Abstract
Background
Cancer patients often suffer from emotional distress as a result of the oncological process. The purpose of our study was to determine whether practice of Jacobson’s relaxation technique reduced consumption of psychotropic and analgesic drugs in a sample of cancer patients.
Methods
This was a multicenter pre–post intervention design. Participants were 272 patients aged over 18 years attending 10 Spanish public hospitals with oncological pathologies and anxiety symptoms. The intervention consisted of a protocol of abbreviated progressive muscle relaxation training developed by Bernstein and Borkovec. This was followed up by telephone calls over a 1-month period. The intervention was performed between November 2014 and October 2015. Sociodemographic variables related to the oncological process, mental health variables, and intervention characteristics were measured.
Results
A reduction in the consumption of psychotropic and analgesic drugs was observed throughout the follow-up period. Improvement was observed throughout the 4-week follow-up for all the parameters assessed: anxiety, relaxation, concentration, and mastery of the relaxation technique.
Conclusions
The practice of abbreviated Jacobson’s relaxation technique can help to decrease the consumption of psychotropic and analgesic drugs. Patients experienced positive changes in all the evaluated parameters, at least during the 1-month follow-up. To confirm these findings, additional long-term studies are needed that include control groups.
Trial registration
ISRCTN 81335752, DOI 10.1186/ISRCTN81335752 17. Date of registration: 22/11/2016 (retrospectively registered).
Similar content being viewed by others
Background
It has been estimated that between 20% and 50% of patients with cancer experience pain [1] and this estimate increases to up to 90% when the illness is very advanced [2]. Furthermore, approximately 30% of patients experience emotional distress during the course of treatment [3, 4].
The management of oncological pain is particularly difficult and although different recommendations exist, there is currently no clear consensus. The World Health Organization, the American Cancer Society, and the European Society for Medical Oncology mention in their guidelines on managing cancer pain the importance of medications (aside from analgesic treatment) such as psychotropic drugs, although they stipulate that these should be taken only for pain that may otherwise be unmanageable or difficult to control [5,6,7]. Despite following these recommendations, a high percentage of patients cannot control their pain. A literature review by Deandrea et al. [8] reported that approximately 43.4% are unable to control their pain and some sources suggest that this figure may be as high as 80%.
Cancer patients often experience emotional distress, such as anxiety and depression, and may consume psychotropic drugs to manage both pain and emotional symptoms [9,10,11].
Previous studies indicate that the consumption of psychotropic drugs, especially anxiolytics and antidepressants, is high among cancer patients. Syrowatka et al. [12] reported a consumption of 50.6% of anxiolytics in women with breast cancer. Barry et al. [13] found that 51% of patients with metastasis cancer took anxiolytics for pain during the active treatment phase. The consumption of antidepressants has been reported as between 10% and 64% [12,13,14]. Thus, research indicates that a large number of patients consume three or more psychotropic drugs [13].
It is clear, therefore, that consumption of a combination of analgesic and psychotropic drugs is common in cancer patients. Indeed, Kierner et al. [15] reported that the prevalence of consumption of psychotropic drugs and analgesics was as high as 75% and 90%, respectively, during the final illness phases. These results suggest that consumption increases with the evolution of the illness.
Polypharmacy in oncological patients is therefore a problem. In addition, although cancer patients may take a range of drugs, they may not always manage to control their symptoms.
Oncological patients are often treated with a range of drugs (e.g., anticancer, antiemetic, psychopharmaceutical, and analgesic drugs), which increases the risk of drug interactions and adverse effects [16]. The risks of polypharmacy also include an increase in episodes of falls, frailty, hospitalization, postoperative complications, and even higher mortality [16]. All these problems can lead to greater disability and lower patient autonomy, particularly for older patients [17].
This evidence highlights the need for strategies that can control pain and emotional distress in patients undergoing complex oncological processes but that help to decrease polypharmacy as much as possible.
