Abstract
Background
Withholding or withdrawing life-sustaining treatment in end-of-life patients is a challenging ethical issue faced by physicians. Understanding physicians’ experiences and factors influencing their decisions can lead to improvement in end-of-life care.
Objectives
To investigate the experiences of Thai physicians when making decisions regarding the withholding or withdrawal of life-sustaining treatments in end-of-life situations. Additionally, the study aims to assess the consensus among physicians regarding the factors that influence these decisions and to explore the influence of families or surrogates on the decision-making process of physicians, utilizing case-based surveys.
Methods
A web-based survey was conducted among physicians practicing in Chiang Mai University Hospital (June - October 2022).
Results
Among 251 physicians (response rate 38.3%), most of the respondents (60.6%) reported that they experienced withholding or withdrawal treatment in end-of-life patients. Factors that influence their decision-making include patient’s preferences (100%), prognosis (93.4%), patients’ quality of life (92.8%), treatment burden (89.5%), and families’ request (87.5%). For a chronic disease with comatose condition, the majority of the physicians (47%) chose to continue treatments, including cardiopulmonary resuscitation (CPR). In contrast, only 2 physicians (0.8%) would do everything, in cases when families or surrogates insisted on stopping the treatment. This increased to 78.1% if the families insisted on continuing treatment.
Conclusion
Withholding and withdrawal of life-sustaining treatments are common in Thailand. The key factors influencing their decision-making process included patient’s preferences and medical conditions and families’ requests. Effective communication and early engagement in advanced care planning between physicians, patients, and families empower them to align treatment choices with personal values.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Over the past few decades, the care and support provided to terminally ill patients have been influenced by the incorporation of palliative care [1,2,3,4]. The principle of withholding and withdrawal life-sustaining treatment has been also increasingly integrated into end-of-life care. Life-sustaining treatment was traditionally administered to critically ill patients for the purpose of preserving life such as cardiopulmonary resuscitation (CPR), mechanical ventilator, hemodialysis, and antibiotics. Its utility has been challenged in cases of patients dealing with incurable diseases. Consequently, life-sustaining treatment is often considered futile in these circumstances. As a result, a decision to limit life-sustaining treatment can be made to alleviate the patient’s suffering and enhance the quality of life for both the patient and their family [5,6,7].
Decisions regarding the withholding or withdrawal of life-sustaining treatment require collaboration between the patient and their relatives. Physicians play a crucial role in communicating with patients about prognosis and treatment options [8]. When patients and relatives receive comprehensive information, decisions are made based on the patient’s preferences, leading to an improved quality of life and better outcomes [9, 10]. However, decision-making about treatment limitations remains controversial due to ethical dilemmas and legal issues [11].
While there are guidelines that help in decision-making, including laws that support the right to refuse medical treatment. Limiting life-sustaining treatment remains challenging for physicians. They must consider numerous factors, such as the patient’s autonomy in decision-making, medical standards, and their own beliefs [12, 13]. The personal experiences and perceptions of physicians influence the care they provide [14].
Previous studies have shown that physicians in Asian countries choose to withhold and withdraw life support treatment less than Western medicine [15]. Western countries generally adopt a more permissive and legally accepted approach to withholding and withdrawing life-sustaining treatment. For example, this is the case in the UK, Germany, the Netherlands, and Australia [16]. Legal frameworks and guidelines typically support this view, emphasizing patient autonomy and the importance of advance directives [17]. In contrast, Asian countries have more variability and a lower prevalence of these practices [18]. For instance, Japan and South Korea have complex approaches to withdrawing life-sustaining treatment, shaped by legal precedents and cultural factors [17]. In Japan, despite existing guidelines, there is still legal uncertainty and hesitation among healthcare providers due to past legal cases. In South Korea, landmark cases like Boramae Hospital and Severance Hospital have influenced guidelines but also highlighted the tension between legal requirements and medical practices. Consequently, these countries tend to have more cautious practices, influenced by legal, cultural, and social factors.
