Abstract
Aims
To describe clinic management and referral pathways among adults with type 1 diabetes (T1D) aged > 25 years attending a public outpatient diabetes service.
Methods
Retrospective cohort study of people with T1D aged > 25 years seen by endocrinologists in one Australian urban public outpatient in 2017. Electronic and paper medical records were reviewed using a dataset adapted from the UK National Institute for Health and Care Excellence 2015 guidelines.
Results
Among the 111 people with T1D (mean age 41 ± 13 years, 55% men, mean body mass index 27.1 ± 5.6 kg/m2), mean HbA1c was 8.1 ± 1.9% (66 ± 19 mmol/mol) (lower than the Australian National Diabetes Audit: 8.5%/69 mmol/mol) with 25.5% meeting the guideline target of < 53 mmol/mol (7.0%). Most people had seen a diabetes educator (80.2%) or dietitian (73.0%) and had complication screening. Complication rates were high (nephropathy 20.4%, retinopathy 27.4%, peripheral neuropathy 30.1%, ischaemic heart disease/acute infarction 10.5%). Overall, 27% of referrals occurred following an acute inpatient admission or emergency department presentation and 13% for management of diabetes in pregnancy.
Conclusions
A high proportion of people with T1D accessed public specialist care either during pregnancy or after a largely avoidable acute glycaemia-related hospital presentation. Subsequent care was in line with national specialist standards. This area has a “wait for acute event” rather than “complication prevention” model of care, associated with under-referral to the local multidisciplinary specialist service. Understanding how widespread this model of care is, and ways to reduce its prevalence, are urgently required.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Type 1 diabetes (T1D) is a lifelong autoimmune condition which requires long-term specialist team involvement [1]. The condition is associated with a significant increase in morbidity and mortality, with an estimated loss in life expectancy at birth of 12.2 years compared with the general population [2]. Individuals with T1D are admitted to hospital more frequently than those without diabetes including for both diabetes (e.g. diabetic ketoacidosis acidosis (DKA), renal disease) and non-diabetes (e.g. infections) related conditions [3]. This poses a considerable financial burden on the individual and healthcare system.
With good self-management and quality care (including structured diabetes education) much of the acute hospital and emergency department (ED) attendance related to hyper- and hypoglycaemia can be avoided [4, 5]. Long term hyperglycaemia related complications can be prevented by intensive monitoring and control of glycaemia by multidisciplinary teams [3, 4]. The risk of these macrovascular and microvascular complications can be further reduced through blood pressure and lipid management [6,7,8,9]. Such treatment standards have been defined by guidelines for the management of T1D [10, 11]. These guidelines emphasise the importance of effective self-management and patient education in achieving treatment targets, as well as regular complication screening as a means of secondary prevention of complications [1].
In Australia, the 2017–18 Australian National Diabetes Audit (ANDA) provides the most recent data on the current quality of care for all adults with T1D in Australia [12, 13]. They reported a national mean glycated haemoglobin (HbA1c) for people > 18 years of 8.5% (69.4 mmol/mol). Several studies of individual Australian young adult/transition clinics have described the challenges of managing hyperglycaemia among young adults aged < 25 years [14, 15]. However, few studies have looked explicitly at those beyond the young adult years in Australia, investigating what happens to such people after the additional issues for many young adults have “settled down” and maturity is well in place, or among those diagnosed after the age of 25 years [16, 17].
The aim of this study was to describe the outpatient management of T1D adults aged > 25 years at a public diabetes service and to assess how this relates to Australian population-based data, national and international guidelines. A prior audit among young adults had shown a high rate of readmissions for DKA [14], and hence we were particularly interested in hospital admission rates to provide an objective measure of the effectiveness of the management programs.
