Abstract
Background
Metabolic syndrome (MetS) is a group of diseases characterized by insulin resistance. MetS has high prevalence among women, which is impacted by food intake. MetS is related to high level of inflammation; however, the impacts of whole diets on biochemical and anthropometrical markers and the effects on MetS need to be further elucidated. In this case, the objective of this study was to assess the relationship between food intake, biochemical and anthropometrical markers in women with MetS.
Methods
This is a cross-sectional study, in which 1 hundred and 22 women participated in the assessment of biochemical (glycated hemoglobin, glycaemia, insulin, uric acid, total cholesterol, HDL-c, LDL-c, triglycerides, C-reactive protein) and anthropometrical (body mass, height, waist circumference - WC) variables. Participants also performed blood pressure and 24-hour dietary recall assessments. Out of the 122 participants, 44 (36%, age: 59 ± 11 years) had MetS and were included in the analysis.
Results
The consumption of monounsaturated fats had direct relationship with glycaemia (b = 7.48), whereas the consumption of fibers had inverse relationship with body mass (b = − 0.71) and WC (b = − 0.56).
Conclusion
The intake of monounsaturated fats and fiber was related to higher blood sugar levels and lower body mass and WC, respectively. These relationships elucidate and highlight the significance and importance of adequate diet in women with MetS.
Similar content being viewed by others
Introduction
There is a relationship between visceral adiposity and diabetes mellitus, and both are related to atherosclerosis [1, 2]. In 1977, the combination of obesity, diabetes mellitus, and other clinical conditions was named metabolic syndrome (MetS) [3, 4]. Many definitions have been proposed, highlighting visceral adiposity and insulin resistance causing metabolic abnormalities [5]. Different criteria have been used to classify MetS [6,7,8,9]. In 2009, to facilitate the comparison between studies, a group of researchers proposed a common definition considering changes in fast glycaemia, hypertension, hypertriglyceridemia, low high-density lipoprotein, or the use of drugs to control any of these factors, and the presence of visceral obesity [10].
There are different interventions to reduce the risk of MetS [9]. Changes in lifestyle and eating habits are important, including controlling caloric intake and the intake of saturated fat, cholesterol, salt, and sugar. Increased consumption of fruits, vegetables, and whole grains are also recommended [11]. The risk of developing MetS is significantly affected by inadequate food consumption. In addition to food choices, food consumption patterns are also important. Identifying a diet in which individuals with MetS are able to adhere to, with moderate consumption of macronutrients, is critical [11, 12]. Carbohydrate consumption influences glycaemia, lipidic profile, inflammatory markers, and insulin resistance [13, 14]. Metabolic markers are used for clinical decisions asthey provide essential information for preventing, diagnosing and treating these diseases [15, 16]. To prescribe or guide an individualized diet, it is necessary to consider the metabolic markers for better prescription. Anthropometric measurements and food consumption patterns are also important to manage health, eating, and nutritional conditions [17].
MetS increases systemic inflammation, which differs from others inflammation processes because it involves the immunological system and impacts metabolic homeostasis. These impacts increase inflammatory markers, reduce daily energetic expenditure, promote disfunction in β cells from the pancreas, and increase hepatic and cardiovascular diseases [18, 19].
The influence of dietary habits on the control or prevention of many diseases is well known. However, more information is needed to elucidate the role of nutritional habits on inflammatory markers in people with MetS [9, 11]. Moreover, there is a gap in literature related to the impact of dietary components on different biochemical markers in individuals with MetS [20]. Furthermore, there is still a need for information regarding the impact of diets on MetS components [21]. Considering the scarcity of studies in this area, this study will provide knowledge regarding the potential effects of dietary habits on MetS and promote evidence-based practice. Therefore, this study aimed to assess the relationship between dietary components, biochemical markers, and anthropometric variables in women with MetS. The hypothesis was that adequate dietary intake would be associated with better biochemical profile and anthropometric markers.
