Abstract
Background
Interventions that promote adjuvant endocrine therapy (AET) adherence are critical to improve breast cancer survival. The development of interventions would benefit from a better understanding of the reasons for adherence and the causal relationships of determinants using theoretical or model approaches. The aim of the present study was to identify reasons for AET adherence in breast cancer patients with sequential relationships and inter-relationships.
Methods
A total of 210 participants with estrogen receptor positive breast cancer who received AET completed a questionnaire assessing demographic/medical, psychological, and endocrine therapy (ET)-specific factors. A descriptive analysis was performed to identify meaningful variables. Selected variables were subjected to hierarchical regression and path analyses. The path model was tested and modified based on the research framework and the results of regression weights and model fit.
Results
Analysis of sequential effects showed that ET-specific factors contributed the largest proportion of variance (13.4%) to predict AET adherence, followed by psychological factors (4.6%) and demographic/medical factors (3.1%). Analysis of inter-relationships showed that demographic/medical factors such as AET regimen type and cancer stage have direct effects on AET adherence, whereas psychological factors contribute indirectly through the mediating effects of ET-specific factors.
Conclusion
Assessments and interventions that encompass the patient’s medication beliefs, self-efficacy, and depression are needed to promote AET adherence.
Similar content being viewed by others
Background
To reduce the risk of recurrence and mortality in women diagnosed with hormone receptor positive breast cancer, current guidelines generally recommend 10 years of adjuvant endocrine therapy (AET) [1]. Despite the efficacy of AET, adherence rates range from 41% to 72% when measured over 4 years [2]. Early discontinuation or non-adherence to AET is associated with increased mortality [3]. Therefore, interventions aimed at improving AET adherence are critical to increase breast cancer survival rates.
The development of patient-centered intervention strategies is important to promote patient adherence to treatment. Identifying the determinants of adherence and explaining the causal relationship of determinants using theoretical or model-based methods may help understand the reasons for adherence and thus the development of patient-centered intervention approaches.
Two analytical methods were proposed to examine the relationships between variables based on current models [4]. Hierarchical regression analysis is useful to assess the effect of determinants on predicting the outcome in a sequential manner. Path analysis is well suited to evaluate the inter-relationships between determinants and their direct and indirect effects on the outcome.
A study that examined the hierarchical effects of determinants for AET adherence suggested the existence of three levels of determinants, namely, demographic/medical factors, psychological factors, and endocrine therapy (ET)-specific factors [5]. Demographic/medical factors include variables such as age, education, employment status, type of AET, and operation type [5,6,7]. Depression, anxiety, and perceived physical symptoms [8,9,10] could be categorized into psychological factors. ET-specific factors include necessity-concerns beliefs on medication and self-efficacy with regard to AET [8, 11].
However, the inter-relationships between AET adherence factors have not been investigated yet. The patient adherence model hypothesized patient-related determinants of adherence in a more comprehensive way to determine inter-relationships between AET adherence factors [12]. According to the determinants of the patient adherence model, which examined for dyspepsia medication adherence, demographic/medical and psychological factors could contribute to necessity-concerns beliefs on medication and self-efficacy. These associations could be applied to the analysis of patients who are prescribed AET. The design of patient centered interventions to improve adherence could be considerably facilitated by determining the reasons for adherence from both sequential relationships and inter-relationships.
The purpose of the present study was to identify reasons for adherence with sequential relationships and inter-relationships. Based on previous studies [8, 12], we proposed two hypotheses within the research framework (Fig. 1). First, three levels of determinants would affect AET adherence sequentially. Second, demographic/medical and psychological factors could affect ET-specific factors, and determinants could contribute indirectly to ET therapy adherence. We identified the level of determinants that are predictable and the level of determinants with a high impact using hierarchical regression analysis. In addition, the path model from the research framework was evaluated and modified to identify the optimal model to explain AET adherence using path analysis.
Methods
Design and participants
A cross-sectional design was used in the present study. Participants were recruited from the outpatient clinic of Asan Medical Center, a University-affiliated hospital in South Korea, between July 15 and August 24, 2016. All patients with histologically confirmed breast cancer were consecutively screened for eligibility. The selection criteria were as follows: age ≥ 20 years; a completed regimen of neoadjuvant or adjuvant chemotherapy; a diagnosis of stage 0, 1, 2, or 3 breast cancer; no history of psychiatric or neurologic illness; no recurrence or presence of secondary breast cancer; and ongoing AET for breast cancer at the time of the visit. After screening for eligibility, 400 eligible patients were asked to participate by a research nurse and 254 patients consented. Out of 254 patients, 44 patients were excluded because they had not responded entirely to all of the questions in the questionnaire. In total, data from 210 patients (52.5%) were used in the analyses. All participants completed written informed consent forms approved by the Institutional Review Board (no. 2016–0351).