Methods
This was a retrospective audit of people with T1D aged > 25 years who saw an endocrinologist in the adult multidisciplinary diabetes clinics (also attended by a diabetes educator and diabetes dietitian) at Campbelltown Hospital, New South Wales between 1/1/2017 and 31/12/2017. The age threshold was chosen as those aged up to 25 years are seen within the paediatric (0–18 years) and transition (18–25 years) diabetes services. Individuals were identified through the endocrinologist, educator and dietitian patient records which were kept separately. People with latent autoimmune diabetes in adults (LADA) and type 2 diabetes were excluded. Pregnant women were included in this study to match their inclusion in the national audit. HbA1c, blood pressure and body mass index (BMI) were, however, reported for both the whole study population and with pregnant women excluded as targets vary in pregnancy. Electronic and archived (paper) medical records were reviewed by SP/CF. The clinic data collection tool was based upon the UK National Institute for Health and Care Excellence (NICE) T1D audit tool [11] adapted for local use. The most recent weight, body mass index and blood pressure were recorded. Data relating to Emergency Department (ED) presentations and hospital admissions between 2010 and 2017 were collected from the electronic records. Diabetes related admissions were defined as those for an acute glycaemic event (e.g. DKA), ischaemic heart disease, cerebrovascular disease, peripheral vascular disease, diabetic foot disease, nephropathy, depression and/or infection. Non-diabetes related admissions were defined as admissions unrelated to acute or chronic complications of diabetes. Attendance at the structured education program, Dose Adjustment for Normal Eating (OzDAFNE), was recorded following introduction into the service in 2016. Two courses had been rolled out by the time of data collection. The data were collated into an Excel spreadsheet, and subsequently coded and transferred to IBM SPSS. The proportion of the population seen in the clinic catchment was calculated from the local government agency T1D data in the National Diabetes Services Scheme (NDSS) Diabetes map (https://map.ndss.com.au/#!/: updated January 2019). Comparison was made with guideline recommendations and national [12, 13, 16] population-based reports. International reports were used where national data were lacking [18, 19]. Care standards (e.g. treatment targets and complication screening) were based on the most recent Australian guidelines available at the time of the audit [10]. No lipid targets were specified in the T1D guidelines so type 2 diabetes guidelines were used [20].
Data were analysed using IBM SPSS Statistics Software, Version 25. Frequencies and percentages are shown for categorical variables, with mean ± standard deviation (SD) or median (range) shown for continuous variables. Pearson chi-squared tests and one-way analysis of variance (ANOVA) were performed to compare categorical and continuous characteristics between groups. Statistical significance was defined as p-value < 0.05 and 95% confidence intervals were used.
Ethics
The project was approved as a Quality Improvement Project by the Campbelltown Hospital Quality and Safety Office, under the ethical framework overseen by the South Western Sydney Local Health District Human Research Ethics Committee (SWSLHD HREC) (CT01_2017, 1/07/2017).
Results
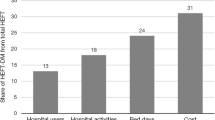
Figure 1 shows the source of the 111 people with T1D who had seen an endocrinologist. Based on the NDSS diabetes map, 137/1330 (10.3%) of the catchment T1D population were seen by the service. Figure 1 also shows that the majority of people were referred to the clinic from the emergency department (27%), after diagnosis in the hospital (21%), once pregnant by the obstetricians (13%) or from the hospital transition clinic (6%). The others were mainly referred by the general practitioner (GP) (24%). Excluding people seen with newly diagnosed T1D in hospital, the majority (63%) of people seen in the clinic had a disease duration greater than 11 years (median). Of these, 30/88 (34%) entered the service following an acute ED presentation or inpatient admission, 14/88 (16%) entered the service once pregnant and 27/88 (31%) were referred by the GP after a mean duration of 22 years of T1D. For the chart review, only one set of paper records was missing. Table 1 shows the characteristics of the cohort. The mean age was 41.4 ± 12.7 years, of whom 55% were men and 77.5% were born in Australia. The majority of people (81.1%) were treated with a basal-bolus insulin regimen and 16.2% used an insulin pump. Overall, 55.5% of people used carbohydrate counting to calculate their bolus insulin dosing. The median diabetes duration was 11 years (range 0.1—54.0). Twenty-five of eighty people (31.2%) with documented smoking status were smokers.
Table 2 compares the metabolic levels and screening rates achieved with the guideline targets and national cohort data. While the HbA1c of the majority of people was above the national target of < 7%, the mean was below that achieved in ANDA. Almost all people with T1D (94.8%) were self-monitoring blood glucose at least daily, with a quarter testing ≥ 4 times/day as recommended, and a further 46.9% with the precise daily frequency unspecified. Overall, 13.6% of people experienced hypoglycaemia (< 4 mmol/L) on a daily basis. The mean systolic and diastolic blood pressures were within guideline target range, below the national mean, with 49.5% both systolic and diastolic blood pressure within target. The mean total cholesterol (TC) and low-density lipoprotein (LDL) cholesterol were both above target range, with < 20% achieving the lipid targets. Table 3 shows that recording metabolic, renal and foot assessments and attendance with educator or dietitian were generally the same or better than ANDA/UK National Diabetes Audit (UKNDA). However, BMI recording, podiatry and psychologist attendance were less frequent than ANDA. A relatively high proportion had evidence of nephropathy, peripheral neuropathy and macrovascular complications.
