Abstract
Objective
This prospective study evaluated the clinical performance of large class II restorations made with different techniques over 24 months.
Materials and methods
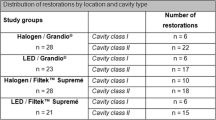
Thirty patients received two class II restorations (n = 60) using a nanohybrid composite and different restorative techniques (direct (DT), semidirect (SDT)), in a split-mouth randomized design. The same adhesive system was applied for all restorations. For DT, the restorative material was applied directly inside the tooth preparation. For SDT, a tooth preparation impression was obtained using alginate and a silicone flexible die was prepared. The restoration was made chairside on the model and additionally light cured. After that, it was cemented in preparation using resinous cement. All restorations were evaluated using the FDI criteria after 7 days, 6, 12, and 24 months postoperatively.
Results
After 24 months, 24 patients attended the recall and 48 restorations were evaluated. Fisher’s statistical analysis (5%) showed no difference between the techniques. Nevertheless, Friedman’s test showed significant differences for some criteria after 12 months of evaluation for both techniques. Postoperative sensitivity was reported in one DT restoration. Also, after 24 months, one SDT restoration presented marginal fracture, which was deemed unsatisfactory.
Conclusions
After a 24-month follow-up, no significant difference between the tested techniques was detected. The restorations performed with both techniques produced clinically acceptable restorations.
Clinical relevance
This study demonstrated the viability of applying two different operatory techniques (direct and semidirect) for class II resin composite restorations.

Similar content being viewed by others
References
Villarroel M, Fahl N, De Sousa AM, De Oliveira OB (2011) Direct esthetic restorations based on translucency and opacity of composite resins. J Esthet Restor Dent 23:73–87. https://doi.org/10.1111/j.1708-8240.2010.00392.x
Sunnegårdh-Grönberg K, van Dijken JW, Funegård U, Lindberg A, NilssonM (2009) Selection of dental materials and longevity of replaced restorations in public dental health clinics in northern Sweden. J Dent 37:673–678. https://doi.org/10.1016/j.jdent.2009.04.010
Torres CRG, Rêgo HM, Perote LC, Santos LF, Kamozaki MB, Gutierrez NC, Di Nicoló R, Borges AB (2014) A split-mouth randomized clinical trial of conventional and heavy flowable composites in class II restorations. J Dent 42:793–799. https://doi.org/10.1016/j.jdent.2014.04.009
Magne P, Dietschi D, Holz J (1996) Esthetic restoration for posterior teeth: practical and clinical considerations. Int J Periodont Rest Dent 16:105–119
Dietschi D, Spreafico R (1997) Adhesive metal-free restorations: current concepts for the esthethic treatment of posterior teeth. Quintenssence Publishing Co, Germany
Ozakar-Ilday N, Zorba YO, Yildiz M, Erdem V, Seven N, Demirbuga S (2013) Three-year clinical performance of two indirect composite inlays compared to direct composite restorations. Med Oral Patol Oral Cir Bucal 18(3):e521–e528
Siéssere S, Vitti M, de Sousa LG, Semprini M, Regalo SCH (2004) Educational material of dental anatomy applied to study the morphology of permanent teeth. Braz Dent J 15(3):238–242
Alharbi A, Rocca GT, Dietschi D, Krejci I (2014) Semidirect composite onlay with cavity sealing: a review of clinical procedures. J Esthet Restor Dent 26(2):97–106. https://doi.org/10.1111/jerd.12067
Gerrow JD, Price RB (1998) Comparison of the surface detail reproduction of flexible die material systems. J Prosthet Dent 80(4):485–489
Antonelli JR, Gulker I (2000) A modified indirect working die technique for fabricating provisional restorations for multiple teeth. Quintessence Int 31(6):392–396
Yoshikawa T, Burrow MF, Tagami J (2001) A light curing method for improving marginal sealing and cavity wall adaptation of resin composite restorations. Dent Mater 17(4):359–366
Torres CRG, Zanatta RF, Huhtala MFR, Borges AB (2017) Semidirect posterior composite restorations with a flexible die technique. J Am Dent Assoc 148(9):671–676. https://doi.org/10.1016/j.adaj.2017.02.032