Study variables
Adherence
Adherence to AET therapy was assessed using the Morisky Medication Adherence Scale-8 (MMAS-8) questionnaire, which uses an 8-item scale [13,14,15]. Scores obtained on the MMAS-8 range from 0 to 8, with higher scores indicating higher adherence. Permission to use the validated Korean MMAS-8 was obtained from Dr. Morisky.
Demographic/medical level variables
Demographic variables included age, marital status, menopausal status, employment status, educational level, and family history of cancer. Medical variables included the type of AET, time from the start of AET, type of surgery, cancer stage, and completion of chemotherapy or radiotherapy. Demographic and medical variable data of the participants were retrieved using the electronic medical record (EMR) system with the consent of patients.
Psychological level variables
Menopause-related symptoms were measured using the 11-item Menopause Rating Scale (MRS) [16]. Patients responded to 11 items on a 5-point Likert scale ranging from 0 (no complaints) to 4 (severe symptoms). The Korean version of the MRS scale was obtained from the MRS network (http://www.menopause-rating-scale.info) after obtaining permission from Dr. Heinemann.
Symptoms of depression were measured using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D) developed by the National Institute of Mental Health. The Korean version of the CES-D that was specifically developed for Korean populations was used [17, 18]. Patients were asked to indicate their responses using a 4-point Likert scale (from 0 = rarely or never to 3 = almost all or all of the time). Scores ranged from 0 to 60, with higher scores reflecting more severe depression symptoms.
The short version of the Fear of Progression Questionnaire (FoP-Q-SF), a 12-item scale [19, 20], was used to measure the degree of fear of disease progression. The FoP-Q-SF items were scored on a 5-point Likert scale ranging from 1 (never) to 5 (very often), with higher values indicating higher levels of anxiety.
ET-specific level variables
The beliefs about AET were assessed using the Beliefs about Medicines Questionnaire (BMQ)-Specific. The questionnaire includes five queries that address the necessity of prescribed medications (necessity beliefs) and five queries that address concerns regarding potentially adverse consequences while taking the medications (concern beliefs). Each subscale score ranges from 5 to 25, with higher BMQ-necessity scores meaning higher perceived medication necessity, and higher BMQ-concern scores indicating higher perceived medication concerns. The BMQ-Specific was used with the permission of the questionnaire developer, Prof. Horne [21]. The original English version of the BMQ-Specific was translated to Korean and then translated back to English by two independent clinical experts and a native English speaker to ensure semantic and structural equivalency [22].
Participants responded to questions of the Korean version of the general self-efficacy (GSE) scale [23], which was originally developed in Germany by Matthias Jerusalem and Ralf Schwarzer [24]. The GSE is a 10-item psychometric scale ranging from 0 to 40, with higher scores representing a higher level of self-efficacy.
Analysis
A descriptive analysis of the demographic/medical, psychological, and ET-specific characteristics was performed. The correlation between these independent variables and the MMAS was determined to identify meaningful variables that could be subjected to hierarchical regression and path analyses. Correlation analysis was used for continuous variables, and the t or F test was used for categorical variables.
To identify the sequential effects of the three levels of determinants, selected variable sets were entered into a hierarchical regression analysis in three steps: demographic/medical variables, psychological variables, and ET-specific variables.
The inter-relationships between selected demographic/medical, psychological, and ET-specific variables were investigated. The first path model was designed in accordance with the hypothesis of three levels of determinants. The path model was tested and modified by adding and removing a path based on the research framework and the results of regression weights and model fit [4, 25]. The model fit was compared using the Chi-square, normed fit index (NFI), comparative fit index (CFI), and root mean square error of approximation (RMSEA) methods. Standardized coefficients and calculated direct, indirect, and total effects were reported. IBM SPSS 23 and AMOS 21 were used for analysis.
Results
Characteristics according to the three levels
A total of 210 patients were included in the study. The mean age of patients was 50.31 years (SD = 9.03, range = 25–76), and most of them were married (90.4%). There were 19 (9.0%) participants who had a family history of breast cancer, and 83 (39.5%) participants who had a family history of other cancers. Most participants had conservational surgery (87.1%), and received selective estrogen receptor modulators (SERMs) (77.6%). The mean time on AET was 26.75 months (Table 1).
