Abstract
Background
Leishmaniasis is an infectious disease caused by various species of the protozoan parasites of the Leishmania genus and transmitted by phlebotomine sandflies. The protozoa multiply in phagocytic cells, mainly macrophages, which play an important role defending the organism from pathogens. The most effective treatment for leishmaniasis is the chemotherapy and besides the high cost, these drugs are toxic and require a long period of treatment. Currently, some herbal products are considered an important alternative source of a new leishmanicidal agent, which includes the plant Physalis angulata, . We evaluated effects of an aqueous extract from roots of Physalis angulata (AEPa) on Leishmania proliferation, morphology and also determined whether physalins were present in the extract contributing to the knowledge of its pharmacological efficacy.
Methods
Morphological alterations were determined by light microscopy, transmission and scanning electron microscopy. Host cell viability was evaluated by MTT, and propidium iodide. AEPa were submitted in full HRESITOF analysis.
Results
AEPa promoted a dose-dependent reduction on promastigotes (IC50 = 39.5 μg/mL ± 5.1) and amastigotes (IC50 = 43.4 μg/mL ± 10.1) growth. This growth inhibition was associated with several morphological alterations observed in promastigote forms. No cytotoxic effect in mammalian cells was detected (IC50 > 4000 μg/mL). Furthemore, the presence of physalins A, B, D, E, F, G and H were described, for the first time, in the P. angulata root.
Conclusions
Results demonstrate that AEPa effectively promotes antileishmanial activity with several important morphological alterations and has no cytotoxic effects on host cells.
Similar content being viewed by others
Background
American tegumentar leishmaniasis (ATL) is a parasitic disease prevalent in many parts of the tropical and subtropical world and affects 12 million people in the entire world [1]. It is estimated that 2 million cases occur worldwide, including more than 22.000 cases in Brazil, with 32 % of them in the Amazon region [1, 2]. ATL is a disease with a wide spectrum of clinical variability that depends on both infecting species of Leishmania and the immune response of the host [3].
Chemotherapy is the only effective treatment for this disease. However, it is expensive and usually requires a long-term invasive and toxic intervention. During recent decades, studies have demonstrated that a number of plant-derived chemical compounds may act as new therapeutic tools against Leishmania [4–6]. One of these agents is Physalis angulata (Solanaceae), a plant distributed in tropical and subtropical regions of the world, including Amazon region that has been used traditionally as folk medicine [7, 8]. River people from the Amazonian usually employ the root from P. angulata for therapeutic interventions for malaria, asthma, hepatitis, dermatitis, rheumatism treatment and as anti-inflammatory agent [9–13]. The phytochemistry of P.angulata is known to contain glucocorticoids, flavonoids, withanolides and physalins [13]. Among the compounds thought to be responsible for the leishmanicidal effects of P. angulata are the physalins, which have been mostly isolated from the plant’s stems and leaves [14, 15]. In addition, antiprotozoal effect of physalins was also been reported against Plasmodium sp. [16] and Trypanosoma cruzi [17]. Nevertheless, to isolate enough physalins to observe the above-mentioned effects, researchers have used large quantities of P. angulata leaves and/or stems. As the purification process is time, effort, and resource consuming, the trend nowadays is to determine whether or not effective therapeutic results can be achieved from plant extracts, once extracts and/or infusions from P. angulata are most commonly used in popular medicine as a treatment for those infirmities [7, 8, 12, 13]. To date, no study has assessed whether extracts from P. angulata’s root affect Leishmania parasites, the main host cell (macrophage), or determined the presence of physalins in the root extract.
Therefore, based in effective action of P. angulata against Leishmania parasites, we reported here, for the first time, ultrastructural alterations in promastigote forms of Leishmania (Leishmania) amazonensis and host cell viability after exposure to aqueous root extract obtained from P. angulata. In addition, we also determined the presence of physalins in the root extract.
Methods
Plant materials
P. angulata of the family Solanaceae was collected in the Pará state, Brazil, and identified by Dr. Ricardo Secco (Department of Botany, Emilio Goeldi Museum) and a voucher specimen (no. 653) was deposited in the herbarium of the Emilio Goeldi Museum (Belém, Pará, Brazil). Extraction process were carried out according to the method described by Bastos et al. [11] and 1.0 mg/mL of aqueous extract from root of Physalis angulata (AEPa) was dissolved in Dulbecco’s Modified Eagle’s Medium (DMEM) or RPMI and used as the standard solution for assays.