There is evidence that complementary therapies, such as muscle relaxation, are effective in improving the quality of life of patients with cancer [18,19,20,21,22,23,24,25,26]. However, there is a lack of research on the effect of such therapies on pain and the consumption of psychotropic drugs and analgesics in cancer patients.
Therefore, the aim of this study was to determine whether the practice of Jacobson’s relaxation technique reduced consumption of psychotropic and analgesic drugs in a sample of cancer patients.
Methods
Design
This was a multicenter pre–post intervention study. The study was conducted in accordance with the CONSORT guidelines.
Participants
The study was conducted between November 1, 2014, and October 1, 2015, in the oncological units of 10 Spanish public hospitals. Patient recruitment took place in these units using posters, informative flyers, and information provided to relevant health professionals (oncologists, nurses, and psychologists). Cancer patients exhibiting anxiety, muscular tension, sleeping difficulties, sadness, or anxiety attacks, and who agreed to participate, were recruited. The exclusion criteria were patients exhibiting hallucinations, delirium, or other psychotic symptoms, because the practice of muscle relaxation can lead to potentially unpleasant extracorporeal sensations.
Data collection
The following participant data were collected: 1) sociodemographic and medical characteristics: medical center, age, gender, marital status, and educational level; 2) oncological process: cancer diagnosis, cancer therapy (chemotherapy, radiotherapy, hormone therapy, biological therapy, and surgery), any side effects of the cancer treatment, cancer pain, and analgesic use; 3) mental health issues: use of anxiolytics, hypnotics, and antidepressants; 4) other variables related to the intervention, such as symptoms motivating inclusion in the study and questions such as “Have you practiced the technique at home?” or “What is the frequency, per week, that you practice the technique?” Participants were also asked whether the technique helped them control the anxiety and pain. Finally, the level of anxiety prior to the session was recorded, together with the degree of relaxation achieved, the degree of concentration during the exercises, the command of the technique, and the level of confidence in its use.
One researcher collected data on the day of the session and once a week during the 4 weeks follow-up via phone communication.
In this study, the effect of the intervention on medication consumption could only be assessed for drugs issued as emergency prescriptions or refills.
Sample size calculation
The sample size was calculated using EPIDATA version 4.1. As different hospitals were gradually included throughout the study, we estimated the sample size based on an infinite population-based sample. With a 95% confidence level, an expected proportion of 20% of anxiety disorders in the cancer population, and a maximum error of estimation of 5%, the estimated sample size was 246 patients. An expected loss rate of 5% was assumed; therefore, the final estimated sample size was 259 patients.
Intervention
A guided session was organized for all participants to teach them the abbreviated progressive muscle relaxation training developed by Bernstein and Borkovec [27]. The sessions were conducted individually or in groups, according to the needs of each patient. To reduce possible interexaminer bias and ensure consistency in the selection criteria, all researchers conducting the intervention had been fully trained on the selection criteria, the information provided to participants, the data collection procedures, and the application of the technique. Written guidance on the relaxation sessions was distributed to all researchers. The main researcher was present at the initial treatment intervention at all hospital centers. A pilot test was performed with the initial 30 patients. Patients were seated during the performance of the technique, which took place in comfortably furnished rooms with armchairs, cushions, soothing lighting, and an overall tranquil environment. Each session lasted for approximately 1 h and consisted of an explanation of the main characteristics of the abbreviated Jacobson’s relaxation technique developed by Bernstein and Borkovec [27]; a relaxation session; an opportunity for participants to ask questions; and data collection using a data collection notebook established for this study.
Upon completion of the session, patients were given an information sheet about the intervention. This comprised a brief description of the session, based on text and images, to help them practice the technique at home.
