Abstract
Background
Primary hyperparathyroidism which is rare in adolescents presents commonly with non-specific symptoms and systemic complaints. Though there are few reported cases of genu valgus, genu valgus progressing to extensive bone disease despite mildly elevated calcium had not been reported before.
Case presentation
A 12-year-old male had been evaluated for bilateral (left > right) genu valgus and short stature. Serum calcium and phosphate levels had been normal. X-ray of the femora and pelvic bones had not shown additional abnormalities. Valgus deformity progressed despite left femoral plating, and a left distal femoral medial closed wedge osteotomy had been performed at 15 years. Plain imaging at that time had shown localised osteopaenia. At the age of 17 years, he developed multiple fragility fractures of his left hip rendering him wheelchair-bound. Further evaluation revealed a serum PTH level of 2571 (10–65) pg/mL with calcium of 2.82 (2.2–2.6) mmol/L and inorganic phosphate of 1.7 (2.2–4.7) mg/dL. The lumbar spine DXA scan showed a Z-score of -5.8. A left parathyroid adenoma was localised and there was evidence of hyperparathyroid bone disease including brown tumours. He underwent left parathyroidectomy and left thyroid lobectomy after which his PTH level dropped to 4.03 pg/mL. He developed hypocalcaemia which was managed successfully with calcium and alfacalcidol replacement.
Conclusions
Primary hyperparathyroidism can present with genu valgus in adolescents. Initial normocalcaemia which could be due to concomitant vitamin D deficiency could mask this leading to delayed diagnosis until severe irreversible bone disease ensues.
Similar content being viewed by others
Background
Primary hyperparathyroidism in adolescents is rare compared to that of adults [1]. While it is commonly recognised in adults with screening during the asymptomatic period, adolescents are commonly diagnosed when they are symptomatic [2, 3]. However, symptoms are commonly generalised and non-specific due to hypercalcaemia. These include bone pain, asthenia, weight loss, abdominal pain, vomiting and lethargy [1, 2]. In some parts of the world, bone disease including fractures and deformities as well as renal complications have been commonly reported even in younger patients [1, 4, 5].
Though bone disease had been described as a presenting feature of primary hyperparathyroidism in adolescents, it is extremely uncommon for it to present with genu valgus. In fact, primary hyperparathyroidism is not considered in the diagnostic workup of an adolescent with genu valgus [6]. There are several case reports of adolescents with primary hyperparathyroidism presenting with genu valgus. However, fractures have not been a common manifestation in them, and they were noted to have hypercalcaemia at the time of presentation. We report an adolescent who initially presented with genu valgus and normocalcaemia progressing to severe bone disease with multiple fractures despite having mild hypercalcaemia.
Case presentation
An 18-year-old Sri Lankan male was referred for evaluation of short stature, multiple bone deformities and fragility fractures for six years.
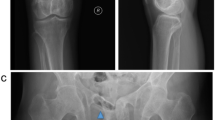
He had been well until the age of 12 years with uncomplicated birth and childhood. At the age of 12 years, left and subsequently, right genu valgus and short stature were noted. He did not have any other problems during the initial presentation. The documented examination has not revealed any other abnormalities. Standing X-rays of bilateral tibia/ femora and pelvic bones (AP view) have shown bilateral asymmetric genu valgus, but no reduction of bone density or abnormalities suggestive of rickets in epiphyseal plates (Fig. 1 A).
Standing X-rays of bilateral tibia/ femora and pelvic bones (AP view) at the presentation showing bilateral asymmetric genu valgus, but no reduction of bone density or abnormalities suggestive of rickets in epiphyseal plates (A). Follow-up x-ray of the same projection one year later demonstrating corrective left distal femoral osteotomy with internal fixation screws on the medial aspect of the distal femoral epiphysis and metaphysis. A more pronounced deformity is evident compared to the prior X-ray causing a mild pelvic tilt in the standing position (B)
Blood investigations at the initial presentation revealed an ionized calcium of 1.4 mmol/L (1.2–1.4 mmol/L) and the inorganic phosphate level was 1.1 mmol/L (0.95–1.75 mmol/L, age-based for 12–15 years). Serum creatinine, haemoglobin, alanine transaminase and aspartate transaminase were within the normal range. Serum vitamin D or parathyroid hormone levels had not been performed.