Liquid chromatography/time-of-flight mass spectrometry analysis
High resolution mass spectral (HRESITOF) analysis was performed on a micrTOF II - ESI-TOF (Brucker Daltonics, Billerica, MA, USA). The capillary voltage was monitored at 4500 V (120 V output). A solution of NA-TFA (10 mg/mL) was used for Internal calibration (TOF). N2 was used at 200 °C; flow and pressure were set at 4 L/min nebulization and 0.4 bar. Liquid chromatography was performed with a Prominence liquid chromatography system model LC-20A from Shimadzu Technology (Kyoto, Japan), fitted with a diode array detector (DAD), SPDM-20A (Shimadzu, Kyoto, Japan) working in the range of 220–250 nm, a two pump LC-20 AD (Shimadzu, Kyoto, Japan), and a DGU-20A-5 degasser; a CBM-20A interface was used (Shimadzu, Kyoto, Japan). The analysis was performed at room temperature. The optimal chromatographic conditions consisted of an isocratic solvent system containing 25 % of acetronitrile in water, delivered to the C18 Phenomenex Onyx Monolithic 3 μm column (100 mm × 4.6 mm I.D.) at a flow rate of 0.3 mL/min. The eluent was monitored at a 225 nm detection wavelength.
Parasites
Leishmania (Leishmania) amazonensis (IFLA/67/BR/PH8) promastigotes were obtained from the Evandro Chagas Institute and cultured at 26 °C in NNN medium. Subsequently, promastigotes were cultured in RPMI medium supplemented with 10 % fetal bovine serum (FBS), 0.2 M glutamine, 0.125 M pyruvic acid and 5 mM penicillin/streptomycin.
Isolation of peritoneal murine macrophages
Females BALB/c mice (6 to 8 weeks old) were euthanized and resident macrophages were obtained by washing the peritoneal cavities with DMEM, pH 7.2. Then, peritoneal macrophages were allowed to adhere on round glass coverslips placed 24-well culture plate in a DMEM medium supplemented with 10 % FBS for 1 h at 37 °C in a humidified atmosphere containing 5 % CO2. After that, non-adherent cells were washed away with phosphate buffered saline (PBS), pH 7.2, and macrophages were incubated overnight in DMEM medium supplemented with 10 % FBS at 37 °C in a 5 % CO2 atmosphere. All experiments were performed at least three times with treated and untreated cells. The experiments were conducted in compliance with the Brazilian animal protection law (Lei Arouca number 11.794/08) of the National Council for the Control of Animal Experimentation (CONCEA, Brazil). The protocol was approved by the Committee on the Ethics of Animal Experiments of the Federal University of Pará (CEPAE/ICB/UFPA - grant number BIO086-12).
Antipromastigote assay
L. (L.) amazonensis promastigotes (106 parasites/mL) in the logarithmic growth phase were inoculated in a 24-well plate containing RPMI medium supplemented with 10 % FBS with different concentrations of AEPa, and incubated at 25 °C. Every 24 h, aliquots were harvested and promastigotes were counted in a Neubauer chamber. Cells were counted daily up to 96 h of treatment. The cultures were performed in triplicate. One known antileishmanial drug (Amphotericin B) at 0.1, 0.25, 0.5 and 1 μg/mL was included as a positive control. The inhibitory concentration (IC50) was determined using SigmaPlot (version 12).
Antiamastigote assay
Adhered macrophages were infected with L. (L.) amazonensis promastigotes (stationary growth phase) at a parasite/macrophage ratio of 10:1 and incubated for 3 h at 37 °C and 5 % CO2. After 1 h, free parasites were removed by washing with PBS. Cells were treated with 20, 50 and 100 μg/mL of AEPa, respectively, for 1 h daily and incubated for 3 days post infection, replacing the culture medium. Cells were then washed with PBS, fixed with Bouin’s fixative, stained with Giemsa and covered with Entellan® (Merck®). The number of parasites was determined by examining three coverslips for each treatment. At least 200 infected macrophages were counted and results were expressed as survival index when compared to controls. The survival index was obtained by multiplying the percentage of the infected macrophages by the mean number of amastigotes per infected macrophage and divided by the total number of macrophages. The percentage of inhibition was determined based in the survival index compared with control. The inhibitory concentration (IC50) was determined using SigmaPlot (version 12). One known antileishmanial drug Glucantime (50 μg/mL) was included as a positive control.
