Abstract
Introduction
The aim of this study was to verify whether the use of short implants could optimize stress distribution of bone surrounding implants in atrophic mandibles with different bone qualities.
Methods
A three-dimensional model of the atrophic mandible with three levels of bone quality was made using computer software. Short implants (6 mm) and standard implants (10 mm) were used in four designs: Design 1 "All-On four", Design 2 "All-On-four" with two short implants, Design 3 four vertical implants with two short implants, and Design 4 six short implants. The distal short implants were placed at the first molar position. All twelve models were imported into finite element analysis software, and 110 N oblique force was loaded on the left second premolar. Maximum principal stress values of peri-implant bone and the volumes of bone with over 3000 microstrians (overload)were analyzed.
Result
Stress values and volumes of overload bone increased in all four groups with the decline of bone quality. The highest stress values were found in the cortical bone surrounding the Design 1 inclined implant in two lower bone quality mandibles, and the lowest in Design 3. However, Design 1 had less overload bone tissue than all three designs with short implants.
Conclusion
Short implants placed posteriorly helped decrease stress values in peri-implant bone, while bone surrounding short implants had a high resorption risk in low bone quality mandible.
Similar content being viewed by others
Introduction
Dental implants have become the best choice for prosthodontic restoration of edentulous jaws, for significantly recovering the masticatory ability with long-term stable results. However, alveolar bone resorption brings more challenges to the implant inserting, such as bone augmentation procedures, increasing the cost and complication risks [1, 2].
Maló’s “All-on-4” concept, in which four implants are placed between mental foramens with the posterior two tilted, avoids bone resorption areas and gains sufficient bone for standard implants, presenting a high success rate [3]. Tilted placed implants eliminate the need for bone grafting, while bone tissue around them suffers higher stress than around the vertical implants [4]. At the same time, the distal cantilever can cause greater deformation in the superstructures and induce mechanical complications [5, 6].Therefore, more alternative schemes still need to be found.
With the improvement of implant surface treatment methods, more implant specifications are available. At present, short implants are usually considered to be less than 6–8 mm [7].They can replace long implants in atrophic alveolar bone, with less procedure, cost and time [8].
Short implants have been used in fully edentulous jaws as a supplement, and the design even can be seen that full-arch prostheses are supported all by short implants [9]. In some biomechanics studies, compared with traditional “all-on-4” concept, the addition of short implants in the posterior area helps decrease the stress in peri-implant bone [10, 11].The use of short implants in edentulous jaw restoration seems to be worth a try.
There are several methods to analyze the stress of dental implants and bone, including in vitro and in vivo strain gauge tests, photoelastic analysis and finite element analysis (FEA) [12,13,14]. FEA is the most commonly used method because it can simulate different complex situations and provide rich information. In the previous FEA studies about short implants, the cortical bone and cancellous bone were modeled respectively to better simulate the actual situation of the jaw, but the whole jaw was regarded as the same setting, which may mislead the use of short implants in the posterior areas. Actually, there are differences in bone quality between the anterior and posterior jaws [15]. Bone quality has been proved to associate with implant survival rate, and the implant failure rate is higher under low bone quality [16,17,18]. Some FEA studies show that the stress and strain of the peri-implant bone are negatively correlated with the length and diameter of the implant [19,20,21]. Therefore, there may be some potential risks in the use of short implants in the posterior jaws with low bone quality.
Given the possible influence of bone quality on short implants and the inadequacy of current literature, this study aimed to verify whether short implants in atrophic mandibles with different bone qualities optimize the stress distribution in the peri-implant bone, by using the finite element analysis.
