Abstract
Background
The interrelation between metabolic syndrome (MetS) and Parkinson’s disease (PD) likely arises from shared pathological mechanisms. This study thus aims to examine the impact of MetS and its components on PD.
Methods
This study utilized data extracted from the National Health and Nutrition Examination Survey database spanning 1999 to 2020. The random forest algorithm was applied to fill in the missing data. Propensity score optimal full matching was conducted. The data were adjusted by total weights derived from both sampling and matching weights. The weighted data were utilized to create multifactor logistic regression models. Odds ratios (ORs) and average marginal effects, along with their corresponding 95% confidence intervals (CIs), were calculated.
Results
MetS did not significantly affect the risk of PD (OR: 1.01; 95% CI: 0.77, 1.34; P = 0.92). Hypertension elevated the risk of PD (OR: 1.33; 95% CI: 1.01, 1.76; P = 0.045), accompanied by a 0.26% increased probability of PD occurrence (95% CI: 0.01%, 0.52%; P = 0.04). Diabetes mellitus (DM) had a 1.38 times greater likelihood of developing PD (OR:1.38; 95% CI: 1.004, 1.89; P = 0.046), corresponding to a 0.32% increased probability of PD occurrence (95% CI: -0.03%, 0.67%; P = 0.07). Nevertheless, no correlation was observed between hyperlipidemia, waist circumference and PD.
Conclusion
MetS does not affect PD; however, hypertension and DM significantly increase the risk of PD.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS) encompasses the accumulation of excessive abdominal fat, insulin resistance (IR), abnormal lipid levels, and high blood pressure [1, 2]. Quantifying the prevalence of MetS is challenging due to the lack of global statistics. Nevertheless, given that MetS occurs at a rate approximately three times higher than diabetes, its prevalence might be estimated at approximately 25% of the global population [3]. Parkinson’s disease (PD) is projected to experience a fourfold increase in frequency over the next 30 years, becoming the second most prevalent neurodegenerative illness [4]. PD is characterized by clinical manifestations [5] such as bradykinesia, stiffness, a flexed posture, “freezing” episodes, and the loss of postural reflexes. These motor abnormalities, commonly observed in PD, result from the depletion of dopamine neurons in the brain’s nigrostriatal pathway.
Despite the elusive nature of PD pathophysiology, emerging evidence suggests a complex involvement of MetS in the disease’s pathological processes. These processes encompass IR, neuroinflammation, accumulation of α-synuclein proteins, and mitochondrial dysfunction [6]. A chronic hyperglycemic state may lead to changes in postsynaptic dopamine receptors, as suggested by research on rat models [7]. Obesity-related low-grade inflammation can induce neuroinflammation through various pathways, including the choroid plexuses and disruption of the blood–brain barrier. Therefore, we hypothesized that metabolic and neurodegenerative diseases may be interrelated because of their shared pathophysiological mechanisms. Although several studies have investigated the association between MetS components and PD events, the results have been inconsistent [8] due to varying methodologies and diverse study populations. Establishing whether MetS and its components are independent risk factors for PD is crucial to determining if patients newly diagnosed with MetS should be monitored for PD development and if PD patients might already exhibit concurrent metabolic abnormalities. This study further explores the impact of MetS and its components on PD utilizing the National Health and Nutrition Examination Survey (NHANES) database, which offers a nationally representative sample.
Materials and methods
Study population
Data was obtained from the NHANES, a comprehensive study that investigates a wide range of demographic characteristics and health issues in the United States. The survey sample is selected from all states across the country, ensuring national representation. Due to the age of onset of PD, the study included individuals who were 18 years old or older. And since the special characteristics of pregnant women, they were not included in this study. Cases with missing data for MetS and PD were excluded from the analysis. Data from eleven consecutive two-year cycles, spanning from 1999 to 2000 to 2019–2020 (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, 2017–2018, and 2019–2020), were utilized. The NHANES study received approval from the National Center for Health Statistics Ethics Review Board, with the most recent review conducted on August 24, 2022. Informed consent was obtained from all participants.