Dimashkieh MR, Rayyan MR (2016) Chairside technique for expediting indirect interim restorations. J Prosthet Dent 115(4):510–511. https://doi.org/10.1016/j.prosdent.2015.09.025
Setembrini L, Gultz G, Scherer W, Kaim J (1998) A 30-minute in-office indirect composite inlay technique. J Am Dent Assoc 129(3):366–367
Angeletaki F, Gkogkos A, Papazoglou E, Kloukos D (2016) Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J Dent 53:12–21. https://doi.org/10.1016/j.jdent.2016.07.011
Llena Puy MC, Navarro LF, Faus Llacer VJ, Ferrandez A (1993) Composite resin inlays: a study of marginal adaptation. Quintessence Int 24(6):429–433
Donly KJ (1990) Composite resin inlays: a single appointment technique. Am J Dent 3(5):181–184
Price RB, Gerrow JD (2000) Margin adaptation of indirect composite inlays fabricated on flexible dies. J Prosthet Dent 83(3):306–313
Heintze SD (2007) Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent 9(Supp1):77–106
Peutzfeldt A, Asmussen E (2000) The effect of postcuring on quantity of remaining double bonds, mechanical properties, and in vitro wear of two resin composites. J Dent 28(6):447–452
Prabhu K, Subashini BC, Venkatakrishnan B, Ramesh AS (2018) Comparison of dimensional stability of die stone and die silicone: an in vitro comparative study. J Interdiscip Dentistry 8:92–95. https://doi.org/. https://doi.org/10.4103/jid.jid_95_17
El-Safty S, Akhtar R, Silikas N, Watts DC (2012) Nanomechanical properties of dental resin-composites. Dent Mater 28(12):1292–1300. https://doi.org/. https://doi.org/10.1016/j.dental.2012.09.007
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 152(11):726–732. https://doi.org/10.7326/0003-4819-152-11-201006010-00232
Hickel R, Peschke A, Tyas M, Mjör I, Bayne S, Peters M, Hiller KA, Randall R, Vanherle G, Heintze SD (2010) FDI world dental federation: clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin Oral Investig 14(4):349–366. https://doi.org/10.1007/s00784-010-0432-8
Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G (2007) Recommendations for conducting controlled clinical studies of dental restorative materials. Science Committee Project 2/98--FDI World Dental Federation study design (part I) and criteria for evaluation (part II) of direct and indirect restorations including onlays and partial crowns. J Adhes Dent 9(Suppl1):121–147
Mahmoud SH, El-Embaby AE, AbdAllah AM, Hamama HH (2008) Two-year clinical evaluation of ormocer, nanohybrid and nanofill composite restorative systems in posterior teeth. J Adhes Dent 10(4):315–322
Zhu H, Zhang S, Ahn C (2017) Sample size considerations for split-mouth design. Stat Methods Med Res 26(6):2543–2551. https://doi.org/10.1177/0962280215601137
Loguercio AD, de Paula EA, Hass V, Luque-Martinez I, Reis A, Perdigão J (2015) A new universal simplified adhesive: 36-month randomized double-blind clinical trial. J Dent 43(9):1083–1092. https://doi.org/10.1016/j.jdent.2015.07.005
Coelho-de-Souza FH, Gonçalves DS, Sales MP, Erhardt MC, Corrêa MB, Opdam NJ, Demarco FF (2015) Direct anterior composite veneers in vital and non-vital teeth: a retrospective clinical evaluation. J Dent 43(11):1330–1336. https://doi.org/10.1016/j.jdent.2015.08.011
Mena-Serrano A, Kose C, De Paula EA, Tay LY, Reis A, Loguercio AD, Perdigão J (2013) A new universal simplified adhesive: 6-month clinical evaluation. J Esthet Restor Dent 25(1):55–69. https://doi.org/10.1111/jerd.12005
Perdigão J, Kose C, Mena-Serrano AP, De Paula EA, Tay LY, Reis A, Loguercio AD (2014) A new universal simplified adhesive: 18-month clinical evaluation. Oper Dent 39(2):113–127. https://doi.org/10.2341/13-045-C
Ástvaldsdóttir Á, Dagerhamn J, van Dijken JW, Naimi-Akbar A, Sandborgh-Englund G, Tranæus S, Nilsson M (2015) Longevity of posterior resin composite restorations in adults – a systematic review. J Dent 43(8):934–954. https://doi.org/10.1016/j.jdent.2015.05.001
Brouwer F, Askar H, Paris S, Schwendicke F (2016) Detecting secondary caries lesions: a systematic review and meta-analysis. J Dent Res 95(2):143–151. https://doi.org/10.1177/0022034515611041