In Thailand, The National Health Act, B.E. 2007, allows individuals to create a living will to refuse life-prolonging treatments or alleviate severe suffering in terminal stages. It permits appointing a surrogate decision maker through an advance directive to make decisions for incapacitated patients. Physicians are vital in providing palliative care from diagnosis to end-of-life. The Act emphasizes the importance of informed decision-making by patients, relatives, or proxies about withholding or withdrawing life-sustaining treatment, clarifying that these actions are not considered euthanasia [19]. The primary objective of this study is to investigate the experiences of Thai physicians when making decisions regarding the withholding or withdrawal of life-sustaining treatments in end-of-life care. Additionally, the study aims to examine physicians’ consensus on the factors that influence decision-making. Finally, it seeks to explore the impact of family influence on physicians’ decision-making through a case-based survey.
Methods
Participants
This cross-sectional study was conducted among physicians who worked at Chiang Mai University Hospital during the period spanning June 2022 to October 2022. A web-based questionnaire was employed to collect the data. It was distributed to all physicians at Chiang Mai University Hospital, a tertiary care hospital in northern Thailand, through email addresses obtained from the hospital’s database. All participants provided informed consent before completing the questionnaire.
To estimate the sample size, applying the formula:\(\:n=\frac{N}{(1+{Ne}^{2})\:}\) where n is the sample size, N is the total population size, and e is the margin of error (expressed as a proportion). The total number of physicians actively practicing at Chiang Mai University Hospital amounted to 655 individuals, and a margin of error (e) of 0.05. The calculated sample size was determined to be 248.
Questionnaires
The questionnaire used in this study was developed based on a study published in January 201520. It consisted of three parts as shown in Supplementary file 1. The first part of the questionnaire consisted of respondents’ demographic characteristics. In the second part, we assessed experiences with withholding and withdrawing life-sustaining treatments and physicians’ consensus on the factors influencing decision-making. These factors encompassed patient-related aspects, the care context, communication attitudes with patients and their families or surrogates, as well as perceptions of legal risk exposure. The evaluation employed a Likert scale, where the five response options are categorized into two categories. Specifically, ‘almost always’ and ‘often’ are combined into one category, while ‘sometimes,’ ‘seldom,’ and ‘almost never’ constitute another category. Similarly, ‘strongly agree’ and ‘agree’ are grouped together, while ‘neither agree nor disagree,’ ‘disagree,’ and ‘strongly disagree’ form a separate category.
The third section of the questionnaire aimed to investigate the influence of family members on physicians’ decision-making, utilizing a case-based survey. There were six potential choices related to the decision regarding withholding and/or withdrawing life-sustaining treatment, including full active treatment, including CPR (no withholding or withdrawal of treatment), continuing the most active treatment but excluding CPR (withholding CPR), continuing the current treatment but refraining from administering further complex treatments like hemodialysis or surgery (withholding treatment), continuing the current treatment but abstaining from additional treatments, such as antibiotics for sepsis (withholding treatment), discontinuing all treatments except mechanical ventilation (withdrawal of treatment), discontinuing the mechanical ventilator (withdrawal of treatment) and consulting the ethics committee. We utilized a case scenario translated into Thai version from a previous study [20] with permission from Prof. Dr. Younsuck Koh. Additionally, we conducted both forward and backward translations of the questionnaires. The back-translated version was sent to the original author, Prof. Dr. Younsuck Koh, for final approval.
Data collection
An initial email containing an invitation message, informed consent form, and the link to the web-based questionnaire was sent to all eligible participants. For participants who did not respond within the two-week period, a follow-up email was sent. If the participant did not respond within one month after the second email, they were noted as non-respondents.
Statistical analysis
Statistical analyses were performed using Stata statistical software version 16. Descriptive statistics were employed to summarize the data. Continuous variables were described using mean and standard deviation. Categorical variables were presented as frequency and percentage.
Results
Respondent characteristics
A total of 655 physicians were invited, with 251 completing the full survey, resulting in a response rate of 38.3%. Among all respondents, 51.4% were female. The respondents’ ages varied from 24 to 65 years, with an average age of 34.3 years (SD = 0.6). Their professional backgrounds were diverse including 31.4% in Internal Medicine, 23.1% in Surgery, 12.3% in Family Medicine, and 27.2% in other specialties. The characteristics of the respondents are described in Table 1.