Material and methods
Model
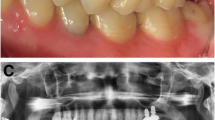
A three-dimensional model of an edentulous atrophic mandible was created from a 62-year-old female patient’s CBCT data in Mimics Medical 21 software (Materialise NV, Leuven, Belgium). The mandible model was ported in the SolidWorks 2018 (Dassault Systèmes SolidWorks Corporation, Waltham, MA, USA), and mirrored the left part to create a symmetrical mandible model(Fig. 1a). For the need to create bone segments with different bone densities, an ideal model was created with a homogeneous layer of cortical bone in each region. Based on the classification proposed by Lekholm and Zarb [22] and Demenko’s study [23], cortical bone and cancellous bone were established separately in different sites (Fig. 1b). Three jaws with different bone densities in the anterior and posterior area were created (Fig. 1c).
a The mandible model was created from a patient ‘s CBCT data, mirrored the left of the edentulous jaw. b Four types of bone were set as: Type I entire part assumed to be cortical; Type II 2mm thickness of cortical bone with inner high-density cancellous bone; Type III 1mm thickness of cortical bone with inner high-density cancellous bone; Type IV 1mm thickness of cortical bone with low-density cancellous bone. c Three kinds of jaws with different bone quality were: A anterior Type I bone and posterior Type II bone ; B anterior Type II bone and posterior Type III bone; C anterior Type II bone and posterior Type IV bone.
Drawing on the Bicon dental implants(Bicon, Boston, MA, USA), we built two specifications of implants, 4 × 6 mm short implant and 4 × 10 mm standard implant sharing the same thread depth and pitch, in SolidWorks (Fig. 2a).
There were four edentulous mandible implants restoration designs as follow (Fig. 2b):
-
(1)
4 standard implants placed in interforaminal regions as the “all -on -4” concept, two straight implants at the lateral incisor sites and two tilted implants angled at 45 degrees lateral bilaterally inserted into the second premolars
-
(2)
6 implants, straightly adding 2 short implants distally at the first molar sites to the 1) protocol
-
(3)
6 implants, 4 standard implants straightly placed at lateral incisor and first premolar sites and two short implants at the first molar sites
-
(4)
6 short implants placed at the lateral incisor, first premolar and first molar sites
The same simplified restoration and abutments models are created for the four designs, and all structures are assembled in Solidworks.
Analysis
The assembled models were ported into the FEA software Abaqus 2018 (Dassault Systèmes SIMULIA Corp, RI, USA). All structures were considered linearly elastic, homogenous, and isotropic, except the mandible was set as orthotropy [13]. The material properties of all the models are listed in Table 1 [12, 24, 25].
A static 30-degree oblique load of 110 N in the buccal-lingual direction was applied at the second premolar site on the framework [26] (Fig. 2c). All the surface contacts were set bonded, which meant the bone-implant interface was considered complete osseointegration. The mandible was given a fixed boundary condition at the mentum and the attachments of the masseter and medial pterygoid. Quadratic tetrahedral elements (c3d10) were used to ensure the accuracy of the results, and the value of mesh size of the peri-implant bone was set up to 0.05 mm.
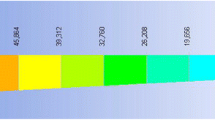
The stress–strain analysis was performed using maximum principal stress and strain. The peak values of maximum principal stress of peri-implant bone tissue were recorded. The volume of elements with strains over 3000 microstrans (με) in bone was counted for the risk of overload, according to the Frost's mechanostat theory [27]. The difference in stress and strain distribution was directly shown in nephograms.
Results
Maximum principal stress
In four designs, the peak values of maximum principal stress were all in the cortical bone around the distal implants (Fig. 3). When the mandible had a high bone density, stress values were at a low level in four models. Stress mainly concentrated at the cortical and cancellous bone junction, like the neck of implants and threads deep into cortical bone. The highest peak stress value appeared in Design 4, followed by Design 2. While the “All-on-4” design had the lowest stress value (Fig. 4).
