Abstract
Background
Polycystic ovary syndrome (PCOS) is a common endocrine–metabolic disorder due to genetic and environmental factors. Genetic variants located in intron 1 of Fat mass and obesity-associated (FTO) gene are associated with increased risk of obesity and metabolic disorders. This study aims to investigate the association of common FTO polymorphism rs9939609 in South Indian women with PCOS to assess its association with metabolic and endocrine parameters. FTO genotyping was done on 100 PCOS patients and 70 controls by Sanger sequencing.
Results
The distribution of rs9939609 was observed between groups (28% TT, 57% TA, and 15% AA for PCOS and 37.1% TT, 51.4% TA, and 11.4% AA for the controls). In the PCOS group, across the carriers of different genotypes, a significant association was found between body mass index (BMI), fasting glucose levels, and testosterone with the presence of at least one risk allele of FTO rs9939609. Logistic regression analysis showed the association of fasting glucose levels and testosterone (OR 1.30 [1.03–1.63] and OR 5.83 [1.61–21.11], respectively) with FTO rs9939609.
Conclusions
Our findings indicated that FTO SNP rs9939609 was not associated with PCOS, but suggested a significant association of rs9939609 with hyperandrogenemia, fasting glucose levels, and BMI in South Indian women with PCOS.
Similar content being viewed by others
Background
Polycystic ovary syndrome (PCOS) is a common female endocrinology disorder with a prevalence between 5 and 26% depending on the population and diagnostic criteria applied [1, 2]. Three criteria were utilized for the diagnosis of PCOS. The National Institutes of Health (NIH) criteria introduced only oligo-anovulation and hyperandrogenism in PCOS diagnosis [3]. Another criterion is Androgen Excess and PCOS Society (AE-PCOS) criteria, which hyperandrogenism is central in diagnosis with combination with oligo-anovulation and/or PCO [4]. Finally, Rotterdam criteria define PCOS by the presence of at least two out of three criteria: oligo- or anovulation, clinical and/or biochemical hyperandrogenism, and polycystic ovaries (PCO) based on Rotterdam criteria [5]. PCOS remains a syndrome which means that no single diagnostic criterion (such as PCO and hyperandrogenism) is enough for clinical diagnosis [5]. The recent international PCOS guideline suggested the Rotterdam criteria for diagnosing PCOS [6].
Recent meta-analysis reports indicate the prevalence of PCOS 11.04% (Rotterdam), 3.39% (NIH), and 8.03% (AE-PCOS) [7]. According to another meta-analysis among different ethnicity, the prevalence of 5.6% was in Chinese women (Rotterdam), for Caucasians (NIH) 5.5%, Middle Eastern (NIH) 6.1%, (Rotterdam) 16.0%, (AE-PCOS) 12.6%, and Black women (NIH) 6.1% [8].
According to the Rotterdam criteria, a prevalence of 6% in South India was reported in 2017 [9]. Furthermore, the prevalence of 35.3% (Rotterdam), 34.3% (NIH), and 28.9% (AE-PCOS) in Kashmir valley has been reported [10].
PCOS women have multiple risk factors such as obesity, central obesity, and insulin resistance, which increase the risk of type II diabetes (3–7 times) according to the Rotterdam criteria [5]. Some studies reported that women with PCOS are exposed to other long-term risk factors such as cardiovascular disease [11,12,13] and endometrial cancer [14]. Metabolic syndrome, a combination of central obesity, dyslipidemia, hypertension, elevated fasting glucose levels, and insulin resistance, is observed in 30–40% of women with PCOS [15].
South Asians showed higher metabolic consequences of PCOS arising from a younger age with a greater degree of insulin resistance related to central adiposity, in contrast to White Caucasians with this condition [16]. Obesity is an important factor in the etiology of PCOS [17, 18]. Since both obesity and PCOS are highly hereditary, there is a strong possibility for a shared genetic predisposition leading to their co-occurrence [19].
In 2007, a single nucleotide polymorphism (SNP) of fat mass and obesity-associated (FTO) gene was reported by a genome-wide association study which was associated with increased body mass index (BMI) in both children and adults [20, 21]. The FTO gene is located on chromosome 16q12.2 [20] and encodes alpha-ketoglutarate-dependent dioxygenase protein expressed in a wide range of tissues, including adipose tissue and specific parts of the brain. However, the exact function of this protein is unclear. Most studies have shown that FTO is a regulator of fat mass, energy homeostasis, and adipogenesis [22]. Genetic variants of FTO and altered expression have been found to be linked with many obesity-related chronic diseases such as type-II diabetes [23] and cancer [24].