Experiences and physicians’ consensus on the factors that influence decision-making in end-of-life care
Most physicians (60.6%) reported almost always or often withholding or withdrawing treatment for patients with no real chance of recovering a meaningful life. Nonetheless, most of them (54.2%) felt that there was an ethical difference between withholding and withdrawal treatment.
As shown in Table 2, among physicians who have experienced withholding or withdrawing treatment, almost all physicians reported agreement that the patient’s preferences and families’ requests were important factors in withholding or withdrawing treatment (100% and 87.5%, respectively). Despite this, only 48% of physicians felt comfortable talking to the family about limiting life-sustaining treatment. Furthermore, legal risk exposure was another factor taken into consideration in end-of-life care decision-making (26.3%).
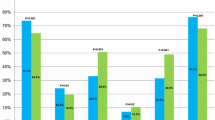
The influence of families or surrogates on end-of-life care practices in different situations
Table 3 describes the management in different situations based on providing care for a 50-year-old male with a chronic disease in a comatose state after cardiac arrest. In the absence of families, surrogates, or advanced directives, the majority of the physicians (47%) chose to continue treatments, including cardiopulmonary resuscitation (CPR) in the event of a cardiac arrest. In contrast, only 2 physicians (0.8%) would do everything, in cases where families or surrogates insisted on stopping the treatment. This increased to 78.1% if the families insisted on continuing treatment. The results of decisions categorized by experience of withholding or withdrawing, job position, or years of practice are shown in Supplementary file 2.
Discussion
In a sample of physicians from various specialties working in a tertiary hospital in Thailand, we found that most of them have encountered situations involving the withholding and withdrawal of life-sustaining treatment. However, their experiences tend to involve withholding treatment more frequently than withdrawing it. Factors that physicians consider essential in determining the limitations of treatment include patient’s preferences and their medical condition. However, most physicians tend to rely on the families’ requests.
Even though palliative care has developed significantly in Thailand [21, 22], similarly in many countries, doctors still tend to choose to withhold more often than withdraw [20, 23]. This might be because doctors perceive that withdrawing is more psychologically difficult [24, 25] and ethically problematic. Furthermore, they believe that there are different ethical considerations between withholding and withdrawing treatment [24, 26]. This is consistent with the evidence in this study that most doctors believed there were different ethics between these two alternative treatments. In addition to the reasons mentioned above, religion [27, 28], law [29], and experience in caring for terminally ill patients also affect the decision-making process of either withholding or withdrawing treatment [30, 31]. The evidence also suggests that specialized education in palliative medicine could play a significant role for physicians in making less aggressive decisions regarding end-of-life care [32, 33].
This study found that patient’s preferences are the most important factor in decision-making which is consistent with various guidelines that focus on patient autonomy [34]. The second important factor is the patient’s condition. If the patient’s condition reaches a point where life-sustaining treatment becomes ineffective or unbeneficial, those treatments may be considered medically futile. Life-sustaining treatments may only prolong the dying process without providing any meaningful benefit [35]. Therefore, it is important for physicians to initiate early communication with patients, particularly those affected by incurable diseases. Physicians should involve patients in discussions about advance care plans, providing them to make well-informed decisions regarding their preferences for the end-of-life period. Furthermore, the ability to evaluate patients at the end of life is essential not only for effective communication but also for providing essential psychological and emotional support. Therefore, this approach ensures that the patient’s autonomy is followed.
Another aspect that respondents considered when making their decisions is families’ requests. This aligns with the practices in many Asian and Western countries where families play an essential role in the decision-making process at the end-of-life stage [20, 36]. However, a previous study shows that the family’s role in end-of-life decision-making in Asian countries (Japan, Korea, and Taiwan), particularly when compared with England, traditionally places a greater emphasis on families and communities rather than on individuals [17]. Families or surrogates often understand the patient’s beliefs and preferences. As a result, they may function as representatives of the patient, ensuring that the patient’s desires are respected when they are unable to make decisions.
