Abstract
Background
Polycystic ovarian syndrome (PCOS) is of frequent occurrence in Saudi females and is often associated with obesity, insulin resistance, hypogonadotropic hypogonadism, and infertility. Since these features are also associated with leptin receptor (LEP-R) deficiency, several studies have attempted to link LEP-R gene polymorphisms to PCOS.
Methods
The purpose of this study is to assess the possible association of LEP-R gene polymorphism (rs1137101) with the main obesity-linked metabolic parameters in Saudi female patients affected by PCOS. A cohort of 122 Saudi female subjects, attending the outpatient’s clinics at Makkah, Saudi Arabia and diagnosed with PCOS was investigated. Metabolic parameters in serum samples, including lipidogram, glucose, leptin, ghrelin and insulin and obesity markers (BMI, W/H ratio, HOMA) were assayed and compared with values from 130 healthy female volunteers (controls). The genotyping of rs1137101 polymorphism in the leptin receptor gene by amplification (PCR) followed by DNA sequencing, was conducted in both groups (PCOS and controls).
Results
Waist/hip ratio (W/H ratio), leptin serum levels and triglycerides appeared to be associated with PCOS but, aside from W/H ratio (AA s GG p = 0.009), this association also occurred for controls. No significant association in the leptin gene polymorphic locus rs1137101 with PCOS was seen in the results of the present study. In the control group, BMI, W/H ratio, leptin, Insulin, and HOMA-IR were significantly higher in the GG genotype compared to AA.
Conclusion
Despite previous suggestion about a relationship between rs1137101, serum leptin levels, and PCOS, our studies do not show any statistical association and further investigations; possibly by also evaluating obese patients should be needed to elucidate this issue better.
Similar content being viewed by others
Introduction
Leptin receptor (LEP-R; OB-R; CD295), which is encoded by the LEPR gene, is a single-trans-membrane domain protein receptor of the cytokine receptor family [1] that binds the hormone leptin [2]. Cell membranes of a variety of cells in different organs and tissues harbor the LEP-R, signifying the role played by leptin in these tissues [3,4,5]. Even in the hypothalamus, the LEP-R is located in the cell membrane and is actively involved in the control of hunger and thirst and influences sleep, moods, and body temperature [6, 7]. Leptin, a polypeptide hormone, is a major player in regulating adipose tissue mass through hypothalamus effects on hunger and energy usage [6, 8]. Leptin binding to its receptor activates a series of chemical signals that influence hunger and helps in the generation of a feeling of fullness (satiety). Lean people generally have lower levels of leptin compared to their obese counterparts, and female gender, produce more leptin than their male counterpart [9]. Interest in the role of leptin in the weight control developed in the early ‘90s, and for over two decades leptin is closely linked to body weight fluctuations [10,11,12,13]. More recently it has become evident that such weight-related alterations may be a consequence of genetic variations in the LEP-R gene in the absence of any qualitative or quantitative leptin abnormality [14, 15]. In the LEP-R gene, several mutations are reported that alter the normal functional capacity of the LEP-R protein, resulting in an apparent “leptin receptor deficiency,” hence preventing either the binding of leptin to the receptor or the receptor from responding to the bond leptin. The consequences include excessive hunger, weight gain, and hypogonadotropic hypogonadism [16]. Severe obesity due to excessive eating (hyperphagia) begins in early childhood in LEP-R deficiency disorders and the hypogonadotropic hypogonadism, is caused by alleviated secretion of hormones involved in direct sexual development. Affected individuals experience the absence of or delay in puberty and later may suffer from infertility disorder. In a recent investigation, a statistically significant association was found between polycystic ovarian syndrome (PCOS), obesity and leptin, where the overweight and obese women with PCOS had higher serum levels of leptin compared with controls, though they have no association between PCOS and other adipokines, such as resistin and adiponectin [17]. This should prompt the researcher to deeply investigate this issue also in the influence of leptin gene polymorphism. Several polymorphisms have been reported in the LEP-R gene, which has been linked to a number of different disorders. One of the non-synonymous polymorphisms rs1137101 (Gln223Arg), is linked to insulin resistance, metabolic syndrome, dyslipidaemias, diabetes mellitus, obesity, besides several cancers (breast, colorectal, thyroid, prostate), preterm delivery, osteoarthritis, atherosclerosis, and ischemic heart disease [18,19,20,21,22,23,24,25]. We hypothesized that LEP-R gene polymorphisms might be associated with PCOS since the latter is associated with obesity, insulin resistance, hypogonadotropic hypogonadism, and infertility, all being common features of LEP-R deficiency [26]. Some associations have been reported, but the results have frequently been contradictory.
