of hepatic glycogenesis [37, 38]. Thus, the significantly higher liver glycogen content recorded in the Diabetic treated (Group IV) compared to the diabetic control (Group III) specified that AEMC was mediated by stimulating insulin secretion, retarding carbohydrates digestion, or by increasing hepatic glycogen synthesis.
In present investigation diabetic group showed low insulin level than control group which indicates the β-cell failure in diabetic rats. The insulin level increased non-significantly 20 to 60 min in short term administration of AEMC, but in diabetic AEMC treated serum insulin increased significantly. The possible mechanism behind the increase in insulin secretion in acute administration of AEMC might have increased the activity of β-cell receptors or showed insulin like activity, or decreases blood glucose concentrations by acting on GLUT-4. In sub-chronic administration of AEMC, the serum insulin level in diabetic treated groups increased as compared to diabetic group. Serum insulin was also increased in the normal AEMC treated rats. These results are in agreement with the findings of Rotshteyn and Zito [39] and Fernandes et al. [22]. This significant change in serum insulin level in long term exposure of AEMC might be due to increasing the number of β-cell receptors or β-cell proliferation. These results also suggest that AEMC increases the renewal and number of β cells in the pancreas as compared to untreated diabetic rats or may permit the recovery of STZ destroyed β cells and stimulates pancreatic insulin secretion [40]. In support with the present study the elevation of insulin levels was also observed with the administration of AEMC by other authors [36, 41].
Increase in GLP-1 level, from 0 to 60 min was observed in normal and diabetic rats in both short term and long term treatment with AEMC. In diabetic rats highest increase in GLP-1 level was at 20 min of AEMC administration, as compared to 0 min. The results also suggest that induction of GLP-1 on administration of AEMC was more pronounced in diabetic rats as compared to normal. It is possible that in normal rats high increase in GLP-1 is prohibited due to normal physiology and normal level of glucose regulating hormones including GLP-1. Since there is decrease in insulin as well as GLP-1 in diabetic rats, GLP-1 induction is more pounced to decrease enhanced glucose level. These findings indicate that the GLP-1 level is highly significant in sub-chronic administration of AEMC compared to acute administration of AEMC. The Mechanism of elevation of GLP-1 on sub-chronic administration of AEMC in normal and diabetic rats may be due to increased L-cell receptors or L-cell regeneration. The secretion of GLP-1 by AEMC may be due to the presence of sugars, amino acids, small peptides, water soluble alkaloids and plant secondary metabolites, which are known to stimulate GLP-1 secretion [42]. These nutrient molecules activate the enteroendocrine cells of gut by G-protein coupled receptors [43].
In support with the present study Cicero and Tartagni [44] reported that administration of Beriberis plant at the dose of 500 mg/kg bw, showed that Berberine is an alkaloid present in Beriberis plant that affects glucose metabolism, increasing insulin secretion, stimulating glycolysis, Berberine also increases glucose transporter-4 (GLUT-4) and GLP-1 levels. Other results in support of increase in GLP-1 were observed in Smallanthus sonchifolius [45], Agave tequilana Gto. and Dasylirion spp. [46], Ilex paraguariensis [47], Cinnamomum zeylanicum [48], Pinus koraiensis [49], Glycine max [50] and Berberis [45].
Conclusion
Results of present study supported the traditional use of aqueous extract of M. charantia significantly for the hypoglycemic action in the management of diabetes.
Change history
12 June 2018
Following publication of the original article [1], the authors reported that there was an error in the acknowledgements.
06 June 2018
Following publication of the original article [1], the authors reported that there was an error in the acknowledgements. In this Correction, the incorrect and correct acknowledgements are shown.
Abbreviations
- AEMC:
-
Aqueous extract of Momordica charantia
- AMPK:
-
Adenosine monophosphate activated protein kinase
- ANOVA:
-
Analysis of variance
- DM:
-
Diabetes mellitus
- DPP:
-
Dipeptidyl peptidase
- DRDE:
-
Defence research & development establishment
- ELISA:
-
Enzyme linked immunosorbent assay
- FBG:
-
Fasting blood glucose
- GI:
-
Gastrointestinal
- GLP-1:
-
Glucagon like peptide
- GLUT:
-
Glucose transporter
- HbA1C:
-
Glycosilated haemoglobin
- IAEC:
-
Institutional animal ethics committee
- KOH:
-
Potassium hydroxide
- PKC:
-
Protein kinase-C
- STZ:
-
Streptozoticin
- T2DM:
-
Type 2 diabetes mellitus
References
Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–7.