Ethical considerations
Ethical approval was granted by the corresponding clinical research ethical committee of each center involved in the study [28] (University Hospital of Getafe, 06/26/2014; Puerta del Hierro-Majadahonda, 07/24/2014; Foundation Alcorcon, 11/03/2014; Fuenlabrada, 12/03/2014; Bellvitge, 09/10/2014; Salamanca, 07/18/2014; Navarra, 03/27/2015; Hospital Germans Trias i Pujol, 11/21/2014; and Cantabria 08/01/2014). All data were treated anonymously and confidentially according to the Spanish Personal Data Protection Act [29]. The trial was registered with ISRCTN (trial number 81335752). The clinical trial registration was postponed because the study was registered with the Spanish Agency of Medicine and, therefore, inclusion in the Spanish Registry of Clinical Studies was not required. In addition, the study sponsor considered the study to be a behavioral intervention rather than a clinical trial owing to the lack of drugs, biologics, and devices. All procedures were conducted according to the Declaration of Helsinki [30]. All participants provided written informed consent after having been fully informed about the study aims. Finally, although adverse effects from the practice of this technique have not been reported, it is important to emphasize that these types of techniques are not a substitute for medical treatment.
Data analysis
The SAS v9.3 software (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. The level of significance for statistical decision-making was set at 0.05. A descriptive univariate analysis was conducted: for qualitative variables we report percentages and 95% confidence intervals (CI) for each category; and for quantitative variables we report means and standard deviations (SD).
To determine changes in the assessed variables throughout the 4 weeks, we used adjusted models for each assessment according to the week and the initial assessment, and incorporated repeated measures of each subject throughout the entire 4-week period [31]. Logistic regression was used for qualitative variables (“Have you practiced the technique at home?”, “Do you think that the technique is helping you to control the anxiety symptoms?”, “Do you think that the technique is helping you to control the pain?”), and linear regression was used for quantitative variables (anxiety, relaxation, concentration, and mastery of the technique). We calculated estimates and 95% CIs of the mean (or percentage) for each assessment and week, and calculated adjusted contrasts using the Tukey correction to analyze differences in the variables between 2 consecutive weeks.
Results
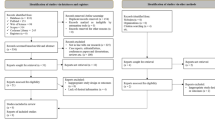
Initial recruitment comprised 272 patients from the oncological services of the participating hospitals who were experiencing anxiety, satisfied all eligibility criteria, and agreed to participate. Of these, six (2%) were excluded from the analysis, as they failed to practice the technique at home (Fig. 1).
Table 1 describes the sociodemographic characteristics, medical characteristics, and effects of the intervention for patients that practiced the technique at home. The mean age was 52.56 years [SD, 11.33 years], and 76.32% (95% CI, 71.18–81.45) of the sample were women. Up to 96.24% (95% CI, 93.94–98.54) were receiving chemotherapy treatment and 86.84% (95% CI, 82.76–90.92) reported side effects. In total, 46.62% (95% CI, 40.59–52.64) reported pain, for which 100% took an analgesic. Regarding psychotropic drugs, 31.58% (95% CI, 25.97–37.19) took anxiolytics, 12.03% (95% CI, 8.1–15.96) took antidepressants, and 21.80% (95% CI, 16.82–26.79) took hypnotics.
Table 2 shows the changes over the 4 weeks in anxiety, relaxation, concentration, and mastery of the technique, and the tests of fixed effects in the model (using the type III sum of squares test). Changes in the assessed parameters were influenced by the 4-week follow-up as a covariate and by the initial value. The anxiety level prior to the session was positively influenced by the initial value (F(1,1014) = 2464.7; p < 0.001) and negatively influenced by the 4-week follow-up (F(3,1014) = 11.66; p < 0.001). In the other models, the value of the assessed parameters was positively influenced by the initial value and by the 4-week follow-up.
Table 3 highlights the differences in estimates for the parameters evaluated for each of 2 consecutive weeks. This enabled us to follow the changes in each parameter using the estimated difference between 2 consecutive weeks. As the table shows, for all the assessed parameters, there was a statistically significant difference between at least one pair of consecutive weeks. The differences between 2 consecutive weeks were statistically significant for each pair of consecutive weeks for relaxation, concentration, and mastery of the technique.