The significance of family was also apparent in this study, as an example of a case scenario involving an incurable disease. Most physicians are likely to follow the families’ request if they insisted on discontinuing the treatment. On the other hand, few physicians will continue full life-sustaining treatment. This may be due to the lack of clear guidelines in Thailand on the limitations of treatment or the absence of advanced directives. Moreover, physicians may consider law or ethics issues that make decision-making more complicated [24, 26, 29]. Compared to another Asian survey [20], our respondents were also likely to rely on families’ or surrogates’ requests. In Hong Kong, where guidelines on life-sustaining treatment for the terminally ill are well established [37], there is a tendency for physicians to engage families more frequently in conversations concerning end-of-life matters compared to their European counterparts [38]. In comparison to the American Medical Association (AMA) guidelines [39] of the US on withholding or withdrawing life-sustaining treatment, both Hong Kong and US guidelines emphasize the importance of involving family and surrogate decision-makers in end-of-life decisions while prioritizing the patient’s wishes and decision-making capacity. However, the AMA guidelines emphasize the individual’s right to make decisions about their own health and well-being, strongly stating that physicians should explain that surrogates should make decisions to withhold or withdraw life-sustaining interventions only when the patient lacks decision-making capacity. While Hong Kong’s guidelines allow for more involvement of the family or surrogate in communication and aim to resolve disagreements between the patient’s and family’s decisions, they stipulate that the patient’s decision should not be overridden. In Thailand, the absence of clear guidelines for the inclusion of family members in the decision-making process regarding the withholding and withdrawing of life-sustaining treatment highlights the need for government or relevant authorities to establish and disseminate such guidelines to inform and support clinical practice. Additionally, hospital-level ethics committees may be useful in assisting with decision-making in complex situations.
Patients’ financial problems, the lack of ICU beds, and the financial impact on hospitals, although reported at lower rates, are critical factors in end-of-life care decision-making. These elements introduce significant ethical and practical challenges. Financial concerns among patients can significantly impact how physicians adjust their clinical decisions. It may lead to difficult choices about the intensity of treatments and the use of advance directives [40, 41]. For instance, in settings with limited resources, the high cost of prolonged life-sustaining treatments may give rise to ethical issues that influence the continuation or withdrawal of care. In addition, decisions influenced by the financial impact on the hospital can be controversial, as they may conflict with the primary objective of patient-centered care. This highlights the need for policies ensuring that all patients receive proper care regardless of their financial condition. It raises questions about equity and access to healthcare, as well as the importance of having robust guidelines and ethical frameworks to support physicians in making these challenging decisions.
Furthermore, it is interesting that while 57% of physicians have experienced withholding or withdrawing treatment, only 48% feel comfortable discussing it with families. This discrepancy suggests that while physicians may frequently encounter these situations, they often struggle with the communication aspect. This discomfort can be attributed to several factors, including fear of causing distress to families and personal ethical dilemmas [42]. Therefore, improving education about palliative care for doctors is crucial [43]. It is necessary to provide knowledge about communication skills, ethical decision-making, and importantly, understanding the concepts of withholding and withdrawing treatments. This can assist physicians in navigating these challenging conversations more comfortably.
In situations where the patient lacks decision-making capacity and has no available relatives or advance directive. Physicians may consult with ethics committees to ensure they are following regulations and ethical guidelines. These consultations can provide guidance on decision-making processes. Therefore, the development of guidelines is important to assist physicians in handling difficult situations.
There are several limitations to this study. Firstly, it was conducted in a single setting in Thailand, so the findings may not be applicable to other settings. Secondly, the study design is cross-sectional, which can introduce recall bias when respondents are asked about past events. However, this bias is expected to be rare and may only affect decision-making discomfort. Respondents who have experienced the events should be able to recall them accurately. Thirdly, there might be unrecorded details or factors beyond the reported information when considering different scenarios. Conducting more comprehensive and in-depth studies on decision-making issues would be beneficial.