He underwent left femoral plating, but valgus deformity progressed over time. X-ray of the same projection done one year later demonstrated corrective left distal femoral osteotomy with internal fixation screws on the medial aspect of the distal femoral epiphysis and metaphysis. However, the deformity was more pronounced compared to the prior X-ray causing a mild pelvic tilt in the standing position (Fig. 1B).
Three years later, at the age of 15 years, he sought advice from another unit for the persistent genu valgus, where he underwent left distal femoral medial closed wedge osteotomy. Post-operative x-ray of the bilateral knee joints revealed evidence of the second osteotomy with internal fixation screws in situ. Local osteopaenia was noted around the internal fixation screws. Some callus formation is seen laterally around the distal femoral metaphysis/epiphysis (Fig. 2). He was prescribed vitamin D 1000 IU daily which was continued until the current presentation.
Post-operative x-ray of bilateral knee joints after the left distal femoral medial closed wedge osteotomy showing evidence of the second osteotomy with internal fixation screws in situ. Local osteopaenia is observed around the internal fixation screws. Some callus formation is seen laterally around the distal femoral metaphysis/epiphysis
Two years later, at the age of 17 years, he developed a left femoral shaft fracture while standing up. Subsequent evaluation revealed multiple femoral fractures and he was unable to weight-bear since then. He was mobilised in a wheelchair since then. He has had normal puberty and intellectual development. He had been on a balanced non-vegetarian diet and there were no features of any other chronic illnesses. He was a product of non-consanguineous parents. Family history did not reveal any skeletal diseases or tumour syndromes.
His height was 147.5 cm. There was kyphosis and genu valgus. The examination was otherwise unremarkable.
Generalised osteopenia and bilateral femoral neck fractures were noted in the x-ray of bilateral hip joints (Fig. 3A). Left femur x-ray showed marked osteopaenia, diffuse ground glass density in the medullary cavity of the femur and pathological fractures with marked deformities (Fig. 3B). X-rays of the hands showed fully fused epiphyses, terminal tufting more marked in bilateral 2nd and 3rd fingers and osteopenia in the middle and distal phalanges of all the fingers as well as the distal aspect of the proximal phalanges bilaterally. There was no definite subperiosteal resorption. Early Madelung deformity was seen but, the length of the metacarpals was normal. There was no evidence of rickets (Fig. 4). Laboratory investigations during this presentation are summarised in Table 1.
X-rays of the hands showed fully fused epiphyses, terminal tufting more marked in bilateral 2nd and 3rd fingers and osteopenia in the middle and distal phalanges of all the fingers as well as the distal aspect of the proximal phalanges bilaterally. There was no definite subperiosteal resorption. Early Madelung deformity was seen but, the length of the metacarpals was normal. There was no evidence of rickets
Laboratory investigations were in favour of primary hyperparathyroidism. The ultrasound scan of the neck showed a large well-defined heterogeneous hyperechoic lesion in the lower and mid portion of L/thyroid measuring 51 × 30 × 16 mm. Contrast-enhanced CT of the neck confirmed a well-defined rounded soft tissue density with moderate heterogeneous enhancement along the posterior aspect of the L/lobe of the thyroid. This was suggestive of a parathyroid adenoma. Additionally, diffusely scattered lytic bone lesions with associated bone expansion were noted in the imaged axial skeleton and upper humeri suggestive of brown tumours of hyperparathyroid bone disease (Fig. 5). The PTH level from the aspirate of guided FNAC was > 3000 pg/mL further confirming localisation.
DXA scan of the lumbar spine suggested very low bone density with a BMD of 0.122 g/cm2 and a Z-score of -5.8. There were no calculi or nephrocalcinosis in the ultrasound scan kidney-ureter-bladder.