Figure 1 also shows the proportion of people who had one or more hospital admissions or ED presentations after entering the service by referral source, with the highest proportions amongst those referred following an acute hospital presentation or those referred by their GP.
When comparing those who were referred to the service acutely (i.e. following an acute inpatient admission, ED presentation or referral from another hospital) to non-acute referrals (i.e. those referred by the GP, transition clinic or other Endocrinologist), non-acute referrals were diagnosed at a younger age and had a longer duration of diabetes than those referred acutely (Table 4.)
Discussion
We studied 111 T1D adults who attended a multi-disciplinary public outpatient diabetes service in 2017 and found that our study population had a lower mean HbA1c and blood pressure compared to national data with high rates of patient education, educator and dietitian involvement. Despite this high quality of care, the prevalence of diabetes complications was high (31%) and 27% had one or more diabetes related admissions while under the service. Many were originally referred following an inpatient admission or emergency presentation due to either acute or chronic diabetes related issues, rather than from diagnosis. Similarly, those referred non-acutely from an outpatient setting tended to already have had their diabetes for many years.
While there are a range of studies of type 1 diabetes in childhood and the transition period [22,23,24], few exist focussing on those aged > 25 years i.e. from the end of the transition period. Most studies are national/international [12, 16, 17, 25] losing the granularity shown in our own study. As shown elsewhere, despite a suboptimal proportion of people achieving metabolic targets, most metabolic outcomes in our study compared favourably not only with the national standards shown in Tables 2–3, but also with other national and international data shown in Supplementary Table 1 [12, 16, 17, 25]. Among those not meeting blood pressure or total cholesterol targets, few were recorded as being on antihypertensive or lipid-lowering therapy respectively. Furthermore, of those receiving pharmacological therapies, a minority were meeting the metabolic targets [26, 27]. The prevalence of smoking was elevated at 31% compared to 12.7% in ANDA [12]. While this may be skewed by under-reporting of non-smokers among the 31 individuals without smoking status documented, even if all were non-current smokers, this would still indicate a high proportion of smokers (25/111 ie 23%). An alternative explanation is that the smoking is more associated with reduced self-management adherence [28] and/or more associated with co-morbidities [29], both increasing the chance of hospitalisation/referral.
Attendance rates with dietitians and diabetes educators were high, almost 1.5 times those reported in ANDA [13] and not shown in the other studies. This represents the multidisciplinary team (MDT) model of care used as part of best practice internationally [30, 31]. We anticipate rates of education to increase, as more OzDAFNE sessions are now being offered [32]. There were, however, lower recorded attendance rates to podiatrists (despite high rates of foot disease [33]), and mental health professionals, (despite high documented rates of depression). Moreover, it is likely that these rates of depression are under-reported due to poor record-keeping and compounded by high reported rates of psychological distress within the South West Sydney Local Health District, 2.1% above the state average [34]. These lower rates of access to mental health support are common both in Australia and internationally [35,36,37] and reflect the frequent absence of e.g. psychologists from the diabetes MDT (including this service).
Rates of retinopathy, peripheral neuropathy and macroalbuminuria were all higher than those reported in ANDA [12], including approximately double the prevalence reported for the latter two. Macrovascular complications were not reported for T1D alone in ANDA; however our study found markedly higher rates (6–12 fold) than the UKNDA [19], despite 30% of UKNDA subjects being under 30 years of age. We postulate that these complication rates are a consequence of delayed referral to specialist care.
Implications for practice
Multidisciplinary care provided by a public service represents an ideal model of care in T1D, which is accessible to all people regardless of financial status and able to be audited and regulated. This is exemplified by the largely tax funded Swedish healthcare system and UK National Health Service, whereby nearly all people with T1D attend multi-disciplinary specialist clinics through hospitals [38]. In Sweden, upon diagnosis of T1D, individuals are registered in diabetes registries and undergo annual quality registration. Under the NHS, it is possible to undertake national audits (e.g. the national diabetes in pregnancy audit [39] and implement and monitor national type 1 diabetes guidance [11]. In contrast, the current Australian healthcare system delivers fragmented, inconsistent diabetes care through a mixed private, public healthcare system. This is compounded by socioeconomic disparities, (e.g. in this catchment area) with rates of hospitalisation of people from low socioeconomic groups in Australia reported to be 1.6 times higher compared to those from higher socioeconomic groups (303 vs 195 per 100,000) [40].