On the other hand, the strength of this study lies in addressing an important and sensitive topic in medical practice, specifically the lack of clear guidelines in Thailand for making decisions about limiting life-sustaining treatments. The information gathered from this study can be used to develop plans and assist physicians in making informed decisions regarding the withdrawal and withholding of life-sustaining treatments in the future.
Conclusion
Most physicians have experienced the withholding and withdrawal of life-sustaining treatment. From a Western bioethical perspective, there is no ethical difference between withholding and withdrawing life-sustaining treatments. However, physicians usually perceive these actions differently. Withdrawing treatment feels more like taking action, which can be harder emotionally, leading to a distinction in practice [16]. When considering the limitations of life-sustaining treatments in patients who were incapacitated and unable to make decisions, the first factor considered in the treatment choice was the patients’ preferences, followed by the requests of their relatives. There are some challenging situations, especially when resources are limited, and financial concerns arise. To support physicians in making these important decisions, there is a need for clear clinical practice guidelines and ethics, enhanced professional education, and improved communication skills.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author (Lalita Chutarattanakul, MD.) on reasonable request.
References
Hughes MT, Smith TJ. The growth of palliative care in the United States. Annu Rev Public Health. 2014;35:459–75. https://doi.org/10.1146/annurev-publhealth-032013-182406.
Yamaguchi T, Kuriya M, Morita T, et al. Palliative care development in the Asia-Pacific region: an international survey from the Asia Pacific Hospice Palliative Care Network (APHN). BMJ Support Palliat Care Mar. 2017;7(1):23–31. https://doi.org/10.1136/bmjspcare-2013-000588.
Rhee JY, Garralda E, Torrado C, Blanco, S, Ayala I, Namisango E, et al. Palliative care in Africa: a scoping review from 2005–16. Lancet Oncol. 2017;18(9):e522-e531. https://doi.org/10.1016/S1470-2045(17)30420-5.
Clark D, Baur N, Clelland D, et al. Mapping levels of Palliative Care Development in 198 countries: the Situation in 2017. J Pain Symptom Manage Apr. 2020;59(4):794–e8074. https://doi.org/10.1016/j.jpainsymman.2019.11.009.
Kavalieratos D, Corbelli J, Zhang D, et al. Association between Palliative Care and Patient and Caregiver outcomes: a systematic review and Meta-analysis. Jama Nov. 2016;22(20):2104–14. https://doi.org/10.1001/jama.2016.16840.
Higginson IJ, Evans CJ. What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J Sep-Oct. 2010;16(5):423–35. https://doi.org/10.1097/PPO.0b013e3181f684e5.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med Aug. 2010;19(8):733–42. https://doi.org/10.1056/NEJMoa1000678.
Curtis JR, Vincent J-L. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376(9749):1347–53. https://doi.org/10.1016/S0140-6736(10)60143-2.
Garrido MM, Prigerson HG. The end-of-life experience: modifiable predictors of caregivers’ bereavement adjustment. Cancer Mar. 2014;15(6):918–25. https://doi.org/10.1002/cncr.28495.
Greer JA, Applebaum AJ, Jacobsen JC, Temel JS, Jackson VA. Understanding and addressing the role of coping in Palliative Care for patients with Advanced Cancer. J Clin Oncol Mar. 2020;20(9):915–25. https://doi.org/10.1200/jco.19.00013.
McQuoid-Mason DJ. Should doctors provide futile medical treatment if patients or their proxies are prepared to pay for it? S Afr Med J Jan. 2017;30(2):108–9. https://doi.org/10.7196/SAMJ.2017.v107i2.12191.
WMA - The World Medical Association WM. WMA declaration on end-of-life medical care. 2022. https://www.wma.net/policies-post/wma-declaration-on-end-of-life-medical-care/
Bosslet GT, Pope TM, Rubenfeld GD, et al. An official ATS/AACN/ACCP/ESICM/SCCM Policy Statement: responding to requests for potentially inappropriate treatments in Intensive Care Units. Am J Respir Crit Care Med. 2015;191(11):1318–30. https://doi.org/10.1164/rccm.201505-0924ST.