He underwent left parathyroidectomy and left thyroid lobectomy since there was a concern about possible parathyroid malignancy peri-operatively. A nodular, capsulated and brownish parathyroid measuring 60 × 30 × 24 mm was removed. Histology confirmed a well-circumscribed parathyroid adenoma with a thin fibrous capsule. There were no bizarre cells or increased mitoses. One week after the surgery, the PTH level dropped to 4.03 pg/mL. He was discharged home on calcium carbonate containing elemental calcium of 1000 mg three times daily and alfacalcidol one microgram twice daily. Two months after the surgery, his alkaline phosphatase was 1811 IU/L and calcium and phosphate were within the normal range. His replacement doses were gradually decreased to calcium carbonate containing elemental calcium of 500 mg twice daily and alfacalcidol 0.5 µg twice daily six months after surgery. Currently, he is feeling well and has been followed up with a plan for future orthopaedic interventions. To date, he is mobilised with the help of a wheelchair.
The timeline of events is summarised in Table 2.
Discussion and conclusions
Our patient initially presented with bilateral genu valgus and short stature with no other obvious abnormalities in physical examination and biochemistry. Subsequently, it progressed to severe disease with very low bone density and multiple fragility fractures. Yet, the calcium level was only mildly elevated. This course of the illness has not been reported before.
We performed a systematic literature review to identify reports of patients with primary hyperparathyroidism presenting with genu valgus. The search was done in PubMed on 1st September 2022 with the search strategy as follows; (hyperparathyroidism[Title/Abstract]) AND (genu valg*[Title/Abstract] OR knock knee[Title/Abstract]). This provided 21 results. A similar search in Google Scholar obtained 9 results. After removing the duplicates, 27 abstracts were reviewed. Nineteen abstracts were selected to review full-text from which four were removed (English full-text not available- 3, duplicate—1) and fifteen were included. With eight additional records identified through cross-referencing, a total of 23 reports were included in the literature review [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29] (Table 3).
Thirty patients have been reported (16 females). The median age at presentation was 13 years (Age at diagnosis taken as age at presentation for three patients). One patient had low serum calcium levels [10], whereas all the other patients were hypercalcaemic. All patients with reported histology have had parathyroid adenomas. In addition to genu valgus, 12 had features of rickets clinically or radiologically. Osteopaenia was commonly observed in radiological studies. Sixteen patients were reported to have radiological features characteristic of hyperparathyroid bone disease including cysts, brown tumours and subperiosteal resorption. Slipped upper femoral epiphyses were also noted in some.
Fractures have been observed only in two patients. One was a 17-year-old boy who initially presented at 14 years of age with lower limb pain and bilateral genu valgus [11]. At the diagnosis, his corrected calcium was 3.02 mmol/L. DXA scan showed BMD Z scores of -5 at the hip and -4.9 at the spine. He was found to have previously unrecognised bilateral femur shaft fractures which have partially healed. The other patient was a 15-year-old male who presented with bone pains and a right tibial shaft fracture [29]. However, this boy had been treated for right tibial osteomyelitis which also might have contributed to this complication. His calcium was 12 mg/dL at the time of diagnosis. It was notable both these boys had features of rickets, but not hyperparathyroid bone disease.
Our patient’s clinical picture is distinct from all the patients reported above since he initially presented with bilateral genu valgus and then it progressed to severe bone disease with very low bone density and fragility fractures. He was found to have features of hyperparathyroid bone disease, but no definite evidence of rickets. Though his PTH level was grossly elevated, there was only mild hypercalcaemia. In fact, his calcium at the initial presentation was normal. Vitamin D deficiency could have masked hypercalcemia at the initial presentation. However, his vitamin D level was 24.96 ng/mL at the time of endocrine evaluation which was only slightly below the reference range. Calcium: phosphorous ratio could have been a useful tool at the initial evaluation since his calcium was at the upper end of the reference range and phosphate was at the lower half of the reference range for his age. This index has emerged as a reliable tool for identifying patients with primary hyperparathyroidism [30]. Age-specific reference ranges are needed in interpreting phosphate levels and calcium: phosphate ratio. The presence of osteopaenia in subsequent plain radiographs would have been another clue to an alternative diagnosis.
