Abstract
Purpose
The diagnosis of primary hyperparathyroidism (PHPT) and chronic hypoparathyroidism (HypoPT) is still challenging, especially in patients asymptomatic or with non-classical phenotypes and for physicians not skilled in calcium-phosphorous (Ca–P) disorders. The serum calcium/phosphorous (Ca/P) ratio has been proposed as accurate index to identify PHPT, while it has never been tested in HypoPT. The aim of this study is to investigate the diagnostic power of the serum Ca/P ratio in the diagnosis of primary parathyroid dysfunctions (both PHPT and HypoPT) in a large series of data.
Methods
A multicentric, retrospective, cross-sectional study (ClinicalTrials.gov: NCT03747029) was carried out including 432 PHPT patients and 217 HypoPT patients compared with 389 controls. Serum Ca, P, creatinine, parathyroid hormone and 25OH-vitamin D were collected. Serum Ca and P were expressed in mmol/L. Ca/P diagnostic performance was evaluated by receiver operating characteristic (ROC) curve, sensitivity, specificity and accuracy.
Results
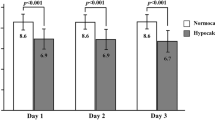
The Ca/P ratio was significantly higher in PHPT and lower in HypoPT patients than controls (p < 0.0001). At ROC curve analysis, the Ca/P ratio above 2.55 was defined to identify PHPT patients (sensitivity 85.7%, specificity 85.3%) and below 1.78 to identify HypoPT patients (sensitivity 88.2%, specificity 87.9%).
Conclusions
The Ca/P ratio is a highly accurate index to identify PHPT when Ca/P is above 2.55 and HypoPT when it is below 1.78. These results demonstrate the reliability of this index to rule in/out primary parathyroid dysfunctions and remark the importance of measuring serum P in clinical practice.



Similar content being viewed by others
References
J.L. Shaker, L. Deftos. Calcium and Phosphate Homeostasis. [Updated 2018 Jan 19]. In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000
M.D. Walker, S.J. Silverberg, Primary hyperparathyroidism. Nat. Rev. Endocrinol. 14, 115–125 (2018)
S. Minisola, L. Gianotti, S. Bhadada, S.J. Silverberg, Classical complications of primary hyperparathyroidism. Best Pract. Res. Clin. Endocrinol. Metab. 32, 791–803 (2018)
M. Peacock, Calcium metabolism in health and disease. Clin. J. Am. Soc. Nephrol. 5(Suppl 1), S23–S30 (2010)
B. Madeo, S. De Vincentis, E. Kara, F. Vescini, T. Trenti, et al. Reliability of calcium-phosphorus (Ca/P) ratio as a new, accurate and inexpensive tool inthe diagnosis of some Ca-P disorders. J. Endocrinol. Investig. 42, 1041–1049 (2019)
M. Mannstadt, J.P. Bilezikian, R.V. Thakker, F.M. Hannan, B.L. Clarke et al. Hypoparathyroidism. Nat. Rev. Dis. Prim. 3, 17055 (2017)
B. Madeo, E. Kara, K. Cioni, S. Vezzani, T. Trenti et al. Serum calcium to phosphorous (Ca/P) ratio is a simple, inexpensive, and accurate tool in the diagnosis of primary hyperparathyroidism. JBMR 2, 109–117 (2018)
J.P. Bilezikian, L. Bandeira, A. Khan, N.E. Cusano, Hyperparathyroidism. Lancet 391, 168–178 (2018)
S.J. Silverberg, J.P. Bilezikian, “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J. Clin. Endocrinol. Metab. 88, 5348–5352 (2003)
A.N. Hollenberg, A. Arnold, Hypercalcemia with low-normal serum intact PTH: a novel presentation of primary hyperparathyroidism. Am. J. Med. 91, 547–548 (1991)
S. Corbetta, Normocalcemic hyperparathyroidism. Front. Horm. Res. 51, 23–39 (2019)
W.D. Fraser, Hyperparathyroidism. Lancet 374, 145–158 (2009)
C. Marcocci, F. Cetani, Clinical practice. Primary hyperparathyroidism. N. Engl. J. Med. 365, 2389–2397 (2011)
J.P. Bilezikian, M.L. Brandi, R. Eastell, S.J. Silverberg, R. Udelsman et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J. Clin. Endocrinol. Metab. 99, 3561–3569 (2014)
M.M. Tuna, M. Caliskan, M. Unal, T. Demirci, B.A. Dogan et al. Normocalcemic hyperparathyroidism is associated with complications similar to those of hypercalcemic hyperparathyroidism. J. Bone Min. Metab. 34, 331–335 (2016)
