Abstract
Background
Endometriosis is an estrogen-dependent and chronic inflammatory disease affecting up to 10% of women. It is the result of a combined interaction of genetic, epigenetic, environmental, lifestyle, reproductive and local inflammatory factors. In this study, we investigated whether single nucleotide polymorphisms (SNPs) mapping to TNF-alpha (TNF, rs1800629) and IL-1beta (IL1B, rs1143634) and variable number tandem repeat polymorphism mapping to IL1-Ra (IL1RN intron 2, rs2234663) genetic loci are associated with risk for endometriosis in a Mexican mestizo population.
Methods
This study included 183 women with confirmed endometriosis (ENDO) diagnosed after surgical laparoscopy and 186 women with satisfied parity and without endometriosis as controls (CTR). PCR/RFLP technique was used for genotyping SNPs (rs1800629 and rs1143634); PCR for genotyping rs2234663.
Results
We found no statistical differences in age between groups nor among stages of endometriosis and the CTR group. We observed no difference in genotype and allele frequencies, nor carriage rate between groups in none of the three studied polymorphisms. The prevalence of TNF*2-allele heterozygotes (p = 0.025; OR 3.8), TNF*2-allele (p = 0.029; OR 3.4), IL1B*2-allele heterozygotes (p = 0.044; OR 2.69) and its carriage rate (p = 0.041; OR 2.64) in endometriosis stage IV was higher than the CTR group. Surprisingly, the carriage rate of IL1RN*2-allele (ENDO: p = 0.0004; OR 0.4; stage I: p = 0.002, OR 0.38; stage II: p = 0.002, OR 0.35; stage III: p = 0.003, OR 0.33), as well as the IL1RN*2-allele frequencies (ENDO: p = 0.0008, OR 0.55; I: p = 0.037, OR 0.60; II: p = 0.002, OR 0.41; III: p = 0.003, OR 0.38) were lower than the CTR group. Women with endometriosis stage IV (severe) had frequencies more alike to the CTR group in the IL1RN*2 allele frequency (31.2% vs. 27.2%) and carriage rate (37.5% vs. 41.9%).
Conclusion
Although these polymorphisms are not associated with the risk of endometriosis, Mexican mestizo women with severe stage of endometriosis have higher frequencies of TNF*2-, IL1B*2- and IL1RN*2-alleles, which may explain a possible correlation with disease severity rather than predisposition or risk.
Similar content being viewed by others
Background
Endometriosis is recognized as an estrogen-dependent and chronic inflammatory gynecological disease characterized by the presence and growth of endometrial-like tissue outside the uterine cavity. It affects at least 10% of women of reproductive age, leading to infertility and symptoms such as chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, dyschezia and fatigue [1]. Although several hypothesis and multiple factors have been proposed trying to explain its origin, the etiopathogenesis of endometriosis is still unknown. Being such a complex gynecological disease [2] different new theories have been proposed trying to explain its physiopathology nature. The “bacterial contamination theory” [3] suggests that recognition of bacteria could elicit the immune response (inflammation and dysregulation), playing a key role in its pathogenesis as endometriosis appears to be associated with elevated levels of different pathogenic species. The genetic-epigenetic (G/E) theory [4] proposes that after the accumulation of several cellular G/E events, the cell crosses a limit threshold which gives arise to a number of alterations. Epigenetics changes have been reported in ectopic endometrium related to inflammation, estrogen and progesterone receptors.
In this respect, non-immune and immune cells in the peritoneal microenvironment have been identified as the main source of estrogens, prostaglandins, and pro-inflammatory cytokines [5,6,7,8,9]. Hence, local inflammatory cytokine and prostaglandin production, immune cell infiltration, estrogen dominance, progesterone resistance, chronic local inflammation and oxidative stress are correlated and contribute to the central processes leading to pain, remodeling of neighboring tissues, fibrosis, adhesion formation, and infertility. Also, an aberrant immune system seems to play a key role, as it appears that women with endometriosis are more susceptible to autoimmune disorders (systemic lupus erythematous, Sjögren syndrome, rheumatoid arthritis, celiac disease, multiple sclerosis and inflammatory bowel disease) [10, 11] compared to general female population.
Inflammation is influenced by genetic susceptibility. Inflammatory cytokine genes polymorphisms have been subject of study trying to explain the etiology of gynecological (leiomyomas) [12, 13] and non-gynecological pathologies [14,15,16]. Although the contribution of genetics is well supported by many studies, they have not provided a simple and unambiguous answer to the etiology of endometriosis [17, 18].
Different gene loci have been identified as risk factors in endometriosis, including those related to growth factors, matrix remodeling, hormone receptors and metabolism, adhesion molecules, oxidative stress, cytokines, and inflammation [19]. The frequency distribution of gene polymorphisms varies according to the ethnic component of each human subpopulation, which partly explains the predisposition to disease and/or response to nutrients/pharmacological treatment [20, 21]. Tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β) are the first cytokines synthesized during the inflammatory process, while interleukin-1 Receptor antagonist (IL-1Ra) modulates and inhibits IL-1β activity [22].