Table 4 shows the consumption reduction for psychotropic and analgesic drugs throughout the 4 weeks of follow-up. After the intervention, a maximum of 14.71% (95% CI, 5.55–23.86) patients did not require anxiolytics after 1 week, and a maximum of 26.47% (95% CI, 15.25–37.69) patients per week required these drugs on fewer occasions.
Finally, Table 5 describes the effects of the intervention for patients who practiced the technique at home. Throughout the 4-week follow-up period, over 95% of patients had practiced the technique at home, and the mean frequency of practice per week was 6.19–6.57. Over 97% of patients each week reported that relaxation had helped them to control anxiety symptoms. Between 21.01% and 22.69 of patients with pain reported an improvement in pain control.
A maximum of 12.5% (95% CI, 4.19–26.80) patients did not require hypnotics after 1 week and a maximum of 15% (95% CI, 2.68–27.32) required them on fewer occasions. Finally, after the intervention, a maximum of 38.5% (95% CI, 0.47–13.21) patients did not require analgesics after 1 week and a maximum of 30.77% (95% CI, 17.26–44.27) required them on fewer occasions. Furthermore, a maximum of 17.31% (95% CI, 6.06–28.55) of patients reported that the analgesics were more effective.
Discussion
The practice of complementary techniques that induce relaxation can improve the quality of life of patients [18,19,20,21,22,23,24,25,26], and this can result in a decrease of the consumption of certain drugs for some patients.
Between 97.24% and 97.24% of patients who practiced the technique reported an improvement in anxiety. This led to a reduction in the consumption of anxiolytics in a maximum of 26.47% of patients after 1 week and a maximum of 14.71% of patients after 1 week did not require anxiolytic medication.
These results support previous findings by Beard et al. [23], who found statistically significant differences in pre–post anxiety measurements in groups treated with Reiki and relaxation compared with a control group. In addition, Isa et al. [24, 25] investigated the effect of muscle relaxation on anxiety and stress levels among patients with prostate cancer and reported significant differences at 4 and 6 months.
Other complementary therapies have also demonstrated effectiveness in controlling anxiety. Yoga significantly reduced both initial and final anxiety levels (measured using the State–Trait Anxiety Inventory) after an 8-week intervention [21]. A study of patients with breast cancer showed a significant improvement on Hospital Anxiety and Depression Scale scores after weekly acupuncture treatment [20]. The effect of muscle relaxation on the control of anxiety has also been studied in non-oncological patients, such as pregnant women [32], patients with dental anxiety [33], pulmonary hypertension patients [34] and schizophrenia patients [35].
None of these studies investigated the consumption of psychotropic drugs. Our findings suggest that complementary therapies could help patients to reduce the consumption of emergency or refill prescription drugs, as was the case for the patients in our sample.
Despite the fact that patients reported improvements in pain (21.01%–22.69%), this effect had a moderate impact on analgesic consumption (up to 3.85% of participants did not require these and up to 30.77% required them on fewer occasions). Notwithstanding, some patients reported that the analgesics were more effective (17.31%). Neither Beard et al. [23] nor Andersen et al. [19] (who studied muscle relaxation in cancer patients) investigated pain; however, the literature suggests that techniques that involve relaxation, such as music therapy and yoga, can improve pain control [21, 35,36,37,38,39,40,41].
Patients experienced positive changes in all the parameters studied throughout the 1-month follow-up. As patients continued to practice the technique, they experienced an increase in relaxation, concentration, mastery of the technique, and confidence in its usefulness, at least during the first month. Furthermore, anxiety levels prior to the relaxation session decreased over the weeks, suggesting a greater control over anxiety. Our relaxation protocol only included a 1-month follow-up, and we found improvements after the first week. Other similar studies [19, 23,24,25] have lasted for several weeks or months. At present, there is a lack of research on the use of this technique with similar follow-up periods in cancer patients. Thus, future studies need to assess the long-term effect of the intervention.
