Abstract
Background
A new two-piece abutment design consisting of an upper prosthetic component and tissue-level base has been introduced; however, the biomechanical behavior of such a design has not been documented. This study aimed to investigate the effect of a two-piece abutment design on the stress in the implant components and surrounding bone, as well as its influence on microgap formation.
Methods
To simulate the implant models in the mandibular left first molar area, we established nine experimental groups that included three bone qualities (type II, III, and IV) and three implant–abutment designs (internal bone level, tissue level, and a two-piece design). After the screw was preloaded, the maximum occlusal (600 N) and masticatory (225 N) forces were established. Finite element analysis was performed to analyze the maximum and minimum principal stresses on the peri-implant bone; the von Mises stresses in the implants, abutments, bases, and screws, and the microgaps at the implant–abutment, implant–base, and base–abutment interfaces.
Results
For all three loading methods, the two-piece abutment design and bone-level connection exhibited similarities in the maximum and minimum principal stresses in the peri-implant bone. The von Mises stresses in both screws and bases were greater for the two-piece design than for the other connection types. The smallest microgap was detected in the tissue-level connection; the largest was observed at the implant–base interface in the two-piece design.
Conclusions
The present study found no evidence that the abutment design exerts a significant effect on peri-implant bone stress. However, the mechanical effects associated with the base and screws should be noted when using a two-piece abutment design. The two-piece abutment design also had no advantage in eliminating the microgap.
Similar content being viewed by others
Background
Mechanical complications causing damage to dental implants or their superstructures have been associated with the design of the implant components and can lead to biological complications such as peri-implant tissue damage. Owing to the connection between implant complications and their components, knowledge of the biomechanical influence of implant–abutment connection design is essential for the long-term stability and success of dental implant treatment [1].
In general, the traditional classification of implant–abutment connections is based on the presence of geometric features on the implant’s coronal surface [2]. The abutment connections are then divided into either external or internal connections. The internal connections have been proven to be more favorable [3]. The connections can be further classified into bone-level (BL) and tissue-level (TL) connections according to the implant platform’s alignment with the soft tissue. Both designs reportedly correlate with stress distribution in the peri-implant bone and implant components and with the microgap at the implant–abutment interface (IAI) [4,5,6,7]. The stress around the peri-implant bone is responsible for marginal bone loss [8]; implant component overloading can cause mechanical complications, such as screw loosening or implant and abutment fracture; and the microgap is associated with bacterial infiltration, which may lead to biological complications [9].
The effects of different implant–abutment connections on the implant components and surrounding bone have been evaluated in several studies comparing strains and stresses among different abutment connection types (platform switching, external hexagon, and Morse taper). These studies have confirmed the advantages of the Morse taper connection designs [10,11,12]. Other studies have divided the implant–abutment connection into BL and TL types, reporting that TL connection components have lower stress values and may be preferable for maintaining the marginal bone level [6, 13, 14]. Most studies have concluded that the conical connection [15, 16] and TL connection [4, 7] cause the fewest microgaps.
TL connection designs have been proven to have more advantages for stress distribution and microgap minimization; however, BL connections are used in a large proportion of clinical applications owing to their aesthetic advantages [17]. To minimize implant component-related technical or biological complications, implant manufacturers have improved design concepts by using implant–abutment connections, which have both advantages and disadvantages. Nobel Biocare developed the On1 concept that uses an internal connection, a two-piece (TP) abutment design comprising an upper prosthetic component, which can be replaced, and a tissue-level base attached immediately after implant placement. This design protects soft tissue health without requiring removal of the base portion during impression and has been associated with a decrease in the bone margin level at implant sites [18,19,20,21]. However, such a design has an additional upper short screw that is more fragile and requires two connection interfaces (i.e., the implant–base interface (IBI) and the base–abutment interface (BAI), which may lead to more interface-related complications. To the best of our knowledge, the influence that such a design has on the stress of implant components and surrounding bone, as well as microgap formation, has not been documented.