Unwin N, Whiting D, Gan D, Jacqmain O, Ghyoot G. IDF Diabetes Atlas. 4th ed. Brussels: International Diabetes Federation; 2009.
Raptis SA, Dimitriadis GD. Oral hypoglycemic agents: insulin secretagogues, alpha-glucosidase inhibitors and insulin sensitizers. Exp Clin Endocrinol Diabetes. 2001;109:265–87.
Huang TN, Lu KN, Pai YP, Chin H, Huan CJ. Role of GLP-1 in the hypoglycemi effects of wild bitter gourd. Evid Base Complement Alternat Med. 2013;625892:1-13.
Holz GG, Kühtreiber WM, Habener JF. Pancreatic beta-cells are rendered glucose-competent by the insulinotropic hormone glucagon-like peptide-1(7-37). Nature. 1993;361:362–5.
Wadkar KA, Magdum CS, Patil SS, Naikwade NS. Antidiabetic potential and Indian medicinal plants. J Herbal Med Toxicol. 2008;2:45–50.
Cefalu WT, Ye J, Wang ZQ. Efficacy of dietary supplementation with botanicals on carbohydrate metabolism in humans. Endocr Metab Immune Disord Drug Targets. 2008;8:78–81.
Joseph B, Jini D. Antidiabetic effects of Momordica charantia (bitter melon) and itsmedicinal potency. Asian Pac J Trop Dis. 2013;3:93–102.
Basch E, Gabardi S, Ulbricht C. Bittermelon (Momordica charantia): a review of efficacy and safety. Am J Health Syst Pharm. 2003;4:356–9.
Grover JK, Yadav SP. Pharmacological actions and potential uses of Momordica charantia: a review. J Ethnopharmacol. 2004;93(1):123–32.
Krawinkel MB, Keding GB. Bitter gourd (Momordica charantia): a dietary approach to hyperglycemia. Nutr Rev. 2006;64(7):331–7.
Ahmed I, Adeghate E, Sharma AK, Pallot DJ, Singh J. Effects of Momordica charantia fruit juice on islet morphology in the pancreas of the streptozotocin-diabetic rat. Diabetes Res Clin Pract. 1998;40(3):145–51.
Keller AC, Ma J, Kavalier A, He K, Brillantes AM, Kennelly EJ. Saponins from the traditional medicinal plant Momordica charantia stimulate insulin secretion in vitro. Phytomedicine. 2011;19(1):32–7.
Uebanso T, Arai H, Taketani Y, Fukaya M, Yamamoto H, Mizuno A, Uryu K, Hada T, Takeda E. Extracts of Momordica charantia suppress postprandial hyperglycemia in rats. J Nutr Sci Vitaminol. 2007;6:482–8.
Mahomoodally MF, Gurib-Fakim A, Subratty AH. Effect of exogenous ATP on Momordica charantia Linn.(Cucurbitaceae) induced inhibition of d-glucose, l-tyrosine and fluid transport across rat everted intestinal sacs in vitro. J Ethnopharmacol. 2007;110(2):257–63.
Tan MJ, Ye JM, Turner N, Hohnen-Behrens C, Ke CQ, Tang CP, Chen T, Weiss HC, Gesing ER, Rowland A, James DE, Ye Y. Antidiabetic activities of triterpenoids isolated from bitter melon associated with activation of the AMPK pathway. Chem Biol. 2008;15(3):263–73.
Cheng HL, Huang HK, Chang CI, Tsai CP, Chou CH. A cell-based screening identifies compounds from the stem of Momordica charantia that overcome insulin resistance and activate AMP-activated protein kinase. J Agric Food Chem. 2008;56(16):6835–43.
Shih CC, Lin CH, Lin WL, Wu JB. Momordica charantia extract on insulin resistance and the skeletal muscle GLUT4 protein in fructose-fed rats. J Ethnopharmacol. 2009;1:82–90.
Wang ZQ, Zhang XH, Yu Y. Bioactives from bitter melon enhance insulin signaling and modulate acyl carnitine content in skeletal muscle in high-fat diet-fed mice. J Nutr Biochem. 2011;22(11):1064–73.
Sarkar S, Pranava M, Marita RA. Demonstration of the hypoglycemic action of Momordica charantia in a validated animal model of diabetes. Pharmacol Res. 1996;33(1):1–4.