The mechanism of genu valgus in primary hyperparathyroidism is not well established. However, one plausible mechanism is the direct effect of increased parathyroid hormone levels on the growth plate during puberty [18]. It could be partly due to the concomitant vitamin D deficiency. Notably, most reported cases are from South Asian populations where vitamin D deficiency is more prevalent. When undiagnosed primary hyperparathyroidism continues as in our patient and the patient reported by Paruk et al., severe bone disease establishes with reduced bone mineral density and fractures. Severe hyperparathyroid bone disease was also evident in our patient further confirming the severe skeletal involvement of the disease.
This case report highlights the importance of close surveillance for underlying metabolic diseases in patients presenting with genu valgus. Though the initial calcium was normal, a high index of suspicion is warranted particularly in the setting of possible concomitant vitamin D deficiency and progressing disease with osteopaenia in the plain radiograph.
Availability of data and materials
Not applicable.
References
Roizen J, Levine MA. Primary hyperparathyroidism in children and adolescents. J Chin Med Assoc. 2012;75(9):425–34.
el Allali Y, Hermetet C, Bacchetta J, Amouroux C, Rothenbuhler A, Porquet-Bordes V, et al. Presenting features and molecular genetics of primary hyperparathyroidism in the paediatric population. Eur J Endocrinol. 2021;184(2):343–51.
Pashtan I, Grogan RH, Kaplan SP, Devon K, Angelos P, Liu D, et al. Primary hyperparathyroidism in adolescents: The same but different. Pediatr Surg Int. 2013;29(3):275–9.
George J, Acharya S v., Bandgar TR, Menon PS, Shah NS. Primary hyperparathyroidism in children and adolescents. Indian J Pediatr. 2010; 77(2):175–8.
Shah VN, Bhadada SK, Bhansali A, Behera A, Mittal BR, Bhavin V. Influence of age and gender on presentation of symptomatic primary hyperparathyroidism. J Postgrad Med. 2012;58(2):107.
White GR, Mencio GA. Genu valgum in children: diagnostic and therapeutic alternatives. J Am Acad Orthop Surg. 1995;3(5):275–83.
Dikova MI, Petkova B, Alexiev V. Skeletal deformity in children with primary hyperparathyroidism. Acta Chir Orthop Traumatol Cech. 2021;88(5):375–8.
Lee SP, Chai ST, Loh LT, Ali NM. Bilateral genu valgum in an adolescent with primary hyperparathyroidism: a case report and review of literature. J ASEAN Fed Endocr Soc. 2020;35(2):220–3.
Yanrismet Y, Tridjaja B. Genu valgum as a rare clinical manifestation in child with primary hyperparathyroidism: a case report. Arch Dis Child. 2019;104(Suppl 3):A276–A276.
Rao KS, Agarwal P, Reddy J. Parathyroid adenoma presenting as genu valgum in a child: A rare case report. Int J Surg Case Rep. 2019;59:27–30.
Paruk IM, Pirie FJ, Motala AA. Rickets mimicker: a report of two cases of primary hyperparathyroidism in adolescence. J Endocrinol Metabol Diabetes South Africa. 2019;24(1):23–7.
Khan KA, Qureshi SU. Primary hyperparathyroidism masquerading as Rickets. J Coll Physicians Surg Pak. 2019;29(9):891–4.
George G, Raizada N, Jabbar P, Chellamma J, Nair A. Slipped capital femoral epiphysis in primary hyperparathyroidism - case report with literature review. Indian J Endocrinol Metab. 2019;23(4):491.
Pradhan R, Agarwal A, Gupta SK. PHPT masquerading as rickets in children and presenting with rare skeletal manifestations: report of three cases and review of literature. Indian J Endocrinol Metab. 2018;22(5):705–9.
Arambewela MH, Liyanarachchi KD, Somasundaram NP, Pallewatte AS, Punchihewa GL. Case report: Rare skeletal manifestations in a child with primary hyperparathyroidism. BMC Endocr Disord. 2017;17(1):1–6.