The TNF-α gene (TNFA; 6p21.31) displays several single nucleotide polymorphisms (SNP) [23]. Specifically, the SNP in the promoter region (position G-308A) has been identified with an increased synthesis of TNF-α by carriers of the mutated allele (TNF*2) [24, 25]. The IL-1β gene (IL1B; 2q12.21) displays SNPs in the promoter region (T-31C, C-511 T) [26] and in the exon 5 (C+3954T) [27]. The latter has been identified with an increased production of this cytokine [28, 29], and it is associated with inflammatory diseases [30, 31]. The IL-1RA gene (IL1RN; 2q14.21) displays a variable number tandem repeat (VNTR) polymorphism in the intron 2 caused by 86 bp. There are six alleles according to the number of the 86-bp repeats: allele 1 (IL1RN*1) is the most common and has four repeats followed by allele 2 (IL1RN*2) with two repeats and three non-common alleles that have three (IL1RN*3), five (IL1RN*4) and six (IL1RN*5) repeats, respectively [32].
Data reported in the literature have associated endometriosis with several cytokine genes displaying both positive and negative associations [19, 33, 34]. Women with endometriosis might have a particular profile of cytokine polymorphisms, which might well determine them to respond with a greater inflammatory intensity, being this directly responsible of the biological alterations and symptoms suffered by this group of women. The aim of this study was to investigate the association of TNF-α (G-308 A), IL-1β (C+3954T) and IL1-Ra intron 2 VNTR polymorphisms with the risk of endometriosis in Mexican mestizo women.
Methods
Study design and patient population
In this case control study, we enrolled 369 adult women from a tertiary hospital in Mexico City. All women with infertility who attended the Department of Infertility and Sterility at the Instituto Nacional de Perinatología “Isidro Espinosa de los Reyes” (INPer) were considered eligible. The case group, called “endometriosis group” (ENDO), included 183 women diagnosed with endometriosis after undergoing laparoscopic surgery. Endometriosis staging was done according to the revised American Society for Reproductive Medicine (r-ASRM) staging score [35]. We did not include women that were diagnosed with pelvic inflammatory disease and those whose pain or infertility was due to other medical issues but endometriosis.
On the other hand, we invited all fertile women who attended the Department of Family Planning at INPer for bilateral tubal occlusion surgery as a definite contraceptive method to participate as "controls". The inclusion criteria were women without any apparent clinical symptom nor visual presence of endometriosis confirmed during the surgical procedure. The "control group" (CTR) included 186 women without endometriosis and confirmed fertility. We did not include fertile women that were diagnosed with pelvic inflammatory disease, endometriosis, or a medical history of myomas.
The Institutional Review Board and Ethics Committee of the INPer approved the study protocol (212250-06081). All procedures concerning this work comply with the Declaration of Helsinki. All women that accepted to participate were informed about the objectives and outcomes of the study and provided their written informed consent.
Blood samples collection and DNA extraction
Peripheral venous blood samples were collected in 7-mL heparin tubes (Becton Dickinson Vacutainer Systems, Franklin Lakes, NJ, USA) and taken to the laboratory immediately for DNA extraction. Genomic DNA was isolated from whole blood (100 µL) using 1 ml of the DNAzol Reagent (Invitrogen, ThermoFisher Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. The isolated DNA was stored at − 20 °C until it was used for the polymerase chain reaction (PCR) experiments.
TNF, IL1B and IL1RN genotyping
TNF-α (G-308A; rs1800629) and IL-1β (C+3954T, rs1143634) SNPs were determined by the polymerase chain reaction-restriction fragment length polymorphism (PCR-RLFP) method using the restriction enzymes NcoI [36] and TaqI [37], respectively, as described elsewhere. IL-1Ra intron 2 (VNTR; rs2234663) alleles were determined using a PCR protocol [38], as described elsewhere. PCR reagents (10X PCR Buffer, MgCl2, Taq DNA polymerase, and dNTPs) were purchased from Invitrogen (ThermoFisher Scientific, Waltham, MA, USA).
Amplification of the genomic fragments where the polymorphic sites are located was carried out using the primers and PCR settings described in Table 1. For each PCR amplification protocol, we used 50 ng template DNA, 1.5 mM MgCl2, 1 Unit Taq DNA polymerase, 20 pmol of each primer, 0.2 mM of each dNTP and PCR grade water in a total reaction volume of 25 µl. All reactions were performed in a Mastercycler gradient thermal cycler (Eppendorf Scientific, Hamburg, Germany).
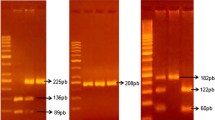
TNF (G-308A; rs1800629) RFLP
We digested 10 µL of PCR product (107 bp) with 4 units of NcoI restriction enzyme (Roche Molecular Biochem, Mannheim, Germany) during 24 h at 37 °C. Digestion product was analyzed by electrophoresis in a 4% agarose gel stained with ethidium bromide and visualized in an Epichemi3 Darkroom Transilluminator (UVP Inc., Upland, California, USA). The identification of two bands of 87 bp and 20 bp revealed TNF*1 allele; meanwhile, a single 107 bp band revealed TNF*2 allele.
IL1B (C+3954T, rs1143634) RFLP
We digested 10 µL of PCR product (182 bp fragment) with 7 units of TaqI restriction enzyme (Roche Molecular Biochem, Mannheim, Germany) during 24 h at 65 °C. Digestion product was analyzed by electrophoresis in a 6% acrylamide gel stained with ethidium bromide and visualized using an Epichemi3 Darkroom Transilluminator (UVP Inc. Upland, CA, USA). The identification of two bands of 97 bp and 85 bp revealed the IL1B*1 allele; meanwhile, a single band of 182 bp revealed the point mutation corresponding to the IL1B*2 allele.