Methods
Participants
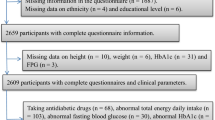
This is a cross-sectional study of women attending the Multi-professional Outpatient Women’s Health Clinic at the University Hospital. One hundred and twenty-two patients were invited to participate during the years of 2018 and 2019. Patients received information about the study objectives and procedures and signed the informed consent form. The research was approved by the local ethics committee (protocol No. 2.837.313). This manuscript follows the EQUATOR network guidelines.
Participants filled a questionnaire (personal and clinical information) (Supplementary file 1) and anthropometric measurements, reported their 24-h dietary intake, and provided blood samples for biochemical analyses. The inclusion criterion was having metabolic syndrome (MetS) based on assessments, and the exclusion criteria were having other acute or chronic diseases, renal impairment, neurological diseases or cancer, pregnancy or lactation. Women with uncommon dietary patterns before 24 h of data collection were also excluded from the research.
The diagnosis of MetS was based on three or more of the following characteristics: i) waist circumference (WC) ≥ 88 cm; ii) HDL < 50 mg / dL or using antilipemic; iii) TG ≥ 150 mg/dl or using medication for dyslipidemia; iv) systolic blood pressure (BP) ≥ 130 and diastolic ≥85 mm / Hg or using antihypertensive drugs; v) Fasting venous glycaemia (FVG) ≥ 100 mg/dl or using hypoglycemic medication [10]. Of the 122 women evaluated, 44 (36%) had MetS and were included in the analyses. The high prevalence of MetS may be explained by the fact that participants were recruited from a clinical setting where they were receiving care for different health conditions, including MetS and its complications.
Anthropometry
Body mass was measured with the subject standing barefoot and wearing light clothes using calibrated scale with 0.1 kg precision. Height was measured using stadiometer with 0.1 cm accuracy. Participants stood barefoot, with feet together, eyes gazing at the horizon without tilting or extending the head. BMI was calculated and was adopted the classification of the WHO reference standard [BMI: (weight/height2)] [22] for adult women and Lipschitz [23] for women aged 60 years or over. WC was measured at the midpoint between the costal arch and the iliac crest using inextensible measuring tape [22].
Biochemical analysis
Blood samples were collected after a 12-hour fasting period in tubes without anticoagulant (to obtain serum) with separating gel; one tube containing sodium fluoride for blood glucose determination, and two tubes containing EDTA as anticoagulant and preservative. Plasma and serum were aliquoted and stored in freezer at − 80 °C (Indrel®) until tests were carried out.
Serum C-reactive protein (CRP) levels were determined by nephelometry (Dade-Behring), ELISA methodology using commercial kits with up to 5.00 mg / L of a reference value. Analyses of total cholesterol (CT), HDL cholesterol, Triglycerides (TG), uric acid, glucose, and glycated hemoglobin (HbA1c) were performed in biochemical autoanalyzer (Dimension-Siemens®), using Siemens kits. LDL-c was calculated using the following formula [24]:
Fasting insulin levels were determined by microparticle immunoassay enzyme on the AXSYN equipment (ABBOTT).
Insulin resistance and beta-cell function were estimated from calculations of the HOMA-IR index [25].
The cutoff points for laboratory tests were in accordance with those already established, with the respective values for each test being considered acceptable. CRP (≤5 mg/dL), CT (< 200 mg/dL), HDL (> 50 mg/dL), LDL (< 130 mg/dL), TG (< 150 mg/dL), urid acid (≥2,6 - ≤ 6 mg/dL), glucose (≤ 70 - < 100 mg/dL), HbA1c (≤4,8 - ≤6%), insulin (≤2,7 - ≤10,4 μU/mL) and HOMA-IR (< 2,5%).
Dietary intake assessment
Dietary intake was determined using a 24-h recall [26] with the aid of the Dietbox® software to define and quantify all the food and beverages consumed in the 24-hour period before the interview [27]. The 24-hour recall has good reproducibility with correlation coefficients between 0.36 to 0.69 and weighted Kappa over 0.4. The validity has correlation coefficients between 0.21 and 0.74 [28].
