Abstract
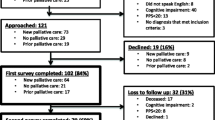
Decisions to withhold or withdraw life-sustaining treatment (LST) precede the majority of ICU deaths. Although professional guidelines generally treat the two as ethically equivalent, evidence suggests withdrawing LST is often more psychologically difficult than withholding it. The aim of the experiment was to investigate whether physicians are more supportive of withholding LST than withdrawing it and to assess how physicians’ opinions are shaped by their religious characteristics, specialty, and experience caring for dying patients. In 2010, a survey was mailed to 2016 practicing US physicians. Physicians were asked whether physicians should always comply with a competent patient’s request to withdraw LST, whether withdrawing LST is more psychologically difficult than withholding it, and whether withdrawing LST is typically more ethically problematic than withholding it. Of 1880 eligible physicians, 1156 responded to the survey (62%); 93% agreed that physicians should always comply with a competent patient’s request to withdraw LST. More than half of the physicians reported that they find withdrawing LST more psychologically difficult than withholding it (61%), and that withdrawing LST is typically more ethically problematic (59%). Physician religiosity was associated with finding withdrawal more ethically problematic, but not with finding it more psychologically difficult. Physicians working in an end-of-life specialty and physicians with more experience caring for dying patients were less likely to endorse either a psychological or an ethical distinction between withdrawing and withholding LST. Most US physicians find withdrawing LST not only more psychologically difficult, but also more ethically problematic than withholding such treatment. Physicians’ opinions are to some extent shaped by their religious characteristics, specialty, and levels of experience caring for dying patients.

Similar content being viewed by others
References
A report of the Hastings Center. (1987). Guidelines on the termination of life-sustaining treatment and the care of the dying. Briarcliff Manor, NY: The Hastings Center.
Aita, K., & Kai, I. (2010). Physicians’ psychosocial barriers to different modes of withdrawal of life support in critical care: A qualitative study in Japan. Social Science and Medicine, 70(4), 616–622.
American Medical Association. E-2.037. Medical futility in end-of-life care. www.ama-assn.org/ama/pub/category/8390.html.
American Medical Association. H-140.966. Decisions near the end of life. http://www.ama-assn.org/apps/pf_new/pf_online?f_n=browse&doc=policyfiles/HnE/H-140.966.HTM. Accessed February 17, 2005.
American Thoracic Society. (1991). Withholding and withdrawing life-sustaining therapy. American Review of Respiratory Disease, 144(3 Pt 1), 726–731.
Attitudes of critical care medicine professionals concerning forgoing life-sustaining treatments. The Society of Critical Care Medicine Ethics Committee. Critical Care Medicine, 20(3), 320–326 (1992).
Balint, J. A. (2000). Decisions at the end of life. Croatian Medical Journal, 41(2), 144–149.
Beauchamp, T. L., & Childress, J. F. (2001). Principles of biomedical ethics (5th ed.). New York: Oxford University Press.
Beck, S., van de Loo, A., & Reiter-Theil, S. (2008). A “little bit illegal”? Withholding and withdrawing of mechanical ventilation in the eyes of German intensive care physicians. Medicine, Health Care and Philosophy, 11(1), 7–16.
Boneh, A., Allan, S., Mendelson, D., et al. (2008). Minireview: Clinical, ethical and legal considerations in the treatment of newborns with non-ketotic hyperglycinaemia. Molecular Genetics and Metabolism, 94(2), 143–147.
Curlin, F. A., Nwodim, C., Vance, J. L., Chin, M. H., & Lantos, J. D. (2008). To die, to sleep: US physicians’ religious and other objections to physician-assisted suicide, terminal sedation, and withdrawal of life support. The American Journal of Hospice & Palliative Care, 25(2), 112–120.
Donohue, P. K., Boss, R. D., Aucott, S. W., et al. (2010). The impact of neonatologists’ religiosity and spirituality on health care delivery for high-risk neonates. Journal of Palliative Medicine, 13(10), 1219–1224.
Dyer, C. (2004). GMC faces challenge over withdrawing treatment. BMJ, 328(7431), 68.
Eidelman, L. A., Jakobson, D. J., Pizov, R., Geber, D., Leibovitz, L., & Sprung, C. L. (1998). Forgoing life-sustaining treatment in an Israeli ICU. Intensive Care Medicine, 24(2), 162–166.
Ellison, C., Gay, D., & Glass, T. (1989). Does religious commitment contribute to individual life satisfaction? Social Forces, 68, 100–123.
Executive Board, American Academy of Neurology. Position of the American Academy of Neurology on certain aspects of the care and management of the persistent vegetative state patient. Neurology, 39(1), 25–26 (1989).
Farber, N. J., Simpson, P., Salam, T., et al. (2006). Physicians’ decisions to withhold and withdraw life-sustaining treatment. Archives of Internal Medicine, 166(5), 560–564.
Fetzer Institute/National Institute on Aging Working Group. (1999). Multidimensional measurement of religiousness/spirituality for use in health research. Kalamazoo, MI: Fetzer Institute.
Fried, T. R., Stein, M. D., O’Sullivan, P. S., et al. (1993). Limits of patient autonomy: Physician attitudes and practices regarding life-sustaining treatments and euthanasia. Archives of Internal Medicine, 153(6), 722–728.