Among the Saudi women, PCOS is of frequent occurrence, though the exact frequency is yet not known (Babay Z; personal communication). In this study, the distribution of genotype and allele frequencies of the non-synonymous SNP rs1137101 (Gln233Arg) in the normal healthy Saudi females and Saudi PCOS patients, was investigated. We determined the effect of the different genotypes on the demographic and metabolic profiles. In this paper, we also present our results of association studies between rs1137101 polymorphism and PCOS and the effect of the polymorphism on demographic and metabolic profile in healthy females and those suffering from PCOS.
Methods
Study design and subjects
The study was conducted as a cross-sectional, case-control study and included 130 Saudi females suffering from PCOS, attending primary health clinics in Makkah, Saudi Arabia, and 122 normal healthy females also attending clinics for minor illnesses. The Institutional Review Board (IRB) at Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia approved the study (IRB No. 235) and each female was required to sign an informed consent form. Patients were attending the clinics of the clinical co-investigator (MHD) and were diagnosed using the criteria set by the Rotterdam consensus [27]. The controls were age-matched (± 2 years SD), with no clinical, biochemical or hormonal abnormalities. They also had normal ultrasonic ovarian morphology and were having regular ovulatory cycles (median 25–35 days). The inclusion and exclusion criteria were as published earlier [28]. None of the individuals were on anti-diabetic or anti-obesity drugs, glucocorticoids, or other hormonal therapy. None of the females were smoking and performed daily normal physical activity.
On a specific day, each patient and control was asked to attend the clinic following overnight fasting. The weight (Kg), height (cm), waist circumference and hip circumference were measured in the standing position and used to calculate the body mass index (BMI) (Kg/cm2) and waist-hip ratio (WHR).
Blood and serum samples
Venous peripheral blood samples were withdrawn following an overnight (12 h) fast. Fasting blood (2 ml) were collected into chilled (+ 4 °C) tubes containing 1.2 mg EDTA and aprotinin (500 KIU/ml, Trasylol, Bayer Corp., Leverkusen, Germany) for total ghrelin levels and 2 ml were drawn in fluoride tubes (gray top) for glucose estimation and 2 ml were collected in plain tubes for the biochemical analysis. All samples were immediately centrifuged, and the serum or plasma was stored at − 80 °C until further analysis. A whole blood sample collected in EDTA tubes was used to obtain genomic DNA using Gentra Systems Kit (Minneapolis, MN, cat # D5500).
Estimation of biochemical and hormonal parameters
Blood serum was used to determine the lipids (cholesterol, triglycerides, high-density lipoprotein [HDL-C] and low-density lipoprotein [LDL-C]), applying enzymatic methods using commercial kits (Boehringer Mannheim). Estimation of leptin, ghrelin and insulin were conducted following the methods presented in Daghestani et al. [28], The homeostatic model assessment insulin resistance (HOMA-IR) and insulin secretion were calculated using the following formulas: HOMA-IR = Fasting serum insulin (μU/ml) × Fasting plasma glucose (mmol l-1)/22.5), where FI is fasting insulin and G is fasting glucose.
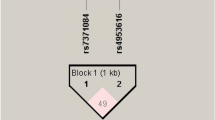
Genotyping of rs1137101 polymorphism in leptin receptor gene by DNA sequencing
The DNA fragment containing the exon 6 of LEP-R gene was amplified by polymerase chain reaction (PCR) using the following primers: sense primer (5′- TATAGGCCTGAAGTGTTAGAAG-3′) and antisense primer (5′- CCCATATTTATGGGCTGAACT-3′). The conditions for PCR amplification were: initial denaturation step at 95 °C for 15 min, followed by denaturation at 95 °C for 1 min for 34 cycles, annealing at 55 °C for 60 s, and DNA extension for 1 min at 72 °C, and final extension for 10 min at 72 °C. The PCR product was checked for purity and size on agarose gel electrophoresis and was subjected to DNA sequencing, applying an ABI Big Dye Terminator protocol using ABI 3100 Avant Genetic Analyzer.