MetS diagnosis
In this study, the revised diagnostic criteria [9] were determined through consultation between the American Heart Association/National Heart, Lung, and Blood Institute and the International Diabetes Federation. The diagnostic criteria consist of the following five elements: (i) a waist circumference of at least 102 cm for men and 88 cm for women in the U.S. population; (ii) elevated triglycerides of at least 150 mg/dL; (iii) decreased high-density lipoprotein (HDL) cholesterol of at least 40 mg/dL for men and 50 mg/dL for women; (iv) systolic blood pressure of at least 130 mmHg and/or diastolic blood pressure of at least 85 mmHg; (v) fasting blood glucose of 100 mg/dL or higher. Drug treatment serves as an alternative indication for the last four elements. If any three of these criteria are met, a diagnosis of MetS may be made.
MetS was categorized into four components: high waist circumference (WC), hypertension, diabetes mellitus (DM), and hyperlipidemia. The diagnosis is based on the presence of each condition and is not limited to a specific indicator under the MetS diagnosis entry. The diagnosis of high WC was the same as the first item of the MetS diagnoses. Hypertension was diagnosed based on the following factors: the mean of three blood pressure readings [≥ 140 mmHg for systolic blood pressure and ≥ 90 mmHg for diastolic blood pressure], antihypertensive drug use, and self-reported high blood pressure. DM diagnosis was based on self-report of diabetes, glucose-lowering medication usage, levels of glycated hemoglobin [≥ 6.5 mmol/L], fasting glucose [≥ 7 mmol/L], random glucose [≥ 11.1 mmol/L], and oral glucose tolerance test [≥ 11.1 mmol/L]. Hyperlipidemia was characterized by hypertriglyceridemia [triglycerides ≥ 150 mg/dL], hypercholesterolemia [total cholesterol ≥ 200 mg/dL, low-density lipoprotein ≥ 130 mg/dL, or HDL < 40 mg/dL for men and 50 mg/dL for women], and the use of lipid-lowering medications.
PD diagnosis
PD was diagnosed based on drug use recorded in the drug file provided by the NHANES database. This study focuses on the second level category called antiparkinson agents according to the Multum Lexicon Therapeutic Classification Scheme. Within this category, two sub-level three level categories are considered: anticholinergic antiparkinson agents and dopaminergic antiparkinsonism agents.
Covariates
Age, sex, race, education, smoking, alcohol and coffee consumption [10] were self-reported by participants. Smoking status was categorized into three groups: non-smokers [< 100 cigarettes in a lifetime], former smokers [≥ 100 cigarettes in a lifetime but not currently smoking], and current smokers [≥ 100 cigarettes in a lifetime and smoking some days or every day]. Alcohol consumption [11] was divided into three categories: non-alcohol user [did not drink last year or had 1 drink for male], mild alcohol user [≥ 1 drinks for females and 2 for males, or binge drinking (≥ 4 drinks on the same occasion for females, ≥ 5 drinks on the same occasion for males) ≥ 2 and < 5 days per month, and heavy alcohol user [≥ 3 drinks for females and 4 drinks for males, or binge drinking on 5 or more days per month]. Coffee consumption refers to the amount of coffee (in grams) consumed from dietary data on the first day. For simplicity in subsequent analysis, the data were categorized into three levels: Q1, Q2, and Q3, with corresponding medians of 0, 179.9, and 503.2 g.