Bone quality has been shown to correlate with the implant survival rate, with a higher failure rate for implants exhibiting low bone quality [22, 23]. To further evaluate the TP abutment design concept, finite element analysis (FEA) was applied to simulate the maximum occlusion and mastication for three bone qualities. The present study aimed to address the following questions: 1) Does the TP abutment design concept affect stress distribution in the implant components and surrounding bone? 2) How do of different implant–abutment connections influence microgap formation?
Materials and methods
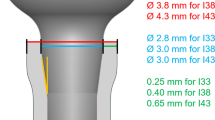
A total of nine three-dimensional finite element models were established (Table 1). Two parameters were considered: bone quality (types II, III, and IV) and the implant–abutment design (BL, TL, or TP connection design). All models consisted of the alveolar bone in the mandibular first molar region and the implant complex (Fig. 1). The simulation of the alveolar bone was performed by reconstructing the cone beam computed tomography data using commercial modeling software (Mimics 21.0, Materialise Group; Geomagic Wrap 2017, 3D Systems). The bone tissue comprised cancellous bone in the center, surrounded by 1 or 2 mm of cortical bone (only type II bone had a cortical bone thickness of 2 mm). The nerve canal was reconstructed using Boolean subtraction. The implant complex was simulated based on the Nobel system, including the following components: the implant, abutment, base, screw, cement layer, and crown. The cement layer thickness was set at 50 µm. Figure 2 shows the dimensions of the three types of implant components. For each system, the same length and diameter were used for both the implant and abutment, although different types of implants, abutments, and screws were used.
Dimensions of three types of implant components and contact surfaces for the analysis of microgap formation. Note: The length and diameter of the implant were 10.6 mm and 4.3 mm; the diameter at the abutment platform was 5.3 mm; the height of the part above the abutment platform was 4 mm, and the diameter was 3.4 mm; the total transmucosal height was 2.05 mm
Table 1 lists the number of elements and nodes in each model. The material properties of the model components, based on previous studies, are summarized in Table 2 [24,25,26,27,28,29,30]. All materials defaulted as homogenous, linearly elastic, and isotropic. To calculate the microgap, the interfaces between the implant, base, abutment, and screws were defined as “contacts”. The coefficient of friction was set to 0.3. The bone–implant interface was defined as a “tie” to symbolize complete osseointegration. In each group, fixation constraints were placed on the mesial and distal sides of the cortical and cancellous bone.
The simulation consisted of two steps (Fig. 3). First, preloading was applied to simulate a tightening torque of 35 N-cm on the screw. Second, external loading was applied to the crown to simulate the maximum occlusal and masticatory loadings [31]. The maximum occlusal loading was applied in the vertical direction. A force of 600 N was applied at eight occlusal points: three on the buccal bevel of the buccal tip, three on the lingual bevel of the buccal tip, and two on the buccal bevel of the lingual tip. The maximum masticatory loading was applied in the vertical and oblique directions (45° to the tooth axis). A force of 225 N was applied to three occlusal points on the buccal bevel of the buccal cusp.
The FEA was completed using ABAQUS 2021 software (Dassault SIMULIA, France). The maximum and minimum principal stress values were calculated to evaluate the tensile and compressive stresses on the peri-implant bones. The tensile and compressive stresses were distinguished by their positive and negative values, respectively. The von Mises stress peaks were used to analyze the biomechanical behavior of the implants, abutments, bases, and screws. The microgap peaks for the IAI, IBI, and BAI were also calculated (Fig. 2).
Results
Maximum and minimum principal stresses
The maximum and minimum principal stress analysis revealed that the tensile and compressive stresses were mainly distributed in the cortical bone. In the models with varied implant–abutment connection designs, the stress distribution in the peri-implant bone was essentially the same. The stress peaks in the TP model were similar to those in the BL model. The effect of the different bone qualities was greater than that of the implant–abutment connection designs. The stress distribution range and peak value increased with decreasing cortical bone thickness and cancellous bone density. At a load of 225 N, the oblique force resulted in a greater range of stress distribution and peak compressive stress (Figs 4, 5 and 6).