The FTO variant (rs9939609) is the most common SNP, consistently associated with obesity and type II diabetes in multiple populations [25]. The rs9939609 polymorphism is located in intron 1 of the FTO, which has two alleles, A and T. A allele is reported as a risk allele for obesity and type II diabetes [26].
An initial report on a large population in the UK revealed a strong association of SNP rs9939609 with obesity [20]. Consequently, several studies have been undertaken to investigate the relationship between the FTO gene and the risk of obesity. A recent meta-analysis based on eight Indian studies demonstrated that FTO variant rs9939609 increased the risk of obesity by 1.15 times [27]. Obesity is a frequent symptom among PCOS patients. It is reported that over 50% of PCOS subjects are overweight/obese [28]. The frequent co-occurrence of PCOS and obesity raises the possibility of shared genetic predispositions to both traits, and therefore, variants shown to influence BMI and risk factors for obesity are also possible candidates for PCOS. Therefore, the FTO gene may have a role in PCOS pathogenesis via BMI and/or obesity [29]. In European women with PCOS, rs9939609 SNP in the FTO gene modifies anthropometric measurements, as well as insulin sensitivity [30].
Thus far, researches have shown contradictory findings. Some studies confirmed an association with PCOS [19, 31,32,33], whereas others reported no such association [15, 34, 35]. These contradictory results may be due to different factors such as ethnicity, diagnosis criteria, or whether BMI was adjusted in each study. A meta-analysis in 2014 has suggested an effect of ethnicity on the association between FTO polymorphism and PCOS, which was significantly associated with East Asians but not Caucasians [36]. Therefore, there is a need for further studies to investigate the association of FTO gene polymorphism with PCOS in other populations, as there is no such report from the Indian population to the best of our knowledge.
This study aimed to investigate the impact of common polymorphism (rs9939609) of FTO gene on South Indian women with PCOS and healthy controls and to assess the association of this polymorphism with metabolic and endocrine parameters.
Methods
Participants
The study was conducted on 100 South Indian PCOS women and 70 controls in the reproductive age range of 18–45 years in December 2017 to October 2019 as a case–control association study. The study was approved by the Institutional Human Ethical Committee, University of Mysore, Manasagangothri, Mysore (No. 151/PhD/2017-18) , and written informed consent was obtained from all the subjects. PCOS samples were collected from private hospitals in Mysuru, Karnataka, India, namely Santasa IVF Centre, and Ashwini hospital.
According to the recent study [9], we assumed a PCOS prevalence of 6% in the South India. The following formula was applied to calculate the sample size in the current study [37]. Based on the following formula, the minimum sample size with a 95% confidence level should be 87 individuals, but we increase the sample size to 100 for the PCOS group to achieve more precise results.
n: sample size; Z: statistic corresponding to the level of confidence; P: expected prevalence; d: precision (corresponding to impact size).
PCOS samples were collected from private hospitals of xxxx, xxxx, India, namely xxxx, and xxxx hospital. They were diagnosed as PCOS according to the consensus of Rotterdam criteria satisfying at least two of the three criteria—chronic anovulation (oligo‑ and/or anovulation) was present, clinical (hirsutism was determined by Ferriman-Gallwey score ≥ 8) [38,39,40] and/or biochemical hyperandrogenism (serum testosterone more than 0.73 ng/ml or 1.82 nmol/L), and PCO (PCO is characterized by ≥ 12 follicles with the measurement of 2–9 mm in diameter, or ovarian volume should be more than 10 ml in at least one ovary) [5]. Women with Cushing's syndrome, adrenal 21-hydroxylase deficiency, androgen-secreting tumors, thyroid dysfunction, hyperprolactinemia, and other pituitary, adrenal or ovarian diseases were excluded. General information, reproductive information (menstruation, fertility), clinical features of PCOS, drug history, family history of PCOS, diabetes, heart disease, hypertension, and daily diet and physical activity were collected from each patient.
The control group was selected from healthy volunteer women aged between 18 and 45 years with normal ovulating cycles as well as normal ultrasound appearance of the ovaries, and without any history of thyroid disorder, dyslipidemia, insulin resistance, hypertension, diabetes, hyperandrogenism. Investigations were conducted by collecting each person's health history and documents, filling the genetic registry, and confirming the information by clinical and hormonal analysis.