Statistical analysis
Data for each female was entered on Excel spreadsheets and subjected to routine analysis using SPSS (Statistical Package for the Social Science, v22, Inc., Chicago, IL, USA). For each parameter mean ± SEM were obtained and results from different groups were compared using Student’s t-test or a Mann-Whitney U-test as appropriate. The patients and controls were grouped according to their genotypes, and the values of anthropometric, biochemical and hormonal parameters were calculated in each group and compared using a paired two-tailed Students ‘t’ test, separately in patients and controls. For all comparisons p < 0.05 was considered statistically significant.
Genotypes were manually counted in the PCOS and controls and those grouped as normal weight and obesity (PCOS and controls). The comparison of the genotype and allele frequencies in the patients and controls was obtained using the Statistical computational software available at Institute fur Humangenetik (URL: https://ihg.gsf.de/cgi-bin/hw/hwa1.pl). The odds ratio (OR), 2. 5-97.5% confidence intervals (CI), Chi-square (χ2) and p-value were calculated for each genotype and allele to compare the significance of the difference between the patients and controls. To assess the use of statistics in our samples and for independent samples evaluated with a t-test, the Cohen’s D test was used, calculated as the mean difference between two groups divided by the pooled standard deviation, according to:
Effect sizes (ES) can also be interpreted in terms of the percent of non-overlap of the treated group’s scores with those of the untreated group. In few words, the effect size gives the probability that a person selected at random from the group who were treated will have a higher score than a person picked at random from the control group. Furthermore, Hedges’s g values were computed from Cohen’s d. The parameter is an inferential measure, which is normally computed by using the square root of the mean square error (SEM) from the analysis of variance testing for differences between the two groups. To measure interaction, the ES correlation was also computed from Cohen’s d. In this case, the R-square value is the percentage of variance in the dependent variable that is accounted for by membership in the independent variable groups. For a Cohen’s d value of 1.0, the amount of variance in the dependent variable by membership in the treatment and control groups is 0,2% and r = 0.447 [29, 30].
Results
The study group included 122 healthy females of Saudi origin and another group of 130 women who were diagnosed as suffering from PCOS. The demographic, metabolic and hormonal parameters in the two groups were as presented in Daghestani et al. (28). The two groups matched for their ages and BMI but showed a significant difference in the W/H ratio, where the PCOS patients had a significantly higher ratio compared to the control group. Among the lipid parameters, all parameters were elevated in the PCOS compared to the control group except HDL, which was significantly lower. Insulin, glucose, and HOMA-IR were also significantly elevated in the PCOS, but leptin, ghrelin, and HOMA-S were not different significantly when compared with the control group.
The genotype and allele frequencies of rs1137101 in the control group were compared to the results in the PCOS patients. Table 1 presents the frequencies and shows that there were no significant differences between the two groups.
To determine differences in the genotype and allele frequencies in patients who were normal weight and obese, the control and patients were separated into two groups based on their BMI. Table 2 presents the genotype (AA, AG, GG) and allele (A and G) frequencies of rs1137101 in the normal weight and obese PCOS patients compared to normal weight and obese controls.
The PCOS and control group were separated into three groups based on the genotypes: AA, AG and GG and the demographic and metabolic data were separately calculated for each genotype. The results in the different genotypes were compared, and the significance of the difference in the results was recorded. In the control group, BMI, W/H ratio, leptin, Insulin, and HOMA-IR were significantly higher in the GG genotype compared to AA. In the PCOS group statistically significant differences were observed for W/H ratio and leptin in the AA vs. GG (p = < 0.05), in the PCOS, while in the AA vs. AG genotypes, the triglyceride levels were higher (p = 0.003). However, this genotype also associated with leptin and triglyceride level in the controls (p = 0.01). The results are presented in Table 3.