Von Mises stresses
In the implants, the von Mises stresses were concentrated mainly at the internal thread and in the implant neck, above the bone level in the TL implant and below the bone level in the BL and TP models. The minimum stress in the implants occurred in the TP-II group (356.55 MPa), while the maximum stress occurred in the BL-IV group (578.29 MPa). The peak stresses in the TL implants were smaller than those in the BL implants under all three loading conditions (Figs. 7 and 10a).
The stresses in the abutments and bases were mainly dispersed in the connection region. The stresses in the abutments of the TL and TP models exhibited smaller peaks and a more even distribution. The lowest stresses were observed in the TL-IV group of abutments (115.02 MPa), whereas the highest were observed in the TP-IV group of bases (607.63 MPa). For all loading conditions, the base in the TP model was subjected to the greatest peak stresses among all connection designs, followed by the BL model (Figs. 8 and 10b).
The stresses in the screws were mainly distributed in the unthreaded bars and were also present in the internal threads of the standard screws in the TP model. Higher stresses were observed for the two screws in the TP model than for the screws in the BL and TL models. The TL-III group of screws had the lowest von Mises stress value (110.65 MPa), and the TP-III group of conventional screws had the highest value (698.93 MPa) (Figs. 9 and 10c).
The peak values for von Mises stress in the implant components under three loading conditions. a Peak values for von Mises stress in the implants; b Peak values for von Mises stress in the abutments and bases (* abutments; ** bases); c Peak values for von Mises stress in the screws (* conventional screws; ** upper short screws)
The bone quality had no effect on the distribution or peak of von Mises stresses in the implants, abutments, bases, or screws. The implants and abutments in the TL connection, as well as the abutments in the TP design, were less affected by the various loadings. The other components, however, experienced elevated stress levels as a result of the oblique loading.
Microgaps
For the BL connection model, the microgap distribution at the IAI was comparable to the distribution at the IBI in the TP model. For the TL connection model, the distribution at the IAI was similar to the distribution at the BAI in the TP model. Under all three loading conditions, the microgap at the IAI for the TL connection model was the smallest, with a minimum value of 2.70 µm (TL-IV group); the microgap at the IBI for the TP connection was the largest, with a minimum value of 22.21 µm (TP-IV group). The size of the microgap was nearly independent of the bone quality. The microgap at the IAI interface for the BL and TL connection types was significantly widened under the 225 N oblique load (Figs. 11 and 12).
Discussion
The TP abutment design preserves the bone interface and connective tissue during the healing period and all restorative operations, avoiding the drawbacks associated with “one abutment one time” or TL implants [20]. However, reports on this design’s biomechanical effects have been limited. In this study, the FEA technique was used to evaluate the stresses in the implant components and surrounding bone as well as the microgap at the connection interface in a TP model. Our results indicated that the TP and BL connections had similar distributions for the maximum and minimum principal stresses in the peri-implant bone; however, the von Mises stress peaks in the bases and screws and the microgap peak at the IBI were significantly larger for the TP connection than for other connection types.
Occlusal overload is among the causes of peri-implant bone resorption. Ideally, the implant–abutment connection design should prevent the transmission of excessive loads to the surrounding bone tissue. Araki and Avag et al. [13, 14] compared the difference in stress and strain in bone tissue between the BL and TL implants. Since the TL implant platform was located above the bone surface, the stresses were all concentrated above the alveolar bone, and the stresses in the bone tissue were much less. In contrast, we did not observe significant differences in the peak tensile or compressive stresses in the bone tissue among the three connection designs. This may be because we utilized loading conditions different from those in the previous study, in which loading forces ranged from 50 to 150 N.