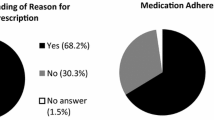
The mean score for AET therapy adherence was 6.36 (SD = 1.65, range = 0.3–8.0). When the mean score was compared to the cutoff for adherence [13], there were 54 (25.7%) highly adherent patients with a score of 8 on the scale, 79 (37.6%) medium adherers with a score of 6 or 7, and 77 (36.7%) low adherers with a score of below 6.
At the demographic/medical level, participants who had invasive cancer (stage 1–3) (t = 2.554, p = 0.011) and received aromatase inhibitors (AI) (t = 2.068, p = 0.040) had higher MMAS scores.
At the psychological level, a lower CES-D score indicating a lower depression level was significantly related to a higher MMAS score. Patient with higher necessity beliefs and self-efficacy and lower concerns beliefs tended to have higher MMAS scores at the ET-specific level.
Sequential effects of determinants according to the three levels
Based on the three levels of determinants, cancer stage, AET regimen type, depression, necessity belief, concerns belief, and self-efficacy were identified as significant variables. To compare the effects of the three levels of determinants, MMAS scores were regressed to the variables using hierarchical regression analysis. The first model contained only cancer stage and AET regimen type and accounted for 3.1% of the variance in ET therapy adherence [F (2,195) = 3.087, p = 0.048]. The second model included the depression variable and accounted for 7.7% of the variance [F (3,194) = 5.418, p = 0.001]. The change of R-square was significant (p = 0.002). The final model included concerns belief, necessity belief, and self-efficacy and accounted for 21.1% of the variance [F (6,191) = 8.488, p < 0.001]. The change of R-square was also significant (p < 0.001). This can be interpreted as ET-specific factors explaining the largest proportion (13.4%) of variance. In the final model, AET regimen type (β = 0.147, p = 0.027), concerns belief (β = − 0.287, p < 0.001), necessity belief (β = 0.284, p < 0.001), and self-efficacy (β = 0.142, p = 0.045) contributed to adherence significantly. The depression and concerns belief scores had negative effects on adherence in accordance with Pearson’s coefficients (Table 2).
Inter-relationships between determinants
The first path model (Fig. 2-path model 1) was tested, and the model fit indices were unacceptable, showing a significant Chi-square value [χ2 (df = 11, n = 210) = 84.404, p < 0.001, CFI = 0.489, RMSEA = 0.179, NFI = 0.508]. The paths were modified according to the statistical analysis results and a review of the literature. The analysis showed that depression had a stronger relation to concerns beliefs (r = 0.506, p < 0.001) and self-efficacy (r = − 0.397, p < 0.001) than to ET adherence (r = − 0.204, p = 0.004), and it had a weak relationship with necessity belief (r = 0.139, p = 0.051). Demographic/medical factors including AET regimen type and cancer stage were not related to psychological and ET-specific factors. After changing the paths and testing the models (Fig. 2-path model 2), a final model was obtained (Fig. 2-path model 3). The model fit indices of the final path model indicated a good fit to the data [χ2 (df = 12, n = 210) = 6.722, p = 0.875, CFI = 1.0, RMSEA < 0.001, NFI = 0.961]. All the direct path coefficients were significant at the 0.05 level. The standardized path coefficients linking depression to concerns beliefs and depression to self-efficacy were relatively large (Fig. 2-b). The total effect was largest in necessity belief to ET adherence (Table 3).
Discussion
In the present study, determinants of AET adherence were examined regarding sequential relationships and inter-relationships.
Univariate analysis showed that MMAS scores differed significantly according to AET regimen type and cancer stage. Also, MMAS scores correlated with depression, beliefs on medication and self-efficacy. Thus, these variables were selected for further multivariate analyses.
Analysis of the sequential effects of the three factors showed that ET-specific factors were responsible for the largest variance (13.4%) to predict AET adherence, followed by psychological factors (4.6%) and demographic/medical factors (3.1%). Additional entry of each factor increased R2 significantly, resulting in a final regression model that accounted for 21.1% of the variance in adherence. This result was consistent with those of previous studies [8, 26] and carries implications for intervention strategies based on the three levels of factors. In detail, depression was statistically significant in model 2, which includes only demographic/medical and psychological factors. However when ET-specific factors were added, depression was no longer significant. Therefore, additional analyses of the direct and indirect effects of the determinants were performed.