BMI as a weight (kg) divided by the square of height (m) and waist circumference (WC) (at the midpoint between the lowest rib and iliac crest) were measured. Obese and overweight were defined according to the World Health Organization [41]. The waist-to-hip ratio (WHR) was calculated by the waist circumference divided by hip circumference. Resting blood pressure (BP) was assessed.
Metabolic analysis
During the 2nd–5th day of the menstrual cycle or any day in amenorrheic patients, the blood samples were collected from each subject after a 10–12 h overnight fast.
Plasma glucose levels were determined by the glucose oxidase–peroxidase method (ARKRAY Inc., Japan). Cholesterol, triglycerides, high-density lipoprotein (HDL) were assessed by an enzymatic method (Meril diagnostics, India), and low-density lipoprotein (LDL) was calculated by Friedewald equation. Fasting insulin levels were estimated by ELISA (CALBIOTECH, USA). Insulin resistance was assessed by homeostasis model assessment (HOMA-IR) Index = (fasting plasma insulin [in microunits per milliliter] × fasting plasma glucose [in milligrams per deciliter])/405 [42] and insulin sensitivity was assessed by the quantitative insulin sensitivity check index (QUICKI) = 1/log fasting insulin (in microunits per milliliter) + log fasting glucose (in milligrams per deciliter) [43]. Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) were estimated by commercial kits (Meril kit, India), and testosterone levels were estimated with an enzyme-linked fluorescent immunoassay method using mini VIDAS instrument (the Compact Automated Immunoanalyzer) and BioMérieux testosterone kit (Biomerieux, France). Five samples with high and five samples with low testosterone concentration were analyzed four times. The intra-assay coefficient of variation was 4.6%.
SNP genotyping
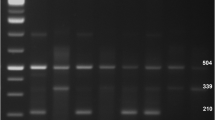
Peripheral blood samples were obtained from all participants and transferred into anticoagulant tubes. Genomic DNA extraction was done using a QIAamp DNA mini kit (QIAGEN, Germany) according to the manufacturer's protocol. Polymerase chain reaction (PCR) was performed with the primers for FTO rs9939609 (forward: 5′-GCAAAATGGCAACACACACT-3′; reverse: 5′-ACCCCCAGTACTACATCTACC-3′) with an initial denaturation 95 °C, 5′, 35 cycles of amplification; denaturation (95 °C, 45′′), annealing(50 °C, 45′′), elongation (72 °C, 30′′), and extension (72 °C, 5′). The PCR products were purified by Qiagen Gel purification kit and sequenced using the ABI 3130xl genetic analyzer (Applied Biosystems, USA).
Statistical analysis
All values were expressed as mean ± standard deviation (SD). For the evaluation of the normality of data distribution, the Shapiro–Wilks test was used. Independent t test and one-way analysis of variance (ANOVA) were applied for comparing the differences between groups. Leven's test was used to test the homogeneity of variance, and to recognize any heterogeneity of variance, Games–Howell test was performed. Post hoc was executed for multiple comparisons. Analysis of covariance (ANCOVA) was applied to exclude the possible confounding effects of age and BMI.
For comparison of genotype and allele frequency between groups, Chi-square test was applied. We used the binary logistic regression (forward LR) method to identify the PCOS development risk factors. All biochemical and hormonal variables and FTO (rs9939609) gene were analyzed by logistic regression to identify risk factors for PCOS.
Additionally, logistic regression was performed to analyze the association of metabolic variables with FTO polymorphism. In the regression model, FTO polymorphism as a dependent variable was categorized into two groups: AA + AT [mutant allele] and TT [wild allele]. Variables which were found to have an individually significant interaction were retained in the model. A p value < 0.05 was considered statistically significant. All analyses were performed on SPSS software (SPSS, version 23.0; IBM). SNPSTATS program [44] was applied to calculate the Hardy–Weinberg equilibrium, genotype, and allele frequency differences.
Results
Metabolic and endocrine characteristics of PCOS and control subjects
One hundred PCOS patients and 70 control subjects participated in the study. Clinical and hormonal measurements are presented in Table 1. In the PCOS group, 54% were obese and overweight, while the percentage was only 34% in the control group.
As expected, BMI and WC, LH, LH/FSH ratio, and testosterone levels were significantly higher in the PCOS group. Higher levels of other metabolic parameters such as BP ≥ 130/85 mm Hg, cholesterol, LDL, fasting glucose levels, insulin, HOMA-IR, QUICKI were observed, whereas there was a significant reduction in HDL (HDL < 50 mg/dL) when compared with the control group (Table 1).
Fasting glucose levels showed no significant differences between PCOS and control groups after age and BMI were adjusted by ANCOVA (Table 1).