Achieving metabolic targets nationally are also less likely due to less well-defined targets and treatment indications in Australian T1D treatment guidelines [10], in contrast to American [41] and UK guidelines [10, 42]. Whilst Australia has some care standards in place, they are poorly defined, particularly for T1D. This is in contrast to the UK system, which has nine well-defined annual care processes for T1D management, all of which are regularly audited. Furthermore, Australian guidelines lack specific clinical indications for commencing antihypertensive and lipid-lowering therapy in T1D.
Our interpretation of the metabolic outcomes and complication rates shown here is therefore that the while public hospital care reflects best practice, the local population “model of care” has led to a biased clinic population, often with poorly managed diabetes prior to entry into the clinic. This is also demonstrated in the discrepancy between median duration of diabetes (11 years) and median duration of clinic attendance (2 years). Essentially, the pattern seems to reflect a population-based model of care involving referral (or hospitalisation) after complications have developed, rather than a focus on preventative management. One alternative explanation for the concentration of those with complications in the clinic are that they are those attend the private sector until diabetes and/or non-diabetes related co-morbidities lead them to choose to consolidate care at the one site. However, a high proportion of attenders entered acutely and not by referral (i.e. by asking their GP for a referral). Alternatively, attenders may be those unable (e.g. through cost or health literacy issues) or unwilling to self-manage. Factors which may contribute to this pattern include a higher proportion from low socioeconomic groups and lower health literacy in the catchment. However, self-management and metabolic metric were as good, if not better than those in e.g. ANDA. Barriers to care have been minimised through e.g. reduced clinic waiting time for newly diagnosed patients, as referrals are triaged by an endocrinologist. Logistically, access to clinic is convenient with close proximity to public transport (train and bus stations) and readily available patient parking. Such factors are likely to be cost-saving for local patients particularly those with multiple co-morbidities/complications as care is delivered free of charge under Medicare, with ease of access to multiple other specialties and services from one location.
Strengths / Weaknesses
This is the first Australian study of its kind to show the current referral pathways into a multi-disciplinary public hospital diabetes clinic. Consistent practice standards and patient demographics of this clinic were strengthened by a breadth of data from multiple endocrinologists practicing in this service, thus not solely evaluating one physician’s quality of care.
This single-centre study was limited by a small study population, at a single site and represented a specific sample of people with T1D in an outer urban centre, hence may not be generalisable to the wider Australian outpatient diabetes clinic population. In addition, this study only analysed admissions to one hospital, hence is likely to underestimate admissions particularly in people with care and admissions elsewhere. Further multi-centre studies are needed to better understand the trends/disparities across various Australian outpatient diabetes clinics. As data were collected retrospectively, the medical records were variable with frequent missing data, only those seen by an endocrinologist in 2017 were included and causative analysis could not be performed. Medical records were fragmented and inconsistent. A more structured approach to medical records including use of diabetes registers, may help standardise and improve care and auditing processes. Since conducting this audit, this service has transitioned to electronic medical records and integrated the use of a secure, Australian web-based database (Biogrid Diabetes Database) designed by Endocrinologists to improve data collection and thus facilitate the ability to perform regular clinical care audits.
Thirteen percent of people were referred to the diabetes clinic by Obstetric colleagues. This could bias some of the metabolic outcomes favorably due to stricter targets in pregnancy. To account for this, HbA1c and blood pressure were also analysed with pregnant women excluded and the means remained lower than the national means [12]. These women are generally referred for glycaemic control during pregnancy, raising concerns in relation to whether these women received adequate pre-pregnancy counselling and glycaemic control [43, 44]. Pre-pregnancy planning clinics have since been introduced in this hospital.
Conclusion
In conclusion, quality of care in this clinic was in line, if not better, than national standards, with high rates of multidisciplinary team attendance and complication screening. This complex cohort illustrates a suboptimal population-based model of care as people with T1D are referred following a potentially preventable glycaemia related hospital presentation, and/or with longstanding diabetes duration. This is likely to reflect under-referral and thus, high rates of complications prior to enrolment in the local specialist service. Further work is needed to identify how widespread this “model of care” is under the Australian and other health systems, the reasons for under-management of T1D outside the public hospital specialist service and how to reduce hospital admissions and long-term complications.