Statistical analysis
The missing data for the two primary variables, MetS and PD, were excluded from the analysis. Missing values for the remaining variables were imputed using the random forest algorithm, which employs known variables as independent variables and variables with missing values as dependent variables to predict the missing values. This method offers high prediction accuracy and robustness. To balance the effects of covariates between groups with and without MetS, including its components, the propensity score matching (PSM) approach was utilized. Given the limited number of PD patients, optimal full matching was chosen to minimize sample loss. Sampling weights were calculated before matching. These weights were generated for complex sample designs using mobile examination center exam weights (WTMEC4YR for 1999–2002 and WTMEC2YR for 2003–2020), along with the variables SDMVPSU and SDMVSTRA. The matching process took into account the sampling weight [12,13,14]. The total weight was calculated by multiplying the sampling and matching weight. The data was then weighted using the total weight. The standardized mean difference (SMD) was the statistical measure used to assess balance, with a value of < 0.1 indicating equilibrium. Continuous variables were described using mean and standard error, while categorized variables were described using frequency and percentage. The balance of covariates was re-evaluated by independent-samples t-test and chi-square test. The study estimated the effect of MetS and its component on PD in the weighted sample by total weights, adjusting for the covariates to improve precision and reduce bias. Simultaneously, a stratification analysis of variables that failed to match balance was conducted. Effect sizes were expressed as odds ratios (ORs) and the average marginal effects with a 95% confidence interval (CI). The significance level for two-tailed tests was set at 0.05. A sensitivity analysis was performed using the conventional method of intervariable adjustment, multi-factor logistic regression, with data weighted by sampling weights. It is important to note that the results of the analysis of the four components of MetS should be interpreted as exploratory due to the potential for type 1 errors from multiple comparisons. This research was analyzed using R software (version 4.2.2, R Development Core Team. Vienna, Austria) with the following packages: missForest (version 1.5) for imputation, MatchIt (version 4.5.0) for PSM, cobalt (version 4.5.1) for assessing post-PSM data balance, survey (version 4.1-1) for weighting and logistic regression, marginaleffects (version 0.15.1) for estimating average marginal effects, and ggplot2 (version 3.4.2) and cowplot (version 1.1.1) for visualization.
Results
Population characteristics
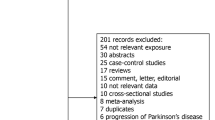
The study included data of 63,576 individuals after applying filters, including 591 participants with PD. The data was weighted to represent the estimated population of the United States, which is approximately 223,670,260. The specific screening procedure is illustrated in Fig. 1. The population with MetS had a higher prevalence of males, advanced age, and greater levels of coffee intake. The MetS group consisted of a significant proportion of former smokers and light drinkers while having a lower proportion of current smokers and heavy drinkers than those without MetS. Table 1 presents the characteristics of the populations with and without MetS. After performing PSM, differences were noted in sex, alcohol and coffee consumption between those with and without MetS, as shown in Supplementary Material Table S1. The baseline characteristics of hypertension, hyperlipidemia, DM, and different WC after PSM are shown in Tables S2-S5 of the Supplementary Material.
Balance test for PSM
For the data weighted by total weight, the balance statistic SMD was calculated, and the balance of covariates was achieved between individuals with and without MetS or its components (SMD < 0.1), as shown in Supplementary Material Table S6. Figure 2 demonstrates the balance of the data for PS before matching, after matching with matching weights weighted and after matching with total weights.
Association between MetS and PD
The presence of MetS did not significantly impact the risk of PD (OR: 1.01; 95% CI: 0.77, 1.34; P = 0.92), as seen in Table 2. Conversely, DM increased the likelihood of developing PD (OR:1.38; 95% CI: 1.004, 1.89; P = 0.047). DM was associated with a slight increase of 0.32% (95% CI: -0.03%, 0.67%; P = 0.07) in the likelihood of developing PD. Individuals with hypertension had a 1.33-fold increased likelihood of developing PD compared with those without hypertension (OR: 1.33; 95% CI: 1.006, 1.76; P = 0.045). Hypertension was associated with a 0.26% (95% CI: 0.01%, 0.52%; P = 0.04) increase in the likelihood of developing PD. Nevertheless, there was no correlation between hyperlipidemia and WC and PD. Logistic regression analyses in sensitivity analyses suggested that hypertension (OR: 1.38; 95% CI: 1.03, 1.847; P = 0.03), DM (OR: 1.36; 95% CI: 1.07, 1.74; P = 0.01), and high WC (OR: 1.44; 95% CI: 1.13, 1.84; P = 0.003) increased the odds of developing PD, as shown in Table 3.