One of the main differences between our intervention and those used in previous studies is the simplicity of the training. Patients only required a 1-h session to learn the technique, which can be performed in a few minutes in a seated position. Furthermore, although the technique is more effective if practiced in a silent environment with dimmed light, it can be performed anywhere. Therefore, this protocol could be implemented in different hospitals, as it does not require complex resources.
Although complementary techniques are increasingly used in oncology, there are not enough studies to compare our results to; therefore, further studies on this technique are required.
This study has several strengths, such as the use of a large sample from different hospitals (i.e., this was a multicenter study) and the training of staff in the technique. However, there are potential limitations. The lack of a control group means that we cannot confirm that the results derived solely from the intervention. However, the inclusion of control/placebo groups in studies of cancer patients is a challenging procedure from an ethical perspective. In addition, patients were recruited in hospitals using informative flyers, posters, and direct information provided by health professionals caring for the patients. Therefore, we cannot confirm exactly how many prospective participants received this information. Finally, we only evaluated short-term effects of the intervention, so are unable to determine the long-term effects. Nevertheless, as the mortality rate of several cancer types included in the current study was high, this would be challenging data to obtain in future studies.
Conclusions
The practice of abbreviated Jacobson’s relaxation technique developed by Bernstein and Borkovec [27] helped to reduce the consumption of psychotropic and analgesic drugs. Patients experienced positive changes in all the evaluated parameters, at least during the 1-month follow-up. To confirm our findings, additional long-term intervention studies are needed that include control groups.
References
Fischer DJ, Villines D, Kim YO, Epstein JB, Wilkie DJ. Anxiety, depression, and pain: differences by primary cancer. Support Care Cancer. 2010;18(7):801–10.
Goudas LC, Bloch R, Gialeli-Goudas M, Lau J, Carr DB. The epidemiology of cancer pain. Cancer Investig. 2010;23(2):182–90.3.
Singer S, Das-Munshi J, Brähler E. Prevalence of mental health conditions in cancer patients in acute care--a meta-analysis. Ann Oncol. 2010;21(5):925–30.
Linden W, Vodermaier A, MacKenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141(2):343–51.
World Health Organization. Cancer Pain Relief. Geneva: World Health Organization; 1986.
Ripamonti CI, Santini D, Maranzano E, Berti M, Roila F, ESMO Guidelines Working Group. Management of cancer pain: ESMO clinical practice guidelines. Ann Oncol. 2012;23(7):54.
American Cancer Society (2015). Managing Cancer pain: other medical treatments for Cancer pain. In: American Cancer Society Web [Internet]. Atlanta, Georgia. Available from: http://www.cancer.org/treatment/treatmentsandsideeffects/physicalsideeffects/pain/other-medical-treatments-for-cancer-pain. Accessed 28 November 2016.
Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19(12):1985–91.
Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH. Mechanisms in psychosocial interventions for adults living with cancer: opportunity for integration of theory, research, and practice. J Consult Clin Psychol. 2013;81(2):318–35.
Mehnert A, Koch U, Schulz H, Wegscheider K, Weis J, Faller H, et al. Prevalence of mental disorders, psychosocial distress and need for psychosocial support in cancer patients - study protocol of an epidemiological multi-center study. BMC Psychiatry. 2012;12(1):70.
Cancer Pain (PDQ®). Health Professional Version.PDQ Supportive and Palliative Care Editorial Board. Bethesda: National Cancer Institute (US); 2002-2017.
Syrowatka A, Chang SL, Tamblyn R, Mayo NE, Meguerditchian AN. Psychotropic and opioid medication use in older patients with breast Cancer across the care trajectory: a population-based cohort study. J Natl Compr Cancer Netw. 2013;14(11):1412–9.