Keating NL, Landrum MB, Rogers SO Jr., et al. Physician factors associated with discussions about end-of-life care. Cancer Feb. 2010;15(4):998–1006. https://doi.org/10.1002/cncr.24761.
Koh M, Hwee PC. End-of-Life Care in the Intensive Care Unit: how Asia differs from the West. JAMA Intern Med. 2015;175(3):371–2. https://doi.org/10.1001/jamainternmed.2014.7397.
Ko D, Evans-Barns H, Blinderman C. Withholding and withdrawing life-sustaining treatment (including artificial nutrition and hydration). In: Cherny NI, Fallon MT, Kaasa S, et al. editors. Oxford Textbook of Palliative Medicine. Oxford University Press; 2021. p. 0.
Tanaka M, Kodama S, Lee I, Huxtable R, Chung Y. Forgoing life-sustaining treatment – a comparative analysis of regulations in Japan, Korea, Taiwan, and England. BMC Med Ethics. 2020;2020/10/16(1):99. https://doi.org/10.1186/s12910-020-00535-w.
Mark NM, Rayner SG, Lee NJ, Curtis JR. Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med. Sep 2015;41(9):1572–85. https://doi.org/10.1007/s00134-015-3810-5.
Notification of the National Health Commission On the Operational Definitions of Terms Pertaining to Palliative Care for Thailand, B.E. 2563. (A.D. 2020) (NHCO Thailand) (2021).
Phua J, Joynt GM, Nishimura M, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. Mar 2015;175(3):363–71. https://doi.org/10.1001/jamainternmed.2014.7386.
Worldwide palliative care alliance WHO. Global Atlas of Palliative Care. 2nd ed. 2020.
Nilmanat K. Palliative care in Thailand: development and challenges. Can Oncol Nurs J Summer. 2016;26(3):262–4.
Vincent JL. Forgoing life support in western European intensive care units: the results of an ethical questionnaire. Crit Care Med Aug. 1999;27(8):1626–33. https://doi.org/10.1097/00003246-199908000-00042.
Chung GS, Yoon JD, Rasinski KA, Curlin FA. US Physicians’ opinions about distinctions between withdrawing and withholding life-sustaining treatment. J Relig Health Oct. 2016;55(5):1596–606. https://doi.org/10.1007/s10943-015-0171-x.
Aita K, Kai I. Physicians’ psychosocial barriers to different modes of withdrawal of life support in critical care: a qualitative study in Japan. Soc Sci Med Feb. 2010;70(4):616–22. https://doi.org/10.1016/j.socscimed.2009.10.036.
Dickenson DL. Are medical ethicists out of touch? Practitioner attitudes in the US and UK towards decisions at the end of life. J Med Ethics Aug. 2000;26(4):254–60. https://doi.org/10.1136/jme.26.4.254.
Duivenbode R, Hall S, Padela AI. Assessing relationships between Muslim Physicians’ religiosity and end-of-Life Health-Care attitudes and Treatment recommendations: an exploratory National Survey. Am J Hosp Palliat Care Sep. 2019;36(9):780–8. https://doi.org/10.1177/1049909119833335.
Wenger NS, Carmel S. Physicians’ religiosity and end-of-life care attitudes and behaviors. Mt Sinai J Med. Oct 2004;71(5):335–43.
Kim DJ, Choi MS. Life-sustaining treatment and palliative care in patients with liver cirrhosis - legal, ethical, and practical issues. Clin Mol Hepatol Jun. 2017;23(2):115–22. https://doi.org/10.3350/cmh.2017.0018.
Alminoja A, Piili RP, Hinkka H, et al. Does decision-making in end-of-life Care Differ between Graduating Medical students and experienced Physicians? In vivo. 2019;33(3):903–9. https://doi.org/10.21873/invivo.11557.
Hinkka H, Kosunen E, Metsänoja R, Lammi UK, Kellokumpu-Lehtinen P. Factors affecting physicians’ decisions to forgo life-sustaining treatments in terminal care. J Med Ethics. 2002;28(2):109–14. https://doi.org/10.1136/jme.28.2.109.