The various bone qualities had a greater effect on the maximum and minimum principal stresses than the implant–abutment connection design. Lee et al. [6] simultaneously analyzed the biomechanical effects of different implant diameters, connection types, and bone densities. In their study, bone density was identified as the most influential factor for bone tissue strain, with low-density bone leading to greater principal strain peaks (P < 0.001). This present study likewise found that the lowest principal stress was always observed in type II bones because they have a significantly greater elastic modulus than bone types III and IV. The greater the elastic modulus, the greater the resistance to compression [29]. Although patients with poor bone quality should be managed with care in clinical practice, these results suggest that bone quality hardly affected the stresses in the implant components and the microgap at the interfaces. Lemos et al. [11] evaluated the effect of vertical bone loss in normal and osteoporotic bone using 3D FEA. Their results also showed that, unlike progressive bone loss, osteoporotic bone affected only the microstrain in the trabecular bone but not the stress in the implants or prosthetic components.
However, the von Mises stress peaks in the implant components differed among the implant–abutment connection designs in our study. Lee et al. [5] reported that stresses in the implant, abutment, and screw were greater for the BL model than the TL model under both vertical and oblique loading conditions. In particular, the stress value of the BL-connected abutment was 3.5 times higher than that of the TL-connected abutment. Similar results have been obtained in other studies [6, 7, 13]. This may cause the better crown-to-root ratio of the TL model when compared with those for the BL and TP connection designs, allowing the TL implant to provide better leverage and more mechanical advantage than the BL implant. For abutments, the load was transferred from the abutment to the BL implant, relying exclusively on the contact surface between the implant and abutment. However, the wide neck of the implant supported the forces from the crown in the TL connection. Some forces were delivered directly to the implant platform, reducing the stress on the abutment [5]. The base of the TP model included a wide platform, similar to the TL implant, allowing direct contact with the crown and helping distribute the stress in the abutment. However, as it can only be transferred to the implant through the connection interface, this resulted in the highest von Mises stress in the base. Additionally, the two screws in the TP model had greater stress under the same loading, even 2–3 times greater than in the BL and TL models. Pumnil et al. [32] analyzed the stress distributions of four different personalized abutments using static FEA, including a two-piece personalized abutment made of a titanium substrate bonded to a zirconia abutment. The authors reported that the titanium base dispersed the stresses in the implant and observed stress concentrations in the screws, in accordance with the findings of the current study. Thus, addressing the mechanical challenges related to the base and screw in the TP connection design is important.
The implant–abutment connections exerted a significant effect on the microgap. Both in vivo and in vitro studies have shown that no connection designs can completely eliminate microgaps and microleakage, but can only minimize them [2]. Zipprich et al. [33] used X-ray imaging to measure the microgap at the IAI of 20 different implant systems for simulated loading up to 200 N, employing conical and flat connections of 0–18.6 and 4.8–42 µm, respectively. Rack et al. [34] observed a microgap of 22 µm under a load of 100 N using high-resolution radiography combined with hard X-ray synchrotron radiation. In this study, the microgap was 2.70–22.21 µm, consistent with the results detected by X-ray imaging. TL connections had the smallest interface microgap because the TL implant neck was larger, and the forces were directed more toward the model’s interior [3, 7]. In contrast, the BL connection model did not have a large neck, and the forces directed to the outside of the model had a greater leveraging effect, leading to a larger microgap. Similarly, the diameter of the base was larger than that of the implant in the TP model, resulting in a smaller microgap at the BAI than at the IBI. Larger microgaps may lead to micromotion and increase the possibility of screw loosening or fracture [35]. Therefore, stomatologists should advise patients with TP abutments to be mindful of oral hygiene and to make regular hospital visits.
Eskitascioglu et al. [36] used FEA to investigate the effect of one to three different loading positions on an implant-fixed denture and surrounding bone stress distribution, observing that the implant and surrounding bone are under excessive stress when force is applied to a single site. Therefore, eight occlusal points were used in this investigation, based on the actual occlusal position during functional movements [31]. The reported average maximum occlusal force in the molar region is 545.7 N; the maximum masticatory force is approximately 37–40% [31, 37]. Our study simulated maximum occlusal and masticatory forces using loadings of 600 N and 225 N (approximately 37% of 600 N). This loading condition was considered the most extreme case. In this study, the implant material was assumed to be pure titanium with a fracture strength of 690 MPa; the abutments, bases, and screws were titanium alloys with a fracture strength of 920 MPa [38]. The analysis showed that all the materials were within the limits under these extremely loading conditions.