Morphological Analysis of AEPA-treated L. (L.) amazonensis promastigotes
Light microscopy (LM)
To evaluate the morphological changes induced by the AEPa in promastigote forms of L. (L.) amazonensis, the parasites were treated with 50 and 100 μg/mL of AEPa for 72 h. Parasite suspension aliquots were fixed with 4 % paraformaldehyde in 0.1 M PHEM buffer (5 mM magnesium chloride, 70 mM potassium chloride, 10 mM EGTA, 20 mM HEPES, 60 mM PIPES), pH 7.2, and stained with Panotic stain Kit (Laborclin). Cells were examined using an optical microscope Axioplan (Zeiss) and images were obtained using a digital camera model XC 30.
Transmission Electron Microscopy (TEM)
L. (L.) amazonensis promastigotes (106) in the logarithmic growth phase (4 days) were treated with 50 and 100 μg/mL AEPa for 3 days. The samples were processed for conventional TEM, as described by Guimarães et al. [18].
Scanning Electron Microscopy (SEM)
Control and treated promastigotes (50 and 100 μg/mL AEPa) were fixed with 4 % formaldehyde and 2.5 % glutaraldehyde in 0.1 M cacodylate buffer, pH 7.2, for 1 h. After fixation, the cells were placed on glass slides with 0.1 % poly-L-lysine. The cells were washed and post-fixed in 1 % osmium tetroxide, dehydrated in graded ethanol, critical point dried (CO2), coated with platinum and examined with a LEO 1450VP SEM.
Murine macrophage viability assays
MTT assay
The MTT assay is based on the mitochondrial-dependent reduction of MTT 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide] to formazan, and this assay was conducted following the procedure described by Rodrigues et al. [19]. Macrophages were treated with AEPa (10–400 μg/mL) for one hour and cultured at 37 °C, 5 % CO2 for 24 h. After treatment, cells were incubated with 0.5 mg/mL MTT for 3 h. Subsequently resulting solution was read in a microplate reader (BIO-RAD Model 450 Microplate Reader) and absorbance was recorded at 570 nm.
Propidium iodide dye exclusion test
Control and treated macrophages (50 and 100 μg/mL AEPa) were incubated for 30 min with 10 μg/mL of propidium iodide (PI). A total of 10.000 events were acquired for each sample in the region that corresponded to the parasites by flow cytometer BD FACSCantoII and analyzed with BD FACS Diva software. Cells labeled with the PI were considered dead.
Statistical analysis
The differences between mean values in the experimental groups were performed using ANOVA followed Tukey’s post test. All P-values < 0.05 were considered statistically significant. The means and SD of at least three experiments were determined.
Results
Identification of AEPa components by mass spectrometry analysis
To identify the possible active principle(s) responsible for the biological and morphological effects described above, we submitted AEPa to HRESITOF analysis. Several peaks were observed in the eluent from the liquid chromatography column. Among them, we identified the physalins A, B, D, E, F, G and H (Table 1).
Antileishmanial activity of AEPa
The effect of AEPa on L. (L.) amazonensis promastigotes was monitored for 4 days. Reductions of 100 % were observed in the number of viable parasites at 0.5 and 1 μg/mL Amphotericin B, respectively, after 96 h of incubation, representing an IC50 of 0.02 μg/mL ± 0.021 (Fig. 1a). In contrast, the AEPa induced dose-dependent reductions in parasite proliferation of 74.1 % and 99.8 % after 96 h of treatment with 50 μg/mL and 100 μg/mL AEPa, respectively, representing an IC50 of 39.5 μg/mL ± 5.1 μg/mL (Fig. 1b).