Piili RP, Lehto JT, Luukkaala T, Hinkka H, Kellokumpu-Lehtinen P-LI. Does special education in palliative medicine make a difference in end-of-life decision-making? BMC Palliat Care. 2018;2018/07/18(1):94. https://doi.org/10.1186/s12904-018-0349-6.
Forte DN, Vincent JL, Velasco IT, Park M. Association between education in EOL care and variability in EOL practice: a survey of ICU physicians. Intensive Care Med Mar. 2012;38(3):404–12. https://doi.org/10.1007/s00134-011-2400-4.
Bandrauk N, Downar J, Paunovic B, On Behalf of the Canadian Critical Care Society Ethics C. Withholding and withdrawing life-sustaining treatment: the Canadian Critical Care Society position paper. Can J Anesthesia/Journal Canadien d’anesthésie 2018/01/01. 2018;65(1):105–22. https://doi.org/10.1007/s12630-017-1002-1.
Torke AM, Moloney R, Siegler M, Abalos A, Alexander GC. Physicians’ views on the importance of patient preferences in surrogate decision-making. J Am Geriatr Soc. Mar 2010;58(3):533–8. https://doi.org/10.1111/j.1532-5415.2010.02720.x.
Bakke BM, Feuz MA, McMahan RD, Barnes DE, Li B, Volow AM, et al. Surrogate decision makers need better preparation for their role: advice from experienced surrogates. J Palliat Med. 2022/06/01 2022;25(6):857–863. https://doi.org/10.1089/jpm.2021.0283.
Patient Safety & Risk Management Department / Quality & Safety Division Hospital Authorit Guidelines on Life-Sustaining Treatment in the Terminally Ill. 2020. https://www.ha.org.hk/haho/ho/psrm/LSTEng.pdf
Yap HY, Joynt GM, Gomersall CD. Ethical attitudes of intensive care physicians in Hong Kong: questionnaire survey. Hong Kong Med J Aug. 2004;10(4):244–50.
Withholding or Withdrawing Life-Sustaining Treatment. AMA Code of Medical Ethics. May 25, 2024. https://code-medical-ethics.ama-assn.org/ethics-opinions/withholding-or-withdrawing-life-sustaining-treatment.
Luna-Meza A, Godoy-Casasbuenas N, Calvache JA, Díaz-Amado E, Gempeler Rueda FE, Morales O, et al. Decision making in the end-of-life care of patients who are terminally ill with cancer – a qualitative descriptive study with a phenomenological approach from the experience of healthcare workers. BMC Palliat Care. 2021;20(1):76. https://doi.org/10.1186/s12904-021-00768-5.
Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA Oct. 2011;5(13):1447–53. https://doi.org/10.1001/jama.2011.1410.
Horn R. I don’t need my patients’ opinion to withdraw treatment: patient preferences at the end-of-life and physician attitudes towards advance directives in England and France. Med Health Care Philos Aug. 2014;17(3):425–35. https://doi.org/10.1007/s11019-014-9558-9.
Guidet B, Vallet H, Flaatten H, et al. The trajectory of very old critically ill patients. Intensive Care Med Feb. 2024;50(2):181–94. https://doi.org/10.1007/s00134-023-07298-z.
Acknowledgements
Sincere acknowledgment is expressed by the authors to all study participants.
Funding
This work was partially supported by Chiang Mai University.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: conceptualization: NK, KP, CA, LC; data collection: NK, LC; data analysis: NK, CA, KP, ND, LC; draft manuscript: NK, KP, LC. All authors reviewed the results, and revise and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of the Faculty of Medicine, Chiang Mai University (FAM-2565-09004). All participants provided informed consent to the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ketchaikosol, N., Pinyopornpanish, K., Angkurawaranon, C. et al. Physicians’ experiences and perceptions about withholding and withdrawal life-sustaining treatment in Chiang Mai University Hospital: a cross-sectional study. BMC Palliat Care 23, 206 (2024). https://doi.org/10.1186/s12904-024-01511-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-024-01511-6