Information on dietary intake was obtained regarding the consumption of proteins, carbohydrates, sugars, fibers, total fats, polyunsaturated fats, monounsaturated, saturated, trans, cholesterol, fibers, and micronutrients. The researcher encouraged participants to remember the food intake with detailed description of foods and amounts during the interview. The researcher also revised the information at the end of the interview.
To characterize food intake as adequate or not, the total intake of macronutrients follows recommendations of the Updated Brazilian Guideline on Dyslipidemia and Atherosclerosis Prevention of the Brazilian Society of Cardiology [29].
Statistical analysis
Sample characteristics were presented as means and standard deviations (SD). The Shapiro-Wilk test was used to verify data normality. Food consumption was presented by total amounts or daily percentages. The relationship between food consumption, anthropometrical and biochemical variables was assessed using multiple linear regression controlled by medications (hypoglycemic, hypolipemic, and insulin or similar), age and other independent variables. Regressions were expressed as regression coefficients (β) and standard errors (SE); and for variables that presented significance, confidence intervals (CI) were also presented. Residual analyses were performed to verify regression adequacy and the variance inflation factor was also verified (VIF < 2.0). Significance of 5% was adopted, and data were analyzed using the SPSS software version 25.0.”
Results
Medications were used by 98% of participants (n = 43) to manage MetS. A total of 61% (n = 27) used oral hypoglycemic drugs, and 32% (n = 14) used insulins and analogues. Age and anthropometrical, biochemical, and nutritional markers are shown in Table 1. Blood pressure was within normal levels for MetS patients. As for body composition, 43% (n = 19) were overweight and 53% (n = 23) were obese.
Regarding food consumption, 82% (n = 36), 52% (n = 23) and 59% (n = 26) presented high/inadequate consumption of saturated, polyunsaturated, and monounsaturated fats, respectively (Table 1); 66% (n = 29) of women did not consume adequate levels of proteins. The consumption of carbohydrates was adequate for only 34% (n = 29) of participants, and only 7% (n = 3) consumed adequate levels of fibers.
The prevalence (%) of disorders related to MetS among participants is shown in Fig. 1. WC was high (> 88 cm) in 98% (n = 43), 91% (n = 40) had low HDL-C or used drug treatment to reduce HDL-c, 84% (n = 37) had hypertension or used antihypertensives, and 86% (n = 39) had high TG concentration or used medication for dyslipidemia.
Prevalence of metabolic syndrome components of in women. Values were expressed as percentage; WC: Waist Circumference ≥ 88 cm; TG: Triglycerides ≥150 mg/dl or using medication for dyslipidemia; HDL-c: High Density Lipoproteins < 50 mg/dL or using antilipemic drugs; Glycaemia: Fasting venous glycaemia (FVG) ≥ 100 mg/dl or when using hypoglycemic drugs; Blood Pressure: systolic blood pressure (BP) ≥ 130 and diastolic ≥85 mm / Hg or when using antihypertensive drugs
Table 2 shows the relationship between food consumption and biochemical variables. The relationship between consumption of monounsaturated fats and glycemic values was significant (β: 7.48; CI:1.24–13.72; P < 0.05). The consumption of other macronutrients, on the other hand, did not show significant relationship with biochemical variables.
Table 3 shows the relationship between food consumption and anthropometric variables. Inverse relationship was observed between fiber consumption and body mass (β: -0.71; CI: − 1.34 - -0.07; P < 0.05) and waist circumference (β: -0.56; CI: − 1.21 – -0.01; P < 0.05).
Discussion
This research aimed to assess the relationship between food consumption, biochemical markers, and anthropometric values in women with MetS. Significant relationship was observed between consumption of monounsaturated fat and fast glycaemia, and inverse relationship between fiber consumption, body mass and waist circumference.