AEPa action against L. (L.) amazonenis in vitro. Growth curve of L. (L.) amazonensis promastigotes treated with different concentrations of Amphotericin B (AMPB) (a) and AEPa. b Growth was followed up to 96 h. c Effect of AEPa on intracellular amastigote survival of L. (L.) amazonensis. Infected mouse peritoneal macrophages were treated with different concentrations of the extract, for1h/day during 3 days and with glucantime ® (GLU). Results are from experiments performed in triplicate. *p < 0.001, *p < 0.05, ***p < 0.001 compared with control (untreated). CTL: control
Effect of AEPa on L. (L.) amazonensis intracellular amastigotes
The leishmanicidal activity of AEPa was also evaluated in L. (L.) amazonensis-infected macrophage cultures. A reduction in parasite survival was observed for all AEPa concentrations tested. However, more significant results were found at 50 μg/mL and 100 μg/mL of AEPa, achieving reductions of 70.6 % and 70.9 %, respectively (IC50 43.3 μg/mL ± 10.1; Fig. 1c). Glucantime (GLU - Figure 1c) and amphotericin B (AMPB - Additional file 1) were added as reference drugs.
LM analysis of AEPa-treated L. (L.) amazonensis promastigotes
L. (L.) amazonensis promastigotes were analyzed by LM to detect morphological alterations. Untreated parasites showed a typical morphology with an elongated body and a single flagellum (Fig. 2a). After 72 h of treatment with 50 μg/mL and 100 μg/mL of AEPa, promastigotes presented a rounded shape, two flagella and a reduction in cell body (Fig. 2b and c). In addition, treated cultures presented debris suggestive of cellular fragments.
Light microscopy of promastigote forms of L. amazonensis treated with AEPa for 3 days. a Control parasite; b Promastigotes treated with 50 μg/mL of AEPa. Arrow indicates parasites with two flagella. c Promastigotes treated with 100 μg/mL AEPa. Note reduction in the cell size and rounded cell body (arrow). Bars: 20 μm
SEM analysis of AEPa-treated L. (L.) amazonensis promastigotes
SEM was used to further investigate the morphological alterations observed by light microscopy. Promastigotes treated with 50 μg/mL AEPa presented flagellum duplication and atypical cell division (Fig. 3b). When promastigotes were treated with 100 μg/mL AEPa, their rounded appearance became more evident, the body was frequently multi-septated, and the flagellum shortened (Fig. 3c and c). Moreover, SEM analysis suggest that the debris observed by LM is likely to be cellular fragments around the parasites (Fig. 3d).
Scanning electron microscopy of promastigotes of L. amazonensis treated with AEPa from Physalis angulata after incubation for 3 days. a Control. b Parasites after treatment with 50 μg/mL AEPa. Observe the flagellum and cell doubling in apparent atypical cell division, and multi-septation of the cell body (arrows). c and d Parasites after treatment with 100 μg/mL AEPa. Observe reduction in the parasite body, multi-septation of the cell body (white arrows) and of the flagellum. Note the presence of cellular debris around parasite (arrows). Bars: (a) 3 μm (b-d) 1.5 μm
TEM analysis of AEPa-treated L. (L.) amazonensis promastigotes
TEM was used to analyze alterations in the parasite organelles. Promastigotes treated with 50 μg/mL AEPa showed changes in the flagellar membrane that presents some vacuoles near the flagellar pocket membrane (Fig. 4b). When 100 μg/mL AEPa was used, we observed alterations in the kinetoplast’s shape with swelling and duplication of its DNA. Alterations were also observed in the flagellar pocket, where myelin-like structures and the presence of vesicles were seen (Fig. 4c and d). Furthermore, atypical cell division was observed (Fig. 4b), as shown by SEM.
Ultrastructural effects of AEPa on promastigotes of Leishmania (L.) amazonensis. a General view of untreated parasite showing the characteristic structure of kinetoplastids. b Promastigotes treated with 50 μg/mL AEPa for 3 days. Note some vacuoles in the membrane of flagellar pocket (*) and alterations in flagellar membrane (arrow). c and d General view of promastigotes treated with 100 μg/ml AEPa for 3 days. c Observe the presence of myelin-like structures in the flagellar pocket (arrows) and duplication of kinetoplast DNA (arrowhead). (d) Note the presence of a large number of vesicles inside the flagellar pocket (*) and alterations in shape and swelling of kinetoplast (arrowheads). N, nucleus; FP, flagellar pocket; K, kinetoplast; F, flagellum; M, mitochondria. Bars represent A 5 μm; B 2 μm; C 5 μm; C inset 2 μm; D 2 μm
Effects of AEPa on macrophage viability
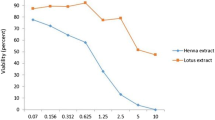
To test the selectivity of AEPa for the L. (L.) amazonensis parasite, murine macrophages were treated with the extract and the viability of these cells was assessed by the MTT reduction and PI. No cytotoxic effect of 10–400 μg/mL of AEPa treatment on macrophages was observed with the MTT assay (Fig. 5a). No differences were detected in the intensity of the red fluorescence in macrophages stained with PI dye (Fig. 5b) when compared treated and untreated macrophages.