The results of the stratified analyses are shown in Supplementary Material Table S7. Among individuals with high coffee consumption, hypertension (OR: 1.94; 95% CI: 1.25, 3.02; P = 0.003) and DM (OR: 1.79; 95% CI: 1.07, 2.98; P = 0.025) were associated with an increased risk of PD. High WC was linked to an increased risk of PD in individuals younger than 50 years (OR: 2.15; 95% CI: 1.28, 3.60; P = 0.004) and those with lower education (OR: 1.99; 95% CI: 1.003, 3.74; P = 0.049).
Discussion
MetS is a widespread and escalating global public health issue associated with multiple chronic illnesses. The study aimed to investigate the relationship between MetS and PD, which are believed to share overlapping pathological processes. However, this study did not find any correlation between MetS and the likelihood of developing PD. When examining the components of MetS, it was revealed that high WC and hyperlipidemia had no impact on PD, while hypertension and DM increased the likelihood of PD.
Previous research has presented contradictory findings regarding the relationship between MetS and PD. Some studies suggest that MetS increases the risk of PD, while others propose the opposite, and some find no significant relationship [15]. MetS, being a composite comprised of various states, produces distinct effects from each component. For example, a study [16] using data from the National Health Insurance Service of Korea found that the incidence of PD was 1.23 times higher in individuals with MetS. High blood pressure, low HDL cholesterol, and high fasting blood glucose were linked to an increased incidence of PD, but not high WC. These findings [17, 18] remained consistent even when considering the length of the follow-up period or the longitudinal research. Additionally, abdominal obesity was associated with an elevated risk of developing PD. MetS was found to increase the risk of progression from mild Parkinsonian signs to PD [19]. MetS exacerbates non-motor symptoms in patients with PD [20], such as cognitive impairment [21]. One study [22] suggests that hypertension exerts a detrimental effect on memory and verbal fluency in early PD. According to a vast Finnish investigation [23], elevated total cholesterol levels were correlated with an increased risk of PD. A meta-analysis [24] revealed a 27% higher relative risk of PD in individuals with DM than in those without. Antihypertensive medication may reduce the risk of PD in patients with newly diagnosed hypertension [25, 26]. Nevertheless, the MetS population has a reduced risk of PD. While elevated serum triglyceride and fasting glucose levels were predictive of a lower incidence of PD, a higher BMI was suggestively associated with an increased risk of PD [27]. MetS was associated with reduced occurrence of falls in patients with PD, indicating a potential beneficial effect on motor symptoms [28]. The results of a Japanese case-control study showed a significant link between DM, hypertension, and high cholesterol levels and a lower risk of PD [29]. Additional studies have demonstrated that a high WC [30] and obesity [31] were linked to a reduced likelihood of PD. Furthermore, a study [32] also found no association between a prior medical history of hypertension, hypercholesterolemia, or diabetes with the chance of developing PD.
Numerous pathogenic processes, including IR, oxidative stress, immunology, and inflammation, may overlap between MetS and PD [8, 33, 34]. This overlap suggests that PD should be treated as a metabolic disease [35, 36]. IR is a key factor in type 2 diabetes and is now recognized as an important mechanism in the association between DM and PD. Insulin, beyond its role in glucose regulation, acts as a major contributor to many diseases [37], including neurological conditions, and plays various functions in the brain [38], including the maintenance of cellular homeostasis, prevention of ROS generation, and promotion of cell survival. The brain is highly responsive to insulin, enabling it to regulate the functions of neurons and glial cells, resulting in changes in emotions, cognition, and behavior [39]. When insulin function in the brain is compromised, it initiates cellular disturbances, resulting in pathological states. For example, MetS and DM can render dopaminergic neurons vulnerable [40] and affect dopamine neuron survival [41]. IR may lead to reduced expression of dopamine transporter proteins on the striatal surface, as demonstrated in animal models [42]. Furthermore, the development of PD may be influenced by mitochondrial dysfunction, oxidative stress, and microglia-mediated inflammatory responses, all of which could contribute to the association between PD and DM.