IL1RN (rs2234663) VNTR
PCR product (20 µL) was analyzed by electrophoresis in a 2% agarose gel stained with ethidium bromide and visualized using an Epichemi3 Darkroom Transilluminator (UVP Inc. Upland, CA, USA). The identification of 412 bp, 240 bp, 326 bp, 498 bp, and 584 bp fragments corresponded to alleles 1, 2, 3, 4 and 5, respectively.
Statistical analyses
All statistical analyses were assessed using the software SigmaStat v. 3.1 (Systat Software Inc., CA, USA). Age and obstetric characteristics were compared using Student's t, U-Mann Whitney, and ANOVA of Kruskall-Wallis tests, where applicable. Allele frequencies, genotype frequencies and carriage rate were computed. The polymorphisms were tested for Hardy–Weinberg equilibrium by the goodness-of-fit χ2 test. The χ2 test was used to examine the differences of allele and genotype frequencies, as well as carriage rate between groups. The risk associations for endometriosis were estimated by the odds ratio (OR) with 95% confidence interval (95% CI) and a p-value < 0.05 was considered statistically significant.
Results
All women included in the CTR (n = 186) and ENDO (n = 183) group self-reported their ethnical origin as Mexican mestizo as their parents and grandparents were born in Mexico. All of them had middle educational (< 13 years) and socioeconomical status and lived in Mexico City or its surroundings. According to the rASRM classification, 63 (34.4%) women had endometriosis stage I (minimal), 54 (29.5%) stage II (mild), 117 (63.9%) stages I–II (minimal/mild), 42 (23.0%) stage III (moderate), 24 (13.1%) stage IV (severe) and 66 (36.1%) stages III–IV (moderate/severe). There were no statistically significant differences in the mean age between the CTR (33.8 ± 3.2 years) and ENDO (32.7 ± 2.5 years) group nor among rASRM stages of endometriosis and the control group (data not shown). Conversely, obstetric characteristics were significantly different between groups (p < 0.05). While the CTR group reported a median of three pregnancies, one vaginal delivery, one Cesarean delivery and zero abortions, the ENDO group reported zero pregnancies.
The genotype and allele frequency distribution of the TNF-α (− 308) polymorphism among the 369 women from the ENDO and CTR group is described in Table 2.
Allele and genotype frequencies in the study population were in Hardy–Weinberg equilibrium (p > 0.05). The distribution of TNF*1-allele homozygotes (p > 0.05) and TNF*2-allele heterozygotes (TNF*1/TNF*2) (p > 0.05) genotype frequencies was not statistically significant between groups. More than 85% of women in both groups were TNF*1 homozygotes. However, according to the r-ASRM staging, the prevalence of TNF*2-allele heterozygotes in stage IV was the only statistically different (p = 0.025) when compared to the CTR group. We did not identify the TNF*2-allele homozygote in our sample. A similar pattern was observed when we analyzed the TNF*1 and TNF*2 allele frequencies. No statistically significant difference was observed between groups (p > 0.05); except when endometriosis stage IV (p = 0.029) was compared to the CTR group. We also analyze the genotype and allele frequency of this polymorphism by grouping together stages I/II and stages III/IV and comparing them to the CTR group. However, no differences were found. The associations analysis suggests an approximate fourfold increased risk for women with endometriosis stage IV with TNF*2-allele heterozygote genotype and an approximate 3.5-fold increased risk with TNF*2-allele.
The genotype and allele frequencies distribution and the carriage rate of the IL-1β (+ 3954) polymorphism among the 369 women from the ENDO and CTR group is showed in Table 3.
Allele and genotype frequencies in the study population were in Hardy–Weinberg equilibrium (p > 0.05). The distribution of the three genotype frequencies (IL1B*1-allele homozygote, IL1B*2-allele heterozygote and IL1B*2-allele homozygote) and the carriage rate was not statistically significant between groups (p > 0.05). We identified that > 70% of women in both groups were IL1B*1 homozygotes. On the other hand, women with endometriosis stage I showed the highest frequency (80%) of this genotype, while those with endometriosis stage IV, the lowest (50%). Although the IL1B*2-allele heterozygote genotype frequency was similar between groups, we only found a statistically significant difference between women with stage IV endometriosis and the CTR group (p = 0.044). The IL1B*2-allele homozygote was found in a very low frequency (< 5%) in both groups and in all four stages of endometriosis. When we analyzed the carriage rate of IL1B*2 allele (*1*2 + *2*2), we found a statistically significant difference between women with endometriosis stage IV and the CTR group (p = 0.041). A similar pattern was observed when we analyzed the IL1B*1 and IL1B*2 allele frequencies. Regarding the IL1B*2-allele, its frequency was very alike between groups (15.1% vs. 16.7%) and no statistically significant difference was found (p > 0.05). Likewise, we found no statistical difference among the four stages of endometriosis and the CTR group, nor stages I/II, III/IV and the CTR group. The associations analysis suggests an approximate threefold increased risk for women with endometriosis stage IV with IL1B*2-allele heterozygote genotype and a tendency to a twofold increased risk with IL1B*2-allele [p = 0.056; OR 2.09; 95%CI (1.04–4.02)].
The genotypes and alleles frequencies distribution and the carriage rate of IL-1Ra (86 bp, VNTR) polymorphism is described in Table 4.