Host cell viability assays. a MTT assay. The viability of the untreated control was taken as 100 %. The viability percentage was calculated for different concentrations of AEPa. No significant differences were found at 10–400 μg/ml of AEPa when compared with the control. b Propidium iodide (PI) exclusion test at 50 and 100 ug/mL in comparison to the control (CTL). No significant differences were observed in macrophages stained with PI dye
Discussion and conclusions
Bioproducts obtained from plants offer perspectives for the discovery of new active and promising compounds with antileishmanial activity. Extracts and physalins obtained from P. angulata have shown a vast range of biological properties [10, 11, 14–16, 20, 21]. However, to date, no reports have described the morphological alterations in parasites of Leishmania genus in response to AEPa treatment.
Results showed that 100 μg/mL AEPa induce 99.8 % antileishmanial activity against L. amazonensis promastigotes (IC50 of 39.5 μg/mL ± 5.1). A similar concentration of flower and leaf extracts from Cymbopogon citratus, Matricaria chamomilla and Piper regnellii Miq. [5] achieved around 98 % antileishmanial activity against L. amazonensis promastigotes. As such, AEPa seems to have a comparable growth inhibitory effect on promastigotes to these other plant extracts. However, they are clearly more potent than some plant extracts that have reported a maximum of 90–96 % of antileishmanial activity against L. amazonensis promastigotes [5, 22].
One of the novel findings of the present study is the description of morphological alterations caused in promastigotes forms following incubation with AEPa. Electron microscopy techniques can be a useful tool in drug studies for the identification of cell surfaces and ultrastructural alterations, as well as specific organelle targets in the parasites. Indeed, identification of morphological changes can help elucidate the mechanisms of drug action [23, 24]. Treatment of promastigotes with 50 or 100 μg/mL AEPa caused a reduction and rounding of the body cellular volume, as well as flagellum duplication, as shown by LM and SEM. Duran et al. [25] observed similar changes in the body shape and flagellum of promastigotes treated with an ethanolic extract of Adana propolis. However, these authors used concentrations of 250 and 500 μg/mL against L. tropica. Santin et al. [26] showed atypical flagella duplication in L. amazonensis promastigotes treated with oil from Cymbopogon citratus. In a review published by Adade and Souto-Padrón. [24], the authors suggested that these alterations may be caused by the interference of drugs and plant extracts in the process of cell division. Since the division process of L. amazonensis promastigotes treated with AEPa initiated at the posterior instead of the normal anterior position [27, 28], it is possible that the extract interfered with the division process of these cells.
SEM analysis revealed cellular debris and body multi-septation in promastigotes treated with AEPa. Studies with Cymbopogon citratus oil against promastigotes of L. chagasi showed multi-septation, and shortening of the cell body and flagellum [29]. This alteration could be caused by cytoskeleton disassembly [24]. In addition, TEM analysis showed the presence of multiple vesicles within the flagellar pocket of AEPa treated-promastigotes. The uptake of macromolecules by promastigotes occurs through the flagellar pocket, which is an invagination of the plasma membrane, devoid of microtubules. This region is the only place where exocytic and endocytic activity occurs [30]. In promastigotes submitted to drug and/or plant extracts treatments, this increased exocytic activity probably occurs to expel the toxic compound [18, 31]. It is likely that the multiple vesicles observed may be employed by L. amazonensis promastigotes for the removal of the toxic compounds present in the AEPa.
Myelin-like figures were also observed in the promastigotes treated with AEPa. These structures are a result of the merging of internal membranes to form concentric structures, which may be indicative of an autophagic process [18, 32, 33] as observed by Meira et al. [17] in Trypanosoma cruzi. Another characteristic feature seen in AEPa-treated promastigotes was the structural modifications of the kinetoplast, such as duplication, and shape and size alterations. Several authors, using plant products, demonstrated similar kinetoplast alterations [18, 34]. The kinetoplast is a unique organelle present only in trypanosomatid protozoa and is, thus, a potential drug target due to its unique structure and function, which is matched in its mammalian host [24, 30, 35].