Subject’s distribution and statistical power were assessed by further tests, by evaluating the effect size on our sampling procedures. Table 4 describes the outputting results. Most of the comparisons (78.8%) showed a small non-overlapping percentage, calculated on Cohen’s d-effect size and demonstrate that for certain parameters (e.g., triglycerides SNP rs1137101 AA vs. AG) Cohen’s d and its co-related Gates’ delta and Hedges g, showed the same population overlapping between PCOS subjects and controls (see Table 4, 29.59 and 30.26%, respectively), assessing the sampling process performed in the study. Yet, this correspondence has not been observed for leptin (SNP rs1137101 AA vs. GG, see Table 4), what might also explain our negative data for leptin polymorphism association with PCOS, inducing out further research to improve cases and controls recruitment.
Discussion
The LEP-R gene has been extensively investigated in several populations, and the association has been investigated with a number of diseases including obesity, preterm delivery, recurrent spontaneous abortion and different cancers [16,17,18,19,20,21,22,23,24,25]. Several polymorphisms have been investigated, and rs1137101 has been commonly associated with several disorders. Our results showed that LEP-R gene SNP rs1137101 do not show any association with obesity either in the healthy normal Saudi population or the females suffering from PCOS. The only important association was reported for the waist/hip ratio (W/H ratio), while the association with lipidogram and leptin was also observed for non-PCOS individuals. Reports showing possible leptin-W/H ratio associations were suggested either for healthy people or several disorders and aging [31,32,33,34].
However, despite some recent conclusions on obese patients [35, 36] and cancer [35, 37], no report was yet published about the possible association of the SNP rs1137101 at the leptin gene. Recent reports showed that obesity should play a major role in the pathogenesis of PCOS through the insulin, leptin and endocannabinoid receptor, and by an association between insulin receptor polymorphism and PCOS was observed [38]. Furthermore, an association of the leptin gene SNPs (Gln223Arg and Pro1019Pro) with PCOS was recently reported in a Korean population [39]. Despite this interesting evidence, our data seem to confirm previous reports showing no association between leptin gene single nucleotide polymorphism and PCOS, though PCOS is frequently associated with insulin resistance and obesity and these conditions are linked to leptin resistance and expression in the leptin receptor. Past analyses demonstrated that patients diagnosed with PCOS did not show any mutation of the leptin coding exons, while the amino acid variants in exon 2, 4 and 12, through a single-stranded conformational polymorphism (SSCP) analysis, followed by sequencing, did not show any association between leptin and PCOS [40], suggesting that much more insightful evidence should be gained by further studies. The results of this study highlight an important point, i.e. the polymorphic change resulting from the substitution of an A by G, changing the codon, CAG to CGG, and replacing Gln, a neutral amino acid by Arg, a basic amino acid, brings about an effect thereby affecting the value of different anthropometric and biochemical parameters, both in normal control and PCOS patients. The exact mechanism by which these changes are brought about needs functional and in-silico studies, whereby the mechanism of leptin-LER-R interaction can be evaluated.
Finally, since our study did not show any statistical association between rs1137101 and PCOS, further investigation, possibly by also evaluating obese patients should be needed to elucidate this issue better.
Conclusion
In conclusion, the results of this study do not show any association between rs1137101 in the LEP-R gene and PCOS development in Saudi females. Association was observed with W/H ratio, leptin level and the lipidogram in the PCOS females. However, the association with leptin and lipidogram was also observed in the non-PCOS females. Further studies are warranted to determine the mechanism of interaction between leptin and its receptor, which results when Gln, a neutral amino acid, is replaced by Arg, a basic amino acid. Furthermore, whether there is any association between other SNPs in LEP-R and PCOS development in Saudis requires further detailed studies.