Nedeljkovic I, Teughels W, De Munck J, Van Meerbeek B, Van Landuyt KL (2015) Is secondary caries with composites a material-based problem? Dent Mater 31(11):e247–e277. https://doi.org/10.1016/j.dental.2015.09.001
da Veiga AM, Cunha AC, Ferreira DM, da Silva Fidalgo TK, Chianca TK, Reis KR, Maia LC (2016) Longevity of direct and indirect resin composite restorations in permanent posterior teeth: a systematic review and meta-analysis. J Dent 54:1–12. https://doi.org/. https://doi.org/10.1016/j.jdent.2016.08.003
Nadine S (2010) Indirect resin composites. J Conserv Dent 13(4):184–194
Spreafico RC, Krejci I, Dietschi D (2005) Clinical performance and marginal adaptation of class II direct and semidirect composite restorations over 3.5 years in vivo. J Dent 33(6):499–507. https://doi.org/10.1016/j.jdent.2004.11.009
Briso AL, Mestrener SR, Delício G, Sundfeld RH, Bedran-Russo AK, de Alexandre RS, Ambrosano GM (2007) Clinical assessment of postoperative sensitivity in posterior composite restorations. Oper Dent 32(5):421–426. https://doi.org/10.2341/06-141
van Dijken JW, Lindberg A (2009) Clinical effectiveness of a low-shrinkage resin composite: a five-year evaluation. J Adhes Dent 11(2):143–148
van Dijken JW (2013) A 6-year prospective evaluation of a one-step HEMA-free self-etching adhesive in class II restorations. Dent Mater 29(11):1116–1122. https://doi.org/10.1016/j.dental.2013.08.205
Cetin AR, Unlu N, Cobanoglu N (2013) A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent 38(2):E31–E41. https://doi.org/10.2341/12-160-C
van Dijken JW, Sunnegårdh-Grönberg K (2005) A four-year clinical evaluation of a highly filled hybrid resin composite in posterior cavities. J Adhes Dent 7(4):343–349
Burke FJ, Watts DC, Wilson NH, Wilson MA (1991) Current status and rationale for composite inlays and onlays. Br Dent J 170(7):269–273
Ramos NC, Luz JN, Valera MC, Melo RM, Saavedra G, Bresciani E (2019) Color stability of resin cements exposed to aging. Oper Dent [Epub ahead of print]. https://doi.org/10.2341/18-064-L
Lu H, Powers JM (2004) Color stability of resin cements after accelerated aging. Am J Dent 17(5):354–358
Mendonça JS, Neto RG, Santiago SL, Lauris JRP, Navarro MF, de Carvalho RM (2010) Direct resin composite restorations versus indirect composite inlays: one-year results. J Contemp Dent Pract 11(3):25–32
Petrovic LM, Drobac MR, Stojanac IL, Atanackovic TM (2010) A method of improving marginal adaptation by elimination of singular stress point in composite restorations during resin photo-polymerization. Dent Mater 26(5):449–455. https://doi.org/10.1016/j.dental.2009.11.160
Türkumen C, Durkan M, Cimilli H, Öksüz M (2010) Tensile bond strength of indirect composites luted with three new self-adhesive resin cements to dentin. J Appl Oral Sci 19(4):363–369
Yamamoto T, Nakamura Y, Nishide A, Kubota Y, Momoi Y (2013) Contraction stresses in direct and indirect composite restorations compared by crack analysis. J Adhes Dent 15(1):47–54. https://doi.org/10.3290/j.jad.a28171
Heintze SD, Reichl FX, Hickel R (2019) Wear of dental materials: clinical significance and laboratory wear simulation methods -a review. Dent Mater J 26:1–11. https://doi.org/10.4012/dmj.2018-140
American Dental Association (2001) Council on Scientific Affairs American Dental Association program guidelines: products for dentin and enamel adhesive materials. (www.ada.org)
Lazaridou D, Belli R, Petschelt A, Lohbauer U (2015) Are resin composites suitable replacements for amalgam? A study of two-body wear. Clin Oral Investig 19(6):1485–1492. https://doi.org/10.1007/s00784-014-1373-4
Karaman E, Yazici AR, Ozgunaltay G, Dayangac B (2012) Clinical evaluation of a nanohybrid and a flowable resin composite in non-carious cervical lesions: 24-month results. J Adhes Dent 14(5):485–492. https://doi.org/10.3290/j.jad.a27794
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Torres, C.R.G., Mailart, M.C., Crastechini, É. et al. A randomized clinical trial of class II composite restorations using direct and semidirect techniques. Clin Oral Invest 24, 1053–1063 (2020). https://doi.org/10.1007/s00784-019-02999-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02999-6