Allele and genotype frequencies in the study population were not in Hardy–Weinberg equilibrium (p < 0.05). The IL1RN*1-allele homozygote genotype was the most common of all in the ENDO group as well as in stages I-III (> 70%), but not for stage IV (58%). Conversely, this genotype was only present in 48% of women without endometriosis. The frequency of the IL1RN*1/IL1RN*2 genotype was higher in the CTR group (29%). The IL1RN*1/IL1RN*3 and IL1RN*1/IL1RN*4 genotypes showed very low frequencies (< 6%) and carriage rate (*1*3 + *1*4; < 10%) in both groups and in all four stages of endometriosis. However, we did not find IL1RN*1/IL1RN*4 genotype in women with endometriosis stage III and IV. The IL1RN*2-allele homozygote genotype frequency was very alike in both groups and no statistical difference was found among groups when compared to the CTR group. When we analyze the carriage rate of IL1RN*2-allele (*1*2 + *2*2), the ENDO group and the four stages of endometriosis had lower frequencies than the CTR group. All groups showed statistical difference, except for endometriosis stage IV. Surprisingly, all OR values were below 0.63 (a protective effect), except again for stage IV (OR 0.83). We found all alleles in both groups, except for IL1RN*5. The most common alleles were IL1RN*1 (68% and 80% in women without and with endometriosis, respectively) and IL1RN*2 (27% and 18% in women without and with endometriosis, respectively), as reported in the literature. Surprisingly, we observed a higher frequency of IL1RN*1 in women with endometriosis and a higher frequency of IL1RN*2 in the CTR group, which was statistically different (p < 0.0008). The frequency of IL1RN*3 and IL1RN*4 was < 3% in both groups. The ENDO group and endometriosis stages I-III had similar frequencies of IL1RN*1-allele (79.8–84.5%); however, this phenomenon was not observed in endometriosis stage IV, which frequency was very alike to that of the CTR group (67 vs. 68%). When we analyzed the IL1RN*2-allele frequency according to rASRM staging, all endometriosis stages showed statistical difference when compared to the CTR group, except for endometriosis stage IV (p > 0.05). Finally, we also found statistical differences in both carriage rate and IL1RN*2-allele frequency in both stage I/II and stage III/IV when compared to the CTR group.
Discussion
Endometriosis is a multifactorial disease where inflammation is actively involved in the initiation, establishment, and development of ectopic endometrial tissue in the peritoneal cavity. This process is highlighted by the involvement of pro-inflammatory cytokines synthesized by immune and non-immune cells present in the peritoneal microenvironment. In this study, we investigated the association of TNF-α (G-308A), IL-1β (C+3954T) and IL-1Ra (intron 2, VNTR) polymorphisms and endometriosis in Mexican mestizo women from Mexico City and its surroundings.
Positive (− 1031), negative (− 308, − 238) or ambiguous (− 863, − 857) associations [39] have been reported between TNF-α polymorphisms and endometriosis. Specifically, the − 308 polymorphism has been evaluated in nine studies [Asia (6), Europe (1) and Australia (1)], including ours (Mexico), and two systematic reviews and meta-analysis in Asians [40, 41] yielding negative associations in all cases. Regionally and geographically, the frequencies of TNF*2-allele have been shown to significantly differ. Wiezer (Austria) [42] and Hsieh (China) [43] described very similar genotype and allele frequencies in contrast to Zhao (Australia) [44], who studied haplotypes and found no association. Our results were very similar to that found by Lee (Korea) [45] and Babaabasi (Iran) [46]. Although the latter identified the TNF*2-allele homozygote (< 7%), we did not, as it appears to be very low or even absent in the American mestizo or Amerindian population [47, 48]. The higher prevalence of the TNF*2 heterozygote genotype observed in endometriosis stage IV (12.5%) might be related to an increased fashion synthesis of TNF-α by immune and non-immune cells, promoting the development and maintenance of endometriosis through the expression of different molecules related to growth, adhesion, maintenance, and survival.
There is still a scientific debate regarding the association of different IL-1β SNPs and endometriosis. All five studies (Turkey, Taiwan, China, Austria, Mexico) that have investigated the relationship between the C+3954T SNP and endometriosis found a negative association. The allele frequencies identified range from 1 to 43% in women with endometriosis [49,50,51,52]. Attar [51], like us, identified an increased frequency in endometriosis stage IV (27%, p = 0.056), which could be related to an increased synthesis of IL-1β by peritoneal immune and non-immune cells that can induce the expression of different molecules involved in the immunological dysfunctions contributing to the establishment and progression of the disease.