Additionally, treatment of intracellular amastigotes of Leishmania (L.) amazonensis with 100 μg/mL AEPa led to a growth inhibitory effect of 70.9 % (IC50 43.3 μg/mL ± 10.1). Luize et al. [5] also showed an inhibitory effect of 92–96 % with Cymbopogon citratus, Matricaria chamomilla and Piper regnellii Miq. extracts when tested against amastigotes. However, it is not possible to directly compare the inhibitory effects of this study with our results, since authors used axenic amastigote cultures instead of amastigotes inside host cells. In previous reports, Guimarães et al. [14, 15] showed that physalins B, F and G, purified from stems of P. angulata, were able to reduce promastigote (IC50 = 6.8, 1.4, and 9.2 μM, respectively) and axenic amastigotes number (IC50 = 0.21 and 0.18 μM for Physalin B and F, respectively) and percentage of Leishmania-infected macrophages at concentrations non-cytotoxic to macrophages. However, no reports have described morphological alterations in parasites. Our study evaluated the antileishmanial effect of AEPa and also morphological alterations indicative of abnormalities in the cell division process. We detected, for the first time, the presence of physalins A, B, D, E, F, G and H in the AEPa, isolated from roots, and believes that these morphological and physiological changes could be related to the presence of these physalins in the AEPa. Furthermore, cytotoxicity tests were employed to verify whether AEPa was selectively toxic against the parasite, therefore sparing the host cell. The assays used did not detect significant changes in host cell viability, suggesting AEPa was specific for the protozoa.
Taken together, our results indicate that the AEPa promotes morphological alteration in promastigotes, a dose-dependent reduction of promastigotes and amastigotes of Leishmania, and have no cytotoxic effects on the host cell. To our knowledge this report is the first ultrastructural analysis of the actions of the aqueous extract from P. angulata on Leishmania and could be helpful for understanding possible mechanisms of action of this agent on parasites and host cells. Therefore, this study is part of a continual search for new drugs, obtained from medicinal plants widely used in Amazon region that can act effectively against neglected diseases such as leishmaniasis.
Abbreviations
- ATL:
-
American tegumentar leishmaniasis
- DMEM:
-
Dulbecco’s modified eagle’s medium
- HRESITOF:
-
High resolution mass spectral
- DAD:
-
Diode array detector
- FBS:
-
Fetal bovine serum
- AEPa:
-
Aqueous extract from root of Physalis angulata
- LM:
-
Light microscopy
- TEM:
-
Transmission electron microscopy
- SEM:
-
Scanning electron microscopy
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide
- PI:
-
Propidium iodide
References
WHO, 2012. [http://www.who.int/leishmaniasis/en/].
Ministério da Saúde. Secretária de Vigilância em Saúde. Leishmaniose tegumentar americana. [http://portalsaude.saude.gov.br/images/pdf/2014/setembro/09/LT-Casos.pdf]
Silveira FT, Lainson R, Corbett CEP. Clinical and Immunopathological Spectrum of American Cutaneous Leishmaniasis with special reference to the disease in Amazonian Brazil - A Review. Mem Inst Oswaldo Cruz. 2010;99:239–51.
Rosa MSS, Mendonça-Filho RR, Bizzo HR, Rodrigues IA, Soares RMA, Padrón TS, et al. Antileishmanial activity of a Linalool-Rich essential oil from Croton cajucara. Antimicrob Agents Chemother. 2003;47:1895–901.
Luize PS, Tiuman TS, Morello LG, Maza PK, Ueda-Nakamura T, Filho BPD, et al. Effects of medicinal plant extracts on growth of Leishmania (L.) amazonensis and Trypanosoma cruzi. Braz J Pharm Sci. 2005;41:85–94.
Laurella LC, Frank FM, Sarquiz A, Alonso MR, Giberti G, Cavallaro L, Catalán CA, Cazorla SI, Malchiodi E, Martino VS, Sülsem VP. In vitro evaluation of antiprotozoal and antiviral activities of extracts from Argentinean Mikania species. Sci W J. 2012;121253.