Hypertension may increase the risk of PD through several mechanisms [43, 44]. First, hypertension induces dysregulation of the autonomic nervous system, leading to an increased cardiac load and rapid blood flow in the arteries, exerting variable degrees of pressure on the cerebrovascular system. Patients with hypertension often experience blood pressure fluctuations, especially at night, resulting in an imbalance in cerebral perfusion, particularly at the level of small arteries and microvessels. The imbalance created by hypertension can lead to an increased risk of neuronal damage, further heightening the likelihood of developing PD. Additionally, arterial stiffness induced by hypertension reduces the elasticity of cerebral blood vessels, leading to increased resistance to cardiac output and subsequently diminishing cerebral perfusion. Furthermore, hypertension can disrupt the blood-brain barrier and cause capillary abnormalities, both of which contribute to accelerated neuronal degeneration, ultimately increasing the risk of PD.
Cholesterol has both preventive and detrimental effects on PD neuropathology [45]. Cholesterol may have potential neuroprotective benefits against the development of PD by modulating ion channels and receptors, which can be influenced by changes in cholesterol levels. However, elevated blood cholesterol levels can indirectly increase the risk of PD. This is due to the induction of oxidative stress, inflammation, and apoptosis caused by a compound called 27-hydroxycholesterol. Furthermore, the presence of cholesterol is associated with the degeneration of dopaminergic neurons in the substantia nigra and the aggregation of α-synuclein in the brain, both of which are factors contributing to the development of PD.
This study incorporates data spanning 11 year-cycles, from 1999 to 2020, extracted from the NHANES database, which represents a substantial study population. To ensure an accurate representation of nearly the entire population of the United States, the data is weighted using a complex sampling procedure, even when performing PSM. Additionally, our study provides two distinct measures of effect. Given the low positivity rate of PD, the numerical magnitude of the OR can be somewhat misleading. Hence, we also offer estimates of the average marginal effect, which is equivalent to the risk difference in this study. This dual approach enhances the comprehensiveness of our findings, allowing readers to better understand the true effect size between variables. However, there are certain unavoidable limitations in this study. It is a cross-sectional study, and while we used PSM and traditional covariate adjustment methods to mitigate the influence of confounding factors, the presence of unknown variables and the potential for reverse causation remain. Therefore, the results of this study do not support the inference of causality. Furthermore, due to the absence of data regarding the symptoms of PD in the database, this study solely relied on the presence or absence of relevant medication to diagnose PD. Consequently, it was unable to gather information on the symptoms of PD in the subset of patients who were not taking medication. The results of the present study suggest that MetS is not associated with PD, whereas DM and hypertension are correlated with PD. Due to the limitations of the research methodology of this study, further validation through additional studies is warranted. Future research should include prospective cohort studies and Mendelian randomization studies to investigate causality, as well as mechanistic studies to elucidate potential pathways.
Conclusion
The findings do not support the hypothesis that MetS plays a direct role in influencing the development of PD. However, within the multifaceted landscape of MetS, it is evident that hypertension and DM are associated with an increased likelihood of developing PD. On the other hand, high WC and hyperlipidemia do not seem to have a significant impact on the risk of PD.
Data availability
The original data for this study are available from publicly available databases (https://www.cdc.gov/nchs/nhanes/index.htm). Further inquiries can be directed to the corresponding author.
Abbreviations
- MetS:
-
Metabolic Syndrome
- IR:
-
Insulin resistance
- PD:
-
Parkinson’s disease
- NHANES:
-
National Health and Nutrition Examination Survey
- HDL:
-
High-density lipoprotein
- WC:
-
Waist circumference
- DM:
-
Diabetes mellitus
- PSM:
-
Propensity score matching
- SMD:
-
Standardized mean difference
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Cornier M-A, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, et al. The metabolic syndrome. Endocr Rev. 2008;29:777–822. https://doi.org/10.1210/er.2008-0024.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28. https://doi.org/10.1016/S0140-6736(05)66378-7.
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20:12. https://doi.org/10.1007/s11906-018-0812-z.