There are few reports on the effect of AET regimen type on adherence. One study reported that AET regimen type is a determinant for adherence [6, 27]. The present data did not show an association between AET regimen type and psychological variables or ET-specific variables. However, among the demographic/medical factors, AET regimen type had a significant relationship with age (t = 10.842, p ≤ 0.001), FSH level (t = 12.488, p < 0.001), and node metastasis (χ2 = 7.123, p = 0.008). Similar to AET regimen type, cancer stage was not related to psychological variables or ET-specific variables in the present study, whereas a relationship with type of surgery (χ2 = 4.378, p = 0.036) was identified from the data. AET regimen type and cancer stage seemed to show a relationship with other demographic/medical factors that affect AET adherence. Additional studies could be suggested to explain these relationships.
The demographic/medical level findings indicated that they have direct effects on AET adherence, rather than indirect effects as predisposing factors of psychological or ET-specific level factors. Variables identified at this level draw attention because they are non-modifiable risk factors and specific characteristics of breast cancer patients.
Depression is a known determinant of medication adherence. However, the mechanism underlying the relationship between depression and medication adherence is not well understood. A previous study suggested that participants who are anxious or depressive in the early stages of treatment are likely to be motivated to take medication [9]. By contrast, the results of our study indicated that highly depressive patients tend to be non-adherent, and this result is consistent with those of other previous studies [8, 28, 29]. We have tried to explain this result as an indirect effect of depression with ET-specific factors, since the effects of self-efficacy and medication beliefs on medication adherence are known. High self-efficacy, high positive beliefs on medication, and low negative beliefs on medication are more likely to lead to adherence to prescribed medications [5, 11, 30]. Several studies which focused on self-efficacy and medication beliefs as mediators linking depression and medication adherence. A Schoenthaler, G Ogedegbe and JP Allegrante [31] found that self-efficacy played a mediating role between depression and medication adherence in hypertensive patients. ME Hilliard, MN Eakin, B Borrelli, A Green and KA Riekert [32] reported that medication beliefs were the mediators in cystic fibrosis patients. The present study supports the idea that depression contributed to ET-specific factors. Higher depression was statistically related to higher concerns beliefs, lower self-efficacy, and consequently lower adherence to AET. Although necessity beliefs were not affected by depression, there was a significant association between concerns beliefs and necessity beliefs. The direct effect of depression on medication adherence was not significant when the mediating variables were included in the model. The mechanism underlying the relationship between depression and medication adherence can be explained using ET-specific factors as mediating factors including self-efficacy and medication beliefs. These results suggest that assessments and interventions need to consider the patient’s medication beliefs, self-efficacy, and depression to promote AET adherence. Interventions could vary according to the associated depression. Interventions for medication beliefs and self-efficacy are usually delivered by educating and counseling, whereas treatments for depression could include a pharmacological approach [28]. In addition, the efficacy of depression self-care intervention for increasing self-efficacy was reported previously [33].
Understanding the mechanism underlying medication adherence is important to increase the adherence rate and promote a positive health outcome, and there are ongoing efforts to explain this mechanism. To the best of our knowledge, these efforts have mainly focused on identifying determinants of AET adherence. Few studies have addressed the relationships among the factors [6, 30]. We designed a research framework based on the hierarchical model of AET adherence determinants [8] and a determinants of adherence model that was developed for dyspepsia medication [12]. Our data showed that associations between psychological factors and ET-specific factors were well fitted to the research framework, whereas demographic/medical factors showed discrepancies with the research framework. Finally, a path model was generated to explain the adherence to AET using demographic/medical, psychological, and ET-specific factors. These results could be used during the development of patient-centered interventions. Tailored interventions could be planned depending on the regimen and cancer stage. Also, the patient’s medication beliefs and self-efficacy should be assessed in combination with depression to implement individualized interventions.
The cross-sectional study design of the present study limits the interpretation of the results as causal relationships. To explain the causal relationships with evidence, we hypothesized relationships based on previous research and evaluated by path analysis. Additional studies are needed to confirm these relationships. Although our sample was from one of the top five major cancer treating about 15% of all breast cancer patients in Korea and the patients were recruited by five different surgeons, bias could have occurred because the participants were recruited in a single tertiary hospital setting and the reason for the rejection of non-participants was not analyzed. More analyses assuring the representativeness of the study population will be needed to decrease the bias. Lastly, the AET adherence data were collected using subjective measurements based on self-reporting. The poor ability of self-reports to measure adherence is well known [34, 35]. Although we used MMAS-8, which has shown reliability and validity, further studies using objective measurements will be necessary.