Increased WC, diastolic blood pressure (DBP), LH/FSH ratio, and testosterone levels are significantly associated with PCOS
All variables and FTO rs9939609 polymorphism (categorized to TT and AA + AT) were applied for the logistic regression analysis to determine PCOS risk factors.
Logistic regression analysis showed the association of increased WC, DBP, LH/FSH ratio, and testosterone levels with PCOS. The final model demonstrated the significant associations of increased WC [OR 1.05 (1–1.09)], DBP [OR 1.26 (1.14–1.38)], LH/FSH ratio [OR 7.66 (3.71–15.77)], and testosterone levels [OR 8.76 (3.65–21.01)] with PCOS. Increased LH/FSH ratio and testosterone levels were more significantly associated than increased WC and DBP (Data not shown) (Additional file 1: Table S1).
Allele and genotype frequency
The genotype distributions of rs9939609 were consistent in the Hardy–Weinberg equilibrium across case–control groups. The genotype frequencies were as follows: 28% TT, 57% TA, and 15% AA for PCOS group and 37.1% TT, 51.4% TA, and 11.4% AA for control group.
Association between the FTO polymorphism and PCOS susceptibility was analyzed under additive, dominant, recessive models. The results in Table 2 demonstrated that the genotypes of rs9939609 were not associated statistically with the increased risk of PCOS (under additive, dominant, and recessive models). The allele frequency comparison is presented in Table 2, and no association was observed with PCOS [OR 1.30 (0.83–2.02)].
The samples were further divided into obese/overweight (BMI ≥ 25) and non-obese groups (BMI < 25) to observe the effect of BMI in the association of rs9939609 with both groups. In PCOS and controls, 54% (54/100) and 31% (24/70) were obese/overweight, respectively. The polymorphism was categorized as AA + AT and TT. The Chi-square results showed no significant association (obese/overweight group [OR 2.05(0.66–6.40)]; non-obese group [OR 1(0.43–2.29)]). Similarly, allelic association in obese/overweight and non-obese groups with PCOS was not significant (obese/overweight group [OR 1.03 (0.52–2.04)]; non-obese group [OR 1.21 (0.65–2.26)]) (Data not shown) (Additional file 1: Table S2).
Association of FTO polymorphism with fasting glucose levels, serum testosterone, and BMI in PCOS subjects
Genetic analysis of inheritance models did not show any significant association between the genotypes of rs9939609 and increased risk of PCOS. Furthermore, a genotype–phenotype association analysis was conducted on the PCOS group (Table 3). Most of the metabolic and endocrine characteristics were similar between genotypes. But individuals with at least one risk allele, AT and AA genotypes, had significantly higher BMI, fasting glucose levels, and testosterone levels compared with individuals carrying the wild TT genotype for SNP rs9939609 (Table 3).
Further analysis by logistic regression showed the association of fasting glucose levels and testosterone levels with FTO polymorphism in PCOS subjects (Table 4). Additionally, we applied logistic regression to analyze the association of variables with FTO variant in control subjects. The associated variable in the final model was LDL with OR: 1.01 and P value: 0.028. Although the p value was significant, the odds ratio showed a slight difference with 1, indicating that LDL is associated with the FTO variant but not strong in the control group.
Discussion
The present study suggests that fasting glucose levels and testosterone levels are associated with FTO variant rs9939609 in South Indian women with PCOS for the first time to the best of our knowledge. However, no association was observed between this polymorphism and the risk of PCOS. Similar PCOS studies across different populations did not show consistent results. Some studies demonstrated that FTO variant rs9939609 is significantly associated with PCOS [19, 31,32,33, 45, 46], while other studies found no association between that variant with PCOS but an association with obesity, hormonal, and metabolic traits in PCOS patients [15, 47,48,49,50].
The meta-analysis in 2014 suggests that there might be an association between FTO polymorphisms and PCOS risk, specifically in an East Asian population, although the association was dependent on adiposity [36]. Two other meta-analysis identified a significant association between FTO gene polymorphism rs9939609 and the risk of PCOS [29, 51], and a recent meta-analysis in 2020 has reported a significant association between FTO rs9939609 polymorphism with PCOS under different inheritance models [52].
Our study found no association between FTO variant rs9939609 and PCOS by genetic inheritance and logistic regression analysis even after subgrouping according to BMI. However, A risk allele was observed as more prevalent in the PCOS population than control but not statistically significant (Table 2).