Tolosa E, Garrido A, Scholz SW, Poewe W. Challenges in the diagnosis of Parkinson’s disease. Lancet Neurol. 2021;20:385–97. https://doi.org/10.1016/S1474-4422(21)00030-2.
Reich SG, Savitt JM. Parkinson’s Disease. Med Clin North Am. 2019;103:337–50. https://doi.org/10.1016/j.mcna.2018.10.014.
Olson L. Biomedicine. Combating Parkinson’s disease–step three. Science. 2000;290:721–4. https://doi.org/10.1126/science.290.5492.721.
Mohamed Ibrahim N, Ramli R, Koya Kutty S, Shah SA. Earlier onset of motor complications in Parkinson’s patients with comorbid diabetes mellitus. Mov Disord. 2018;33:1967–8. https://doi.org/10.1002/mds.27526.
Li L-Y, Liu S-F, Zhuang J-L, Li M-M, Huang Z-P, Chen Y-H, et al. Recent research progress on metabolic syndrome and risk of Parkinson’s disease. Rev Neurosci. 2023;34:719–35. https://doi.org/10.1515/revneuro-2022-0093.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association. Harmonizing the metabolic syndrome: a joint interim statement of. Obes Circulation. 2009;120:1640–5. https://doi.org/10.1161/CIRCULATIONAHA.109.192644. World Heart Federation; International Atherosclerosis Society; and International Association for the Study of.
Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 2016;15:1257–72. https://doi.org/10.1016/S1474-4422(16)30230-7.
Rattan P, Penrice DD, Ahn JC, Ferrer A, Patnaik M, Shah VH, et al. Inverse Association of Telomere length with Liver Disease and Mortality in the US Population. Hepatol Commun. 2022;6:399–410. https://doi.org/10.1002/hep4.1803.
Austin PC, Jembere N, Chiu M. Propensity score matching and complex surveys. Stat Methods Med Res. 2018;27:1240–57. https://doi.org/10.1177/0962280216658920.
Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49:284–303. https://doi.org/10.1111/1475-6773.12090.
Lenis D, Nguyen TQ, Dong N, Stuart EA. It’s all about balance: propensity score matching in the context of complex survey data. Biostatistics. 2019;20:147–63. https://doi.org/10.1093/biostatistics/kxx063.
Souza APdaS, Barros WMA, Silva JML, Silva MRM, Silva ABJ, de Fernandes MS. Effect of metabolic syndrome on Parkinson’s Disease: a systematic review. Clin (Sao Paulo). 2021;76:e3379. https://doi.org/10.6061/clinics/2021/e3379.
Roh J-H, Lee S, Yoon J-H. Metabolic syndrome and Parkinson’s Disease incidence: a nationwide study using propensity score matching. Metab Syndr Relat Disord. 2021;19:1–7. https://doi.org/10.1089/met.2020.0060.
Nam GE, Kim SM, Han K, Kim NH, Chung HS, Kim JW, et al. Metabolic syndrome and risk of Parkinson disease: a nationwide cohort study. PLoS Med. 2018;15:e1002640. https://doi.org/10.1371/journal.pmed.1002640.
Park SH, Nam GE, Han K, Huh Y, Kim W, Lee M-K, et al. Association of dynamic changes in metabolic syndrome status with the risk of Parkinson’s Disease: a Nationwide Cohort Study. J Parkinsons Dis. 2021;11:1751–9. https://doi.org/10.3233/JPD-212589.
Peng Z, Zhou R, Liu D, Cui M, Yu K, Yang H, et al. Association between metabolic syndrome and mild Parkinsonian signs Progression in the Elderly. Front Aging Neurosci. 2021;13:722836. https://doi.org/10.3389/fnagi.2021.722836.
Meléndez-Flores JD, Castillo-Torres SA, Cerda-Contreras C, Chávez-Luévanos B, Estrada-Bellmann I. Clinical features of metabolic syndrome in patients with Parkinson’s disease. Rev Neurol. 2021;72:9–15. https://doi.org/10.33588/rn.7201.2020323.