Abbreviations
- BMI (Kg/cm2):
-
Body Mass Index
- CI:
-
96% confidence intervals
- ECLlA:
-
Electrochemiluminescence immunoassay
- EDTA:
-
Ethylene diamine tetraacetate
- EIA:
-
Enzyme immunoassay
- G:
-
Fasting glucose
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostatic model assessment insulin resistance
- LDL:
-
Low-density lipoprotein
- LEPR gene:
-
Leptin receptor gene
- LEP-R, OB-R, CD295:
-
Leptin receptor
- OR:
-
Odds Ratio
- PCOS:
-
Polycystic ovarian syndrome
- PCR:
-
Polymerase chain reaction
- SEM:
-
Standard Error of the Mean
- SNP:
-
Single Nucleotide Polymorphism
- SSCP:
-
Single-stranded conformational polymorphism
- W/H:
-
Waist/hip ratio
- χ2:
-
Chi-square
References
Gorska E, Popko K, Stelmaszczyk-Emmel A, Ciepiela O, Kucharska A, Wasik M. Leptin receptors. Eur J Med Res. 2010;15(Suppl 2):50–4. https://doi.org/10.1186/2047-783X-15-S2-50.
Brunner I, Nick HHP, Cumin F, Chiesi M, Baum H-P, Whitebread S, Stricker-Krongrad A. Levens n. leptin is a physiologically important regulator of food intake. Int J obesity. 1997;21:1152–60.
Cioffi JA, Shafer AW, Zupancic TJ, Smith-Gbur J, Mikhail A, Platika D, Snodgrass HR. Novel B219/Ob receptor isoforms: possible role of leptin in hematopoiesis and reproduction. Nat Med. 1996;2:585–9.
Barr VA, Lane K, Taylor S. Subcellular localization and internalization of the four human leptin receptor isoforms. J Biol Chem. 1999;274:21416–24.
Caldefie-Chezer F, Poulin A, Tridon A, Sion B, Vasson MP. Leptin: a potential regulator of polymorphonuclear neutrophil bactericidal action? J Leukoc Biol. 2001;69:414–8.
Wada N, Hirako S, Takenoya F, Kageyama H, Okabe M, Shioda S. Leptin and its receptors. J Chem Neuroanat. 2014;61–62:191–9. https://doi.org/10.1016/j.jchemneu.2014.09.002 Epub 2014 Sep 16.
Valladares M, Obregón AM, Weisstaub G, Burrows R, Patiño A, Ho-Urriola J, Santos JL. Association between feeding behavior, and genetic polymorphism of leptin and its receptor in obese Chilean children. Nutr Hosp. 2014;31(3):1044–51. https://doi.org/10.3305/nh.2015.31.3.8049 Spanish. PubMed PMID: 25726191.
Denver RJ, Bonett RM, Boorse GC. Evolution of leptin structure and function. Neurendocrinology. 2011;94(1):21–38. https://doi.org/10.1159/000328435 Epub 2011 Jun 16.
Vettor R, De Pergola G, Pagano C, Englaro P, Laudadio E, Giorgino F. Gender differences in serum leptin in obese people: relationships with testosterone, body fat distribution and insulin sensitivity. Eur J Clin Invest. 1997;27(12):1016–24.
Leibel RL. Molecular physiology of weight regulation in mice and humans. Int J Obes. 2008;32(Suppl 7):S98–108. https://doi.org/10.1038/ijo.2008.245.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–32.
Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz D, Lallone RL, Burley SK, Friedman JM. Weight-reducing effects of the plasma protein encoded by the obese gene. Science. 1995;269:543–6.
Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D, Boone T, Collins F. Effects of the obese gene product on body weight regulation in Ob/Ob mice. Science. 1995;269:540–3.
Park KS, Shin HD, Park BL, Cheong HS, Cho YM, Lee HK, Lee JY, Lee JK, Oh B, Kimm K. Polymorphisms in the leptin receptor (LEPR)--putative association with obesity and T2DM. J Hum Genet. 2006;51(2):85–91 Epub 2005 Dec 7. PubMed PMID:16333525.
Van Rossum CT, Hoebee B, van Baak MA, Mars M, Saris WH, Seidell JC. Genetic variation in the leptin receptor gene, leptin, and weight gain in young Dutch adults. Obes Res. 2003;11:377–86.
Farooqi IS, O’Rahilly S. Human disorders of leptin action. J Endocrinol. 2014;223:T63–70.
Behboudi-Gandevani S, Ramezani Tehrani F, Bidhendi Yarandi R, Noroozzadeh M, Hedayati M, Azizi F. The association between polycystic ovary syndrome, obesity, and the serum concentration of adipokines. J Endocrinol Investig. 2017. https://doi.org/10.1007/s40618-017-0650-x.