Lusakibanza M, Mesia G, Tona G, Karemere S, Lukuka A, Tits M, Angenot L, Frédérich M. In vitro and in vivo antimalarial and cytotoxic activity of five plants used in congolese traditional medicine. J Ethnopharmacol. 2010;129: 398–402.
Ruiz L, Ruiz L, Maco M, Cobos M, Gutierrez-Choquevilca AL, Roumy V. Plants used by native Amazonian groups from the Nanay River (Peru) for the treatment of malaria. J Ethnopharmacol. 2011;133:917–21.
Lin YS, Chiang HC, Kan WS, Hone E, Shih SJ, Won MH. Immunomodulatory activity of various fractions derived from Physalis angulata L. extract. Am J Chin Med. 1992;20:233–43.
Bastos GN, Santos AR, Ferreira VM, Costa AM, Bispo CI, Silveira AJ, et al. Antinociceptive effect of the aqueous extract obtained from roots of Physalis angulata L. on mice. J Ethnopharmacol. 2006;103:241–5.
Bastos GN, Silveira AJ, Salgado CG, Picanço-Diniz DL, Nascimento JL. Physalis angulata extract exerts anti-inflammatory effects in rats by inhibiting different pathways. J Ethnopharmacol. 2008;118:246–51.
Coelho-Ferreira M. Medicinal knowledge and plant utilization in an Amazonian coastal community of Marudá, Pará State (Brazil). J Ethnopharmacol. 2009;126:159–75.
Renjifo-Salgado E, Vargas-Arana G. Physalis angulata. L (Bolsa Mullaca): A review of its traditional uses, chemistry and pharmacology. Boletin Latino Americano Caribe Plant Med Aromat. 2013;12:431–45.
Guimarães ET, Lima MS, Santos LA, Ribeiro IM, Tomassini TB, Dos Santos RR, et al. Activity of physalins purified from Physalis angulata in vitro and in vivo models of cutaneous leishmaniasis. J Antimicrob Chemother. 2009;64:84–7.
Guimarães ET, Lima MS, Santos LA, Ribeiro IM, Tomassini TB, Dos Santos RR, et al. Effects of seco-steroids purified from Physalis angulata L., Solanaceae, on the viability of Leishmania sp. Braz J Pharm. 2010;20:945–9.
Sá MS, De Menezes MN, Krettli AU, Ribeiro IM, Tomassini TC, Ribeiro dos Santos R, et al. Antimalarial activity of physalins B, D, F, and G. J Nat Prod. 2011;74:2269–72.
Meira CS, Guimaraes ET, Bastos TB, Moreira DRM, Tomassini TCB, Ribeiro IM, et al. Physalins B and F, seco-steroids isolated from Physalis angulata L., strongly inhibit proliferation, ultrastructure and infectivity of Trypanosoma cruzi. Parasitol. 2013;140:1811–21.
Guimarães LR, Rodrigues AP, Marinho PS, Muller AH, Guilhon GM, Santos LS, et al. Activity of the julocrotine, a glutarimide alkaloid from Croton pullei var. glabrior, on Leishmania (L.) amazonensis. Parasitol Res. 2010;107:1075–81.
Rodrigues AP, Carvalho AS, Santos AS, Alves CN, Do Nascimento JL, Silva EO. Kojic acid, a secondary metabolite from Aspergillus sp. acts as an inducer of macrophage activation. Cell Biol Int. 2011;35:335–43.
Garcia ES, Castro DP, Ribeiro IM, Tomassini TC, Azambuja P. Trypanosoma rangeli: effects of physalin B on the immune reactions of the infected larvae of Rhodnius prolixus. Exp Parasitol. 2006;112:37–43.
Silva BJM, Rodrigues APD, Farias LHS, Hage AAP, Nascimento JLM, Silva EO. Physalis angulata induces in vitro differentiation of murine bone marrow cells into macrophages. BMC Cell Biol. 2014;15:37.
Delorenzi JC, Attias M, Gattass C, Andrade M, Rezende C, Pinto AC, et al. Antileishmanial activity of an indole alkaloid from Peschiera australis. Antimicrob Agents Chemother. 2001;45:1349–54.
Vannier-Santos MA, De Castro SL. Electron microscopy in antiparasitic chemotherapy: a (close) view to a kill. Curr Drug Targets. 2009;10:246–60.