Availability of data and materials
The data used in this study are not publicly available due to the sensitive nature of hospital patient data. For further details relating to the data, please contact the corresponding author.
Abbreviations
- T1D:
-
Type 1 diabetes
- DKA:
-
Diabetic ketoacidosis
- ANDA:
-
Australian National Diabetes Audit
- LADA:
-
Latent autoimmune diabetes in adults
- BMI:
-
Body mass index
- NICE:
-
National Institute for Health and Care Excellence
- ED:
-
Emergency Department
- OzDAFNE:
-
Australian Dose Adjustment for Normal Eating
- NDSS:
-
National Diabetes Services Scheme
- SD:
-
Standard deviation
- ANOVA:
-
Analysis of variance
- GP:
-
General practitioner
- UKNDA:
-
United Kingdom National Diabetes Audit
- MDT:
-
Multidisciplinary team
References
Comprehensive Medical Evaluation and Assessment of Comorbidities. Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(Supplement 1):S37–47.
Huo L, Harding JL, Peeters A, Shaw JE, Magliano DJ. Life expectancy of type 1 diabetic patients during 1997–2010: a national Australian registry-based cohort study. Diabetologia. 2016;59(6):1177–85.
Angus VC, Waugh N. Hospital admission patterns subsequent to diagnosis of type 1 diabetes in children : a systematic review. BMC Health Serv Res. 2007;7(1):199.
McIntyre HD, Knight BA, Harvey DM, Noud MN, Hagger VL, Gilshenan KS. Dose adjustment for normal eating (DAFNE) - an audit of outcomes in Australia. Med J Aust. 2010;192(11):637–40.
Elliott J, Jacques RM, Kruger J, Campbell MJ, Amiel SA, Mansell P, et al. Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with Type 1 diabetes. Diabet Med. 2014;31(7):847–53.
Diabetes Control and Complications Trial (DCCT) Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine. 1993;329(14):977–86.
Nathan DM. DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37(1):9–16.
Lv J, Perkovic V, Foote CV, Craig ME, Craig JC, Strippoli GF. Antihypertensive agents for preventing diabetic kidney disease. Cochrane Database of Systematic Reviews. 2012;12:CD004136.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Kearney PM, Blackwell L, Collins R, Keech A, Simes J, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371(9607):117–25.
Craig M, Twigg S, Donaghue K, Cheung N, Cameron F, Conn J, et al. National evidence-based clinical care guidelines for type 1 diabetes in children, adolescents and adults. Canberra: Australian Government Department of Health and Ageing. 2011;346.
Centre NCG. Type 1 diabetes in adults: diagnosis and management (NG 17). London: NICE; 2015.
Australian National Diabetes Audit - Australian Quality Clinical Audit Final Report. NADC; 2017.
Australian National Diabetes Audit - Australian Quality Self-Management Audit. NADC; 2018.
Gupta A, Taylor F, O’Sullivan T, Simmons D. Characteristics of young adults with multiple episodes of diabetic ketoacidosis. Intern Med J. 2019;49(7):911–4.
Burns K, Farrell K, Myszka R, Park K, Holmes-Walker DJ. Access to a youth-specific service for young adults with type 1 diabetes mellitus is associated with decreased hospital length of stay for diabetic ketoacidosis. Intern Med J. 2018;48(4):396–402.
Bryant W, Greenfield JR, Chisholm DJ, Campbell LV. Diabetes guidelines: easier to preach than to practise? Medical Journal of Australia. 2006;185(6):305–9.
McKnight JA, Wild SH, Lamb MJ, Cooper MN, Jones TW, Davis EA, et al. Glycaemic control of Type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabet Med. 2015;32(8):1036–50.
National Diabetes Audit - Report 1 Care Processes and Treatment Targets 2017–18. NHS Digital; 2019.
National Diabetes Audit Complications and Mortality 2015–2016. NHS Digital; 2017.
RACGP. General practice management of type 2 diabetes: 2016–18. East Melbourne, Vic: RACGP; 2016.
Lines S, Natarajan B. Proteinuria: The Renal Association; 2017 [Available from: https://renal.org/information-resources/the-uk-eckd-guide/proteinuria/.
Lyons SK, Libman IM, Sperling MA. Diabetes in the Adolescent: Transitional Issues. J Clin Endocrinol Metab. 2013;98(12):4639–45.