Loading conditions are known to influence the stress and microgap [39, 40]. Kim et al. [7] applied a load of 200 N in five directions (0°, 15°, 30°, 45°, and 60°) in order to evaluate the relationship between the loading direction and stress values. In their study, the lowest stress level was observed at a load inclined at 15°, which can be explained by the centrally oriented loading direction and the low torque of the implant and abutment. When the loading angle was increased to 30°, 45°, and 60°, the stress in the implant increased accordingly. The present study likewise found that an oblique force of 45° increased the leverage effect, resulting in greater stresses and microgaps at the same loading of 225 N. Therefore, clinicians should reduce the cusp inclination and minimize the interference of oblique forces when shimming the occlusal contact of the implant prosthesis.
This study had several limitations. First, the finite element model used in our analysis was simplified. For example, while modeling the various bone qualities, only the thickness of cortical bone and the mechanical properties of cancellous bone were altered; their porosity was not considered. This study also assumed that each component was isotropic and that the implant was attached completely to the bone. Although these simplifications sped up the computation process, these assumptions may not reflect clinical reality. Nonetheless, while the exact values among our results may have been affected, these considerations are unlikely to alter the general trend of the findings.
Conclusions
Within the scope of this study, the following conclusions can be drawn:
-
1.
The present study found no evidence that different abutment designs make a significant difference on peri-implant bone stress.
-
2.
The mechanical effects associated with the base and screws should be noted when using a TP abutment design.
-
3.
TL connections ensure the smallest microgaps under maximum occlusal or masticatory force, although the TP abutment design had no advantages in eliminating the microgaps.
Availability of data and materials
All data were calculated by the software itself. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BAI:
-
Base-abutment interface
- BL:
-
Bone-level
- IAI:
-
Implant-abutment interface
- IBI:
-
Implant-base interface
- TL:
-
Tissue-level
- TP:
-
Two-piece
References
Vetromilla BM, Brondani LP, Pereira-Cenci T, Bergoli CD. Influence of different implant-abutment connection designs on the mechanical and biological behavior of single-tooth implants in the maxillary esthetic zone: a systematic review. J Prosthet Dent. 2019;121(3):398-403.e3.
Koutouzis T. Implant-abutment connection as contributing factor to peri-implant diseases. Periodontol 2000. 2019;81(1):152–66.
Lemos CAA, Verri FR, Bonfante EA, Santiago Júnior JF, Pellizzer EP. Comparison of external and internal implant-abutment connections for implant supported prostheses. a systematic review and meta-analysis. J Dent. 2018;70:14–22.
Lee H, Jo M, Noh G. Biomechanical effects of dental implant diameter, connection type, and bone density on microgap formation and fatigue failure: a finite element analysis. Comput Methods Programs Biomed. 2021;200: 105863.
Lee H, Park S, Noh G. Biomechanical analysis of 4 types of short dental implants in a resorbed mandible. J Prosthet Dent. 2019;121(4):659–70.
Lee H, Jo M, Sailer I, Noh G. Effects of implant diameter, implant-abutment connection type, and bone density on the biomechanical stability of implant components and bone: a finite element analysis study. J Prosthet Dent. 2022;128(4):716–28.
Kim JH, Noh G, Hong SJ, Lee H. Biomechanical stress and microgap analysis of bone-level and tissue-level implant abutment structure according to the five different directions of occlusal loads. J Adv Prosthodont. 2020;12(5):316–21.
Qian J, Wennerberg A, Albrektsson T. Reasons for marginal bone loss around oral implants. Clin Implant Dent Relat Res. 2012;14(6):792–807.
Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL. Peri-implant inflammation defined by the implant-abutment interface. J Dent Res. 2006;85(5):473–8.
Pellizzer EP, Lemos CAA, Almeida DAF, de Souza Batista VE, Santiago Júnior JF, Verri FR. Biomechanical analysis of different implant-abutments interfaces in different bone types: an in silico analysis. Mater Sci Eng C Mater Biol Appl. 2018;90:645–50.