In the mandible with middle density, the peak stress value significantly increased in all groups. Design 1 had the highest value, followed by Design 4 and Design 2. Due to the reduction of cortical bone thickness, the middle of short implants in the posterior jaw was entirely surrounded by cancellous bone. Thus, stress only concentrated at the bone around the neck of short implants, and we can see the increase in the area of high-stress value.
As the posterior region was reduced to Class IV, the peak stress values increased further for each group. Design 3 had a lower stress value, but it still reached 91.22 MPa. Design 2 and Group 4 gave similar results, while Group 1 still shown the highest value.
Design 3 showed lower peak stress values in mandibles with different bone densities, yet it was similar to the other two groups with short implants except in the middle density. The results for Design 1 appeared to be more affected by the change of bone density. It should be noted that the peak stress values could only represent the condition of stress concentration points but not the overall situation. In the stress nephograms, the high stress areas just expanded slightly as the bone density decreased.
Overload bone volumes
Strain nephograms were plotted separately for under maximum principal stress (tensile stress) (Fig. 5) and minimum principal Stress (compressive stress) (Fig. 6). Unlike in the stress nephograms, the high strain area mainly concentrated at the cancellous bone around implant threads. Elements with strain over 3000με were calculated for it may disrupt the balance of bone remodeling and lead to bone resorption. The results of four designs in different density jaws were shown in the Fig. 7.
Within the high bone density jaws, there was little volume of bone with resorption risk in all four designs. Highest volume appeared in Design 2 as 0.46mm3. While in the two mandibles with lower density, Design 2 and Design 3 had the similar results. The volume of bone in Design 4 showed a higher increase with the change of bone density, in which the bone surrounding the distal short implant was under more risk of resorption than in others. Design 1 maintained the lowest level of overload bone volume.
Discussion
The fretting of the implant caused by excessive immediate loading in the early stage can lead to the failure of the combination of implant and bone [28]. At the same time, excessive force is thought to cause resorption of the supporting bone even after the osseointegration formed. Previous studies have shown that, similar to periodontitis, excessive force will aggravate bone resorption under the effect of bacteria. However, there is not enough evidence to prove that excessive force can independently cause peri-implant bone resorption. Due to the differences of experimental animals, insertion sites and loading conditions (site, direction, size and frequency), the response of bone to loading can be density increased, accelerated resorption and no significant change. The reason may be that the force applied is not ‘excessive’ enough [29, 30].
In Frost’s mechanostat theory, load-bearing bones, including the mandible, can maintain the balance of density within a range of stress. Excessive force above the threshold can result in a decrease in bone density followed by bone resorption [27]. Frost used strain ranges as thresholds for each stage of bone remodeling, which are difficult to directly measure in vivo. FEA can provide information on the stress in each part of models, and is therefore well suited for the evaluation of bone tissue using this theory [25, 31].
In this study, the maximum principal stress peaks were distributed in the bone tissue around the distal implants on the loading side, whether there were four or six implants. Due to the significant difference of elastic modulus between cortical bone and cancellous bone, with a value ratio close to 10:1, the shielding effect made stress mainly concentrated in the cortical bone [10]. In the case of high bone density, the use of short implants in posterior area did not reduce tensile stress. As the bone quality decreased, the situation changed. The “All-On-4” group showed higher peak stress values than others, and Design 3 had the lowest stress value. This is consistent with the results of previous studies, since they had a similar bone quality setting [10, 11].
Comparing the volume of overload bone in four groups, the result was contrary to the stress value. As seen in the strain nephograms, the overload bone tissue is also mainly located around the distal implants. Owing to the horizontal component, the overload bone under tension and pressure was respectively on the lingual and buccal side of the jaw. More cancellous bone showed a tendency to resorption, related to its low stiffness. It underwent greater deformation even when it bore lower stress than cortical bone. The drop in bone density was accompanied by the decrease of the mechanical properties of the jaw, which lead to a significant increase of overload bone. In middle and low bone quality jaws, the volumes of overload bone in the latter three groups were times more than the “All-on-4” group, probably caused by the interaction between the smaller osseointegration area of the short implants and the bone density [19, 21]. Moreover, most of the four standard implants in Design 1 were placed in anterior regions with higher bone quality. In the presence of poor bone conditions, the implant length plays a more critical role in the distribution of stress than the implant diameter, which explains the greater range of overload strain in the jaw completely restored by short implants.