Groves, R. M., Fowler, F. J., Couper, M. P., et al. (2004). Survey methodology. Hoboken, NJ: Wiley.
Lauderdale, D. S. (2006). Birth outcomes for Arabic-named women in California before and after September 11. Demography, 43(1), 185–201.
Lauderdale, D. S., & Kestenbaum, B. (2000). Asian American ethnic identification by surname. Population Research and Policy Review, 19, 283–300.
Levin, P. D., & Sprung, C. L. (2005). Withdrawing and withholding life-sustaining therapies are not the same. Critical Care, 9(3), 230–232.
Luce, J. M., & White, D. B. (2009). A history of ethics and law in the intensive care unit. Critical Care Clinics, 25(1), 221–237.
Melltorp, G., & Nilstun, T. (1997). The difference between withholding and withdrawing life-sustaining treatment. Intensive Care Medicine, 23(12), 1264–1267.
Miller, F. G., Truog, R. D., & Brock, D. W. (2010). Moral fictions and medical ethics. Bioethics, 24(9), 453–460.
Nolin, T., & Andersson, R. (2003). Withdrawal of medical treatment in the ICU: A cohort study of 318 cases during 1994–2000. Acta Anaesthesiologica Scandinavica, 47(5), 501–507.
Olsen, M. L., Swetz, K. M., & Mueller, P. S. (2010). Ethical decision making with end-of-life care: Palliative sedation and withholding or withdrawing life-sustaining treatments. Mayo Clinic Proceedings, 85(10), 949–954.
Pawlik, T. M. (2006). Withholding and withdrawing life-sustaining treatment: A surgeon’s perspective. Journal of the American College of Surgeons, 202(6), 990–994.
Pellegrino, E. D. (2000). Decisions to withdraw life-sustaining treatment: A moral algorithm. JAMA, 283(8), 1065–1067.
President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to forego life-sustaining treatment: Ethical, medical and legal issues in treatment decisions. Washington, DC: U.S. Government Printing Office, 1983.
Putman, M. S., Yoon, J. D., Rasinski, K. A., & Curlin, F. A. (2013). Intentional sedation to unconsciousness at the end of life: Findings from a national physician survey. Journal of Pain and Symptom Management, 46(3), 326–334.
Rubenfeld, G. D. (2004). Principles and practice of withdrawing life-sustaining treatments. Critical Care Clinics, 20(3), 435–451.
Shanawani, H., Wenrich, M. D., Tonelli, M. R., & Curtis, J. R. (2008). Meeting physicians’ responsibilities in providing end-of-life care. Chest, 133(3), 775–786.
Sheskin, I. M. (1998). A methodology for examining the changing size and spatial distribution of a Jewish population: A Miami case study. Shofar, 17, 97–114.
Solomon, M. Z., O’Donnell, L., Jennings, B., et al. (1993). Decisions near the end of life: Professional views on life-sustaining treatments. American Journal of Public Health, 83(1), 14–23.
Street, K., & Henderson, J. (2001). Ethical debate: The distinction between withdrawing life sustaining treatment under the influence of paralysing agents and euthanasia. BMJ, 323(7309), 388–389.
Sulmasy, D. P., & Sugarman, J. (1994). Are withholding and withdrawing therapy always morally equivalent? Journal of Medical Ethics, 20(4), 218–222.
Vincent, J. L. (1999). Forgoing life support in western European intensive care units: The results of an ethical questionnaire. Critical Care Medicine, 27(8), 1626–1633.
Vincent, J. (2005). Commentary: Withdrawing may be preferable to withholding. Critical Care, 9(3), 226–229.
Wenger, N. S., & Carmel, S. (2004). Physicians’ religiosity and end-of-life care attitudes and behaviors. Mount Sinai Journal of Medicine, 71(5), 335–343.
Wilkinson, D., & Savulescu, J. (2014). A costly separation between withdrawing and withholding treatment in intensive care. Bioethics, 28(3), 127–137.
Withholding and Withdrawing Life-Prolonging Medical Treatment. Guidance for Decision-Making. British Medical Association. Blackwell Publishing – Third Edition. January 16, 2007.
Wolenberg, K. M., Yoon, J. D., Rasinski, K. A., & Curlin, F. A. (2013). Religion and United States physicians’ opinions and self-predicted practices concerning artificial nutrition and hydration. Journal of Religion and Health, 52(4), 1051–1065.
Wood, G. G., & Martin, E. (1995). Withholding and withdrawing life-sustaining therapy in a Canadian intensive care unit. Canadian Journal of Anaesthesia, 42(3), 186–191.
Yazigi, A., Riachi, M., & Dabbar, G. (2005). Withholding and withdrawal of life-sustaining treatment in a Lebanese intensive care unit: A prospective observational study. Intensive Care Medicine, 31(4), 562–567.
Acknowledgments
This study was funded by grant support from The John Templeton Foundation. The study sponsor had no involvement in the design of the study; the collection, analysis, and interpretation of the data; the writing of the report; or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose. Grace S. Chung declares that she has no conflicts of interest. John D. Yoon declares that he has no conflicts of interest. Kenneth A. Rasinski declares that he has no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chung, G.S., Yoon, J.D., Rasinski, K.A. et al. US Physicians’ Opinions about Distinctions between Withdrawing and Withholding Life-Sustaining Treatment. J Relig Health 55, 1596–1606 (2016). https://doi.org/10.1007/s10943-015-0171-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-015-0171-x