Peng Z, Dong S, Tao Y, Huo Y, Zhou Z, Huang W, et al. Metabolic syndrome contributes to cognitive impairment in patients with Parkinson’s disease. Parkinsonism Relat Disord. 2018;55:68–74. https://doi.org/10.1016/j.parkreldis.2018.05.013.
Doiron M, Langlois M, Dupré N, Simard M. The influence of vascular risk factors on cognitive function in early Parkinson’s disease. Int J Geriatr Psychiatry. 2018;33:288–97. https://doi.org/10.1002/gps.4735.
Hu G, Antikainen R, Jousilahti P, Kivipelto M, Tuomilehto J. Total cholesterol and the risk of Parkinson disease. Neurology. 2008;70:1972–9. https://doi.org/10.1212/01.wnl.0000312511.62699.a8.
Aune D, Schlesinger S, Mahamat-Saleh Y, Zheng B, Udeh-Momoh CT, Middleton LT. Diabetes mellitus, prediabetes and the risk of Parkinson’s disease: a systematic review and meta-analysis of 15 cohort studies with 29.9 million participants and 86,345 cases. Eur J Epidemiol. 2023;38:591–604. https://doi.org/10.1007/s10654-023-00970-0.
Lin H-C, Tseng Y-F, Shen A-L, Chao JC-J, Hsu C-Y, Lin H-L. Association of Angiotensin receptor blockers with Incident Parkinson Disease in patients with hypertension: a retrospective cohort study. Am J Med. 2022;135:1001–7. https://doi.org/10.1016/j.amjmed.2022.04.029.
Tseng Y-F, Lin H-C, Chao JC-J, Hsu C-Y, Lin H-L. Calcium Channel blockers are associated with reduced risk of Parkinson’s disease in patients with hypertension: a population-based retrospective cohort study. J Neurol Sci. 2021;424:117412. https://doi.org/10.1016/j.jns.2021.117412.
Sääksjärvi K, Knekt P, Männistö S, Lyytinen J, Heliövaara M. Prospective study on the components of metabolic syndrome and the incidence of Parkinson’s disease. Parkinsonism Relat Disord. 2015;21:1148–55. https://doi.org/10.1016/j.parkreldis.2015.07.017.
Laudisio A, Lo Monaco MR, Vetrano DL, Pisciotta MS, Bentivoglio AR, Bernabei R, et al. Association of metabolic syndrome with falls in patients with Parkinson’s disease. Clin Nutr. 2017;36:559–63. https://doi.org/10.1016/j.clnu.2016.02.004.
Miyake Y, Tanaka K, Fukushima W, Sasaki S, Kiyohara C, Tsuboi Y, et al. Case-control study of risk of Parkinson’s disease in relation to hypertension, hypercholesterolemia, and diabetes in Japan. J Neurol Sci. 2010;293:82–6. https://doi.org/10.1016/j.jns.2010.03.002.
Portugal B, Artaud F, Domenighetti C, Roze E, Degaey I, Canonico M, et al. Body Mass Index, Abdominal Adiposity, and incidence of Parkinson Disease in French Women from the E3N cohort study. Neurology. 2023;100:e324–35. https://doi.org/10.1212/WNL.0000000000201468.
Jeong S-M, Han K, Kim D, Rhee SY, Jang W, Shin DW. Body mass index, diabetes, and the risk of Parkinson’s disease. Mov Disord. 2020;35:236–44. https://doi.org/10.1002/mds.27922.
Simon KC, Chen H, Schwarzschild M, Ascherio A. Hypertension, hypercholesterolemia, diabetes, and risk of Parkinson disease. Neurology. 2007;69:1688–95. https://doi.org/10.1212/01.wnl.0000271883.45010.8a.
Soni R, Shah J. Deciphering intertwined Molecular pathways underlying metabolic syndrome leading to Parkinson’s Disease. ACS Chem Neurosci. 2022;13:2240–51. https://doi.org/10.1021/acschemneuro.2c00165.
Cheong JLY, de Pablo-Fernandez E, Foltynie T, Noyce AJ. The Association between type 2 diabetes Mellitus and Parkinson’s Disease. J Parkinsons Dis. 2020;10:775–89. https://doi.org/10.3233/JPD-191900.