The “All-on-4” concept was invited to provide a simple, economicial and immediate loading scheme for the edentulous jaw. Though tilted implants were thought to put more stress on the supporting bone, they show a high success rate in years of follow-up [32]. In a priori studies, tilted placed distal implants in interforaminal regions helped reduced stress in alveolar bone, in cases that there was no sufficient bone in the posterior areas [33]. Takahashi et al.’s study [4] partially explicated the result associated with the cantilever length. When the load was at the end of the cantilever, the increase of the inclination angle of the end implant helped reduce the length of the cantilever and the moment of force, and the stress in peri-implant bone increased. Besides, when the load was kept at a certain distance from the end implant, the stress rose with the angle of the end implant increasing. The addition of short implants to the posterior area can shorten or even eliminate the cantilever, explaining the reduced stress in bone with the use of short implants in this study.
Short implants enable implant restoration in locations with limited vertical bone, avoiding the additional need for bone augmentation and the following complications [34,35,36,37]. Current literature shows that short implants have a high success rate, as well as similar marginal bone resorption and survival rates compared to longer implants with bone augmentation [38,39,40]. In the study results, short implants in the posterior area had similar bone stress and low risk of overloaded bone as "All-On-4" in the high bone quality mandible. In practice, the bone quality of the mandible is usually acceptable [41], and the use of short implants at the posterior is an alternative. Six or more implants give more options for restoration, such as segmented prostheses. The addition of posterior implants also helps maintain the restoration function in the event of implant loss, especially the distal-end implant [42].
In the study models with poorer bone quality, posterior areas showed a higher trend of bone resorption around short implants. The quality of maxillae, especially the posterior, is often unsatisfactory [41], which gives a warning for the use of short implants. Also, some clinical studies showed that short implants had a higher failure rate in the maxilla than in the mandible [43, 44]. Making the best use of the anterior area seems to be a better choice. While, the design should be selected case by case since the bone quality of the jaws varies considerably between individuals. Some meta-analysis studies show that there seems to be more uncertainty in the survival rate of short implants with the increase of time in function [43, 45, 46], yet these studies included insufficient randomized controlled evaluations and should be interpreted with caution.
Design 3 had better bone stress results among the three short implant designs. When the anterior bone is insufficient for vertical implants, tilted placed implants or short implants between the mental foramina are suitable without bone augmentation. Even in severely atrophic jaws, the only available design is to be supported entirely by short implants, and the bone height remaining also limits the specifications of the short implants [47]. Nonetheless, the bone stress behavior of the interforaminal designs is affected by various factors such as the bicortical anchorage, implant size, and implant distribution [48, 49]. Further experiments and clinical results are still required for validation.
The present study also has some limitations. As a method based on mathematical calculation, the results of FEA are influenced by various parameters, including but not limited to the model geometry, material properties, boundary conditions, loads, and model interface interactions [13]. Though the osseointegration interface followed the bonded settings as similar experiments, complete osseointegration was not in line with the actual situation. The setting of the static load saved the cost of calculation time, but it differed from the real dynamic chewing. Therefore, the results of this study are not precise values and can only be used as a basis for comparison within the designs. By the setting limitation in the study, the effects of different specifications and numbers of implants on stress need to be supplemented in the follow-up research.