The regulation of IL-1β by IL-1Ra should be coordinated during inflammation to cease the immune response and limit the potential for immunopathology [53, 54]. Four studies (Taiwan, Korea, China and Mexico) [49, 52, 55], have evaluated the association between IL1-Ra VNTR polymorphism and endometriosis. Unlike them, who found IL1RN*1-allele homozygote in more than 84% and 92% of women with and without endometriosis, we observed it in 70% and 48%, respectively. Like Hsieh [49] and Wen [52], we found the IL1RN*1/IL1RN*2-allele heterozygote in approximately 10% of women with endometriosis. Nevertheless, this genotype was present in 30% of Mexican women without endometriosis, while they found it in < 6%. Surprisingly, we found the highest prevalence of the IL1RN*2-allele homozygote genotype (10% vs. 1%) and the IL1RN*2-allele in Mexican women with (18% vs. < 7%) and without endometriosis (27% vs. < 4%). Although Wen suggests an approximate 3.5-fold increased risk for Chinese women with endometriosis carrying the IL1RN*2-allele, we found this allele protective in Mexican women (except for endometriosis stage IV). The IL1RN*2-allele homozygote genotype has been associated with more prolonged and more severe proinflammatory immune response due to a decreased bioactivity/concentration of IL-1ra and with an increased production of IL-1β [56, 57]. The relationship between the IL-1RN genotype and its protein concentration has conflicting results because of the diversity of the environment, pathology and populations studied [57,58,59,60]. We do not know the biological meaning of a low frequency of IL1RN*2 allele and homozygote genotype in women with endometriosis. Nevertheless, the highest frequency of the IL1RN*2-allele homozygote genotype (25%) was observed again in endometriosis stage IV. This could lead to an insufficient production of IL-1Ra protein or to an overproduction of IL-1β in response to immune and/or inflammatory stimuli [60, 61], explaining why this allele could influence an individual’s susceptibility to endometriosis. Probably, this allele could genetically be associated with severity of disease (stage IV), rather than with predisposition [62]. Likewise, this could be related to an increased risk for intraperitoneal adhesion development [63], very common in severe stages of disease. A decreased production of IL-1Ra and an increase in IL-1β can contribute to a decrease in fibrinolysis during tissue repair [64].
To the best of our knowledge, the three polymorphisms evaluated in the present work are the first description of these genes in Mexican mestizo women with endometriosis. Although it appears that they are not associated with the risk of endometriosis, we identified that Mexican mestizo women with endometriosis stage IV have higher frequencies of TNF*2-, IL1B*2- and IL1RN*2-alleles than the CTR group, consistent with disease severity. Recent studies focused mainly on stage III/IV endometriosis, both recognized as severe stages of the disease, suggest a greater genetic burden when compared to stage I/II [65,66,67]. Genetic predisposition is an important factor in the etiology of endometriosis. Despite several genes and SNPs have been identified in the physiopathology and development [68, 69] of endometriosis, studies have demonstrated inconsistent and contradictory results due to its heterogeneous clinical manifestations and classification, research methodology, human genetic variability and different genetic ancestries and admixture. Thus, genetic research in endometriosis is complicated and has not been successful in providing replicable results.
A limitation of our study was the staging of endometriosis based on the rASRM score. Although it is the best well-known and the most used, it does not correlate well with clinical features and has drawbacks. Also, we did not include other associated genes and clustered polymorphism sites of lL-1, hence a haplotype analysis could not be done. A strength of our study is that all women (case and controls) were surgically evaluated for the presence/absence of endometriosis. More studies with larger sample sizes, well-matched controls, using other classifications of the disease (ENZIAN, Fertility score), considering more clustered polymorphisms, associated genes and other ethnic populations are necessary to definitively confirm the association of these polymorphisms reported by several studies. It would be necessary to evaluate in Mexican mestizo women other cytokine polymorphisms in the promoter region that have found associated to the disease [e.g. TNF (− 1031 T/C, − 863 C/A, − 857 C/T), IL-6 (− 634 T/C), or TGF-β (− 509 C/T)] [33]. Maybe these, among others, could help us explain the chronic local inflammation that has been related to the initiation, development and spread of endometriosis, as well as with the etiology of the symptoms, such as infertility and pain. Increasing the knowledge of genetic characteristics of inflammatory molecules in women with endometriosis from diverse ethnic groups will help us understand the onset and evolution of the phenomenon better.
Conclusion
Although these three polymorphisms are not associated with the risk of endometriosis, Mexican mestizo women with severe stage of endometriosis (stage IV) have higher frequencies of TNF*2, IL1B*2- and IL1RN*2-alleles, which may explain a possible correlation with disease severity rather than predisposition or risk.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the ClinVar repository with the following accession numbers (web links) to datasets: SCV002073726 (https://www.ncbi.nlm.nih.gov/clinvar/?term=SCV002073726 [clv_acc]), SCV002073727 (https://www.ncbi.nlm.nih.gov/clinvar/?term=SCV002073727 [clv_acc]) and SCV002073728 (https://www.ncbi.nlm.nih.gov/clinvar/?term=SCV002073728 [clv_acc]).
Abbreviations
- CTR:
-
Control group
- CI:
-
Confidence interval
- ENDO:
-
Endometriosis group
- IL-1β:
-
Interleukin-1beta
- IL1B*1:
-
IL-1β wild-type allele
- IL1B*2:
-
IL-1β mutated allele
- IL-1Ra:
-
Interleukin-1 receptor antagonist
- IL1RN*1:
-
IL-1Ra allele 1
- IL1RN*2:
-
IL-1Ra allele 2
- IL1RN*3:
-
IL-1Ra allele 3
- IL1RN*4:
-
IL-1Ra allele 4
- IL1RN*5:
-
IL-1Ra allele 5
- INPer:
-
Instituto Nacional de Perinatología
- OR:
-
Odds ratio
- rASRM:
-
Revised American Society of Reproductive Medicine
- SNP:
-
Single nucleotide polymorphisms
- TNF-α:
-
Tumor necrosis factor-alpha
- TNF*1:
-
TNF-α wild-type allele
- TNF*2:
-
TNF-α mutated allele
- VNTR:
-
Variable number tandem repeat
References
Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382:1244–56.
Wang Y, Nicholes K, Shih IM. The origin and pathogenesis of endometriosis. Annu Rev Pathol. 2020;15:71–95.
Khan KN, Fujishita A, Hiraki K, Kitajima M, Nakashima M, Fushiki S, et al. Bacterial contamination hypothesis: a new concept in endometriosis. Reprod Med Biol. 2018;17:125–33.
Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019;111:327–40.
Iwabe T, Harada T. Inflammation and cytokines in endometriosis. In: Harada T, editor. Endometriosis: pathogenesis and treatment. Tokyo: Springer; 2014. p. 87–106.
Nanda A, Keolo T, Banerjee P, Dutta M, Wangdi T, Sharma P, et al. Cytokines, angiogenesis, and extracellular matrix degradation are augmented by oxidative stress in endometriosis. Ann Lab Med. 2020;40:390–7.
Piccinato CA, Malvezzi H, Gibson DA, Saunders PTK. Contribution of intracrine oestrogens to the aetiology of endometriosis. J Mol Endocrinol. 2018;61:T253–70.
Lin Y-H, Chen Y-H, Chang H-Y, Au H-K, Tzeng C-R, Huang Y-H. Chronic niche inflammation in endometriosis-associated infertility: current understanding and future therapeutic strategies. Int J Mol Sci. 2018;19:2385.
Marquardt RM, Kim TH, Shin JH, Jeong JW. Progesterone and estrogen signaling in the endometrium: What goes wrong in endometriosis? Int J Mol Sci. 2019;20:66.
Zhang T, de Carolis C, Man GCW, Wang CC. The link between immunity, autoimmunity and endometriosis: a literature update. Autoimmun Rev. 2018;17:945–55.
Shigesi N, Kvaskoff M, Kirtley S, Feng Q, Fang H, Knight JC, et al. The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis Endometriosis and autoimmune diseases. Hum Reprod Update. 2019;25:486–503.
Hsieh YY, Chang CC, Tsai FJ, Lin CC, Yeh LS, Tsai CH. Tumor necrosis factor-α −308 promoter and p53 codon 72 gene polymorphisms in women with leiomyomas. Fertil Steril. 2004;82(SUPPL. 3):1177–81.
Pietrowski D, Thewes R, Sator M, Denschlag D, Keck C, Tempfer C. Uterine leiomyoma is associated with a polymorphism in the interleukin 1-b gene. https://doi.org/10.1111/j.1600-0897.2009.00718.x.
Rosier F, Brisebarre A, Dupuis C, Baaklini S, Puthier D, Brun C, et al. Genetic predisposition to the mortality in septic shock patients: from GWAS to the identification of a regulatory variant modulating the activity of a CISH s. Int J Mol Sci. 2021;22:5852.
Yuan F, Hung RJ, Walsh N, Zhang H, Platz EA, Wheeler W, et al. Genome-wide association study data reveal genetic susceptibility to chronic inflammatory intestinal diseases and pancreatic ductal adenocarcinoma risk. Can Res. 2020;80:4004–13.
Meenakshi P, Sumanlatha P. Genetic susceptibility of inflammatory genes in household contacts of tuberculosis patients with diabetes mellitus. J Bacteriol Mycol. 2020;7:1144.
Rahmioglu N, Montgomery GW, Zondervan KT. Genetics of endometriosis. Womens Health. 2015;11:577–86.
Vassilopoulou L, Matalliotakis M, Zervou IM, Matalliotaki C, Krithinakis K, Matalliotakis I, et al. Defining the genetic profile of endometriosis. Exp Ther Med. 2019;17:3267–81.
Kobayashi H, Imanaka S, Nakamura H, Tsuji A. Understanding the role of epigenomic, genomic and genetic alterations in the development of endometriosis (review). Mol Med Rep. 2014;9:1483–505.
Chanock S. Candidate genes and single nucleotide polymorphisms (SNPs) in the study of human disease. Dis Mark. 2001;17:89–98.
Gonzalez-Galarza FF, Christmas S, Middleton D, Jones AR. Allele frequency net: a database and online repository for immune gene frequencies in worldwide populations. Nucleic Acids Res. 2011;39 Database issue:D913–9.
Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281:8–27.
Bayley JP, Ottenhoff THM, Verweij CL. Is there a future for TNF promoter polymorphisms? Genes Immun. 2004;5:315–29.
Wilson AG, Symons JA, McDowell TL, McDevitt HO, Duff GW. Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA. 1997;94:3195–9.
Mira JP, Cariou A, Grall F, Delclaux C, Losser MR, Heshmati F, et al. Association of TNF2, a TNF-alpha promoter polymorphism, with septic shock susceptibility and mortality: a multicenter study. JAMA. 1999;282:561–8.
Banday MZ, Mir AH, Sameer AS, Chowdri NA, Haq E. Interleukin-1β (IL-1β) -31C/T and -511T/C promoter single nucleotide polymorphism in colorectal cancer in ethnic Kashmiri population—a case control study. Meta Gene. 2017;12:94–103.
Xu J, Yin Z, Cao S, Gao W, Liu L, Yin Y, et al. Systematic review and meta-analysis on the association between IL-1B polymorphisms and cancer risk. PLoS ONE. 2013;8:1–11.
Pani P, Tsilioni I, McGlennen R, Brown CA, Hawley CE, Theoharides TC, et al. IL-1B(3954) polymorphism and red complex bacteria increase IL-1β (GCF) levels in periodontitis. J Periodontal Res. 2021;56:501–11.
Pociot F, Mølvig J, Wogensen L, Worsaae H, Nerup J. A TaqI polymorphism in the human interleukin-1 beta (IL-1 beta) gene correlates with IL-1 beta secretion in vitro. Eur J Clin Invest. 1992;22:396–402.