D. Shoback, Clinical practice. Hypoparathyroidism. N. Engl. J. Med. 359, 391–403 (2008)
M.L. Brandi, J.P. Bilezikian, D. Shoback, R. Bouillon, B.L. Clarke et al. Management of hypoparathyroidism: summary statement and guidelines. J. Clin. Endocrinol. Metab. 101, 2273–2283 (2016)
J. Bollerslev, L. Rejnmark, C. Marcocci, D.M. Shoback, A. Sitges-Serra et al. European Society of Endocrinology Clinical Guideline: treatment of chronic hypoparathyroidism in adults. Eur. J. Endocrinol. 173, G1–G20 (2015)
D.M. Shoback, J.P. Bilezikian, A.G. Costa, D. Dempster, H. Dralle et al. Presentation of hypoparathyroidism: etiologies and clinical features. J. Clin. Endocrinol. Metab. 101, 2300–2312 (2016)
N.E. Cusano, J.P. Bilezikian, Signs and symptoms of hypoparathyroidism. Endocrinol. Metab. Clin. N. Am. 47, 759–770 (2018)
L. Cianferotti, G. Marcucci, M.L. Brandi, Causes and pathophysiology of hypoparathyroidism. Best Pract. Res. Clin. Endocrinol. Metab. 32, 909–925 (2018)
E.A. Alore, J.W. Suliburk, D.J. Ramsey, N.N. Massarweh, C.J. Balentine, et al. Diagnosis and Management of Primary Hyperparathyroidism Across theVeterans Affairs Health Care System. JAMA Intern Med. 179, 1220–1227 (2019)
J. Bollerslev, C. Schalin-Jantti, L. Rejnmark, H. Siggelkow, H. Morreau et al. Management of endocrine disease: unmet therapeutic, educational and scientific needs in parathyroid disorders. Eur. J. Endocrinol. 181, P1–p19 (2019)
M. Pawlowska, N.E. Cusano, An overview of normocalcemic primary hyperparathyroidism. Curr. Opin. Endocrinol. Diabetes Obes. 22, 413–421 (2015)
N.E. Cusano, C. Cipriani, J.P. Bilezikian, Management of normocalcemic primary hyperparathyroidism. Best Pract. Res. Clin. Endocrinol. Metab. 32, 837–845 (2018)
H. Lowe, D.J. McMahon, M.R. Rubin, J.P. Bilezikian, S.J. Silverberg, Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J. Clin. Endocrinol. Metab. 92, 3001–3005 (2007)
L. Underbjerg, T. Sikjaer, L. Rejnmark, Long-term complications in patients with hypoparathyroidism evaluated by biochemical findings: a case-control study. J. Bone Min. Res. 33, 822–831 (2018)
M.C. Astor, K. Lovas, A. Debowska, E.F. Eriksen, J.A. Evang et al. Epidemiology and health-related quality of life in hypoparathyroidism in Norway. J. Clin. Endocrinol. Metab. 101, 3045–3053 (2016)
M.R. Rubin, Skeletal manifestations of hypoparathyroidism. Bone 120, 548–555 (2019)
B.L. Clarke, Epidemiology and complications of hypoparathyroidism. Endocrinol. Metab. Clin. N. Am. 47, 771–782 (2018)
I.H. de Boer, T.C. Rue, B. Kestenbaum, Serum phosphorus concentrations in the third National Health and Nutrition Examination Survey (NHANES III). Am. J. Kidney Dis. 53, 399–407 (2009)
W.C. O’Neill, The fallacy of the calcium-phosphorus product. Kidney Int. 72, 792–796 (2007)
Acknowledgements
The authors thank Prof. Paola Ugolini, Department of Romance Languages, SUNY Buffalo, NY, USA, for having proofread the manuscript and Dr Shaniko Kaleci, Department of Department of Diagnostic Medicine, Clinics and Public Health, Azienda Ospedaliero-Universitaria of Modena, Italy, for her contribution in reviewing statistics and study design.
Author contributions
All authors contributed to the study conception and data collection. Analysis were performed by B.M., S.D.V. and V.R. The first draft of the manuscript was written by B.M. and V.R. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board approved the protocol study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Madeo, B., De Vincentis, S., Repaci, A. et al. The calcium-to-phosphorous (Ca/P) ratio in the diagnosis of primary hyperparathyroidism and hypoparathyroidism: a multicentric study. Endocrine 68, 679–687 (2020). https://doi.org/10.1007/s12020-020-02276-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02276-7