Barry DT, Sofuoglu M, Kerns RD, Wiechers IR, Rosenheck RA. Prevalence and correlates of coprescribing anxiolytic medications with extensive prescription opioid use in veterans health administration patients with metastatic cancer. J Opioid Manag. 2016;12(4):259–68.
Ng CG, Mohamed S, Wern TY, Haris A, Zainal NZ, Sulaiman AH. Comparison of psychotropic prescriptions between oncology and cardiology inpatients: result from a pharmacy database in a teaching hospital in Malaysia. Asian Pac J Cancer Prev. 2014;15(10):4261–4.
Kierner KA, Weixler D, Masel EK, Gartner V, Watzke HH. Polypharmacy in terminal stage of cancer. Support Care Cancer. 2016;24(5):2067–74.
Nightingale G, Skonecki E, Boparai MK. The impact of polypharmacy on patient outcomes in older adults with Cancer. Cancer J. 2017;23(4):211–8.
Pamoukdjian F, Aparicio T, Zelek L, Boubaya M, Caillet P, François V, et al. Impaired mobility, depressed mood, cognitive impairment and polypharmacy are independently associated with disability in older cancer outpatients: the prospective physical frailty in elderly Cancer patients (PF-EC) cohort study. J Geriatr Oncol. 2017 May;8(3):190–5.
Bar-Sela G, Danos S, Visel B, Mashiach T, Mitnik I. The effect of complementary and alternative medicine on quality of life, depression, anxiety, and fatigue levels among cancer patients during active oncology treatment: phase II study. Support Care Cancer. 2015;23(7):1979–85.
Andersen C, Rørth M, Ejlertsen B, Stage M, Møller T, Midtgaard J, et al. The effects of a six-week supervised multimodal exercise intervention during chemotherapy on cancer-related fatigue. Eur J Oncol Nurs. 2013;17(3):331–9.
Molassiotis A, Bardy J, Finnegan-John J, Mackereth P, Ryder DW, Filshie J, et al. Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. J Clin Oncol. 2012;30(36):4470–6.
Ulger O, Yagli NV. Effects of yoga on the quality of life in cancer patients. Complement Ther Clin Pract. 2010;16(2):60–3.
Jeon JH, Yoon J, Cho CK, Jung IC, Kim S, Lee SH, et al. Effect of acupuncture for radioactive-iodine-induced anorexia in thyroid cancer patients: a randomized, double-blinded, sham-controlled pilot study. Integr Cancer Ther. 2015;14(3):221–30.
Beard C, Stason WB, Wang Q, Manola J, Dean-Clower E, Dusek JA, et al. Effects of complementary therapies on clinical outcomes in patients being treated with radiation therapy for prostate cancer. Cancer. 2011;117(1):96–102.
Isa MR, Moy FM, Abdul Razack AH, Zainuddin ZM, Zainal NZ. Impact of applied progressive deep muscle relaxation training on the level of depression, anxiety and stress among prostate cancer patients: a quasi-experimental study. Asian Pac J Cancer Prev. 2013;14(4):2237–42.
Isa MR, Moy FM, Razack AH, Zainuddin ZM, Zainal NZ. Impact of applied progressive deep muscle relaxation training on the health related quality of life among prostate cancer patients a quasi experimental trial. Prev Med. 2013;57(Suppl):37.
Littman AJ, Bertram LC, Ceballos R, Ulrich CM, Ramaprasad J, McGregor B, et al. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: effects on quality of life and anthropometric measures. Support Care Cancer. 2012;20(2):267–77.
Bernstein DA, Borkovec T. Progressive relaxation training: a manual for the helping professions helping professions., Champaign. Illinois: Research Press; 1973.
Spanish Government Bulletin. Biomedical research act. 2007. Available from: https://www.boe.es/boe/dias/2007/07/04/pdfs/A28826-28848.pdf.
Spanish Government Bulletin. Personal data protection act. 1999. Available from: https://www.boe.es/buscar/pdf/1999/BOE-A-1999-23750-consolidado.pdf.