Fernandes NPC, Lagishetty CV, Panda VS, Naik SR. An experimental evaluation of the antidiabetic and antilipidemic properties of a standardized Momordica charantia fruit extract. BMC Complement Altern Med. 2007;7:29.
Lolitkar MM, Rao MRR. Note on a Hypoglycaemic principle isolated from the fruits of Momordica charantia. J Uni Bombay. 1962;29:223–4.
Sridhar MG, Vinayagamoorthi R, Suyambunathan VA, Bobby Z, Selvaraj N. Bitter gourd (Momordica charantia) improves insulin sensitivity by increasing skeletal muscle insulin-stimulated IRS-1 tyrosine phosphorylation in high-fat-fed rats. British J Nutr. 2008;99:806–12.
Kolawole OT, Ayankunle AA. Seasonal variation in the anti-diabetic and hypolipidemic effects of Momordica charantia fruit extract in rats. EJMP. 2012;2:177–85.
Nkambo W, Anyama NG, Onegi B. In vivo hypoglycemic effect of methanolic fruit extract of Momordica charantia. L. Afr Health Sci. 2013;13:933–9.
Vasconcelos CFB, Maranhão HML, Batista TM, Carneiro EM, Ferreira F, Costa J, Soares LAL, Sá MDC, Souza TP, Wanderley AG. Hypoglycaemic activity and molecular mechanisms of Caesalpinia ferrea Martius bark extract on streptozotocin-induced diabetes in Wistar rats. J Ethnopharmacol. 2011;137:1533–41.
Trivelli LA, Ranney HM, Lai HT. Hemoglobin components in patients with diabetes mellitus. New Eng J Med. 1971;284:357.
Nathan DM, Singer DE, Hurxthal K, Goodson JD. The clinical information value of the glycosylated hemoglobin assay. N Engl J Med. 1984;310:341–6.
Bunn HF. Evaluation of glycosylated hemoglobin in diabetic patients. Diabetes. 1981;30:613–7.
Toft-Nielsen M, Madsbad S, Holst J. Determints of the effectiveness of glucagon-like peptide-1 in type 2 diabetes. J Clin Endocrinol Metab. 2001;86:3853–60.
Meier J, Weyhe D, Michaely M, Senkal M, Zumtobel V, Nauck M, Holst J, Schmidt W, Gallwitz B. Intervenous glucagon-l-like peptide 1 normalizes blood glucose after major surgery in patients with type 2 diabetes. Crit Care Med. 2004;32:848–51.
Chaturvedi P. Antidiabetic potentials of Momordica charantia: multiple mechanisms behind the effects. J Med Food. 2012;15:101–7.
Lal VK, Gupta PP, Tripathi P, Pandey A. Interaction of aqueous extract of Momordica charantia fruits with Glibenclamide in Streptozotocin induced diabetic rats. American. J Pharmacol Toxicol. 2011;6:102–6.
Matheka DM, Alkizim FO, Kiama TN, Bukachi F. Glucose-lowering effects of Momordica charantia (Karela) extract in diabetic rats. AJPT. 2012;1:62–6.
Nagy MA, Bastawy MA, Abdel-Hamid NM. Effects of Momordica charantia on Streptozotocin-induced diabetes in rats: role of insulin, oxidative stress and nitric oxide. J Health Sci. 2012;2:8–13.
Lanjhiyana S, Garabadu D, Ahirwar D, Bigoniya P, Rana A, Patra K, Lanjhiyana S, Karuppaih MP. Antidiabetic activity of methanolic extract of stem bark of Elaeodendron glaucum Pers. in Alloxanized rat model. Adv Appl Sci Res. 2011;2:47–62.
Habibuddin M, Daghriri HA, Humaira T, AlQahtani MS, Hefzi AA. Antidiabetic effect of alcoholic extract of Caralluma sinaica L. on streptozotocin- induced diabetic rabbits. J Ethnopharmacol. 2008;117:215–20.
Jain S, Bhatia G, Barik R, Kumar P, Jain A, Dixit VK. Antidiabetic activity of Paspalum scrobiculatum Linn. In alloxan induced diabetic rats. J Ethnopharmacol. 2010;127:325–8.
Rotshteyn Y, Zito SW. Application of modified in vitro screening procedure for identifying herbals possessing sulfonylurea-like activity. J Ethnopharmacol. 2004;9:337–44.