In the four designs, the force didn’t lead to direct bone damage even in the lowest bone density [50]. The use of short implants in the posterior region can reduce the bone stress in edentulous restorations to a certain extent. However, in the posterior regions with low bone density, the bone around the short implants over the strain threshold increased and showed a tendency for resorption. In the case of sufficient bone, it is not advisable to completely replace standard implants with short implants. In situations where short implants are required in the posterior regions, it may be helpful to increase the number of short implants [51]. To be clear, the results of this study are only biomechanical results, and the outcome of short implants in edentulous jaws still needs to be proved by long-term clinical research.
Conclusion
According to the result of the FEA study, posteriorly placed short implants can help the stress dispersion in the edentulous mandible with different bone qualities. Short implants can be an alternative in atrophic jaws with high bone quality. However, it brings more risks of bone resorption to use short implants in low bone quality regions. Therefore, the use of short implants in posterior jaws should be cautious.
Availability of data and materials
The data used and analysed during the current study are available from the corresponding author on reasonable request.
References
Marco E, Pietro F, Worthington HV. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2014;5:CD008397. https://doi.org/10.1002/14651858.CD008397.pub2.
Heitz-Mayfield L, Needleman I, Salvi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants. 2014. https://doi.org/10.11607/jomi.2013.g5.
Maló P, de Araújo-Nobre M, Lopes A, Ferro A, Botto J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: a longitudinal study with 10 to 18 years of follow-up. Clin Implant Dent Relat Res. 2019;21(4):565–77. https://doi.org/10.1111/cid.12769.
Takeshi T, Ichiro S, Kaoru S. Influence of number and inclination angle of implants on stress distribution in mandibular cortical bone with All-on-4 Concept. J Prosthodont Res. 2010;54(4):179–84. https://doi.org/10.1016/j.jpor.2010.04.004.
Brilhante BCL, Ferraz MM, Takanori KD, Yoshito NP, Xediek CRL, Ricardo BVA. Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: A prototyping guided 3D-FEA study. Mater Sci Eng C Mater Biol Appl. 2016;69:715–25. https://doi.org/10.1016/j.msec.2016.07.059.
Almeida EO, Rocha EP, Freitas Júnior Amilcar C, Anchieta RB, Ronald P, Nikhil G, Coelho PG. Tilted and short implants supporting fixed prosthesis in an atrophic maxilla: a 3D-FEA biomechanical evaluation. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e332–42. https://doi.org/10.1111/cid.12129.
Jung RE, Bilal A-N, Mauricio A, Gustavo A-O, Stephen B, Nadine B, Vivianne C, Bo C, Andre DS, Faria AR, Stefan F, Gary F, Jeffrey G, Hadi G, Christoph H, Simon J, Asbjørn J, Hideaki K, Johannes K, Chatchai K, Nikos M, Alberto M, Panos P, Michael P, Eik S, Ralf S, Martina S, Christiaan TB, Konstantinos V, Hans-Peter W, Dieter W, Péter W. Group 1 ITI Consensus Report: the influence of implant length and design and medications on clinical and patient-reported outcomes. Clin Oral Implants Res. 2018;29(Suppl 16):69–77. https://doi.org/10.1111/clr.13342.
Bitinas D, Bardijevskytė G. Short implants without bone augmentation vs long implants with bone augmentation: systematic review and meta-analysis. Aust Dent J. 2021;66(Suppl 1):S71–81. https://doi.org/10.1111/adj.12859.
Luigi G, Marco A, Umberto E, Massimiliano S, Paolo T, Denis C. 6-mm-short and 11-mm-long implants compared in the full-arch rehabilitation of the edentulous mandible: a 3-year multicenter randomized controlled trial. Clin Oral Implants Res. 2020;31(1):64–73. https://doi.org/10.1111/clr.13547.
Doganay O, Kilic E. Comparative finite element analysis of short implants with different treatment approaches in the atrophic mandible. Int J Oral Maxillofac Implants. 2020;35(4):e69–76. https://doi.org/10.11607/jomi.8122.
Ziya AY, Derya K, Songul K, Erol C. Biomechanical comparison of implantation approaches for the treatment of mandibular total edentulism. Proc Inst Mech Eng H. 2020;234(10):1139–50. https://doi.org/10.1177/0954411920943427.