Recent studies have emphasized the impact of macronutrient intake on the energetic biomarkers related to metabolic health; genetic effects are more powerful when healthy diets are consumed [31]. Gene/macronutrient interactions modulate the risk of obesity and metabolic diseases [32]. In the present study, high ingestion of fats and low ingesting of fibers was observed. Direct relationship between monounsaturated fat intake and high fast glycaemia was also observed. The consumption of monounsaturated fats can be related to the high consumption of red meat and dairy products; and distinct cardiometabolic effects are related to the consumption of mono and polyunsaturated fats [33]. Jiao et al. [34] found positive association between monounsaturated fat and mortality.
Consumption of red meat, especially processed meat, was related to increase in diabetes. In contrast, the intake of milk, cheese, and yogurt showed neutrality over cardiometabolic effects. Vegetables that provide monounsaturated fat had positive cardiometabolic effects [33, 35, 36]. The 24-h dietary recall confirmed the choice of unhealthy sources of monounsaturated fat such as processed meats and cheese, which have high amounts of saturated fat with postprandial effects, promote the store of fat (lipogenesis), increase inflammatory processes and glycaemia [37, 38].
Another important factor for metabolic homeostasis is the intestinal microbiota, which is dependent on alimentary residues such as fiber, for its surveillance and metabolism [39]. Moreover, the intestinal microbiota provides high butryogenesis rates, with epigenetic and immunomodulatory effects on other organs of the body [40]. This information could help understanding the relationship between high fiber intake and reduction in many pathologies, including metabolic diseases [41,42,43,44,45]. It is important to highlight the low fiber intake found in the present study (13 g/day), which was 50% less than the recommended values of 26 g/day [29].
The analysis of dietary intake and anthropometrics measurements revealed inverse relationship between fiber intake and waist circumference. This result corroborates other studies. Liu et al. [46] evaluated 74.091 nurses over 12 years and observed that those with high fiber intake gain less weight than their peers. Furthermore, overweight and obese women have lower intake of fruits and vegetables [47]. Dietary fiber intake is inversely related to body mass, BMI and WC [48,49,50]. Fiber consumption is critical to promote weight loss in obese or overweight subjects [49, 50]. The most prevalent MetS factor in the present study was high WC (98% > 88 cm). Fibers prevent obesity by supporting the intestinal microbiota, decreasing the absorption of nutrients [51], inhibiting appetite [52, 53], and regulating homeostasis [54, 55].
This study demonstrates that small changes in eating habits, as decrease in monounsaturated fat intake and increase in fiber intake, could reduce the risk factors for women with MetS. While monounsaturated fats have relationship with glycaemia, fibers have inverse relationship with body mass and WC. The data found in this study enhance the importance of dietary fiber intake since it could promote beneficial effects on the anthropometric profile.
The present study has some limitations such as the small sample size, only one dietary intake assessment, and lack of data on physical activity levels. The 24-h dietary recall is subject to errors in the representation of the actual dietary intake. However, there is no gold standard method available for researchers to evaluate dietary intake [56, 57]. Even applied only once, this recall search estimates the absolute intake instead of relative intake through its open structure [58].
Conclusion
The intake of monounsaturated fats and fiber were associated to higher blood sugar levels and low body mass and waist circumference, respectively. These relationships highlight the importance of dietary intake in MetS management.
The present study increases the understanding of the relationship between dietary habits, biochemical and anthropometric markers in women with MetS. The findings indicate that the consumption of fibers is important to the control of visceral obesity in women with MetS. Further longitudinal studies are necessary to evaluate the cause-effect relationship between dietary intake and its effects on physiological and anthropometrical markers in people with MetS.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body Mass index
- BP:
-
systolic blood pressure
- CRP:
-
C-reactive protein
- CT:
-
Total cholesterol
- CI:
-
95% confidence interval
- FVG:
-
Fasting venous glycaemia
- HbA1c:
-
Glycated hemoglobin
- HDL-c:
-
High-density lipoprotein
- LDL-c:
-
Low-density lipoprotein
- MetS:
-
Metabolic syndrome
- SD:
-
Standard deviations
- SE:
-
Standard errors
- TG:
-
Triglycerides
- WC:
-
Waist circumference
- β:
-
Regression coefficients
References
La VJ. Differentiation sexually, factor determinant des formes de l’ob sit. Presse Med. 1947;30:339–40.