Adade CM, Souto-Padrón T. Contributions of ultrastructural studies to the cell biology of trypanosomatids: targets for anti-parasitic drugs. Open Parasitol J. 2010;4:178–87.
Duran G, Duran N, Culha G, Ozcan B, Oztas H, Ozer B. In vitro antileishmanial activity of Adana propolis samples on Leishmania tropica: a preliminary study. Parasitol Res. 2008;102:1217–25.
Santin MR, Dos Santos AO, Nakamura CV, Dias Filho BP, Ferreira IC, Ueda-Nakamura T. In vitro activity of the essential oil of Cymbopogon citratus and its major component (citral) on Leishmania amazonensis. Parasitol Res. 2009;105:1489–96.
Ambit A, Woods KL, Cull B, Coombs GH, Mottram JC. Morphological events during the cell cycle of Leishmania major. Eukaryot Cell. 2011;10:1429–38.
Wheeler RJ, Gluenz E, Gull K. The cell cycle of Leishmania: morphogenetic events and their implications for parasite biology. Mol Microbiol. 2011;79:647–62.
Oliveira VC, Moura DM, Lopes JA, De Andrade PP, Da Silva NH, Figueiredo RC. Effects of essential oils from Cymbopogon citratus (DC) Stapf., Lippia sidoides Cham., and Ocimum gratissimum L. on growth and ultrastructure of Leishmania chagasi promastigotes. Parasitol Res. 2009;104:1053–9.
De Souza W. An introduction to the structural organization of parasitic protozoa. Curr Pharm Des. 2008;14:822–38.
Vendrametto MC, Santos AO, Nakamura CV, Filho BPD, Cortez DAG, Ueda-Nakamura T. Evaluation of antileishmanial activity of eupomatenoid-5, a 19 compound isolated from leaves of Piper regnellii var. pallescens. Parasitol Int. 2010;59:154–8.
Rodrigues JCF, Attias M, Rodriguez C, Urbina JA, Souza W. Ultrastructural and biochemical alterations induced by 22, 26-azasterol, a Δ24(25)-sterol methyltransferase inhibitor, on promastigote and amastigote forms of Leishmania amazonensis. Antimicrob Agents Chemother. 2002;46:487–99.
Santa-Rita RM, Henriques-Pons A, Barbosa HS, Castro SL. Effect of the lysophospholipid analogues edelfosine, ilmofosine and miltefosine against Leishmania amazonensis. J Antimicrob Chemother. 2004;54:704–10.
Ueda-Nakamura T, Mendonça-Filho RR, Morgado-Díaz JA, Maza PK, Dias Filho BP, Cortez AGD, et al. Antileishmanial activity of Eugenol-rich essential oil from Ocimum gratissimum. Parasitol Int. 2006;55:99–105.
Sen R, Chatterjee M. Plant derived therapeutics for the treatment of Leishmaniasis. Phytomed. 2011;18:1056–69.
Acknowledgments
This work was supported by the Conselho Nacional de Desenvolvimento Cientifico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), FAPESPA and Instituto Nacional de Biologia Estrutural e Bioimagem-INBEB (CNPq - Grant number 573767/2008-4). The experiments performed in this study were conducted in compliance with current Brazilian animal protection laws.
The authors are grateful to Dr. Noberto Peporine Lopes for help with the mass spectrometry analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RRPS performed experiments. APDR, LHSF and EOS performed the LM, SEM and TEM analyzes. MNS, DTVA and GNTB Contributed with reagents/materials/analysis tools. BJMS, APDR, RRPS, EOS and JLMN were involved in the discussion of results, writing and manuscript editing. All authors read and approved the final manuscript.
Additional file
Additional file 1
Effect of AMPB on L. (L.) amazonensisintracellular amastigotes. Infected mouse peritoneal macrophages were treated with different concentrations AMPB for 24h. ***p < 0.001 compared with control (CTL).
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
da Silva, R.R.P., da Silva, B.J.M., Rodrigues, A.P.D. et al. In vitro biological action of aqueous extract from roots of Physalis angulata against Leishmania (Leishmania) amazonensis. BMC Complement Altern Med 15, 249 (2015). https://doi.org/10.1186/s12906-015-0717-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-015-0717-1