Moreover, WC, DBP, LH/FSH ratio, and testosterone were detected in the logistic regression analysis as PCOS risk factors, especially LH/FSH ratio and testosterone. The FTO variant was not included in the model.
PCOS patients show several metabolic consequences and cardiovascular risk factors. Increased blood pressure is associated with obesity, glucose intolerance, and insulin‐resistant. The logistic regression analysis showed DBP as a PCOS risk factor. It may be due to DBP being a more effective cardiovascular risk factor than systolic blood pressure (SBP) until age 50 [53]. Our findings verified the study, which reports that the LH/FSH ratio can be used to diagnose PCOS [54]. Hyperandrogenemia is a common feature of PCOS [55], and obesity, especially central obesity, is one of the frequent consequences of PCOS.
Furthermore, we found the association of high testosterone levels with the FTO variant rs9939609 (Table 4). However, different studies have shown contradictory results of the association between the FTO gene and hyperandrogenemia. In one investigation on UK PCOS women, no association was found between FTO genotype and androgen level [19]. Another study on the Polish population showed no relationship between testosterone, sex hormone-binding globulin, and free androgen index with different genotypes [30]. However, some studies have reported an association of hyperandrogenemia with FTO variant 9939609 [33, 48]. The association may be mediated via a mechanism that leads to an increase in adiposity [56].
One study was conducted on European ethnicity women with PCOS, and another study on Sothern Brazilian women with PCOS demonstrated the association of fasting glucose levels with FTO [15, 49]. Nevertheless, few studies failed to report any relationship between glucose level and FTO [47, 57]. Furthermore, some studies showed no relationship between FTO and PCOS after adjusting with BMI [19, 34]; however, there was an association between risk allele A of FTO rs9939609 and increased 2-h glucose levels after correction for BMI. A similar higher 2-h glucose levels was observed in association with rs9939609 in women with PCOS in the absence of BMI adjustment [48]. Our study demonstrated an association between fasting glucose levels and FTO rs9939609 in South Indian PCOS women even after BMI adjustment (Tables 3, 4).
Increased BMI in subjects with AA and AT genotypes of variant rs9939609 of FTO (Table 3) is in agreement with previous studies, which report the relationship of the A allele with increased BMI [19, 30, 47, 48, 50].
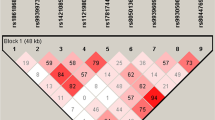
So far, studies were not successful in identifying the mechanism connecting the FTO gene directly to PCOS. Most investigations in which an association was reported between FTO and PCOS susceptibility also detected an increase in adiposity, which might be related to a genetic interaction of the FTO gene with other susceptibility genes, owing to the polygenic background of PCOS [30]. It is also essential to note that polymorphisms in FTO gene intron 1 are in linkage disequilibrium, posing difficulty in associating the best single SNP within this region with PCOS [15].
In the current study, we found the association between rs9939609 and hormonal and metabolic traits (testosterone levels, fasting glucose levels, and BMI) in the PCOS group similar to several previous studies in different populations but no association through inheritance genetic models [15, 47,48,49,50]. It can be due that race and region are two possible influences on the FTO association studies in PCOS subjects towing to ethnic genetic diversities. Furthermore, the Asian studies are commonly limited to East Asia, especially Chinese [31, 45, 50] and Korean population [47], while the participants in the current were exclusively South Indians. Also within Korean and Chinese populations FTO rs9939609 variant was associated with PCOS through obesity and metabolic disorders [45, 47].
Limitations
Some limitations in this study should be noted. Obesity and metabolic abnormalities are more prevalent in PCOS-affected older women than PCOS-affected younger women [58]. In the current study, PCOS and control age groups are 25.42 ± 2.91 and 23.08 ± 3.25, respectively. Since FTO intronic variants are associated with obesity and metabolic consequences, further investigation in various age groups, especially older ages in certain populations, is desired to generalize the result of the current study. Moreover, this study was limited to 100 samples of PCOS and 70 controls in the South of India. However, our study indicates the significant association of hyperandrogenemia, fasting glucose levels, and BMI with FTO variant rs9939609. Therefore, further studies with larger sample sizes are required to generalize the results in other populations.
Conclusions
The present study was the first to investigate the FTO gene variant rs9939609 association with PCOS susceptibility in South Indian women. Our findings indicated that FTO SNP rs9939609 was not related to PCOS, but suggests a significant association of FTO polymorphism rs9939609 with hyperandrogenemia, fasting glucose levels, and BMI in South Indian women with PCOS.
Availability of data and materials
Not applicable.