Maahs DM, Hermann JM, Holman N, Foster NC, Kapellen TM, Allgrove J, et al. Rates of Diabetic Ketoacidosis: International Comparison With 49,859 Pediatric Patients With Type 1 Diabetes From England, Wales, the U.S., Austria, and Germany. Diabetes Care. 2015;38(10):1876–82.
De Bock M, Jones TW, Fairchild J, Mouat F, Jefferies C. Children and adolescents with type 1 diabetes in Australasia: An online survey of model of care, workforce and outcomes. J Paediatr Child Health. 2019;55(1):82–6.
Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther. 2019;21(2):66–72.
Swasey KK, Orchard TJ, Costacou T. Trends in cardiovascular risk factor management in type 1 diabetes by sex. J Diabetes Complications. 2018;32(4):411–7.
Syed A, Hussain S, Nightingale P, De P, Charlton MH, Gangopadhyay K, et al. Cardiovascular risk factors and their management in 1282 adult people with type 1 diabetes. Curr Med Res Opin. 2007;23(12):2921–7.
Solberg LI. Diabetic Patients Who Smoke: Are They Different? The Annals of Family Medicine. 2004;2(1):26–32.
Śliwińska-Mossoń M, Milnerowicz H. The impact of smoking on the development of diabetes and its complications. Diab Vasc Dis Res. 2017;14(4):265–76.
Association AD. 1. Improving Care and Promoting Health in Populations: <em>Standards of Medical Care in Diabetes</em>—<em>2020</em>. Diabetes Care. 2020;43(Supplement 1):S7-S13.
Goenka N, Turner B, Vora J. Commissioning specialist diabetes services for adults with diabetes: summary of a Diabetes UK Task and Finish group report. Diabet Med. 2011;28(12):1494–500.
Dafne Study G. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746.
Osuagwu UL, Osuagwu J, Piya MK, Wong V, Simmons D. Prevalence of Diabetes Mellitus and Risk Factors in South Western Sydney: Where Are We Now? 2019.
District SWSLH. Health Profiles of Local Communities. In: District SWSLH, editor.: NSW Health; 2014.
Petrak F, Baumeister H, Skinner TC, Brown A, Holt RIG. Depression and diabetes: treatment and health-care delivery. Lancet Diabetes Endocrinol. 2015;3(6):472–85.
Diabetes U. Minding the Gap: the provision of psychological support and care for people with diabetes in the UK. 2008.
Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22(10):1379–85.
Simmons D, Wenzel H, Zgibor JC. Integrated Diabetes Care: A Multidisciplinary Approach: Springer; 2016.
Digital N. National Pregnancy in Diabetes (NPID) Audit Report 2018. UK; 2019.
Health AIo, Welfare. Diabetes. Canberra: AIHW; 2019.
Standards of Medical Care in Diabetes—2019 Abridged for Primary Care Providers. Clinical Diabetes. 2019;37(1):11–34.
Cardiovascular disease: risk assessment and reduction, including lipid modification [CG181]. NICE; 2014.
Ray JG, O’Brien TE, Chan WS. Preconception care and the risk of congenital anomalies in the offspring of women with diabetes mellitus: a meta-analysis. QJM. 2001;94(8):435–44.
Sina M, Macmillan F, Dune T, Balasuriya N, Khouri N, Nguyen N, et al. Development of an integrated, district-wide approach to pre-pregnancy management for women with pre-existing diabetes in a multi-ethnic population. BMC Pregnancy and Childbirth. 2018;18(1).
Acknowledgements
This work was undertaken as an Royal Australian College of Physicians project by SP and a Western Sydney University Honours project by CF. We thank the Macarthur Diabetes Service for their assistance.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
SP and CF equally contributed to data collection, analysis and writing the manuscript. DS assisted with audit design, statistical analysis and manuscript review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project was approved as a quality assurance activity by the Quality and Safety Office, under the ethical framework overseen by the South Western Sydney Local Health District Human Research Ethics Committee (CT01_2017, 1/07/2017). As a retrospective quality improvement audit, a waiver of individual patient consent was approved by the SWSLHD HREC, and this study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12902_2022_1057_MOESM1_ESM.docx
Additional file 1: Supplementary Table 1. Proportion of people with T1D achieving metabolic targets in selected published audits
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Patel, S., Farkash, C. & Simmons, D. Type 1 diabetes management and hospitalisation in the over 25’s at an Australian outer urban diabetes clinic. BMC Endocr Disord 22, 143 (2022). https://doi.org/10.1186/s12902-022-01057-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01057-9