Yiannakouris N, Yannakoulia M, Melistas L, Chan JL, Klimis-Zacas D, Mantzoros CS. The Q223R polymorphism of the leptin receptor gene is significantly associated with obesity and predicts a small percentage of body weight and body composition variability. Clin Endocrinol Metab. 2001;86:4434–9.
Chagnon YC, Wilmore JH, Borecki IB, Gagnon J, Perusse L, Chagnon M, et al. Associations between the leptin receptor gene and adiposity in middle-aged Caucasian males from the HERITAGE family study. J Clin Endocrinol Metab. 2000;85:29–34.
Guizar-Mendoza JM, Amador-Licona N, Flores-Martinez SE, LopezCardona ME, Ahuatzin-Tremary R, Sanchez-Corona J. Association analysis of the Gln223Arg polymorphism in the human leptin receptor gene, and traits related to obesity in Mexican adolescents. J Hum Hypertens. 2005;19(5):341–6.
Wauters M, Mertens I, Chagnon M, Rankinen T, Considine RV, Chagnon YC, et al. Polymorphisms in the leptin receptor gene, body composition and fat distribution in overweight and obese women. Int J Obes Relat Metab Disord. 2001;25:714–20.
Mahmoudi T, Farahani H, Nobakht H, Dabiri R, Zali MR. Genetic Variations in Leptin and Leptin Receptor and Susceptibility to Colorectal Cancer and Obesity. Iran J Cancer Prev. 2016;9(3):e7013. https://doi.org/10.17795/ijcp-7013.
He J, Xi B, Ruiter R, Shi T-Y, Zhu M-L, et al. Association of LEP G2548A and LEPR Q223R Polymorphisms with Cancer Susceptibility: Evidence from a Meta-Analysis. PLoS ONE. 2013;8(10):e75135. https://doi.org/10.1371/journal.pone.0075135.
Yang J, Du H, Lv J, Zhang L. Association of rs1137101 polymorphism in LEPR and susceptibility to knee osteoarthritis in a northwest Chinese Han population. BMC Musculoskelet Disord. 2016;17:311. https://doi.org/10.1186/s12891-016-1162-0.
Okobia MN, Bunker CH, Garte SJ, Zmuda JM, Ezeome ER, Anyanwu SN, et al. Leptin receptor Gln223Arg polymorphism and breast cancer risk in Nigerian women: a case control study. BMC Cancer. 2008;8:338. https://doi.org/10.1186/1471-2407-8-338.
Li L, Lee KJ, Choi BC, Baek KH. Relationship between leptin receptor and polycystic ovary syndrome. Gene. 2013;527(1):71–4. https://doi.org/10.1016/j.gene.2013.05.074 Epub 2013 Jun 13.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Daghestani MH, Daghestani M, Daghistani M, El-Mazny A, Bjørklund G, Chirumbolo S, Al Saggaf SH, Warsy A. A study of ghrelin and leptin levels and their relationship to metabolic profiles in obese and lean Saudi women with polycystic ovary syndrome (PCOS). Lipids Health Dis. 2018;17:195.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988.
Mellis C. Lies, damned lies and statistics: clinical importance versus statistical significance in research. Paediatr Respir Rev. 2017. https://doi.org/10.1016/j.prrv.2017.02.002.
Gómez JM, Maravall FJ, Gómez N, Navarro MA, Casamitjana R, Soler J. Interactions between serum leptin, the insulin-like growth factor-I system, and sex, age, anthropometric and body composition variables in a healthy population randomly selected. Clin Endocrinol. 2003;58:213–9.
Lisko I, Tiainen K, Stenholm S, Luukkaala T, Hurme M, Lehtimäki T, et al. Are body mass index, waist circumference and waist-to-hip ratio associated with leptin in 90-year-old people? Eur J Clin Nutr. 2013;67(4):420–2.
Artac M, Bozcuk H, Kiyici A, Eren OO, Boruban MC, Ozdogan M. Serum leptin level and waist-to-hip ratio (WHR) predict the overall survival of metastatic breast cancer (MBC) patients treated with aromatase inhibitors (AIs). Breast Cancer. 2013;20:174–80.