Haller H. Epidemiology and associated risk factors of hyperlipoproteinemia. Z Gesamte Inn Med. 1977;32:124–8.
Gerald BP. Relationship between serum sex hormones and glucose, insulin, and lipid abnormalities in men with myocardial infarction. Proc Natl Acad Sci U S A. 1977;74:1729–33.
Gerald BP. Sex hormones, risk factors and cardiovacular disease. Am J Med. 1978;65:7–11.
Gupta A, Gupta V. Metabolic syndrome : What are the risks for humans ? Biosci Trends. 2010;4(5):204–12.
Alberti KGMM, Zimmet PZ. Definition , Diagnosis and Classification of Diabetes Mellitus and its Complications Part 1 : Diagnosis and Classification of Diabetes Mellitus Provisional Report of a WHO Consultation; 1998. p. 539–53.
Expert panel on detection evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report (NCEP) -adult treatment panel III. J Am Med Assoc. 2001;285(19):2486–97.
Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome-a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 2006;23(5):469–80 Available from: http://doi.wiley.com/10.1111/j.1464-5491.2006.01858.x.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735–52.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; International. Circulation. 2009;120(16):1640–5.
Timóteo AT. Diet in patients with metabolic syndrome: what is the ideal macronutrient composition? Rev Port Cardiol (English Ed). 2018;37(12):1001–6. https://doi.org/10.1016/j.repce.2017.11.021.
Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: results from the a to Z weight loss study. Int J Obes. 2008;32(6):985–91.
Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73 Available from: http://www.nejm.org/doi/10.1056/NEJMoa0804748.
Steckhan N, Hohmann CD, Kessler C, Dobos G, Michalsen A, Cramer H. Effects of different dietary approaches on inflammatory markers in patients with metabolic syndrome: a systematic review and meta-analysis. Nutrition. 2016;32(3):338–48. https://doi.org/10.1016/j.nut.2015.09.010.
Beastall GH. Adding value to laboratory medicine: a professional responsibility. Clin Chem Lab Med. 2013;51(1):221–7.
Schmidt RL, Ashwood ER. Laboratory medicine and value-based health care. Am J Clin Pathol. 2015;144(3):357–8.
Sperandio N, Priore SE. Inquéritos antropométricos e alimentares na população Brasileira: Importante fonte de dados para o desenvolvimento de pesquisas. Cienc e Saude Coletiva. 2017;22(2):499–508.
Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a Meta-analysis. Am J Med. 2006;119(10):812–9.
Saltiel AR, Olefsky JM. Inflammatory linking obesity and metabolic disease and metabolic disease. J Clin Invest. 2017;127(1):1–4.
Calder PC, Ahluwalia N, Brouns F, Buetler T, Clement K, Cunningham K, et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br J Nutr. 2011;106(SUPPL. 3):S5–78.
Semnani-Azad Z, Khan TA, Blanco Mejia S, De Souza RJ, Leiter LA, Kendall CWC, et al. Association of Major Food Sources of fructose-containing sugars with incident metabolic syndrome: a systematic review and Meta-analysis. JAMA Netw Open. 2020;3(7):1–15.
World Health Organization. Obesity: preventing and managing the global epidemic of obesity. Rep WHO Consult Obes. 2000;252.
Lipschitz DA. Screening for nutritional status in the elderly. Prim Care. 1994;21(1):55–67.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Karvetti RL, Knuts LR. Validity of the 24-hour dietary recall. J Am Diet Assoc. 1985;85(11):1437–42 Available from: http://www.ncbi.nlm.nih.gov/pubmed/4056262.