Zil-E-Ali Ahsan, Latif Aiza, Rashid Anam, Malik Asim, Khan Haseeb Ahmed. Presentation of parathyroid adenoma with genu valgum and thoracic deformities - PubMed. J Pak Med Assoc. 2016;66(1):101–3.
Sharma S, Kumar S. Bilateral genu valgum: an unusual presentation of juvenile primary hyperparathyroidism. Oxf Med Case Reports. 2016;2016(7):141–3.
Ramkumar S, Kandasamy Devasenathipathy, MK Vijay, Tripathi M, VP Jyotsna. Genu valgum and primary hyperparathyroidism in children. Int J Case Rep Images. 2014;5(6):401–7.
Ratnasingam J, Tan ATB, Vethakkan SR, Paramasivam SS, Ibrahim L, Lim LL, et al. Primary hyperparathyroidism: a rare cause of genu valgus in adolescence. J Clin Endocrinol Metab. 2013;98(3):869–70.
Dutta D, Kumar M, Das RN, Datta S, Biswas D, Ghosh S, et al. Primary hyperparathyroidism masquerading as rickets: diagnostic challenge and treatment outcomes. J Clin Res Pediatr Endocrinol. 2013;5(4):266.
Walczyk A, Szalecki M, Kowalska A. Primary hyperparathyroidism: A rare endocrinopathy in children. Two case reports Endokrynol Pol. 2011;62(4):346–50.
Harman CR, van Heerden JA, Farley DR, Grant CS, Thompson GB, Curlee K. Sporadic primary hyperparathyroidism in young patients: a separate disease entity? Arch Surg. 1999;134(6):651–6.
Menon PSN, Madhavi N, Mukhopadhyaya S, Padhy AK, Bal CS, Sharma LK. Primary hyperparathyroidism in a 14 year old girl presenting with bone deformities. J Paediatr Child Health. 1994;30(5):441–3.
Kauffmann C, Leroy B, Sinnassamy P, Carlioz H, Gruner M, Bensman A. A rare cause of bone pain in children: primary hyperparathyroidism caused by adenoma. Arch Fr Pediatr. 1993;50(9):771–4.
Rapaport D, Ziv Y, Rubin M, Huminer D, Dintsman M. Primary hyperparathyroidism in children. J Pediatr Surg. 1986;21(5):395–7.
Lloyd HM, Aitken RE, Ferrier TM. Primary hyperparathyroidism resembling rickets of late onset. Br Med J. 1965;2(5466):853–6.
Balch HE, Spiegel EH, Upton AL, Kinsell LW. Hyperparathyroidism: report of 2 cases with some relatively unusual manifestations. J Clin Endocrinol Metab. 1953;13(6):733–8.
Mcclure RD, Lam CR. End-Results in the Treatment of Hyperparathyroidism. Ann Surg. 1945;121(4):454–69.
Ganie MA, Raizada N, Chawla H, Singh AK, Aggarwala S, Bal CS. Primary hyperparathyroidism may masquerade as rickets-osteomalacia in Vitamin D replete children. J Pediatr Endocrinol Metab. 2016;29(10):1207–13.
Madeo B, De Vincentis S, Repaci A, Altieri P, Vicennati V, Kara E, et al. The calcium-to-phosphorous (Ca/P) ratio in the diagnosis of primary hyperparathyroidism and hypoparathyroidism: a multicentric study. Endocrine. 2020;68:679–87.
Acknowledgements
The authors would like to acknowledge the patient who gave consent to publish this case report.
Funding
The authors did not receive funding for the specific case report and patient care was provided as a part of employment at the University Hospital, Kotelawala Defence University.
Author information
Authors and Affiliations
Contributions
All authors provided clinical care to the patient. NLdeS wrote the initial manuscript. MDJ, WKCS, RP and CK edited the manuscript. All authors read and agreed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
All the authors declare that there is no conflict of interest regarding the publication of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Silva, N.L., Jayalath, M.D., Sampath, W.K.C. et al. Primary hyperparathyroidism in an adolescent presenting with genu valgus progressing to extensive bone disease; a case report. BMC Endocr Disord 23, 71 (2023). https://doi.org/10.1186/s12902-023-01328-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01328-z