Zhang P, Tian B. Metabolic syndrome: an important risk factor for Parkinson’s disease. Oxid Med Cell Longev. 2014;2014:729194. https://doi.org/10.1155/2014/729194.
Mischley LK, Shankland E, Liu SZ, Bhayana S, Fox DJ, Marcinek DJ. ATP and NAD + Deficiency in Parkinson’s Disease. Nutrients. 2023;15:943. https://doi.org/10.3390/nu15040943.
Kullmann S, Heni M, Hallschmid M, Fritsche A, Preissl H, Häring H-U. Brain insulin resistance at the crossroads of metabolic and cognitive disorders in humans. Physiol Rev. 2016;96:1169–209. https://doi.org/10.1152/physrev.00032.2015.
Banks WA, Owen JB, Erickson MA. Insulin in the brain: there and back again. Pharmacol Ther. 2012;136:82–93. https://doi.org/10.1016/j.pharmthera.2012.07.006.
Chen W, Cai W, Hoover B, Kahn CR. Insulin action in the brain: cell types, circuits, and diseases. Trends Neurosci. 2022;45:384–400. https://doi.org/10.1016/j.tins.2022.03.001.
Pedrosa MA, Labandeira CM, Valenzuela R, Quijano A, Sanchez-Andrade M, Suarez-Quintanilla JA, et al. AT1 receptor autoantibodies mediate effects of metabolic syndrome on dopaminergic vulnerability. Brain Behav Immun. 2023;108:255–68. https://doi.org/10.1016/j.bbi.2022.12.009.
de Donato A, Buonincontri V, Borriello G, Martinelli G, Mone P. The dopamine system: insights between kidney and brain. Kidney Blood Press Res. 2022;47:493–505. https://doi.org/10.1159/000522132.
Jones KT, Woods C, Zhen J, Antonio T, Carr KD, Reith MEA. Effects of diet and insulin on dopamine transporter activity and expression in rat caudate-putamen, nucleus accumbens, and midbrain. J Neurochem. 2017;140:728–40. https://doi.org/10.1111/jnc.13930.
Santisteban MM, Iadecola C, Carnevale D, Hypertension. Neurovascular dysfunction, and cognitive impairment. Hypertension. 2023;80:22–34. https://doi.org/10.1161/HYPERTENSIONAHA.122.18085.
Iadecola C, Gottesman RF. Neurovascular and cognitive dysfunction in hypertension. Circ Res. 2019;124:1025–44. https://doi.org/10.1161/CIRCRESAHA.118.313260.
Alrouji M, Al-Kuraishy HM, Al-Mahammadawy A-KAA, Al-Gareeb AI, Saad HM, Batiha GE-S. The potential role of cholesterol in Parkinson’s disease neuropathology: perpetrator or victim. Neurol Sci. 2023;44:3781–94. https://doi.org/10.1007/s10072-023-06926-2.
Acknowledgements
The authors would like to express the gratitude to the NHANES database for providing publicly available data and Zhang Jing (Second Department of Infectious Disease, Shanghai Fifth People’s Hospital, Fudan University) for his work on the NHANES database. His outstanding work, nhanesR package and webpage, makes it easier for us to explore NHANES database. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
No explicit funding support from any public, private, or nonprofit organizations.
Author information
Authors and Affiliations
Contributions
Yue Shi: conceptualization, methodology, formal analysis, data curation, and writing-original draft preparation; XueYi Zhang: data curation, writing-original draft preparation, and visualization; Yue Feng and ZongXiang Yue: supervision, and writing-review and editing. All authors contributed to the article and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
Study protocols for NHANES were approved by the NCHS ethnics review board (https://www.cdc.gov/nchs/nhanes/irba98.htm).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conficts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, Y., Zhang, X., Feng, Y. et al. Association of metabolic syndrome and its components with Parkinson’s disease: a cross-sectional study. BMC Endocr Disord 24, 92 (2024). https://doi.org/10.1186/s12902-024-01623-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01623-3