National Institutes of Health. National Cancer Institute. Dietary Assessment Primer, 24-hour Dietary Recall (24HR) at a glance. 2017.
de Selem SSC, de Carvalho AM, Verly-Junior E, Carlos JV, Teixeira JA, Marchioni DML, et al. Validity and reproducibility of a food frequency questionnaire for adults of São Paulo, Brazil. Rev Bras Epidemiol. 2014;17(4):852–9.
Arquivos da Sociedade Brasileira de Cardiologia. Atualização da Diretriz Brasileira De Dislipidemias e Prevenção da Aterosclerose – 2017. SBC, vol. 109; 2017.
IOM/ Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, Fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Natl Acad Press. 2002;5:107–264.
Nettleton JA, Follis JL, Ngwa JS, Smith CE, Ahmad S, Tanaka T, et al. Gene × dietary pattern interactions in obesity: analysis of up to 68 317 adults of European ancestry. Hum Mol Genet. 2015;24(16):4728–38.
Koochakpoor G, Daneshpour MS, Mirmiran P, Hosseini SA, Hosseini-Esfahani F, Sedaghatikhayat B, et al. The effect of interaction between Melanocortin-4 receptor polymorphism and dietary factors on the risk of metabolic syndrome. Nutr Metab. 2016;13(1):1–9. https://doi.org/10.1186/s12986-016-0092-z.
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity. Circulation. 2016;133(2):187–225.
Jiao J, Liu G, Shin HJ, Hu FB, Rimm EB, Rexrode KM, et al. Dietary fats and mortality among patients with type 2 diabetes: analysis in two population based cohort studies. BMJ. 2019;366:8–11.
Afshin A, Micha R, Khatibzadeh S, Mozaffarian D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(1):278–88.
Martínez-González MA, Salas-Salvadó J, Estruch R, Corella D, Fitó M, Ros E. Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis. 2015;58(1):50–60. https://doi.org/10.1016/j.pcad.2015.04.003.
Jakulj F, Zernicke K, Bacon SL, Van Wielingen LE, Key BL, West SG, et al. A high-fat meal increases cardiovascular reactivity to psychological stress in healthy young adults. J Nutr. 2007;137(4):935–9.
O’Keefe JH, Bell DSH. Postprandial hyperglycemia/hyperlipidemia (postprandial Dysmetabolism) is a cardiovascular risk factor. Am J Cardiol. 2007;100(5):899–904.
Wilson AS, Koller KR, Ramaboli MC, Nesengani LT, Ocvirk S, Chen C, et al. Diet and the human gut microbiome: an international review. Dig Dis Sci. 2020;65(3):723–40. https://doi.org/10.1007/s10620-020-06112-w.
O’Keefe SJD. Diet, microorganisms and their metabolites, and colon cancer. Nat Rev Gastroenterol Hepatol. 2016;13(12):691–706 Available from: http://www.nature.com/articles/nrgastro.2016.165.
O’Keefe SJD. The association between dietary fbre defciency and high-income lifestyle-associated diseases: Burkitt’s hypothesis revisited. Lancet Gastroenterol Hepatol. 2019;4(12):984–96.
O’Keefe SJD. Plant-based foods and the microbiome in the preservation of health and prevention of disease. Am J Clin Nutr. 2019;110(2):265–6.
Kim Y, Je Y. Dietary fibre intake and mortality from cardiovascular disease and all cancers: a meta-analysis of prospective cohort studies. Arch Cardiovasc Dis. 2016;109(1):39–54. https://doi.org/10.1016/j.acvd.2015.09.005.
Park Y, Subar AF, Hollenbeck A, Schatzkin A. Dietary Fiber intake and mortality in the NIH-AARP diet and health study. Arch Intern Med. 2011;171(12):1–7 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf.
Benítez-Páez A, Gómez Del Pulgar EM, Kjølbæk L, Brahe LK, Astrup A, Larsen LH, et al. Impact of dietary fiber and fat on gut microbiota re-modeling and metabolic health. Trends Food Sci Technol. 2016;57:201–12.