Abbreviations
- PCOS:
-
Polycystic ovary syndrome
- NIH:
-
National Institutes of Health
- AE-PCOS:
-
Androgen Excess and PCOS Society
- PCO:
-
Polycystic ovaries
- SNP:
-
Single nucleotide polymorphism
- FTO:
-
Fat mass and obesity-associated
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- LH:
-
Luteinizing hormone
- FSH:
-
Follicle-stimulating hormone
- QUICKI:
-
The quantitative insulin sensitivity check index
- BP:
-
Blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- SD:
-
Standard deviation
- ANOVA:
-
Analysis of variance
- ANCOVA:
-
Analysis of covariance
References
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE, Witchel SF (2006) Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an androgen excess society guideline. J Clin Endocrinol Metab 91(11):4237–4245
Sirmans SM, Pate KA (2014) Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol 6:1
Zawadski JK, Dunaif A (1992) Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. Blackwell Scientific Publications, Boston, pp 377–384
Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE, Witchel SF (2009) The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril 91(2):456–488
ESHRE TR, ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod 33(9):1602–1618
Naz MS, Tehrani FR, Majd HA, Ahmadi F, Ozgoli G, Fakari FR, Ghasemi V (2019) The prevalence of polycystic ovary syndrome in adolescents: a systematic review and meta-analysis. Int J Reprod BioMed 17(8):533
Ding T, Hardiman PJ, Petersen I, Wang FF, Qu F, Baio G (2017) The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: a systematic review and meta-analysis. Oncotarget 8(56):96351
Bharathi RV, Swetha S, Neerajaa J, Madhavica JV, Janani DM, Rekha SN, Ramya S, Usha B (2017) An epidemiological survey: effect of predisposing factors for PCOS in Indian urban and rural population. Middle East Fertil Soc J 22(4):313–316
Ganie MA, Rashid A, Sahu D, Nisar S, Wani IA, Khan J (2020) Prevalence of polycystic ovary syndrome (PCOS) among reproductive age women from Kashmir valley: a cross-sectional study. Int J Gynecol Obstet 149(2):231–236
Talbott E, Clerici A, Berga SL, Kuller L, Guzick D, Detre K, Daniels T, Engberg RA (1998) Adverse lipid and coronary heart disease risk profiles in young women with polycystic ovary syndrome: results of a case-control study. J Clin Epidemiol 51(5):415–422
Legro RS, Kunselman AR, Dunaif A (2001) Prevalence and predictors of dyslipidemia in women with polycystic ovary syndrome. Am J Med 111(8):607–613
Luque-Ramírez M, Mendieta-Azcona C, Alvarez-Blasco F, Escobar-Morreale HF (2007) Androgen excess is associated with the increased carotid intima-media thickness observed in young women with polycystic ovary syndrome. Hum Reprod 22(12):3197–3203
Hardiman P, Pillay OS, Atiomo W (2003) Polycystic ovary syndrome and endometrial carcinoma. The Lancet 361(9371):1810–1812
Ramos RB, Spritzer PM (2015) FTO gene variants are not associated with polycystic ovary syndrome in women from Southern Brazil. Gene 560(1):25–29
Wijeyaratne CN, DiliniUdayangani SA, Balen AH (2013) Ethnic-specific polycystic ovary syndrome: epidemiology, significance and implications. Expert Rev Endocrinol Metab 8(1):71–79
Taponen S, Martikainen H, Järvelin MR, Laitinen J, Pouta A, Hartikainen AL, Sovio U, McCarthy MI, Franks S, Ruokonen A (2003) Hormonal profile of women with self-reported symptoms of oligomenorrhea and/or hirsutism: Northern Finland birth cohort 1966 study. J Clin Endocrinol Metab 88(1):141–147
Barber TM, McCarthy MI, Wass JA, Franks S (2006) Obesity and polycystic ovary syndrome. Clin Endocrinol 65(2):137–145
Barber TM, Bennett AJ, Groves CJ, Sovio U, Ruokonen A, Martikainen H, Pouta A, Hartikainen AL, Elliott P, Lindgren CM, Freathy RM (2008) Association of variants in the fat mass and obesity associated (FTO) gene with polycystic ovary syndrome. Diabetologia 51(7):1153–1158
Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, Shields B (2007) A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316(5826):889–894
Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, Najjar S, Nagaraja R, Orrú M, Usala G, Dei M (2007) Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet 3(7):e115
Mizuno TM (2018) Fat mass and obesity associated (FTO) gene and hepatic glucose and lipid metabolism. Nutrients 10(11):1600
Wang Q, Wang J, Lin H, Huo X, Zhu Q, Zhang M (2018) Relationship between fat mass and obesity-associated gene expression and type 2 diabetes mellitus severity. Exp Ther Med 15(3):2917–2921
Huang X, Zhao J, Yang M, Li M, Zheng J (2017) Association between FTO gene polymorphism (rs9939609 T/A) and cancer risk: a meta-analysis. Eur J Cancer Care 26(5):e12464
Al-Serri A, Alroughani R, Al-Temaimi RA (2019) The FTO gene polymorphism rs9939609 is associated with obesity and disability in multiple sclerosis patients. Sci Rep 9(1):1–6
De Luis DA, Aller R, Conde R, Izaola O, de la Fuente B, Sagrado MG (2013) Relation of the rs9939609 gene variant in FTO with metabolic syndrome in obese female patients. J Diabetes Complicat 27(4):346–350
Vasan SK, Karpe F, Gu HF, Brismar K, Fall CH, Ingelsson E, Fall T (2014) FTO genetic variants and risk of obesity and type 2 diabetes: a meta-analysis of 28,394 Indians. Obesity 22(3):964–970
Shi Y, Guo M, Yan J, Sun W, Zhang X, Geng L, Xu L, Chen Z (2007) Analysis of clinical characteristics in large-scale Chinese women with polycystic ovary syndrome. Neuroendocrinol Lett 28(6):807–810
Liu AL, Xie HJ, Xie HY, Liu J, Yin J, Hu JS, Peng CY (2017) Association between fat mass and obesity associated (FTO) gene rs9939609 A/T polymorphism and polycystic ovary syndrome: a systematic review and meta-analysis. BMC Med Genet 18(1):1–7
Kowalska I, Malecki MT, Straczkowski M, Skupien J, Karczewska-Kupczewska M, Nikolajuk A, Szopa M, Adamska A, Wawrusiewicz-Kurylonek N, Wołczynski S, Sieradzki J (2009) The FTO gene modifies weight, fat mass and insulin sensitivity in women with polycystic ovary syndrome, where its role may be larger than in other phenotypes. Diabetes Metab 35(4):328–331
Yan Q, Hong J, Gu W, Zhang Y, Liu Q, Su Y, Zhang Y, Li X, Cui B, Ning G (2009) Association of the common rs9939609 variant of FTO gene with polycystic ovary syndrome in Chinese women. Endocrine 36(3):377–382
Saad WE, El Sebai AA, Maher MM, Heikal AM (2020) Study of the common variant rs9939609 of FTO gene polymorphism in polycystic ovary syndrome. Med Sci 24(106):3845–3854
Branavan U, Wijesundera S, Chandrasekaran V, Arambepola C, Wijeyaratne C (2020) In depth analysis of the association of FTO SNP (rs9939609) with the expression of classical phenotype of PCOS: a Sri Lankan study. BMC Med Genet 21(1):30
Ewens KG, Jones MR, Ankener W, Stewart DR, Urbanek M, Dunaif A, Legro RS, Chua A, Azziz R, Spielman RS, Goodarzi MO (2011) FTO and MC4R gene variants are associated with obesity in polycystic ovary syndrome. PLoS ONE 6(1):e16390
Kim JJ, Choi YM, Cho YM, Hong MA, Chae SJ, Hwang KR, Hwang SS, Yoon SH, Moon SY (2012) Polycystic ovary syndrome is not associated with polymorphisms of the TCF7L2, CDKAL1, HHEX, KCNJ11, FTO and SLC30A8 genes. Clin Endocrinol 77(3):439–445
Cai X, Liu C, Mou S (2014) Association between fat mass-and obesity-associated (FTO) gene polymorphism and polycystic ovary syndrome: a meta-analysis. PLoS ONE 9(1):e86972
Pourhoseingholi MA, Vahedi M, Rahimzadeh M (2013) Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench 6(1):14
Ferriman D, Gallwey JD (1961) Clinical assessment of body hair growth in women. J Clin Endocrinol Metab 21(11):1440–1447
Ramanand SJ, Ghongane BB, Ramanand JB, Patwardhan MH, Ghanghas RR, Jain SS (2013) Clinical characteristics of polycystic ovary syndrome in Indian women. Indian J Endocrinol Metab 17(1):138
Mani H, Davies MJ, Bodicoat DH, Levy MJ, Gray LJ, Howlett TA, Khunti K (2015) Clinical characteristics of polycystic ovary syndrome: investigating differences in White and South Asian women. Clin Endocrinol 83(4):542–549
World Health Organization. Obesity: preventing and managing the global epidemic. 2000.