Yu-Jen WA, Jui-Ting H, Lih-Jyh F, Heng-Li H. Biomechanical effect of implant design on four implants supporting mandibular full-arch fixed dentures: in vitro test and finite element analysis. J Formos Med Assoc. 2020;119(10):1514–23. https://doi.org/10.1016/j.jfma.2019.12.001.
María P-P, Carlos M-M, Gehrke SA, Carlos P-F. Influence of bone definition and finite element parameters in bone and dental implants stress: a literature review. Biology. 2020;9(8):224. https://doi.org/10.3390/biology9080224.
Brunski JB. Biomechanical aspects of the optimal number of implants to carry a cross-arch full restoration. Eur J Oral Implantol. 2014;7(Suppl 2):S111–31.
Shiuan-Hui W, Yen-Wen S, Lih-Jyh F, Shin-Lei P, Ming-Tzu T, Heng-Li H, Jui-Ting H. Relationship between cortical bone thickness and cancellous bone density at dental implant sites in the Jawbone. Diagnostics. 2020;10(9):710. https://doi.org/10.3390/diagnostics10090710.
Goiato MC, dos Santos DM, Santiago JF, Moreno A, Pellizzer EP. Longevity of dental implants in type IV bone: a systematic review. Int J Oral Maxillofac Surg. 2014;43(9):1108–16. https://doi.org/10.1016/j.ijom.2014.02.016.
Henning S, Martin R, Martin LK, Bilal A-N, Kämmerer PW, Diana H. Potential risk factors for early and late dental implant failure: a retrospective clinical study on 9080 implants. Int J Implant Dent. 2020;6(1):81. https://doi.org/10.1186/s40729-020-00276-w.
Chrcanovic BR, Albrektsson T, Wennerberg A. Bone quality and quantity and dental implant failure: a systematic review and meta-analysis. Int J Prosthodont. 2017;30(3):219–37. https://doi.org/10.11607/ijp.5142.
Demenko V, Linetskiy I, Nesvit K, Hubalkova H, Nesvit V, Shevchenko A. Importance of diameter-to-length ratio in selecting dental implants: a methodological finite element study. Comput Methods Biomech Biomed Engin. 2014;17(4):443–9.
Ueda N, Takayama Y, Yokoyama A. Minimization of dental implant diameter and length according to bone quality determined by finite element analysis and optimized calculation. J Prosthodont Res. 2017;61(3):324–32. https://doi.org/10.1016/j.jpor.2016.12.004.
Li T, Kong L, Wang Y, Hu K, Song L, Liu B, Li D, Shao J, Ding Y. Selection of optimal dental implant diameter and length in type IV bone: a three-dimensional finite element analysis. Int J Oral Maxillofac Surg. 2009;38(10):1077–83. https://doi.org/10.1016/j.ijom.2009.07.001.
Lekholm U, Zarb GA. Patient selection and preparation. In: Brånemark PI, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence; 1985. p. 199–209.
Demenko V, Linetsky I, Nesvit V, Linetska L, Shevchenko A. FE study of bone quality effect on load-carrying ability of dental implants. Comput Methods Biomech Biomed Engin. 2014;17(16):1751–61. https://doi.org/10.1080/10255842.2013.766173.
O’Mahony AM, Williams JL, Katz JO, Spencer P. Anisotropic elastic properties of cancellous bone from a human edentulous mandible. Clin Oral Implants Res. 2000;11(5):415–21. https://doi.org/10.1034/j.1600-0501.2000.011005415.x.
O’Mahony AM, Williams JL, Spencer P. Anisotropic elasticity of cortical and cancellous bone in the posterior mandible increases peri-implant stress and strain under oblique loading. Clin Oral Implants Res. 2001;12(6):648–57. https://doi.org/10.1034/j.1600-0501.2001.120614.x.