Liu S, Willett WC, Manson JAE, Hu FB, Rosner B, Colditz G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr. 2003;78(5):920–7.
Krzyszycha R, Szponar B. Body mass index (BMI) and dietary preferences of women living in rural areas. Rocz Państwowego Zakładu Hig. 2009;60(1):75–7.
Tucker LA. Fiber intake and insulin resistance in 6374 adults: the role of abdominal obesity. Nutrients. 2018;10(2):237.
Trigueros L, Peña S, Ugidos AV, Sayas-Barberá E, Pérez-Álvarez JA, Sendra E. Food ingredients as anti-obesity agents: a review. Crit Rev Food Sci Nutr. 2013;53(9):929–42.
Solah VA, Kerr DA, Hunt WJ, Johnson SK, Boushey CJ, Delp EJ, et al. Effect of fibre supplementation on body weight and composition, frequency of eating and dietary choice in overweight individuals. Nutrients. 2017;9(2):1–14.
Eastwood MA, Morris ER. Physical properties of dietary fiber that influence physiological function: a model for polymers along the gastrointestinal tract. Am J Clin Nutr. 1992;55(2):436–42.
Lafond DW, Greaves KA, Maki KC, Leidy HJ, Romsos DR. Effects of two dietary fibers as part of ready-to-eat cereal (RTEC) breakfasts on perceived appetite and gut hormones in overweight women. Nutrients. 2015;7(2):1245–66.
Lee I, Shi L, Webb DL, Hellström PM, Risérus U, Landberg R. Effects of whole-grain rye porridge with added inulin and wheat gluten on appetite, gut fermentation and postprandial glucose metabolism: a randomised, cross-over, breakfast study. Br J Nutr. 2016;116(12):2139–49.
Byrne CS, Chambers ES, Morrison DJ, Frost G. The role of short chain fatty acids in appetite regulation and energy homeostasis. Int J Obes. 2015;39(9):1331–8. https://doi.org/10.1038/ijo.2015.84.
Sánchez D, Miguel M, Aleixandre A. Dietary fiber, gut peptides, and adipocytokines. J Med Food. 2012;15(3):223–30.
Schacter DL, Gilbert DT, Daniel MW. Semantic and episodic memory. 2nd ed. New York: Worth; 2011. p. 240–1.
National Institutes of Health; National Cancer Institute. Dietary Assessment Primer, 24-hour Dietary Recall (24HR) At a Glance Available from: https://dietassessmentprimer.cancer.gov/. [cited 3 Dec 2020].
DeBiasse MA, Bowen DJ, Quatromoni PA, Quinn E, Quintiliani LM. Feasibility and acceptability of dietary intake assessment via 24-hour recall and food frequency questionnaire among women with low socioeconomic status. J Acad Nutr Diet. 2018;118(2):301–7. https://doi.org/10.1016/j.jand.2017.08.011.
Acknowledgements
We would like to thank CAPES for the fellowship provided to the authors.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
KM: Conception and Design, methodology, data collection, analysis and interpretation of data, drafting the article, final approval. VW: Conception and Design, analysis and interpretation of data, article drafting, final approval. MQ: Critical revision, data interpretation, final approval. DF: Conception and Design, analysis of data, final approval. CC: Critical revision, supervision, final approval. EV: Critical revision, data interpretation, final approval. DV: Conception and Design, methodology, article drafting, supervision, final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Ethics Committee in Research with Human Beings of the State University of Londrina (protocol No. 2.837.313). Patients received information about the study objectives and procedures and signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Michalichen, K.C., Weber, V.M.R., Queiroga, M.R. et al. Impacts of food consumption on biochemical markers and anthropometric variables of women with metabolic syndrome. BMC Women's Health 22, 423 (2022). https://doi.org/10.1186/s12905-022-02010-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-02010-7