Kumar DS, Sharathnath KV, Yogeswaran P, Harani A, Sudhakar K, Sudha P, Banji D. A medicinal potency of Momordica charantia. Int J Pharma Sci Rev Res. 2010;1:95–100.
Saha SK, Haque E, Islam D, Rahman M, Islam R, Parvin A, Rahman S. Comparative study between the effect of Momordica charantia (wild and hybrid variety) on hypoglycemic and hypolipidemic activity of alloxan induced type 2 diabetic long-evans rats. J Diabetes Mellitus. 2012;2:131–7.
Ramos SM, Tovar AR, Torres N. Diet: friend or foe of enteroendocrine cells–how it interacts with enteroendocrine cells. Adv Nutr. 2012;3:8–20.
Reimann F, Tolhurst G, Gribble FM. G-protein-coupled receptors in intestinal chemo-sensation. Cell Metabol. 2012;15:421–31.
Cicero AF, Tartagni E. Antidiabetic properties of berberine: from cellular pharmacology to clinical effects. Hosp Pract (Minneap). 2012;40:56–63.
Habib NC, Honoré SM, Genta SB, Sánchez SS. Hypolipidemic effect of Smallanthus sonchifolius (yacon) roots on diabetic rats. Chem Biol Interact. 2011;194:31–9.
Silvas UJE, Cani PD, Delmée E, Neyrinck A, López MG, Delzenne NM. Physiological effects of dietary fructans extracted from Agave tequilana Gto. And Dasylirion spp.Unidad de Biotecnología e Ingeniería Genética de Plantas, México. Br J Nutr. 2008;99:254–61.
Hussein GM, Matsuda H, Nakamura S, Hamao M, Akiyama T, Yoshikawa TK. Mate tea (Ilex paraguariensis) promotes satiety and body weight lowering in mice: involvement of glucagon-like peptide-1. Biol Pharm Bull. 2011;34:1849–55.
Hlebowicz J, Hlebowicz A, Lindstedt S, Björgell O, Höglund P, Holst JJ, Darwiche G, Almér LO. Effects of 1 and 3 g cinnamon on gastric emptying, satiety, and postprandial blood glucose, insulin, glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, and ghrelin concentrations in healthy subjects. Am J Clin Nutr. 2009;89:815–21.
Pasman WJ, Heimerikx J, Rubingh CM, Berg R, O'Shea M, Gambelli L, Hendriks HF, Einerhand AW, Scott C, Keizer HG, Mennen LI. The effect of Korean pine nut oil on in vitro CCK release, on appetite sensations and on gut hormones in post-menopausal overweight women. Lipids Health Dis. 2008;20:10.
Park S, Ahn IS, Kim JH, Lee MR, Kim JS, Kim HJ. Glyceollins, one of the phytoalexins derived from soybeans under fungal stress, enhance insulin sensitivity and exert insulinotropic actions. J Agric Food Chem. 2010;58:1551–7.
Acknowledgements
We are thankful to Department of zoology, Hemvati Nandan Bahuguna Central University Garhwal Uttarakhand, India, for providing necessary facilities.
Funding
The authors would like to express their sincere appreciation to the Deanship of Scientific Research at the King Saud University, Riyadh, Saudi Arabia for funding this Research Group project no RGP-009.
Availability of data and materials
The data that support the findings of this study are available from [Gulzar Ahmad Bhat (first author)] who is writing his thesis based on the current study, so are not publicly available as of now. Data will, however, be available from the authors upon reasonable request and with permission of [Gulzar Ahmad Bhat] after submission of the thesis.
Author information
Authors and Affiliations
Contributions
GAB carried out the experiments and assisted with data analysis. HAK and ASA secured funding for project and help in manuscript preparation. PS participated in the design of the study. RS did extract preparation and assisted with manuscript preparation. BAP carried out subject recruitment, data collection, coordination of the study and compliance. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures described in this study were performed in accordance to the guidelines of Institutional Animal Ethical Committee (BU/ Pharma/ IAEC/12/031).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
The original version of this article was revised: the affiliation of one of the author Rambir Singh had been listed incorrectly. It should be Department of Biomedical Sciences, not Department of Biological Sciences.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bhat, G.A., Khan, H.A., Alhomida, A.S. et al. GLP-I secretion in healthy and diabetic Wistar rats in response to aqueous extract of Momordica charantia. BMC Complement Altern Med 18, 162 (2018). https://doi.org/10.1186/s12906-018-2227-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-018-2227-4