Fu P, Xie S, Zhang X. Investigation of the IL-1β +3954 C>T polymorphism and the risk of sepsis: a case–control study. Medicine. 2020;99: e21022.
Kim HJ, Kim EH, Park AK, Shin Y, Kang J, Lim J, et al. Detection of association between periodontitis and polymorphisms of IL-1β + 3954 and TNF-α-863 in the Korean population after controlling for confounding risk factors. J Periodontal Res. 2020;55:905–17.
Vamvakopoulos JE, Taylor CJ, Morris-Stiff GJ, Green C, Metcalfe S. The interleukin-1 receptor antagonist gene: a single-copy variant of the intron 2 variable number tandem repeat (VNTR) polymorphism. Eur J Immunogenet. 2002;29:337–40.
Tempfer CB, Simoni M, Destenaves B, Fauser BCJM. Functional genetic polymorphisms and female reproductive disorders: part II—endometriosis. Hum Reprod Update. 2009;15:97–118.
Méar L, Herr M, Fauconnier A, Pineau C, Vialard F. Polymorphisms and endometriosis: a systematic review and meta-analyses. Hum Reprod Update. 2020;26:73–103.
Canis M, Donnez JG, Guzick DS, Halme JK, Rock JA, Schenken RS, et al. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817–21.
Wilson AG, di Giovine FS, Blakemore AIF, Duff GW. Single base polymorphism in the human tumour necrosis factor alpha (TNF alpha) gene detectable by NcoI restriction of PCR product. Hum Mol Genet. 1992;1:353.
Kornman KS, Crane A, Wang HY, di Giovine FS, Newman MG, Pirk FW, et al. The interleukin-1 genotype as a severity factor in adult periodontal disease. J Clin Periodontol. 1997;24:72–7.
Tarlow JK, Blakemore AI, Lennard A, Solari R, Hughes HN, Steinkasserer A, et al. Polymorphism in human IL-1 receptor antagonist gene intron 2 is caused by variable numbers of an 86-bp tandem repeat. Hum Genet. 1993;91:403–4.
Abutorabi R, Baradaran A, Sadat Mostafavi F, Zarrin Y, Mardanian F. Evaluation of tumor necrosis factor alpha polymorphism frequencies in endometriosis. Int J Fertil Steril. 2015;9:329–37.
Lyu J, Yang H, Lang J, Tan X. Tumor necrosis factor gene polymorphisms and endometriosis in Asians: a systematic review and meta-analysis. Chin Med J. 2014;127:1761–7.
Li J, Chen Y, Wei S, Wu H, Liu C, Huang Q, et al. Tumor necrosis factor and interleukin-6 gene polymorphisms and endometriosis risk in Asians: a systematic review and meta-analysis. Ann Hum Genet. 2014;78:104–16.
Wieser F, Fabjani G, Tempfer C, Schneeberger C, Zeillinger R, Huber JC, et al. Tumor necrosis factor-alpha promotor polymorphisms and endometriosis. J Soc Gynecol Investig. 2002;9:313–8.
Hsieh Y-Y, Chang C-C, Tsai F-J, Hsu Y, Tsai H-D, Tsai C-H. Polymorphisms for interleukin-4 (IL-4) -590 promoter, IL-4 intron3, and tumor necrosis factor alpha −308 promoter: non-association with endometriosis. J Clin Lab Anal. 2002;16:121–6.
Zhao ZZ, Nyholt DR, Le L, Thomas S, Engwerda C, Randall L, et al. Genetic variation in tumour necrosis factor and lymphotoxin is not associated with endometriosis in an Australian sample. Hum Reprod. 2007;22:2389–97.
Lee MK, Park AJ, Kim DH. Tumor necrosis factor-alpha and interleukin-6 promoter gene polymorphisms are not associated with an increased risk of endometriosis. Fertil Steril. 2002;77:1304–5.
Babaabasi B, Ahani A, Sadeghi F, Bashizade-Fakhar H, Khorram Khorshid HR. The association between TNF-alpha gene polymorphisms and endometriosis in an Iranian population. Int J Fertil Steril. 2019;13:6–11.
Garza-González E, Bosques-Padilla FJ, El-Omar E, Hold G, Tijerina-Menchaca R, Maldonado-Garza HJ, et al. Role of the polymorphic IL-1B, IL-1RN and TNF-A genes in distal gastric cancer in Mexico. Int J Cancer. 2005;114:237–41.
Acosta O, Solano L, Ore D, Salazar-Granara A, Sandoval J, Fujita R. Polimorfismo −308G/A en la región promotora del gen factor de necrosis tumoral alfa (TNFA) en diferentes subpoblaciones peruanas. Revista Horizontez Médicos. 2010;10:47–54.
Hsieh YY, Chang CC, Tsai FJ, Wu JY, Shi YR, Tsai HD, et al. Polymorphisms for interleukin-1 beta (IL-1 beta)-511 promoter, IL-1 beta exon 5, and IL-1 receptor antagonist: nonassociation with endometriosis. J Assist Reprod Genet. 2001;18:506–11.
Wieser F, Hefler L, Tempfer C, Vlach U, Schneeberger C, Huber J, et al. Polymorphism of the interleukin-1beta gene and endometriosis. J Soc Gynecol Investig. 2003;10:172–5.