Lemos CAA, Verri FR, Noritomi PY, Kemmoku DT, Souza Batista VE, Cruz RS, de Luna Gomes JM, Pellizzer EP. Effect of bone quality and bone loss level around internal and external connection implants: a finite element analysis study. J Prosthet Dent. 2021;125(1):137.e1-137.e10.
Santiago Junior JF, Verri FR, Almeida DA, de Souza Batista VE, Lemos CA, Pellizzer EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl. 2016;63:292–300.
Araki H, Nakano T, Ono S, Yatani H. Three-dimensional finite element analysis of extra short implants focusing on implant designs and materials. Int J Implant Dent. 2020;6(1):5.
Avağ C, Akkocaoğlu M. The evaluation of stress on bone level and tissue level short implants: a finite element analysis (FEA) study. J Stomatol Oral Maxillofac Surg. 2023;124(1S): 101298.
Matsuoka T, Nakano T, Yamaguchi S, Ono S, Watanabe S, Sato T, Yatani H. Effects of implant-abutment connection type and inter-implant distance on inter-implant bone stress and microgap: three-dimensional finite element analysis. Materials (Basel). 2021;14(9):2421.
Pessoa RS, Muraru L, Júnior EM, Vaz LG, Sloten JV, Duyck J, Jaecques SV. Influence of implant connection type on the biomechanical environment of immediately placed implants - CT-based nonlinear, three-dimensional finite element analysis. Clin Implant Dent Relat Res. 2010;12(3):219–34.
Siebert C, Rieder D, Eggert J, Wichmann MG, Heckmann SM. Long-term esthetic outcome of tissue-level and bone-level implants in the anterior maxilla. Int J Oral Maxillofac Implants. 2018;33(4):905–12.
Studenikin R. Prosthodontics using removable platform switching technologies (Multiunit, On1) as exemplified by conical connection implant systems for early and immediate loading. Int J Dent. 2021;2021:6633804.
Rompen E, Fabbri G, Staas T, Valantiejiene V, Linkevicius T. Clinical investigation of the On1 two-piece abutment concept preliminary results. Clin Oral Implants Res. 2008;29(Suppl. 17):319–319.
Fabbri G, Staas T, Linkevicius T, Valantiejiene V, González-Martin O, Rompen E. Clinical performance of a Novel two-piece abutment concept: results from a prospective study with a 1-year follow-up. J Clin Med. 2021;10(8):1594.
Lambrechts T, Doornewaard R, De Bruyckere T, Matthijs L, Deschepper E, Cosyn J. A multicenter cohort study on the association of the one-abutment one-time concept with marginal bone loss around bone level implants. Clin Oral Implants Res. 2021;32(2):192–202.
Staedt H, Rossa M, Lehmann KM, Al-Nawas B, Kämmerer PW, Heimes D. Potential risk factors for early and late dental implant failure: a retrospective clinical study on 9080 implants. Int J Implant Dent. 2020;6(1):81.
Liu C, Xing Y, Li Y, Lin Y, Xu J, Wu D. Bone quality effect on short implants in the edentulous mandible: a finite element study. BMC Oral Health. 2022;22(1):139.
Kitagawa T, Tanimoto Y, Odaki M, Nemoto K, Aida M. Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res B Appl Biomater. 2005;75(2):457–63.
Tang CB, Liul SY, Zhou GX, Yu JH, Zhang GD, Bao YD, Wang QJ. Nonlinear finite element analysis of three implant- abutment interface designs. Int J Oral Sci. 2012;4(2):101–8.
Wu T, Fan H, Ma R, Chen H, Li Z, Yu H. Effect of lubricant on the reliability of dental implant abutment screw joint: an in vitro laboratory and three-dimension finite element analysis. Mater Sci Eng C Mater Biol Appl. 2017;75:297–304.
Liu Y, Gao S, Han Y, Yang Q, Arola D, Zhang D. Bearing capacity of ceramic crowns before and after cyclic loading: an in vitro study. J Mech Behav Biomed Mater. 2018;87:197–204.