Barrios Ospino Y, Díaz N, Meertens L, Naddaf G, Solano L, Fernández M, Flores A, González M. Relation between leptin serun with weight and body fat distribution in postmenopausal women (in Spanish). Nutr Hosp. 2010;25:80–4.
Méndez-Hernández A, Gallegos-Arreola MP, Moreno-Macías H, Espinosa Fematt J, Pérez-Morales R. LEP rs7799039, LEPR rs1137101, and ADIPOQ rs2241766 and 1501299 polymorphisms are associated with obesity and chemotherapy response in Mexican women with breast cancer. Clin Breast Cancer. 2017. https://doi.org/10.1016/j.clbc.2017.03.010.
Zayani N, Omezzine A, Boumaiza I, Achour O, Rebhi L, Rejeb J, Ben Rejeb N, Ben Abdelaziz A, Bouslama A. Association of ADIPOQ, leptin, LEPR, and resistin polymorphisms with obesity parameters in Hammam Sousse Sahloul heart study. J Clin Lab Anal. 2017. https://doi.org/10.1002/jcla.22148.
Domingos PL, Farias LC, Pereira CS, das Graças Pena G, Reis TC, Silva RR, Fraga CA, de Souza MG, Soares MB, Jones KM, Menezes EV, Nobre SA, Rodrigues Neto JF, de Paula AM, Velásquez-Meléndez JG, Sena Guimarães AL. Leptin receptor polymorphism Gln223Arg (rs1137101) in oral squamous cell carcinoma and potentially malignant oral lesions. Springerplus. 2014;3:683. https://doi.org/10.1186/2193-1801-3-683.
Chen ZJ, Shi YH, Zhao YR, Li Y, Tang R, Zhao LX, Chang ZH. Correlation between single nucleotide polymorphism of insulin receptor gene with polycystic ovary syndrome. Zhonghua Fu Chan Ke Za Zhi. 2004;39(9):582–5.
Li L, Lee KJ, Choi BC, Baek KH. Relationship between leptin receptor and polycystic ovary syndrome. Gene. 2013;527(1):71–4.
Oksanen L, Tiitinen A, Kaprio J, Koistinen HA, Karonen S, Kontula K. No evidence for mutations of the leptin or leptin receptor genes in women with polycystic ovary syndrome. Mol Hum Reprod. 2000;6(10):873–6.
Acknowledgements
We thankfully acknowledge the grant from the Research Center, of the Female Scientific and Medical Colleges, Deanship of Scientific Reseach, King Saud University. We also acknowledge the participation of all patients and controls and the help provided by any other worker in the finalization of this study.
Funding
This research project was supported by a grant from the "Research Center" of the Female Scientific and Medical Colleges, Deanship of Scientific Research, King Saud University to Dr. Maha Daghestani. The funding body played no role in the designing of the study, collection, analysis, interpretation of the data or writing of the manuscript.
Availability of data and materials
All data is available with the first author (Dr. Maha Daghestani, Department of Zoology, Female Center for Scientific & Medical Colleges, King Saud University, Riyadh, Saudi Arabia) and can be provided when required.
Author information
Authors and Affiliations
Contributions
MD1 designed the experiment, carried all the experiments, MD1 MD2 and MD3 arranged the subjects/samples of the study. AW and SC performed the statistical analysis. MD1 and AW prepared the tables, drafted and finalized the manuscript. MD2, MD3, GB and SC participated in the manuscript revision and finalization. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical approval for this study was obtained from the local Institutional Review Board (IRB), at the Umm Al Qura University, Makkah Al Mukaramah, Saudi Arabia (IRB No. 235). Written informed consent was obtained from all subjects before their participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest, state that the manuscript has not been published or submitted elsewhere, state that the work complies with the Ethical Policies of the Journal and the work has been conducted under internationally accepted ethical standards after relevant ethical review.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Daghestani, M.H., Daghestani, M.H., Daghistani, M.H. et al. The influence of the rs1137101 genotypes of leptin receptor gene on the demographic and metabolic profile of normal Saudi females and those suffering from polycystic ovarian syndrome. BMC Women's Health 19, 10 (2019). https://doi.org/10.1186/s12905-018-0706-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-018-0706-x