Conclusion
The present study investigated the determinants of AET adherence as AET regimen type and cancer stage at the demographic/medical level, depression at the psychological level, and belief and self-efficacy at the ET-specific level. Despite the direct effects of AET regimen type and cancer stage on AET adherence, depression contributes as an ET-specific factor such as concerns beliefs and self-efficacy. To promote AET adherence, assessments and interventions should consider the patient’s medication beliefs, self-efficacy, and depression level.
Abbreviations
- AET:
-
Adjuvant endocrine therapy
- AI:
-
Aromatase inhibitor
- BMQ:
-
Beliefs about Medicines Questionnaire
- CES-D:
-
Center for Epidemiological Studies-Depression Scale
- CFI:
-
Comparative fit index
- CT:
-
Chemotherapy
- EMR:
-
Electronic medical record
- ET:
-
Endocrine therapy
- FAM HX:
-
Family history
- FoP-Q-SF:
-
Fear of Progression Questionnaire
- FSH:
-
Follicle-stimulating hormone
- GSE:
-
General self-efficacy
- MMAS:
-
Morisky Medication Adherence Scale
- MRS:
-
Menopause Rating Scale
- NFI:
-
Normed fit index
- RMSEA:
-
Root mean square error of approximation
- RT:
-
Radiotherapy
- SERM:
-
Selective estrogen receptor modulator
References
Burstein HJ, Temin S, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis CA, Rowden D, Solky AJ, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(21):2255–69.
Murphy CC, Bartholomew LK, Carpentier MY, Bluethmann SM, Vernon SW. Adherence to adjuvant hormonal therapy among breast cancer survivors in clinical practice: a systematic review. Breast Cancer Res Treat. 2012;134(2):459–78.
Hershman DL, Shao T, Kushi LH, Buono D, Tsai WY, Fehrenbacher L, Kwan M, Gomez SL, Neugut AI. Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat. 2011;126(2):529–37.
Berndt AE, Williams PC. Hierarchical regression and structural equation modeling: two useful analyses for life course research. Family & community health. 2013;36(1):4–18.
Brett J, Fenlon D, Boulton M, Hulbert-Williams NJ, Walter FM, Donnelly P, Lavery B, Morgan A, Morris C, Watson E. Factors associated with intentional and unintentional non-adherence to adjuvant endocrine therapy following breast cancer. European journal of cancer care. 2016;
Jacob Arriola KR, Mason TA, Bannon KA, Holmes C, Powell CL, Horne K, O'Regan R. Modifiable risk factors for adherence to adjuvant endocrine therapy among breast cancer patients. Patient Educ Couns. 2014;95(1):98–103.
Hershman DL, Kushi LH, Shao T, Buono D, Kershenbaum A, Tsai WY, Fehrenbacher L, Gomez SL, Miles S, Neugut AI. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28(27):4120–8.
Stanton AL, Petrie KJ, Partridge AH. Contributors to nonadherence and nonpersistence with endocrine therapy in breast cancer survivors recruited from an online research registry. Breast Cancer Res Treat. 2014;145(2):525–34.
Van Liew JR, Christensen AJ, de Moor JS. Psychosocial factors in adjuvant hormone therapy for breast cancer: an emerging context for adherence research. Journal of cancer survivorship : research and practice. 2014;8(3):521–31.
Bender CM, Gentry AL, Brufsky AM, Casillo FE, Cohen SM, Dailey MM, Donovan HS, Dunbar-Jacob J, Jankowitz RC, Rosenzweig MQ, et al. Influence of patient and treatment factors on adherence to adjuvant endocrine therapy in breast cancer. Oncol Nurs Forum. 2014;41(3):274–85.
Wouters H, Stiggelbout AM, Bouvy ML, Maatman GA, Van Geffen EC, Vree R, Nortier JW, Van Dijk L. Endocrine therapy for breast cancer: assessing an array of women's treatment experiences and perceptions, their perceived self-efficacy and nonadherence. Clin. breast cancer. 2014;14(6):460–7. e462
Fransen GA, Mesters I, Janssen MJ, Knottnerus JA, Muris JW. Which patient-related factors determine self-perceived patient adherence to prescribed dyspepsia medication? Health Educ Res. 2009;24(5):788–98.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich, Conn). 2008;10(5):348–54.
Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15(1):59–66.
Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64(3):255–7. discussion 258-263
Heinemann K, Ruebig A, Potthoff P, Schneider HP, Strelow F, Heinemann LA, Do MT. The menopause rating scale (MRS) scale: a methodological review. Health Qual Life Outcomes. 2004;2:45.