Barbier L, Vander Sloten J, Krzesinski G, Schepers E, Van der Perre G. Finite element analysis of non-axial versus axial loading of oral implants in the mandible of the dog. J Oral Rehabil. 1998;25(11):847–58.
Faverani LP, Barão VA, Ramalho-Ferreira G, Delben JA, Ferreira MB, Garcia Júnior IR, Assunção WG. The influence of bone quality on the biomechanical behavior of full-arch implant-supported fixed prostheses. Mater Sci Eng C Mater Biol Appl. 2014;37:164–70.
Tada S, Stegaroiu R, Kitamura E, Miyakawa O, Kusakari H. Influence of implant design and bone quality on stress/strain distribution in bone around implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2003;18(3):357–68.
D’Souza KM, Aras MA. Three-dimensional finite element analysis of the stress distribution pattern in a mandibular first molar tooth restored with five different restorative materials. J Indian Prosthodont Soc. 2017;17(1):53–60.
Pumnil S, Rungsiyakull P, Rungsiyakull C, Elsaka S. Effect of different customized abutment types on stress distribution in implant-supported single crown: a 3D finite element analysis. J Prosthodont. 2022;31(5):e2–11.
Zipprich H, Weigl P, Ratka C, Lange B, Lauer HC. The micromechanical behavior of implant-abutment connections under a dynamic load protocol. Clin Implant Dent Relat Res. 2018;20(5):814–23.
Rack A, Rack T, Stiller M, Riesemeier H, Zabler S, Nelson K. In vitro synchrotron-based radiography of micro-gap formation at the implant-abutment interface of two-piece dental implants. J Synchrotron Radiat. 2010;17(2):289–94.
Sammour SR, Maamoun El-Sheikh M, Aly E-G. Effect of implant abutment connection designs, and implant diameters on screw loosening before and after cyclic loading: in-vitro study. Dent Mater. 2019;35(11):e265–71.
Eskitascioglu G, Usumez A, Sevimay M, Soykan E, Unsal E. The influence of occlusal loading location on stresses transferred to implant-supported prostheses and supporting bone: a three-dimensional finite element study. J Prosthet Dent. 2004;91(2):144–50.
Lundgren D, Laurell L. Occlusal force pattern during chewing and biting in dentitions restored with fixed bridges of cross-arch extension. II. Unilateral posterior two-unit cantilevers. J Oral Rehabil. 1986;13(2):191–203.
Steinemann SG. Titanium–the material of choice? Periodontol. 2000;1998(17):7–21.
Xiao S, Kong X, Yao J, Liu J, Li L, Jiang T, et al. Differences in root stress and strain distribution in buccal and lingual orthodontics: a finite element analysis study. Medicine in Novel Technology and Devices. 2022;14: 100119.
Kul E, Korkmaz İH. Effect of different design of abutment and implant on stress distribution in 2 implants and peripheral bone: a finite element analysis study. J Prosthet Dent. 2021;126(5):664.e1-664.e9.
Acknowledgements
Not applicable.
Funding
This research was supported by the National Natural Science Foundation of China (82201110) and the Science and Technology Development Plan Project of Yantai (2019YD052).
Author information
Authors and Affiliations
Contributions
The study's conception and design were contributed by Huimin Nie, Wenjuan Zhou, and Zhonghao Liu. Material preparation, data collection, and analysis were performed by Yantai Tang, Yan Yang, and Weijie Wu. The original draft of the manuscript was written by Huimin Nie, Yantai Tang, and Yan Yang. The manuscript was reviewed by Wenjuan Zhou and Zhonghao Liu. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the procedures were approved by the Ethics Committee of Binzhou Medical University Affiliated Yantai Stomatological Hospital (No. 2023–002) and conducted in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nie, H., Tang, Y., Yang, Y. et al. Influence of a new abutment design concept on the biomechanics of peri-implant bone, implant components, and microgap formation: a finite element analysis. BMC Oral Health 23, 277 (2023). https://doi.org/10.1186/s12903-023-02989-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-02989-x