Lundqvist S, Haraldson T. Oral function in patients wearing fixed prosthesis on osseointegrated implants in the maxilla: 3-year follow-up study. Scand J Dent Res. 1992;100:279–83.
Frost HM. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004;74(1):3–15. https://doi.org/10.1043/0003-3219(2004)074%3c0003:AUOBPA%3e2.0.CO;2.
Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res. 1998;43(2):192–203. https://doi.org/10.1002/(sici)1097-4636(199822)43:2%3c192::aid-jbm14%3e3.0.co;2-k.
Delgado-Ruiz RA, Calvo-Guirado JL, Romanos GE. Effects of occlusal forces on the peri-implant-bone interface stability. Periodontol 2000. 2019;81(1):179–93. https://doi.org/10.1111/prd.12291.
Ignace N, Joke D, Katleen V. Occlusal overload and bone/implant loss. Clin Oral Implants Res. 2012;23(Suppl 6):95–107. https://doi.org/10.1111/j.1600-0501.2012.02550.x.
Hyeonjong L, Soyeon P, Gunwoo N. Biomechanical analysis of 4 types of short dental implants in a resorbed mandible. J Prosthet Dent. 2019;121(4):659–70. https://doi.org/10.1016/j.prosdent.2018.07.013.
Ramos CB, Tomas A, Ann W. Tilted versus axially placed dental implants: a meta-analysis. J Dent. 2015;43(2):149–70. https://doi.org/10.1016/j.jdent.2014.09.002.
Ozan O, Kurtulmus-Yilmaz S. Biomechanical comparison of different implant inclinations and cantilever lengths in all-on-4 treatment concept by three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2018;33(1):64–71. https://doi.org/10.11607/jomi.6201.
Thomas S-J, Baungaard NH. Prosthetic rehabilitation of the partially edentulous atrophic posterior mandible with short implants (≤ 8 mm) compared with the sandwich osteotomy and delayed placement of standard length implants (> 8 mm): a systematic review. J Oral Maxillofac Res. 2018;9(2):e2. https://doi.org/10.5037/jomr.2018.9202.
Lizio G, Pellegrino G, Felice P. Posterior Jaws rehabilitation with < 7mm-short Implants. A review. J Stomatol Oral Maxillofac Surg. 2021. https://doi.org/10.1016/j.jormas.2021.09.010.
Esposito M, Barausse C, Pistilli R, Piattelli M, Di Simone S, Ippolito DR, Felice P. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone Five-year results from a randomised controlled trial. Int J Oral Implantol. 2019;12(1):39–54.
Marco E, Jacopo B, Carlo B, Roberta G, Gilberto S, Pietro F. Short implants versus longer implants in vertically augmented atrophic mandibles: A systematic review of randomised controlled trials with a 5-year post-loading follow-up. Int J Oral Implantol. 2019;12(3):267–80.
Giovanna I, Vittoria P, Pietro F, Carlo B, Adriano P, Massimo DF. Are <7-mm long implants in native bone as effective as longer implants in augmented bone for the rehabilitation of posterior atrophic jaws? A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2020;22(5):552–66. https://doi.org/10.1111/cid.12946.
Carlo B, Roberto P, Luigi C, Lorenzo B, Agnese F, Pietro F. A 5-year randomized controlled clinical trial comparing 4-mm ultrashort to longer implants placed in regenerated bone in the posterior atrophic jaw. Clin Implant Dent Relat Res. 2022;24(1):4–12. https://doi.org/10.1111/cid.13061.
Felice P, Pistilli R, Barausse C, Piattelli M, Buti J, Esposito M. Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial. Int J Oral Implantol. 2019;12(1):57–72.
Oliveira MR, Gonçalves A, Gabrielli MA, de Andrade CR, Vieira EH, Pereira-Filho VA. Evaluation of alveolar bone quality: correlation between histomorphometric analysis and Lekholm and Zarb classification. J Craniofac Surg. 2021;32(6):2114–8. https://doi.org/10.1097/SCS.0000000000007405.