Cho MJ, Kim KH. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatric Assoc. 1993;32(3):381–99.
Kim Y, Min YH. Menopausal Symptoms and Associated Factors in Breast Cancer Patients Receiving Hormone Therapy. J Korean Clin Nurs Res. 2017;23(1):120–9.
Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients--validation of the short form of the fear of progression questionnaire (FoP-Q-SF). Z Psychosom Med Psychother. 2006;52(3):274–88.
Shim EJ, Lee JW, Min YH. Does depression decrease the moderating effect of self-efficacy in the relationship between illness perception and fear of progression in breast cancer? Psycho-oncology. 2017;27(2):539–47.
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24.
Kim Y, Min YH. Validity and reliability of the Korean version of the beliefs about medicines questionnaire-specific for breast cancer patients on hormone therapy. J Health Info Stat. 2017;42(2):136–43.
General Self-Efficacy Scale (GSE) [http://userpage.fu-berlin.de/~health/selfscal.htm].
Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In J. Weinman, S. Wright, & M. Johnston, measures in health psychology: a user’s portfolio. Causal and control beliefs Windsor. Nfer-Nelson: England; 1995.
Wang Y, Wang X, Liu F, Jiang X, Xiao Y, Dong X, Kong X, Yang X, Tian D, Qu Z. Negative life events and antenatal depression among pregnant women in rural China: the role of negative automatic thoughts. PLoS One. 2016;11(12):e0167597.
Bright EE, Petrie KJ, Partridge AH, Stanton AL. Barriers to and facilitative processes of endocrine therapy adherence among women with breast cancer. Breast Cancer Res Treat. 2016;158(2):243–51.
Sedjo RL, Devine S. Predictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancer. Breast Cancer Res Treat. 2011;125(1):191–200.
Mausbach BT, Schwab RB, Irwin SA. Depression as a predictor of adherence to adjuvant endocrine therapy (AET) in women with breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat. 2015;152(2):239–46.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–7.
Walker HE, Rosenberg SM, Stanton AL, Petrie KJ, Partridge AH. Perceptions, attributions, and emotions toward endocrine therapy in young women with breast cancer. Journal of adolescent and young adult oncology. 2016;5(1):16–23.
Schoenthaler A, Ogedegbe G, Allegrante JP. Self-efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health education & behavior : the official publication of the Society for Public Health Education. 2009;36(1):127–37.
Hilliard ME, Eakin MN, Borrelli B, Green A, Riekert KA. Medication beliefs mediate between depressive symptoms and medication adherence in cystic fibrosis. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2015;34(5):496–504.
McCusker J, Lambert SD, Cole MG, Ciampi A, Strumpf E, Freeman EE, Belzile E. Activation and self-efficacy in a randomized trial of a depression self-care intervention. Health education & behavior : the official publication of the Society for Public Health Education. 2016;43(6):716–25.
Greenlaw SM, Yentzer BA, O'Neill JL, Balkrishnan R, Feldman SR. Assessing adherence to dermatology treatments: a review of self-report and electronic measures. Skin research and technology : official journal of International Society for Bioengineering and the Skin (ISBS) [and] International Society for Digital Imaging of Skin (ISDIS) [and] International Society for Skin Imaging (ISSI). 2010;16(2):253–8.
Kim EY. Development and Application of Direct Data Capture for Monitoring Medication Compliance in Clinical Trials. Healthcare Inf Res. 2017;23(4):249.
Acknowledgements
The authors thank Min Sun Lee, Sae Byul Lee, Sei Hyun Ahn, Byung Ho Son, Jong Won Lee, Hee Jung Kim, and Beom Seok Ko for their assistance in the collection of data for this study.
Funding
This work was supported by a grant from the National Research Foundation (NRF) of Korea funded by the Ministry of Science, ICT and Future Planning (no. 2015R1C1A2A01053155).
Availability of data and materials
The datasets generated and analyzed in the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
YH Min and JY Lee contributed to the conception and design of the study, and the analysis and interpretation of data; YH Min acquired data; JY Lee and YH Min drafted the article and revised it critically for important intellectual content. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at Asan Medical Center, Seoul, Korea (no. 2016–0351). All participants completed written informed consents before the data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, J.Y., Min, Y.H. Relationships between determinants of adjuvant endocrine therapy adherence in breast cancer. BMC Women's Health 18, 48 (2018). https://doi.org/10.1186/s12905-018-0522-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-018-0522-3