Legro RS, Castracane VD, Kauffman RP (2004) Detecting insulin resistance in polycystic ovary syndrome: purposes and pitfalls. Obstet Gynecol Surv 59(2):141–154
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85(7):2402–2410
SNPStats. https://www.snpstats.net/start.htm. Accessed 10 February 2021.
Li T, Wu K, You L, Xing X, Wang P, Cui L, Liu H, Cui Y, Bian Y, Ning Y, Zhao H (2013) Common variant rs9939609 in gene FTO confers risk to polycystic ovary syndrome. PLoS ONE 8(7):e66250
Rizwan S, Ghazanvi S, Rasheed N, Ullah MI (2018) Association of FTO common RS9939609 polymorphism with obesity and polycystic ovarian syndrome in pakistani women. J Med Res Biol Stud 1:101
Kim JJ, Choi YM, Hong MA, Kim JM, Hwang SS, Lee GH, Chae SJ, Hwang KR, Yoon SH, Kim SH (2014) Gene dose effect between a fat mass and obesity-associated polymorphism and body mass index was observed in Korean women with polycystic ovary syndrome but not in control women. Fertil Steril 102(4):1143–1148
Wehr E, Schweighofer N, Möller R, Giuliani A, Pieber TR, Obermayer-Pietsch B (2010) Association of FTO gene with hyperandrogenemia and metabolic parameters in women with polycystic ovary syndrome. Metabolism 59(4):575–580
Saxena R, Welt CK (2013) Polycystic ovary syndrome is not associated with genetic variants that mark risk of type 2 diabetes. Actadiabetologica 50(3):451–457
Yuan H, Zhu G, Wang F, Wang X, Guo H, Shen M (2015) Interaction between common variants of FTO and MC4R is associated with risk of PCOS. Reprod Biol Endocrinol 13(1):1–6
Ying LI, Yongxia CH (2017) Fat mass and obesity associated gene polymorphism and the risk of polycystic ovary syndrome: a meta-analysis. Iran J Public Health 46(1):4
Wang X, Wang K, Yan J, Wu M (2020) A meta-analysis on associations of FTO, MTHFR and TCF7L2 polymorphisms with polycystic ovary syndrome. Genomics 112(2):1516–1521
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42(6):1206–1252
Malini NA, George KR (2018) Evaluation of different ranges of LH: FSH ratios in polycystic ovarian syndrome (PCOS)–Clinical based case control study. Gen Comp Endocrinol 1(260):51–57
Madnani N, Khan K, Chauhan P (2014) Polycystic ovarian syndrome: a review. Indian J Dermatol Venereol Leprol 80(2):154
Song DK, Lee H, Oh JY, Hong YS, Sung YA (2014) FTO gene variants are associated with PCOS susceptibility and hyperandrogenemia in young Korean Women. Diabetes Metab J 38(4):302–310
Kowalska I, Adamska A, Malecki M, Karczewska-Kupczewska M, Nikolajuk A, Szopa M, Gorska M, Straczkowski M (2012) Impact of the FTO gene variation on fat oxidation and its potential influence on body weight in women with polycystic ovary syndrome. Clin Endocrinol 77(1):120–125
Hsu MI (2013) Changes in the PCOS phenotype with age. Steroids 78(8):761–766
Acknowledgements
We acknowledge all participants of our study for their valuable samples. We thank Dr. N.B.Ramachandra for his help and support during the research work. We especially thank Dr. Sonia Mandappa, director of Mother care clinic and Ashwini. We thank Mediwave hospital lab staff for helping in sample collection. We thank department of studies Genetics & Genomics, University of Mysore, Manasagangothri, Mysuru, India.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ZN was involved in the conceptualization, methodology, investigation, data acquisition and analysis, funding acquisition and writing—original draft and review. SSM was involved in the supervision and project administration. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Institutional Human Ethical Committee, University of Mysore, Manasagangothri, Mysore (No. 151/PhD/2017-18), and written consent was obtained from all the subjects.
Consent for publication
None.
Competing interests
We declare that we have no (financial and non-financial) competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary tables: S1 and S2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Naghshband, Z., Malini, S.S. Association of FTO gene variant rs9939609 with hyperandrogenemia and fasting glucose levels in South Indian women with polycystic ovarian syndrome. Egypt J Med Hum Genet 23, 79 (2022). https://doi.org/10.1186/s43042-022-00236-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00236-6