World Medical Association. World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull world health organ. 2001;79(4):373–374. Available from: http://www.who.int/bulletin/archives/79(4)373.pdf.
Verbeke G, Molenberghs G. (1997) linear mixed models in practice. Berlin: A SAS-Oriented Approach. Springer; 1997.
Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashanian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. J Midwifery Women Health. 2006;50:36–40.
Lundgren J, Carlsson SG, Berggren U. Relaxation versus cognitive therapies for dental fear-a psychophysiological approach. Health Psycol. 2006;25(3):267–73.
Li Y, Wang R, Tang J, Chen C, Tan L, Wu Z, et al. Progressive muscle relaxation improves anxiety and depression of pulmonary arterial hypertension patients. Evid Based Complement Alternat Med. 2015:792895.
Chen WC, Chu H, Chou YH, Chen CH, Chang YC, O'Brien AP, et al. Efficacy of progressive muscle relaxation training in reducing anxiety in patientswith acute schizophrenia. J Clinical Nursing. 2009;18:2187–96.
Payne RA. Relaxation technique. A practical handbook for the health care profesional. In: Barcelona: àidotribo; 2002.
Nelson A, Hartl W, Jauch KW, Fricchione GL, Benson H, Warshaw AL, et al. The impact of music on hypermetabolism in criticalillness. Curr Opin Clin Nutr Metab Care. 2008;11(6):790–4.
Costa A, Montalbano LM, Orlando A, Ingoglia C, Linea C, Giunta M, et al. Music for colonoscopy: a single-blind randomized con-trolled trial. Dig Liver Dis. 2010;42(12):871–6.
Tan X, Yowler CJ, Super DM, Fratianne RB. The efficacy of music therapy protocols for decreasing pain, anxiety, and mus-cle tension levels during burn dressing changes: a prospective randomized crossover trial. J Burn Care Res. 2010;31(4):590–7.
Pittman S, Kridli S. Music intervention and preoperative anxiety:an integrative review. Int Nurs Rev. 2011;58(2):163.
Buffum MD, Sasso C, Sands LP, Lanier E, Yellen M, Hayes A. Amusic intervention to reduce anxiety before vascular angiogra-phy procedures. J Vasc Nurs. 2006;24(3):68–73.
Acknowledgments
We express our most sincere gratitude to all the professionals who selflessly participated in this study. Thanks also to all the participating patients for their collaboration. We are grateful to Social Work Caja Cantabria for their funding support from the 16th edition of the Valdecilla National Nursing Research Award. We thank Diane Williams, PhD, from Edanz Group (http://www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
This project won the Valdecilla National Research Award, which financed part of its development. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
PP and CA designed the study. CF directed the study. MP, DP, CS, and MH collected the data and conducted the intervention under the supervision of PP. Finally, EB, CF, PP, and CA participated in the analysis of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the corresponding clinical research ethical committee of each center involved in the study [28] (University Hospital of Getafe, 06/26/2014; Puerta del Hierro-Majadahonda, 07/24/2014; Foundation Alcorcon, 11/03/2014; Fuenlabrada, 12/03/2014; Bellvitge, 09/10/2014; Salamanca, 07/18/2014; Navarra, 03/27/2015; Hospital Germans Trias i Pujol, 11/21/2014; and Cantabria 08/01/2014). All participants provided written informed consent after having been fully informed about the study aims.
Competing interests
The authors declare no conflict of interest. The authors have full control of all primary data, and we agree to allow the journal to review the data if requested.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Parás-Bravo, P., Alonso-Blanco, C., Paz-Zulueta, M. et al. Does Jacobson’s relaxation technique reduce consumption of psychotropic and analgesic drugs in cancer patients? A multicenter pre–post intervention study. BMC Complement Altern Med 18, 139 (2018). https://doi.org/10.1186/s12906-018-2200-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-018-2200-2