Attar R, Agachan B, Kucukhuseyin O, Toptas B, Attar E, Isbir T. Association of interleukin 1beta gene (+3953) polymorphism and severity of endometriosis in Turkish women. Mol Biol Rep. 2010;37:369–74.
Jie Wen, Lin Deng. [Research on relationship between gene polymorphisms of interleukin-1 family and endometriosis]—PubMed. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2006;:653–7.
Arend WP, Malyak M, Guthridge CJ, Gabay C. Interleukin-1 receptor antagonist: role in biology. Annu Rev Immunol. 1998;16:27–55.
Hurme M, Santtila S. IL-1 receptor antagonist (IL-1Ra) plasma levels are co-ordinately regulated by both IL-1Ra and IL-1 I genes. Eur J Immunol. 1998;28:2598–602.
Chun S, Kim H, Ku S-Y, Suh CS, Kim SH, Kim JG. The association between endometriosis and polymorphisms in the interleukin-1 family genes in Korean women. Am J Reprod Immunol. 2012;68:154–63.
Wang P, Xia HHX, Zhang JY, Dai LP, Xu XQ, Wang KJ. Association of interleukin-1 gene polymorphisms with gastric cancer: a meta-analysis. Int J Cancer. 2007;120:552–62.
Danis VA, Millington M, Hyland VJ, Grennan D. Cytokine production by normal human monocytes: inter-subject variation and relationship to an IL-1 receptor antagonist (IL-1Ra) gene polymorphism. Clin Exp Immunol. 1995;99:303–10.
Bioque G, Crusius JBA, Koutroubakis I, Bouma G, Kostense PJ, Meuwissen SGM, et al. Allelic polymorphism in IL-1 beta and IL-1 receptor antagonist (IL-1Ra) genes in inflammatory bowel disease. Clin Exp Immunol. 1995;102:379.
Tountas NA, Casini-Raggi V, Yang H, Di Giovine FS, Vecchi M, Kam L, et al. Functional and ethnic association of allele 2 of the interleukin-1 receptor antagonist gene in ulcerative colitis. Gastroenterology. 1999;117:806–13.
Mwantembe O, Gaillard MC, Barkhuizen M, Pillay V, Berry SD, Dewar JB, et al. Ethnic differences in allelic associations of the interleukin-1 gene cluster in South African patients with inflammatory bowel disease (IBD) and in control individuals. Immunogenetics. 2001;52:249–54.
Santtila S, Savinainen K, Hurme M. Presence of the IL-1RA allele 2 (IL1RN*2) is associated with enhanced IL-1beta production in vitro. Scand J Immunol. 1998;47:195–8.
Arend WP. The balance between IL-1 and IL-1Ra in disease. Cytokine Growth Factor Rev. 2002;13:323–40.
Wieser F, Tempfer C, Schneeberger C, van Trotsenburg M, Huber J, Wenzl R. Interleukin-1 receptor antagonist polymorphism in women with peritoneal adhesions. BJOG Int J Obstet Gynaecol. 2002;109:1298–300.
Thakur M, Rambhatla A, Qadri F, Chatzicharalampous C, Awonuga M, Saed G, et al. Is there a genetic predisposition to postoperative adhesion development? Reprod Sci. 2021;28:2076–86.
Sapkota Y, Attia J, Gordon SD, Henders AK, Holliday EG, Rahmioglu N, et al. Genetic burden associated with varying degrees of disease severity in endometriosis. Mol Hum Reprod. 2015;21:594–602.
Rahmioglu N, Nyholt DR, Morris AP, Missmer SA, Montgomery GW, Zondervan KT. Genetic variants underlying risk of endometriosis: insights from meta-analysis of eight genome-wide association and replication datasets. Hum Reprod Update. 2014;20:702–16.
Liu JL, Zhao M. A PubMed-wide study of endometriosis. Genomics. 2016;108:151–7.
Joseph S, Mahale SD. Endometriosis knowledgebase: a gene-based resource on endometriosis. Database. 2019;2019:62.
Deiana D, Gessa S, Anardu M, Daniilidis A, Nappi L, D’Alterio MN, et al. Genetics of endometriosis: a comprehensive review. Gynecol Endocrinol. 2019;35:553–8.
Acknowledgements
We like to thank the Dirección de Investigación y Posgrado de la Universidad Iberoamericana Ciudad de México for their support in the realization of this project
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
The authors’ contributions are as follows: the study and research question were formulated by CHG. OCO and JJD performed the laparoscopic surgeries and the staging according to rASRM. JMC collected the samples, performed the DNA extraction and genotyping. OGC and MBJ performed and supervised the quality standards of the statistical analyses. JMC and APC analyzed the data and wrote the first draft of the manuscript. JMC, OCO, JJD, OGC, MBJ, APC and CHG contributed to the interpretation and discussion of the results and commented on the drafts. JMC and CHG review and edited the final draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board and Ethics Committee of the INPer approved the study protocol (212250-06081). All procedures concerning this work comply with the ethical standards of “Ley General de Salud en Materia de Investigación para la Salud”, as well as the Declaration of Helsinki. All women that accepted to participate were informed about the objectives and outcomes of the study and gave their informed written consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mier-Cabrera, J., Cruz-Orozco, O., de la Jara-Díaz, J. et al. Polymorphisms of TNF-alpha (− 308), IL-1beta (+ 3954) and IL1-Ra (VNTR) are associated to severe stage of endometriosis in Mexican women: a case control study. BMC Women's Health 22, 356 (2022). https://doi.org/10.1186/s12905-022-01941-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01941-5