Daudt Polido W, Aghaloo T, Emmett TW, Taylor TD, Morton D. Number of implants placed for complete-arch fixed prostheses: a systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):154–83. https://doi.org/10.1111/clr.13312.
Xinxin Xu, Jiao H, Xuewei Fu, Yunchun K, Hui Y, Jinlin S, Ling Xu. Short implants versus longer implants in the posterior alveolar region after an observation period of at least five years: a systematic review and meta-analysis. J Dent. 2020;100:103386. https://doi.org/10.1016/j.jdent.2020.103386.
Pommer B, Mailath-Pokorny G, Haas R, Buseniechner D, Millesi W, Fürhauser R. Extra-short (< 7 mm) and extra-narrow diameter (< 3.5 mm) implants: a meta-analytic literature review. Eur J Oral Implantol. 2018;11(Suppl 1):S137–46.
Vazouras K, de Souza AB, Gholami H, Papaspyridakos P, Pagni S, Weber HP. Effect of time in function on the predictability of short dental implants (≤6 mm): a meta-analysis. J Oral Rehabil. 2020;47(3):403–15. https://doi.org/10.1111/joor.12925.
Panos P, Andre DS, Konstantinos V, Hadi G, Sarah P, Hans-Peter W. Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: a meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):8–20. https://doi.org/10.1111/clr.13289.
Pistilli R, Barausse C, Gasparro R, Berti C, Felice P. Minimally invasive fixed rehabilitation of a totally edentulous severely atrophic mandible with 4-mm ultrashort immediately loaded implants: a case report. Int J Periodontics Restorative Dent. 2020;40(4):549–59. https://doi.org/10.11607/prd.4157.
Pimentel MJ, Silva WJ, Del Bel Cury AA. Short implants to support mandibular complete dentures—photoelastic analysis. Braz Oral Res. 2017;31:e18. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0018.
Peixoto HE, Camati PR, Fernanda F, Sotto-Maior BS, Martinez EF, Peruzzo DC. Rehabilitation of the atrophic mandible with short implants in different positions: a finite elements study. Mater Sci Eng C Mater Biol Appl. 2017;2017(80):122–8. https://doi.org/10.1016/j.msec.2017.03.310.
Ferreira MB, Barão VA, Delben JA, Faverani LP, Carolina HA, Assunção WG. Non-linear 3D finite element analysis of full-arch implant-supported fixed dentures. Mater Sci Eng C Mater Biol Appl. 2014;38:306–14. https://doi.org/10.1016/j.msec.2014.02.021.
Reza T, Hamidreza A, Ehsan A, Farzaneh H. Does increasing the number of short implants reduce marginal bone loss in the posterior mandible? A prospective study. Br J Oral Maxillofac Surg. 2016;54(7):731–5. https://doi.org/10.1016/j.bjoms.2016.04.010.
Acknowledgements
Not applicable.
Funding
This work was supported by Medical Innovation Project of Fujian Province (2021CXA035), Natural Science Foundation of Fujian Province (2021J01792) and the Startup Fund for scientific research of Fujian Medical University (2020QH2046).
Author information
Authors and Affiliations
Contributions
CL, JX and DW conceived and designed the study. CL and YX performed the finite element analysis. CL, YLi, YLin wrote the paper. CL reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the 1964 Helsinki declaration and its later amendments, and was approved by the Research Ethics Committee of School and Hospital of Stomatology, Fujian Medical University (No. 69, 2021). Written informed consent was obtained from all participants in this study.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, C., Xing, Y., Li, Y. et al. Bone quality effect on short implants in the edentulous mandible: a finite element study. BMC Oral Health 22, 139 (2022). https://doi.org/10.1186/s12903-022-02164-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-022-02164-8